Abstract
In June 2000 the ERA-EDTA Registry office moved to Amsterdam and started collecting core data on renal replacement therapy (RRT) entirely through national and regional registries. This paper reports the pediatric data from 12 registries. The analysis comprised 3,184 patients aged less than 20 years and starting RRT between 1980 and the end of 2000. The incidence of RRT rose from 7.1 per million of age-related population (pmarp) in the 1980–1984 cohort to 9.9 pmarp in the 1985–1989 cohort, and remained stable thereafter. The prevalence increased from 22.9 pmarp in 1980 to 62.1 in 2000. Hemodialysis was the commonest form of treatment at the start of dialysis, but peritoneal dialysis gained popularity during the late 1980s. Pre-emptive transplantation accounted for 18% of the first treatment modality in the 1995–2000 cohort. The relative risk of death of patients starting dialysis in the period 1995–2000 was reduced by 36% {adjusted hazard ratio (AHR) 0.64 [95% confidence interval (CI) 0.41–1.00]} and that of those receiving a first allograft by 42% [AHR 0.58 (95% CI 0.34–1.00)], compared with patients in the period 1980–1984. The prevalence of RRT in children has continued to rise, while its incidence has been stable for about 15 years. Patient survival has improved in both dialysis patients and transplant recipients. The development of this pediatric registry will form the basis for more-detailed and focused studies in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
When dialysis and renal transplantation were first established in the 1960s treatment was offered mainly to young adults, but once its success had been established treatment was extended to older children. Shortly thereafter, a few pioneering centers developed techniques for the treatment of very small children and infants. At that time the results of the treatment of children were less good in terms of patient and graft survival than for adults, reflecting some of the technical difficulties. Also the quality of life was often unsatisfactory. This initial phase was followed by the development of an increasing number of specialist pediatric nephrology centers with staff experienced in technical aspects of renal replacement therapy (RRT) as well as in the care of children in terms of growth, development, and emotional and psychosocial needs. In Europe the ERA-EDTA Registry used to gather data on RRT in children mainly from individual renal units by means of center and patient questionnaires, and the results were published as an annual report, the most recent of which was in 1996 [1].
In June 2000 the ERA-EDTA Registry office moved to the Academic Medical Center in Amsterdam and it was decided at this time that data would be collected exclusively from national and regional registries [2]. A new database was built in order to combine data from different countries and the first report was published the following year [3]. The European Society of Paediatric Nephrology decided to join this new registry. The aim of this paper is to describe the first results of data collection in the pediatric population from 12 national and regional registries.
Materials and methods
Data collection
Data from the renal registries of Austria, Dutch-speaking Belgium, French-speaking Belgium, Catalonia (Spain), Denmark, Finland, Greece, Iceland, The Netherlands, Norway, Scotland (UK), and Sweden were chosen for inclusion in this report because of the quality and the availability of their data. Data from 7 of these registries were available for the years 1980–2000. Data from Dutch-speaking Belgium were available for 1994–2000, from French-speaking Belgium for 1985–2000, from Catalonia for the years 1985–2000, from Denmark for the years 1990–2000, and from Sweden for the years 1991–2000. The data consisted of a limited number of patient and treatment variables. This set included a meaningless national registry patient identifier, date of birth, gender, primary renal disease, date of start of first RRT, history of RRT with dates and changes of modality, treatment center, date and cause of death, and information concerning transfer from or to other renal registries. Details about data collection and data processing have been described previously [3].
Data analysis
The date of onset of end-stage renal disease (ESRD) was defined as the date of start of RRT. All children and young people less than 20 years at the start of RRT were included. We excluded patients not residing in the area of a contributing registry and patients with a missing start date. The incidence of RRT was defined as the number of new cases per year. The prevalence was defined as the number of patients alive and on RRT on 31 December. For both parameters the mid-year population was used as denominator. Renal diseases and causes of death were defined according to the ERA-EDTA coding systems, and subsequently classified into groups (see Appendix). To allow analysis of differences related to age, the data were analyzed in four equal age bands 0–4, 5–9, 10–14, and 15–19 years. These age bands were chosen because they correspond to widely available population statistics. The age group of 15–19 years was included because several important aspects of growth and development occur at this age. In order to evaluate the changes in patient characteristics, treatment, and outcome with time the data were analyzed in four cohorts 1980–1984, 1985–1989, 1990–1994, and 1995–2000.
