Abstract
World Kidney Day (WKD) is intended to raise awareness and increase detection of chronic kidney disease (CKD), but most emphasis is placed on adults rather than children. We examined yield of screening for CKD and hypertension among poor children in Mexico. On WKD (2006, 2007), children (age < 18 years) without known CKD were invited to participate at two screening stations. We measured body mass index (BMI), blood pressure, and serum creatinine, and performed dipstick urinalysis. The Schwartz equation was used to estimate glomerular filtration rate (GFR; reduced GFR defined as < 60 ml/min per 1.73 m2). Proteinuria and hematuria were defined by a reading of ≥ 1+ protein or blood on dipstick. Hypertension was defined by gender, age, and height-specific norms. In total, 240 children were screened (mean age 8.9 ± 4.1 years; 44.2% male). Proteinuria and hematuria were detected in 38 (16.1%) and 41 (17.5%), respectively; 15% had BMI > 95th percentile for age. Reduced GFR was detected in four (1.7%) individuals. Systolic hypertension was more prevalent in younger children (age 0–8 years, 19.6%; age 9–13 years, 7.1%; age 14–17 years, 5.3%) suggesting a possible white-coat effect. Hematuria, proteinuria, hypertension and obesity were frequently detected among children in a community based screening program in Mexico. This form of screening might be useful in identifying children with CKD and hypertension in developing nations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
World Kidney Day (WKD) is an initiative of the International Society of Nephrology and International Federation of Kidney Foundations that is intended to raise awareness and increase the detection of chronic kidney disease (CKD) in the general population [1]. The message of WKD is that kidney disease is ‘common’, ‘harmful’ and ‘treatable’. The initiative calls for CKD to be recognized as a global public health problem while promoting early detection and treatment of CKD, a focus particularly relevant as treatment for end-stage renal disease with dialysis and transplantation may not be affordable or accessible to many living in developing nations.
CKD has been become a ‘silent epidemic’ in developing countries, mainly due to an increasing prevalence of diabetes and hypertension in the general population [2–4]. To date, most of the public campaigns for detection of CKD and its risk factors have placed emphasis on adults rather than children. Screening programs for CKD in healthy adults have been performed in several countries, including Mexico [5, 6]; however, there is little information on such programs performed among children living in developing countries [3]. The screening of children may provide an early opportunity for identification of risk factors and, ultimately, prevention of CKD in adulthood [7, 8].
We conducted a cross-sectional study to examine the diagnostic yield of screening for chronic kidney disease and hypertension among children in poor Jalisco neighborhoods in Mexico on World Kidney Day in 2006 and 2007.
Methods
Children in Jalisco state
The state of Jalisco is in western Mexico and has a population of 6.7 million, of whom approximately 60% live in the capital city of Guadalajara, with the remainder dispersed in urban and rural areas. Approximately 2.7 million (41%) are children aged less than 20 years [9]. Standards of living have risen in recent decades, and per capita income is approximately US$ 6,000 per annum, although 10% of Jalisco households currently do not have running water or sewage systems [10]. Approximately 42% of Jalisco children are members of poor families, with a daily household income < US$ 13 [9]. Although child mortality rates in Jalisco have decreased over the past 25 years, the mortality rate among children is still considerably higher than in developed countries, at 14.4/1,000 live births in 2006 [11].
The public healthcare system in Jalisco (like elsewhere in Mexico) is multi-tiered and highly centralized. Social security benefits are available to individuals employed by corporations or the state, although this represents less than half of the Jalisco population. Fewer than 2% of the population can afford private health insurance. The remaining 56% do not have access to social security and cannot afford access to private healthcare services. Primary care for uninsured children in Jalisco is provided by the facilities of the state Health Secretariat and by the Hospitales Civiles de Guadalajara. Approximately 44% of the population < 19 years old have no access to primary care. The Hospitales Civiles de Guadalajara has two large healthcare facilities that serve children without social security coverage. In 2007, close to 50,000 outpatient clinic visits and 10,000 hospitalizations were recorded. The two facilities are staffed by 142 pediatricians and offer almost all subspecialty services. Renal care for children is delivered by four pediatric nephrologists.
