Abstract
Objectives: To describe the new generation of palate surgery based on the systematic review. Methods: Searches to identify publications relevant to OSA treatment and upper airway palate surgery, published between January 2001 and February 2018 were included. All adult OSA patients, with documented airway evaluation methods and absent hypopharyngeal collapse. Post-operative outcomes measures included success rates of treatment, AHI, Epworth scale, QOL, and snoring VAS. Results: A total of 2715 patients who had palate surgery were identified in 59 papers; UPPP accounted for 16.7% of all the procedures. The percentage of UPPP procedures were 25.67%, from 2011 to 2018, there were only 12.6% of UPPP procedures. The average follow-up was 8.18 months. Meta-analysis on the AHI change for all procedures showed the fixed effect AHI per follow-up (FU) month change was 1.45 (95% CI 1.33, 1.8), p < 0.001, while for ESS, the fixed effect AHI per FU month change was 0.61 (95% CI 0.56, 0.66), p < 0.001. The overall mean decrease in AHI was from 35.66 to 13.91 (p < 0.001) and the overall mean decrease in ESS was from 11.65 to 5.08 (p < 0.001). The mean AHI change was 19.9 (p < 0.001). The mean ESS change was 5.8 (p < 0.001). The overall pooled success rate was 67.5%. Meta-analysis of the procedures showed that the respective mean AHI reduction was 24.7 for the anterior palatoplasty (p = 0.015), 19.8 for the lateral/expansion pharyngoplasty (p = 0.046), and 17.2 for the uvulopalatopharyngoplasty (p = 0.360). Conclusions: Upper airway surgery has evolved to more reconstructive surgery. With more enhanced objective airway evaluation diagnostic techniques, the success rates of palate surgery have improved as well.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
2.1 Introduction
Obstructive sleep apnea (OSA) is categorized under the sleep disordered breathing continuum ranging from simple snoring to OSA. OSA due to upper airway collapse arising from pharyngeal and tongue muscle relaxation during sleep results in hypoxemia with increased sympathetic overdrive, increased blood pressure, and hypercapnia. The stoppages in breathing would result in arousals from sleep and sleep disruptions causing sleep fragmentation leading to excessive daytime sleepiness, tiredness, lethargy, morning headaches, poor concentration, fatigue, poor memory, and irritability.
Most sleep specialists have shown a strong correlation between OSA and hypertension, atherosclerosis, and cerebrovascular accidents (strokes) [1]. Studies have also shown a higher mortality rate among patients with cardiovascular disease who also have OSA [1]. Therefore, it would be reasonable to say that early and effective treatment of OSA is of great essence.
Treatment of OSA can range from nasal continuous positive airway pressure (CPAP) as the “gold” standard, to oral appliances, to upper airway surgery. Upper airway surgery has evolved and improved significantly over the past 10–20 years [2,3,4,5,6,7,8,9,10,11,12]; however, the concept of surgical success has not changed much during this period (50% reduction and/or AHI apnea-hypopnea index (AHI) <20) [13].
In the 1960s, Quesada and Perello [14] introduced the more ablative technique of treating snoring by the removal of the uvula and soft palatal soft tissue. Forty years on, new palatal techniques have been introduced; in the early 2000s, Michel Cahali [15] introduced the lateral pharyngoplasty which had promising results, while Pang and Woodson introduced the expansion sphincter pharyngoplasty [16], which showed far better outcomes for patients with lateral pharyngeal wall collapse.
The basic fundamentals of the new generation of palate surgeries are:
-
(a)
to address the exact anatomical site of collapse,
-
(b)
preserving the mucosa and soft tissues,
-
(c)
while respecting muscle and anatomical function of each structure.
Coupled with these newer palatoplasty techniques, one must not forget the introduction of more comprehensive methods for airway evaluation. Drug induced sleep endoscopy (DISE) has changed the reality of what the airway is when asleep versus when awake. Studies have shown that the treatment plans of patients with and without DISE performed are markedly changed in over 60–70% of patients [17,18,19,20] (whether they had DISE performed before their surgery).