Differences between groups were analyzed with chi-square tests for categorical variables. A two-sided P value less than 0.05 was considered statistically significant. Statistical analysis of mortality was performed by the Kaplan-Meier method and by Cox proportional hazards regression. In the latter analysis, the relative risk of death was expressed as the adjusted hazard ratio (AHR). The 1st day on dialysis when this was the first form of RRT was taken as the starting point for the analysis of patient survival on dialysis. The death of the patient was the event studied. Transplantation, recovery of renal function, and loss to follow-up were censored observations. For the analysis of patient survival after transplantation, we took the date of the first renal transplant as the 1st day of follow-up. Death was the event, whereas the follow-up time was censored at loss of follow-up. The follow-up time of patients alive and on RRT as of 31 December 2000 was censored at that date.
Results
There were 3,184 patients from 12 registries who started RRT during the period 1980–2000 included in the study. Table 1 shows the general population statistics of these countries or regions, according to registry of origin. Figure 1 shows the incidence of RRT per million of age-related population (pmarp) by registry (upper panel) and by age group (lower panel). Overall, the incidence of RRT for patients aged 0–19 years was 7.1 pmarp in the period 1980–1984 and in the 15 years thereafter was relatively stable at 9 to 10 pmarp. The incidence was highest in the 15- to 19-year age group. In children aged 0–4 years there was an almost threefold increase with time from 2.4 pmarp in 1980–1984 to 6.2 pmarp in 1985–1989. There was a high incidence of RRT in these children aged 0–4 years in Finland (15.5 pmarp in 1995–2000) due to the large number of infants in this country with hereditary nephropathy. Figure 2 shows the increase in prevalence of RRT in children and adolescents from 22.9 pmarp in 1980 to 62.1 pmarp in 2000.
Table 2 shows the contribution in incident patients of the commonest conditions leading to chronic renal failure. Hypoplasia/dysplasia and hereditary diseases were the commonest in the 0- to 4-year age group, while glomerulonephritis and pyelonephritis became progressively more common with increasing age. There was little gender difference between the disease groups, apart from pyelonephritis, hypoplasia/dysplasia, and hereditary nephropathy, which were more common in males.
Table 3 shows the changes with time of the first treatment modality in the different age groups. Overall, hemodialysis was the commonest form of treatment at the start (day 1) of RRT in the cohort 1995–2000 (48%), followed by peritoneal dialysis (34%), while pre-emptive transplantation accounted for the remaining 18%. Hemodialysis was used much more often in the older children, while peritoneal dialysis was the preferred therapy in children below 5 years of age. Table 3 also shows that peritoneal dialysis and transplantation were more often the first treatment modality in recent years compared with the 1980–1984 time period. There was a large difference between countries in the initial form of RRT, as shown in Fig. 3. Pre-emptive transplantation was most commonly used in Norway, Sweden, and Denmark, while peritoneal dialysis was most popular in Finland, Scotland, and the Netherlands. The frequent use of peritoneal dialysis in Finland occurred in all age groups and was therefore not due to the high incidence of hereditary nephropathy alone. Table 4 shows that the number of transplants pmarp in children aged 0–4 years has now reached the level of that in the other pediatric age categories.