Details of screening program
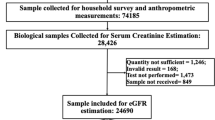
On World Kidney Day in 2006 and 2007, medical staff from the Hospitales Civiles de Guadalajara set up screening stations at the two hospital facilities. The screening staff included nephrologists for both adults and children, nephrology fellows, dieticians and medical students. Screening programs were preceded by a 2-week promotional campaign prior to WKD using print, radio and television media and noted a personal or family history of diabetes or hypertension (and a family history of kidney disease) as major risk factors for CKD. All interested individuals were invited to participate. Persons who were aware that they had “kidney disease” and those > 18 years of age were excluded from this analysis.
Data were collected by the screening program staff using a standard form. All screening staff were instructed on how to read urine dipsticks and take blood pressure measurements prior to start of screening. Baseline data obtained from each participant or parent/guardian on World Kidney Day in 2006 included age, gender, and personal history of diabetes, hypertension, or nephrolithiasis. Height (in centimeters) and weight (in kilograms) were measured and used to calculate body mass index (in kilograms, per meter squared). Systolic and diastolic blood pressures were measured with manual sphygmomanometers (Welch Allyn, New York, USA) and cuffs appropriate for the patient′s sizes [12]. All participants were asked to provide blood and urine specimens, which were used for measurement of serum creatinine (in milligrams per deciliter) (Abbott Clinical Chemistry, Abbott Laboratories, USA) and for dipstick urinalysis (Multistix 10 SG, Bayer de Mexico, S.A. de C.V., Mexico). An identical process was used on World Kidney Day 2007, except that participants or parents were also asked if they had a family history of diabetes, hypertension or kidney disease.
The screening test results were available on the same day by noon. Serum creatinine measurements were processed in the participating hospitals′ laboratories. Screening program participants returned to the hospital to obtain their test results the same day. Abnormal screening test results were conveyed to parents or guardians of participating children. Those with abnormal results were then referred to pediatric nephrology clinics for a full assessment. Some of the following tests were performed or repeated as indicated: urinalysis, urine culture, complete blood count, serum creatinine, serum urea, creatinine clearance, 24 h urine protein excretion, kidney ultrasound and kidney biopsy.
Definitions of proteinuria, hematuria, hypertension and glomerular filtration rate
Proteinuria and hematuria were defined as 1+ or greater protein and 1+ or greater blood, respectively, on dipstick urinalysis [13]. The study subjects were considered hypertensive if their measured blood pressure was ≥ 95th percentile for age, gender and height according to published normative values [12]. The Schwartz formula using serum creatinine, height of patient and appropriate constant was used to estimate glomerular filtration rate (GFR) [14–17].
Analytical methods
Means, standard deviations (SDs) and percentages were used to describe data as appropriate. Outcomes of interest included hematuria, proteinuria, GFR < 60 ml/min/1.73 m2 and hypertension as defined above. Numbers needed to screen (NNS) were calculated in the standard fashion [18]. Body mass index (kilograms, per meter squared) percentiles (BMI) were calculated for each participant according to normative values in the Centers for Disease Control and Prevention growth charts [19]. Children older than 2 years and with BMI > 95th percentile were classified as overweight [20]. Statistical analyses were performed with Stata software, version 9.1 (College Station, Texas, USA) and SAS software, version 9.1 (Cary, NC, USA). This study was approved by the institutional review boards at the Hospital Civil de Guadalajara and the University of Alberta, who waived the requirement for participants to provide informed consent.
Results
Study population
In total 240 children (44.2% male) participated in the WKD 2006 (n = 122) and 2007 (n = 118) screening programs. The demographic and clinical characteristics of the participants are shown in Table 1. Among study participants, the distribution of observed BMI was right-shifted when compared to normative values (Fig. 1), reflecting a higher proportion of obese children among those screened than in the general United States population. Specifically, 15% of all subjects were overweight as defined by BMI > 95th percentile for age and gender.
Prevalence of urinary abnormalities, hypertension, and reduced glomerular filtration rate
The prevalences of urinary abnormalities are shown in Table 2.
Approximately 16.1% of participants had proteinuria, and 17.5% had hematuria. Hypertension was detected more commonly among younger children (ages 0–8 years) and prevalence decreased in older children. Greater than 90% of the children screened had normal GFR. However, four (1.7%) patients had GFR < 60 ml/min per 1.73 m2, and 12 (5.1%) patients had GFR < 60–90 ml/min per 1.73 m2.