The authors discuss the systematic review of the medical literature and meta-analysis of papers on upper airway palate surgery for OSA between the years January 2001 and February 2018 and review the success rates of palate surgery over the past 17 years.
2.2 Methodology
A comprehensive systematic literature review using searches of MEDLINE, Google Scholar, Cochrane Library, PubMed, and Evidence Based Medicine Reviews to identify publications relevant to OSA treatment and upper airway palate surgery with its variants. All relevant studies published between January 2001 and December 2017 were included.
The authors looked at surgical outcomes and results, with the inclusion criteria being:
-
1.
Patients: adults, more than 18 years of age, with AHI > 5.
-
2.
Comparison: quantitative data pre- and post-palate surgery.
-
3.
Outcomes: including either success rates of treatment, pre-operative and post-operative AHI, Epworth sleepiness scale (ESS), quality of life (QOL), and/or snoring visual analog scale (VAS).
-
4.
Study design: published, peer-reviewed studies with at least a 3 month follow-up period post-surgery.
-
5.
Intervention: palatal surgery involving either the soft and/or hard palate, lateral pharyngeal wall, palatopharyngeus, with or without tonsil surgery and/or uvular procedure. The authors excluded (a) procedures performed in addition to palate surgery (i.e. tongue surgery, skeletal surgery), (b) LAUP, (c) studies with qualitative outcomes only, (d) patients who had previous upper airway surgery, and (e) patients who have central sleep apnea.
The following combined search terms were used on PubMed and MedLine (using both British and American spellings): “upper airway surgery and sleep apnea/obstructive sleep apnea,” “palate surgery and sleep apnea/obstructive sleep apnea,” “airway modifications and sleep apnea/obstructive sleep apnea,” “pharyngoplasty and sleep apnea/obstructive sleep apnea,” “palatoplasty and sleep apnea/obstructive sleep apnea,” “tonsil surgery and sleep apnea/obstructive sleep apnea,” “systematic review and sleep apnea/obstructive sleep apnea,” and “meta-analysis and sleep apnea/obstructive sleep apnea.”
A total final number of 59 articles were identified and included. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement and checklist were followed as much as possible during this review.
The authors analyzed the pooled results (pre-operative and post-operative) of all palate procedures performed on the entire group of OSA patients. The authors also looked at the results (pre-operative and post-operative) of the three main categories of palate procedures (namely lateral/expansion palatal procedures, anterior palatal procedures, and the classic uvulopalatopharygoplasty).
2.3 Statistical Method
Meta-analysis was conducted using the Cochrane Review Manager (version 5.3), (The Nordic Cochrane Centre, The Cochrane Collaboration). Random effect models are used to generate pooled estimates. Data was analyzed using generic inverse radiance method and p < 0.05 is regarded as statistically significant. Combined summary statistics of the standardized (STD) paired difference in mean for the individual studies are shown. Combined STD paired differences in means were calculated and a 2-sided p-value <0.05 was considered to indicate statistical significance. An χ2-based test of homogeneity was performed and the inconsistency index (I2) statistic was determined. If I2 was >50% or >75%, the studies were considered to be heterogeneous or highly heterogeneous, respectively. If I2 was below 25%, the studies were considered to be homogeneous. If the I2 statistic (>50%) indicated that heterogeneity existed between studies, a random effects model was calculated. For the second part, due to the high heterogeneity in each subgroup (I2 = 91.4% p < 0.001, I2 = 89.8% p < 0.001, and I2 = 95.0% p < 0.001, respectively), a random effects analysis was performed using the DerSimonian and Laird method. In order to check the differences in the reduction on AHI between each surgical technic, Z-scores have been computed. A p-value <0.05 has been considered statistically significant. The entire meta-analysis was carried out using “Stata IC 12.1.”