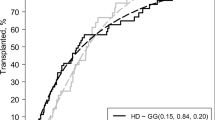
In dialysis patients the crude 2-year patient survival in the 0- to 19-year age group increased from 90.9% in 1980–1984 to 94.2% in 1995–2000, whereas in transplant recipients it rose from 95.2% to 96.9%. The greatest improvements have been achieved in the youngest age group. In these children aged 0–4 years the 2-year survival in dialysis patients increased from 71.3% in 1980–1984 to 87.9% in 1995–2000. Also in this age group patient survival following renal transplantation rose from 93.6% in 1985–1989 (this time period was taken as a reference, as in 1980–1984 the number of transplant recipients in this age category was too low for statistical analysis) to 97.6% in 1995–2000. Figure 4 shows the improvement in survival in dialysis patients over time, adjusted for age and gender. In patients aged 0–19 years the relative risk of death of those patients starting dialysis in the period 1995–2000 was 0.64 [95% confidence interval (CI) 0.41–1.00] compared with patients starting dialysis in 1980–1984. The improvement was greatest in the subgroup of patients aged 0–4 years AHR 0.21, 95% CI 0.09–0.51. An even greater improvement was observed in the survival of transplant recipients (Fig. 5). Adjusted for age, gender, and donor type the relative risk of death of those aged 0–19 years receiving a first renal allograft in 1995–2000 was 0.58 (95% CI 0.34–1.00), compared with patients in the 1980–1984 period.
The causes of death are shown in Fig. 6. Infection and cardiac causes comprised the major categories, although almost one-quarter was classified as unknown. Cardiac causes of death predominated in those on hemodialysis, in contrast to infections in patients on peritoneal dialysis or those with a functioning graft. Of the separate codes, cerebrovascular accident, cardiac arrest, and septicemia were those most frequently reported in all modalities, accounting for respectively 8.0%, 7.4%, and 7.1% of all deaths in the entire group. Potentially preventable causes of death, such as hyperkalemia, hypertensive cardiac failure, fluid overload, and cerebrovascular accident, together accounted for 15.4% in the entire group, and for 21.1%, 10.3%, and 11.7% in the hemodialysis, peritoneal dialysis, and transplant patients, respectively. In 2.0% of the 6.7% of hemodialysis patients who died of a malignancy, this malignancy had possibly been induced by immunosuppressive therapy after a previous transplant.
Discussion
These data are the first for children on RRT in Europe that have been produced by the ERA-EDTA Registry since its problems with data collection during the late 1990s. In June 2000, the ERA-EDTA Registry changed its policy of data collection, moved its office to Amsterdam, and started an entirely new database. The data are now obtained only from national or large regional registries that can provide complete and accurate data. Thus reliance can be placed on their quality. The development of this new ERA-EDTA database not only permits comparisons of pediatric RRT data between countries in Europe but also with registry data elsewhere in the world. The combined pediatric and adult database will enable it in future studies to look at the impact of renal failure in childhood on life expectancy and quality of life in adulthood.
There has been no major change among the countries surveyed in the number of older children accepted for RRT over the past 20 years. This contrasts with the large increase during the 1980s in the age group up to 5 years. The latter may reflect the improving skill and confidence of pediatric nephrologists in overcoming the technical problems associated with RRT among infants and very young children. The much higher incidence of RRT in children classified as having hereditary nephropathy in Finland is due to congenital nephrosis (Finnish type), which is currently the most-common cause of ESRD in that country among children below 15 years of age [4]. Our analysis shows that the incidence of RRT in children in Europe is similar to that reported in US whites below the age of 10 years, but lower than in US whites in the age groups 10–14 and 15–19 years [5]. The incidence of RRT in Australia, however, is quite similar to ours across all childhood age categories [6].
As one would expect, RRT prevalence rates have continued to rise as a consequence of improving patient survival together with the increase in RRT incidence which took place during the 1980s. The overall prevalence has more than doubled over the 20 years of the current analysis. Also there was a wide geographical variation in prevalence of RRT in children. One can at present only speculate as to the reasons for these differences between countries, but the aim of future analyses will be to answer this question. As with incidence, the prevalence of RRT in Europe was similar to that of Australia across all age categories [6], but compared with the United States the European prevalence was lower in the 10- to 14- and 15- to 19-year age groups [5].
This analysis confirmed what had been expected with regard to the types of primary renal disease, in that glomerulonephritis and pyelonephritis predominated in the older child, as in other parts of the world [5, 6]. Cystic kidneys, hypoplasia/dysplasia, and hemolytic uremic syndrome have contributed to a lesser degree throughout the pediatric age groups, while hereditary disease and hypoplasia/dysplasia, as elsewhere, have been the main causes of ESRD in the 0- to 4-year age group [6].