Potential yield of screening
We calculated the number of participants in whom screening would be required to detect one case of hematuria, proteinuria or systolic hypertension. When the entire population was considered, the number needed to screen (NNS) was 6 [95% confidence interval (95%CI) 4, 8] and 6 (95%CI 5, 9) to detect one case of hematuria and proteinuria, respectively. The number needed to be screened to detect one case of systolic hypertension was 8 (95%CI 6, 12). The results were similar across strata defined by age and gender (data not shown).
Follow-up of abnormal screening test results
All children with proteinuria, hypertension, and reduced GFR were seen in follow-up clinics at the participating pediatric nephrology centers in Guadalajara. Urinary abnormalities persisted in 38 (15.8%) children. Twelve (5%) of these had proteinuria >500 mg/day. Creatinine clearance was <80 ml/min per 1.73 m2 in 9 (3.7%) children. Seven patients had undergone kidney biopsy, and, of these children, four had mesangial proliferation and three were diagnosed with focal segmental glomerulosclerosis. Appropriate treatments were arranged for these children at the discretion of the attending pediatric nephrologists.
Discussion
Urinary abnormalities and hypertension were frequently detected in children in a community based screening program carried out in Mexico on WKD, and 1.7% of participants had GFR < 60 ml/min per 1.73 m2. During follow-up for abnormal screening test results, 15.8% children had persistent urinary abnormalities and 3.7% had creatinine clearance < 80 ml/min per 1.73 m2. Overall, the number of participants that would need to be screened in order for an abnormality to be detected was favorable and remained less than 10 for all subgroups considered. These findings suggest that the use of a similar case-finding technique in other Mexican communities would be useful to detect CKD and hypertension among asymptomatic children. Owing to the select nature of participants identified by the advertising campaign, further studies are required to determine whether more broadly targeted screening of children would also have had acceptable yield.
Community wide urinary screening has been performed in other Latin American countries, including Mexico. The estimated prevalence of proteinuria in the Mexican general population aged between 20 years and 69 years was 9.2% in 2000 [6]. In Bolivia, among apparently healthy subjects, many of whom were children, the prevalence of hematuria and proteinuria was 14.3% and 2.1%, respectively. Similar data for the prevalence of hypertension among children in developing nations are not readily available. Nevertheless, the prevalence of hypertension among older children in our study is consistent with school-based screening studies in developed countries, which report a prevalence ranging from 1.8–4.2% in Europe and 4.5–13.8% in the USA [21–25]. The prevalence of hypertension was higher among the younger participants in this study; this may be partially attributed to a white-coat effect. Younger children may be more susceptible to spuriously elevated blood pressure in a clinical setting [26].
Obesity is becoming a common cause of childhood hypertension in affluent countries [12, 27]. Approximately 20% of school age children in the USA are overweight [21], with especially rapid increases in prevalence among certain ethnic groups. For example, among Mexican–American adolescents, the prevalence of obesity increased by more than 10% between 1988–1994 and 1999–2000 [27]. Among the children in our study, more than half had BMIs greater than the 50th percentile for age, and 15% had BMI > 95th percentile [19], confirming that obesity is common (21%) among Jalisco children in the current era [9]. Since our study was cross-sectional, we cannot confirm whether the prevalence of obesity is increasing over time. If true, this would imply that the prevalence of hypertension among Jalisco children will also continue to increase. Increasing rates of obesity in children have been linked to a higher prevalence of hypertension, which, in turn, is a major risk factor for CKD and cardiovascular disease [12, 28].