2.4 Results
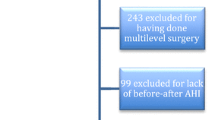
The PubMed/Medline database search revealed 2103 papers, 945 papers were not relevant, a further 802 did not meet the inclusion criteria; 243 papers were on multi-level upper airway surgery, 99 papers were subsequently excluded for they did not document pre- and post-surgery AHI, finally, 14 papers were not included as they lacked documentation of follow-up duration, leaving 59 papers [15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73] that met the inclusion criteria.
There were a total of 59 scientific papers included for analysis. All these papers met the inclusion criteria and reported their results in a clear and concise way. A total of 2694 patients underwent a varied number of palatal surgery types that included the traditional uvulopalatopharyngoplasty (UPPP), Han modified UPPP, uvulo-palatal flap (UPF), extended UPF (EUPF), modified extended UPF (MEUP), Z-palatoplasty (ZPPP), lateral pharyngoplasty (LP), relocation pharyngoplasty (RP), expansion sphincter pharyngoplasty (ESP), anterior palatoplasty (AP), functional expansion sphincter pharyngoplasty (FESP), limited palatal muscle resection (LPMR), barbed anterior palatoplasty (BAP), partial palate resection (PPR), soft palatal webbing flap palatopharyngoplasty (SPWF), barbed Roman blinds technique (BRBT), barbed repositioning pharyngoplasty (BRP), anterolateral advancement pharyngoplasty (AAP), and the barbed expansion sphincter pharyngoplasty (BESP) (Table 2.1).
The authors showed that many sleep specialists/surgeons have moved away from the traditional UPPP and/or its modified variants. Ever since the introduction of the Cahali [15] LP in 2003 and the Pang et al. [16] ESP in 2007, most surgeons have adopted and utilized the newer innovative techniques to address the lateral pharyngeal wall collapse and anterior–posterior soft palatal narrowing.
Over the past 18 years (January 2001 to February 2018), the authors described that (in these 59 papers) the uvulopalatopharyngoplasty technique only accounted for 16.7% of all the 2715 pooled patient procedures performed.
Interestingly, from January 2001 to December 2010, the percentage of UPPP procedures were 25.6% (264 out of 1034), and from January 2011 to February 2018, the percentage of UPPP procedures were only 12.6% (213 out of 1681).
From the 59 papers analyzed, there were 2715 patients who had upper airway surgery and met the criteria. The average follow-up was 8.18 months (range 6 to 54 months). The mean decrease in AHI (pre- to post-procedure) was from 35.66 to 13.91 (p < 0.001). The mean decrease in ESS (pre- to post-procedure) was from 11.65 to 5.08 (p < 0.001). The mean AHI change was 19.9 (SD 8.32, range of 4.9 to 36.9) (p < 0.001). The mean ESS change was 5.8 (SD 2.2, range of 2 to 10) (p < 0.001). The overall pooled success rate was 67.5% (the range of success rates was from 25% to 94.1%).
After having divided the procedures into the three main categories, the meta-analysis of the respective palate procedure showed that the surgical technique that achieved the better reduction on AHI was the anterior palatoplasty, with a mean reduction of 24.7 (range 20.79–28.6) (p = 0.015), while the mean reduction of AHI for the lateral/expansion pharyngoplasty procedures was 19.8 (range 16.90–22.64) (p = 0.046), and the mean reduction of AHI for the classical uvulopalatopharyngoplasty was 17.2 (range 12.68–21.83) (p = 0.360).
2.5 Discussion
Since the late 1960s, the understanding and management of OSA have evolved and deepened. Sleep specialists widely accept that upper airway surgery can have good success rates for selected OSA patients who have favorable anatomical surgical structure. Most agree that the key to surgical success is patient selection, hence, clearer visualization of the airway during drug induced sleep endoscopy (DISE) [74,75,76,77,78,79,80,81] has enhanced the surgeon’s ability to select the appropriate procedure for the appropriate patient.