Our analysis has shown wide variations in first treatment modality with regard both to age group and country. Peritoneal dialysis has predominated in infancy, giving way to hemodialysis with increasing age. Pre-emptive transplantation has made a smaller but useful contribution, being used in 13%–25% of patients in 1995–2000 depending on age group, with little change with time over the last 15 years. A similar pattern of treatment modalities across age categories has been reported from Australia [6]. It is disappointing to note from our data the absence of any major increase in the rate of pre-emptive transplantation since the time period 1985–1990, in view of its advantages over dialysis. Norway has had the highest pre-emptive transplant rate, which is in line with the emphasis in that country on transplantation as the main form of RRT in all age groups. Hemodialysis was the commoner type of dialysis in all countries except Finland where peritoneal dialysis has predominated. The predominance of peritoneal dialysis in this country can be explained only to a limited extent by the large number of very young children on RRT.
Our data confirm the findings of others reporting a lower survival for younger children [5, 7]. As in other studies [8, 9, 10], we noted an improvement with time in patient survival among both dialysis and transplanted patients, although most of the improvement in the transplant recipients occurred prior to 1995. It is encouraging to note that in the most-difficult age group to treat, i.e., those under 5 years, the mortality has continued to fall in more-recent years. The improvement of patient survival among transplant recipients is at least in part explained by the better graft survival in the recent past [11].
In general, the pattern of the causes of death in this analysis was comparable to that in other countries, where cardiac and infectious disease compete for the role of leading cause of death [5, 7, 12]. However, the high percentage of causes reported as unknown in our series complicates the interpretation of the data. The current high survival rates in pediatric RRT patients will make it difficult to achieve much further improvement over the next few years. Further efforts should however be made to reduce the number of potentially preventable cases of death, which now comprise up to 21.1% of deaths in hemodialysis patients.
In conclusion, this first analysis of pediatric data from the Amsterdam-based ERA-EDTA Registry has shown that the prevalence of RRT has continued to increase, while the rise in incidence has flattened out over the past 15 years. Peritoneal dialysis has tended to increase over time as a first treatment modality at the expense of hemodialysis, with considerable variation between countries. It is disappointing that the rate of pre-emptive transplantation has failed to increase since 1985. Overall, pediatric patient survival on RRT improved to an important extent, especially in children under 5 years. Over the next few years it is planned to extend our analyses as additional registries become affiliated to the ERA-EDTA Registry. This will increase the scope for further comparisons between European countries and other international registries.
References
Mehls O, Rigden S, Ehrich JHH, Berthoux F, Jones EHP, Valderrabano F (1996) Report on management of renal failure in Europe, XXV, 1994. The child-adult interface. Nephrol Dial Transplant 11 [Suppl1]:22–36
Briggs JD, Jager KJ (2001) The first year of the new ERA-EDTA Registry. Nephrol Dial Transplant 16:1130–1131
Dijk PCW van, Jager KJ, Charro F de, Collart F, Cornet R, Dekker FW, Grönhagen-Riska C, Kramar R, Leivestad T, Simpson K, Briggs JD (2001) Renal replacement therapy in Europe: the results of a collaborative effort by the ERA-EDTA registry and six national or regional registries. Nephrol Dial Transplant 16:1120–1129
Finnish Registry for Kidney Diseases (1999) Report 1998, Helsinki, p 7
US Renal Data System (2001) USRDS 2001 Annual Data Report: atlas of end-stage renal disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, Md, pp 107–116
Craig JC (2001) Paediatrics. In: Russ GR (ed) ANZDATA Registry Report 2001. Australia and New Zealand Dialysis and Transplant Registry, Adelaide, South Australia, pp 91–93
Neu AM, Ho PLM, McDonald RA, Warady BA (2002) Chronic dialysis in children and adolescents. The 2001 NAPRTCS Annual Report. Pediatr Nephrol 17:656–663
Goh D, Evans JHC, Houston IB, Mallick NP, Morton MJS, Johnson RWG, Postlethwaite RJ (1994) The changing pattern of children’s dialysis and transplantation over 20 years. Clin Nephrol 42:227–231
Reiss U, Wingen AM, Schärer K (1996) Mortality trends in pediatric patients with chronic renal failure. Pediatr Nephrol 10:41–45
Groothoff JW, Gruppen MP, Offringa M, Hutten J, Lilien MR, Kar NJ van de, Wolff ED, Davin JC, Heymans HSA (2002) Mortality and causes of death of end-stage renal disease in children: a Dutch cohort study. Kidney Int 61:621–629
Elshihabi I, Chavers B, Donaldson L, Emmett L, Tejani A (2000) Continuing improvement in cadaver donor graft survival in North American children. The 1998 Annual Report of the North American Renal Transplant Cooperative Study (NAPRTCS). Pediatr Transplant 4:235–246
Schärer K, Reiss U, Mehls O, Gretz N, Möhring K, Müller-Wiefel DE, Wingen A (1993) Changing pattern of chronic renal failure and renal replacement therapy in children and adolescents: a 20-year single center study. Eur J Pediatr 152:166–171
Acknowledgements.