Although end-stage renal disease is rare in the pediatric population, there are environmental, racial, genetic, cultural and socioeconomic differences that affect its incidence and prevalence. Population-based estimates of the prevalence of childhood CKD and end-stage renal disease (ESRD) in developed nations have been described. The recently published population-based data from the ItalKid project quotes a mean prevalence of creatinine clearance <75 ml/min per 1.73 m2 as 74.7 cases per year per million of the age-related population younger than 20 years [29]. In 2005 the Canadian Organ Replacement Registry reported a range of age-specific incidence rates of ESRD from a minimum of 5.4 per million population in girls aged 5–9 years to a maximum of 21.8 per million population in young men aged 15–19 years [Canadian Institute for Health Information, Canadian Organ Replacement Register (200 X data) (2009), Canada, personal communication]. Data on incidence and prevalence of CKD are not available from developing nations due to reduced healthcare resources and lack of organized efforts to detect CKD or document ESRD among children. Although limited by a small number of study subjects, we found that 1.7% of screened asymptomatic subjects had GFRs < 60 ml/min per 1.73 m2, and, at follow-up, 3.7% had creatinine clearances < 80 ml/min per 1.73 m2. These results, combined with the known higher rates of CKD among adults from developing countries [2], suggest that the burden of undiagnosed CKD among children in Mexico might be greater than anticipated. Further studies to confirm these estimates, as well as to document the etiology of CKD, are required.
Several recent articles have highlighted the growing burden of kidney disease in developing nations, and the International Society of Nephrology and other organizations have recently initiated programs advocating the use of low-cost therapies for prevention (rather than treatment) of kidney failure and its causes [30–32]. While this effort is extremely important, we also argue that the general message of World Kidney Day, that kidney disease is ‘common’, ‘harmful’ and ‘treatable’, should be extended to include the pediatric population in developing nations. Raising awareness about markers of kidney disease and risk factors for both hypertension and kidney disease in children may play a role in delaying or preventing chronic kidney disease or other chronic non-communicable diseases in adulthood [33–35]. In countries where there are limited resources for healthcare, these measures to prevent CKD and ESRD are critically important.
Our study had several limitations that should be considered. Although the data were collected according to a priori definitions, they were obtained from a small sample of children in a single Mexican city and, therefore, may not be generalizable to all Mexican children. The families who self-select to participate in public screening programs during World Kidney Day may not be representative of the general population, resulting in under- or over-estimation of prevalence. In this study the screening programs were preceded by a promotional campaign for chronic kidney disease awareness, and this may have enhanced the prevalence of CKD in the sample tested.
It is also important to recognize that screening urinalysis, serum creatinine assay and blood pressure (BP) measurement were performed once in study participants and that repeat testing was performed only in those with abnormalities. The specificity of all three measures is known to be increased by repeated testing. For instance, false positive diagnosis of proteinuria can be related to physical activity, position, fever, hydration status and diet [36]. In a previous community based screening study of Bolivian people drawn from the general population, only 23.9% of participants with abnormal dipstick urinalysis findings returned for follow-up, and, among these, 35% had a normal urinalysis result on recheck [4]. Recent publications from community based chronic kidney disease screening programs among indigenous and non-indigenous children in Australia suggest that urine dipsticks (MultiStix 10 SG) had a sensitivity of 62% and specificity of 97% at baseline for detecting albuminuria when compared to a reference value (urine albumin-to-creatinine ratio) [37]. In this latter study, the prevalence of baseline albuminuria and hematuria was 7.3% and 5.5%, respectively, among those children screened in Australia, but it declined to 1.5% and 1.1%, respectively, after 2 years of follow-up. Similarly, prevalence of systolic hypertension decreased from 7.2% at the initial screen to 1.1% in the follow-up examination at 2 years. In total, only 20% of children whose screen had produced positive findings at baseline had persistent markers of CKD at follow-up. Therefore, the use of a single urinalysis in our study may have led to over-estimation of the prevalence of urinary abnormalities.
The Schwartz equation, used to estimate GFR in this study, tends to over-estimate GFR as much as 20% due to differences in calibration among clinical laboratories, and it is known to be imprecise, especially among children who are malnourished or obese [38]. Nevertheless, the Schwartz equation is one of the most well-accepted methods to calculate estimated GFR in children [17, 39]. Finally, a white-coat effect may have led to an over-estimate of the prevalence of hypertension among younger participants in our study. Although the use of ambulatory blood pressure monitoring would have avoided this limitation, this was not feasible due to resource limitations.
In summary, proteinuria, hematuria and hypertension were frequently detected among children in a voluntary community based screening program carried out in Jalisco, Mexico, on World Kidney Day. Follow-up studies also found persistent urinary abnormalities in a significant proportion of children. These findings suggest that screening on WKD may be useful in identifying children with CKD and hypertension in Mexico and, perhaps, in other developing nations.