Since the beginning of the early 2000s, DISE has enabled sleep surgeons to visually locate the exact anatomical site that collapses during the patient’s sleep, hence, addressing that particular anatomical site. In addition, since 2003, the introduction of the LP [15, 18] and the ESP [16, 57, 82] in 2007, these 2 newer techniques have revolutionized the concept of sleep apnea surgery from ablative surgery to one that involves reconstruction while preserving the function of the uvula and sparing more mucosa.
Over the past 40 years, there has been an improvement in the success rates of palate surgery from 40.7% [8, 9], to 55% [83] to this current meta-analysis at 69.6%, in comparison to a systemic review by Rotenberg and Pang et al. [84], who reviewed 82 papers over a 20-year (1994–2015) CPAP treatment period, and demonstrated that the non-adherence rate of CPAP therapy remained high at 34% (plateau) throughout these 20 years. Despite improvements in the CPAP technology, dynamic breath-to-breath pressure titration, and including the use of Bi-level therapy, CPAP compliance has been at a dismal low level.
The authors demonstrate a clear shift of the sleep surgeons’ preference towards more innovative anatomically targeted surgical procedures, instead of the old traditional non-selective UPPP. It demonstrates a change in philosophy in the thought process of sleep surgeons and that sleep surgeons are aware that sleep apnea surgery is reconstructive and not ablative surgery. The steady decrease of the UPPP technique, 2001–2010, from 25.6% (264 out of 1034) to 12.6% (213 out of 1681) in the following next 8 years, 2011–2018, is indicative of the paradigm shift.
There was a significant reduction in both AHI and ESS, the mean decrease in AHI (pre- to post-procedure) was from 35.66 to 13.91 (p < 0.001), while the mean decrease in ESS (pre- to post-procedure) was from 11.65 to 5.08 (p < 0.001).
The mean AHI change was 22.7 (SD 8.32, range of 4.9 to 36.9) (p < 0.001), with mean ESS change 5.8 (SD 2.2, range of 2 to 10) (p < 0.001) and mean success rate of 67.5%.
The meta-analysis of the respective palate procedures demonstrated that the surgical procedure that achieved the best AHI reduction was the anterior palatoplasty, with a mean reduction of 24.7 (range 20.79–28.6) (p = 0.015), followed by the lateral/expansion pharyngoplasty procedures at a reduction of 19.8 (range 16.90–22.64) (p = 0.046), and the least reduction was the classical UPPP, at 17.2 (range 12.68–21.83) (p = 0.360).
The authors acknowledge that there are some short-comings with the analysis, (a) although the data presented may be statistically significant, it may not be clinically significant, (b) the patients selected for anterior palatoplasty might have a less difficult anatomy, compared to those in whom a lateral/expansion procedure was done, (c) all these 59 articles are fairly heterogeneous, each article differs in their methodology, (d) these different articles report their data and results differently, (e) different authors have different surgical techniques to address the palate, (f) different nomenclature of palatal procedures will inevitably have some overlap in surgical steps, and, as with most medical literature, there is always a reporter bias (i.e. authors tend to and are more willing to report and publish good results).
The objective of this paper is not to illustrate nor demonstrate the different surgical techniques in the treatment of OSA, but rather to highlight the importance that (1) the efficacy of upper airway surgery has been steadily improving with better airway evaluation techniques, (2) there are innovative, logical yet simple surgical techniques that address the relevant anatomical site of obstruction, that work, and (3) sleep specialists need to continue to attend sleep courses to upgrade themselves and learn new diagnostic and therapeutic methods, in order for their patients to benefit with better success rates.
2.6 Conclusion
The authors highlight that (1) the surgical success rates of upper airway surgery has been steadily improving with the introduction of better airway evaluation techniques, (2) newer innovative surgical techniques can address the relevant anatomical site of obstruction, that work, and (3) there is an obvious shift towards the new generation of palate surgeries and away from the traditional ablative UPPP technique.