We would like to thank the patients and staff of all the dialysis and transplant units who have contributed data via their national and regional renal registries. We also would like to thank the following registries for the contribution of these data: Austrian Dialysis and Transplant Registry (OEDTR), General Hospital of Wels, Wels, Austria (Dr. R. Kramar, Dr. H.K. Stumvoll); Dutch-speaking Belgian Registry (Dr. J. Donck, Ir H. Augustijn); French-Belgian Nephrologists Registry, Centre Hospitalier Etterbeek-Ixelles, Brussels, Belgium (Dr. F. Collart); Registry of Renal Patients (RMRC), Catalan Transplant Organization (OCATT), Barcelona, Spain (Dr. M. Clèries, Mr. E. Vela); Danish National Registry (Dr. H. Løkkegaard); Finnish Kidney Disease Registry and Department of Medicine, Helsinki University Hospital, Helsinki, Finland (Dr. C. Grönhagen-Riska, Dr. P. Finne); Greek National Registry, General Hospital of Athens G. Gennimatas, Athens, Greece (Dr. G.A. Ioannidis, Dr. N. Papagalanis); Icelandic Renal Registry, Landspitali—University Hospital, Reykjavik, Iceland (Dr. P. Asmundsson); Dutch End-Stage Renal Disease Registry (RENINE), Erasmus University Hospital, Rotterdam, The Netherlands (Dr. F.T. de Charro); Norwegian Renal Registry, Institute of Immunology, Rikshospitalet University Hospital, Oslo, Norway (Dr. T. Leivestad); Scottish Renal Registry, Glasgow Royal Infirmary, Glasgow, Scotland, UK (Dr. K. Simpson); Swedish Registry for Active treatment of Uremia, Skövde, Sweden (Dr. J. Ahlmén, Dr. S. Schön) and the other ERA-EDTA Registry committee members and ERA-EDTA Registry staff members for their advice in the analysis and the drafting of this paper: Dr. G. Colasanti, Ir. R. Cornet, Dr. F.W. Dekker, Dr. C. Grönhagen-Riska, Dr. T. Feest, Dr. H.J. Schober-Halstenberg, Dr. K. Simpson, Dr. B. Stengel, and Dr. D. Tsakiris. The ERA-EDTA Registry is funded by the European Renal Association-European Dialysis and Transplant Association (ERA-EDTA). The following companies have committed funds in the form of unrestricted educational grants to assist the ERA-EDTA in the financial support of the Registry: Amgen, Baxter, Fresenius Medical Care, Gambro, Hoffmann-La Roche, Hospal, Ortho-Biotech and Shire.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
ERA-EDTA codes for primary renal disease (Table 5) and cause of death (Table 6) in children.
Rights and permissions
About this article
Cite this article
van der Heijden, B.J., van Dijk, P.C.W., Verrier-Jones, K. et al. Renal replacement therapy in children: data from 12 registries in Europe. Pediatr Nephrol 19, 213–221 (2004). https://doi.org/10.1007/s00467-003-1376-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-003-1376-x