References
Levey AS, Andreoli SP, DuBose T, Provenzano R, Collins AJ (2007) Chronic kidney disease: common, harmful and treatable-World Kidney Day 2007. Pediatr Nephrol 22:321–325
Jafar TH (2006) The growing burden of chronic kidney disease in Pakistan. N Engl J Med 354:995–997
Mani MK (2005) Experience with a program for prevention of chronic renal failure in India. Kidney Int 67:S75–S78
Plata R, Silva C, Yahuita J, Perez L, Schieppati A, Remuzzi G (1998) The first clinical and epidemiological programme on renal disease in Bolivia: a model for prevention and early diagnosis of renal diseases in the developing countries. Nephrol Dial Transplant 13:3034–3036
Amato D, Alvarez-Aguilar C, Castaneda-Limones R, Rodriguez E, Avila-Diaz M, Arreola F, Gomez A, Ballesteros H, Becerril R, Paniagua R (2005) Prevalence of chronic kidney disease in an urban Mexican population. Kidney Int 68:S11–S17
Rosas M, Attie F, Pastelin G, Lara A, Velazquez O, Tapia-Conyer R, Martinez-Reding J, Mendez A, Lorenzo-Negrete A, Herrera-Acosta J (2005) Prevalance of proteinuria in Mexico: a conjunctive consolidation approach with other cardiovascular risk factors: the Mexican Health Survey 2000. Kidney Int 68:S112–S119
Lawlor DA, Smith GD (2005) Early life determinants of adult blood pressure. Curr Opin Nephrol Hypertens 14:259–264
Cutler JA, Roccella EJ (2006) Salt reduction for preventing hypertension and cardiovascular disease: a population approach should include children. Hypertension 48:818–819
Encuesta Nacional de Salud y Nutricion (2006) Resultados por Entidad Federativa, Jalisco Instituto Nacional de Salud Publica Cuernavaca, Morelos, Mexico.
Instituto Nacional de Geografia y Estadistica. Jalisco. Informacion Estadistica. Defunciones generales por principales causas de defuncion. Available at: https://doi.org/www.inegi.gob.mx. Accessed 17 December 2007
Consejo Nacional de Poblacion (CONAPO). Indicadores Demograficos Basicos, Jalisco Available at: https://doi.org/www.conapo.gob.mx. Accessed 20 August 2008
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114:555–576
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ (2003) The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 289:2560–2572
Schwartz GJ, Haycock GB, Edelmann CM Jr, Spitzer A (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58:259–263
Schwartz GJ, Gauthier B (1985) A simple estimate of glomerular filtration rate in adolescent boys. J Pediatr 106:522–526
Schwartz GJ, Feld LG, Langford DJ (1984) A simple estimate of glomerular filtration rate in full-term infants during the first year of life. J Pediatr 104:849–854
Hogg RJ, Furth S, Lemley KV, Portman R, Schwartz GJ, Coresh J, Balk E, Lau J, Levin A, Kausz AT, Eknoyan G, Levey AS (2003) National Kidney Foundation′s Kidney Disease Outcomes Quality Initiative clinical practice guidelines for chronic kidney disease in children and adolescents: evaluation, classification, and stratification. Pediatrics 111:1416–1421
Rembold CM (1998) Number needed to screen: development of a statistic for disease screening. BMJ 317:307–312
Centers for Disease Control and Prevention. Available at: https://doi.org/www.cdc.gov/growthcharts. Accessed 13 June 2008
Himes JH, Dietz WH (1994) Guidelines for overweight in adolescent preventive services: recommendations from an expert committee. The Expert Committee on Clinical Guidelines for Overweight in Adolescent Preventive Services. Am J Clin Nutr 59:307–316
Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ (2004) Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics 113:475–482
Stergiou GS, Yiannes NJ, Rarra VC, Alamara CV (2005) White-coat hypertension and masked hypertension in children. Blood Press Monit 10:297–300
Pall D, Katona E, Fulesdi B, Zrinyi M, Zatik J, Bereczki D, Polgar P, Kakuk G (2003) Blood pressure distribution in a Hungarian adolescent population: comparison with normal values in the USA. J Hypertens 21:41–47
Genovesi S, Giussani M, Pieruzzi F, Vigorita F, Arcovio C, Cavuto S, Stella A (2005) Results of blood pressure screening in a population of school-aged children in the province of Milan: role of overweight. J Hypertens 23:493–497
Jago R, Harrell JS, McMurray RG, Edelstein S, El Ghormli L, Bassin S (2006) Prevalence of abnormal lipid and blood pressure values among an ethnically diverse population of eighth-grade adolescents and screening implications. Pediatrics 117:2065–2073
Sorof JM, Portman RJ (2000) White coat hypertension in children with elevated casual blood pressure. J Pediatr 137:493–497
Ogden CL, Flegal KM, Carroll MD, Johnson CL (2002) Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA 288:1728–1732
Francischetti EA, Genelhu VA (2007) Obesity-hypertension: an ongoing pandemic. Int J Clin Pract 61:269–280
Ardissino G, Dacco V, Testa S, Bonaudo R, Claris-Appiani A, Taioli E, Marra G, Edefonti A, Sereni F (2003) Epidemiology of chronic renal failure in children: data from the ItalKid project. Pediatrics 111:e382–e387
Dirks JH, Robinson SW, Alderman M, Couser WG, Grundy SM, Smith SC, Remuzzi G, Unwin N (2006) Meeting report on the Bellagio conference ‘prevention of vascular diseases in the emerging world: an approach to global health equity’. Kidney Int 70:1397–1402
Dirks JH, de Zeeuw D, Agarwal SK, Atkins RC, Correa-Rotter R, D′Amico G, Bennett PH, El Nahas M, Valdes RH, Kaseje D, Katz IJ, Naicker S, Rodriguez-Iturbe B, Schieppati A, Shaheen F, Sitthi-Amorn C, Solez K, Viberti G, Remuzzi G, Weening JJ (2005) Prevention of chronic kidney and vascular disease: toward global health equity—the Bellagio 2004 declaration. Kidney Int 68:S1–S6
Mani MK (2006) Nephrologists sans frontieres: preventing chronic kidney disease on a shoestring. Kidney Int 70:821–823
Geleijnse JM, Hofman A, Witteman JC, Hazebroek AA, Valkenburg HA, Grobbee DE (1997) Long-term effects of neonatal sodium restriction on blood pressure. Hypertension 29:913–917
Brenner BM, Mackenzie HS (1997) Nephron mass as a risk factor for progression of renal disease. Kidney Int Suppl 63:S124–S127
Srinivasan SR, Myers L, Berenson GS (2006) Changes in metabolic syndrome variables since childhood in prehypertensive and hypertensive subjects: the Bogalusa Heart Study. Hypertension 48:33–39
Pugia MJ, Lott JA, Kajima J, Saambe T, Sasaki M, Kuromoto K, Nakamura R, Fusegawa H, Ohta Y (1999) Screening school children for albuminuria, proteinuria and occult blood with dipsticks. Clin Chem Lab Med 37:149–157
Haysom L, Williams R, Hodson E, Lopez-Vargas P, Roy LP, Lyle D, Craig JC (2009) Diagnostic accuracy of urine dipsticks for detecting albuminuria in indigenous and non-indigenous children in a community setting. Pediatr Nephrol 24:323–331
Haycock GB (1989) Creatinine, body size and renal function. Pediatr Nephrol 3:22–24
Zappitelli M, Joseph L, Gupta IR, Bell L, Paradis G (2007) Validation of child serum creatinine-based prediction equations for glomerular filtration rate. Pediatr Nephrol 22:272–281
Acknowledgments
Drs. Tonelli and Hemmelgarn are supported by Population Health Investigator Awards from the Alberta Heritage Foundation for Medical Research (AHFMR) and by New Investigator Awards from the Canadian Institutes of Health Research. Dr. Koshy is supported by a Clinical Fellowship award from AHFMR. This study was funded by a grant from the Foundation of the Hospitales Civiles de Guadalajara. The sponsor did not participate in analyses or influence the decision to submit this article for publication. The authors have no relevant competing financial interests to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koshy, S.M., Garcia-Garcia, G., Pamplona, J.S. et al. Screening for kidney disease in children on World Kidney Day in Jalisco, Mexico. Pediatr Nephrol 24, 1219–1225 (2009). https://doi.org/10.1007/s00467-009-1136-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-009-1136-7