References
Giles TL, Lasserson TJ, Smith B, White J, Wright JJ, Cates CJ. Continuous positive airways pressure for obstructive sleep apnoea in adults: a cochrane collaboration review. New York: Wiley; 2008. p. 1–103. Ref Type: Report.
Friedman M. Sleep and snoring surgical and non-surgical therapy. New York: Elsevier; 2009.
Hormann K, Verse TM. Surgery for sleep disordered breathing. 2nd ed. Berlin: Springer-Verlag; 2010.
Pang KP, Rotenberg BW, Woodson BT. Advanced surgical techniques in snoring and obstructive sleep apnea. San Diego: Plural Publishing; 2013.
O’Connor C, García-Iriarte M, Casado JC, Plaza G, Gómez-Ángel D. Evolution of palate surgery for the treatment of snoring and obstructive sleep apnea-hypopnea syndrome (OSAHS): Pharyngoplasties En. In: Plaza G, Baptista P, O’Connor C, editors. Sleep-disordered breathing: diagnosis and treatment. Barcelona: INDICA; 2017. p. 265–319. ISBN: 978–84–607-8314-4.
Lugo SR. Surgical management in snoring and sleep-disordered breathing. New Delhi: Jaypee; 2017. ISBN: 0009351528898.
Yaremchuk K. Palatal procedures for obstructive sleep apnea. Otolaryngol Clin North Am. 2016;49:1383–97.
Li HY. Updated palate surgery for obstructive sleep apnea. Adv Otorhinolaryngol. 2017;80:74–80.
Caples SM, Rowley JA, Prinsell JR, et al. Surgical modifications of the upper airway for obstructive sleep apnea in adults: a systematic review and meta-analysis. Sleep. 2010;33:1396–407.
Braga A, Carboni LH, do Lago T, et al. Is uvulopalatopharyngoplasty still an option for the treatment of obstructive sleep apnea? Eur Arch Otorhinolaryngol. 2013;270:549–54.
Choi JH, Cho SH, Kim SN, et al. Predicting outcomes after uvulopalatopharyngoplasty for adult obstructive sleep apnea: a meta-analysis. Otolaryngol Head Neck Surg. 2016;155:904–13.
Verse T, Stuck BA. Moderne Modifikationen der Uvulopalatopharyngoplastik. HNO. 2017;65:90–8.
Sher AE, Schechtman KB, Piccirillo JF. The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep. 1996;19:156–77.
Quesada P, Pedro-Botet J, Fuentes E, Perelló E. Resección parcial del paladar blando como tratamiento del síndrome de hipersomia y respiración periódica de los obesos. Acta Otorrinolaringol Esp. 1979;30:119–24.
Cahali MB. Lateral pharyngoplasty: a new treatment for obstructive sleep apnea hypopnea syndrome. Laryngoscope. 2003;113:1961–8.
Pang KP, Woodson BT. Expansion sphincter pharyngoplasty, a new technique for the treatment of obstructive sleep apnea. Otolaryngol Head Neck Surg. 2007;137:110–4.
Li H, Li K, Chen N, et al. Modified Uvulopalatopharyngoplasty: the extended Uvulopalatal flap. Am J Otolaryngol. 2003;24:311–6.
Cahali MB, Formigoni GG, Gebrim EM, Miziara ID. Lateral pharyngoplasty versus uvulopalatopharyngoplasty: a clinical, polysomnographic and computed tomography measurement comparison. Sleep. 2004;27:942–50.
Friedman M, Ibrahim H, Vidyasagar R, et al. Z-palatoplasty (ZPP): a technique for patients without tonsils. Otolaryngol Head Neck Surg. 2004;131:89–100.
Li HY, Chen NH, Lee LA, et al. Use of morphological indicators to predict outcomes of palatopharyngeal surgery in patients with obstructive sleep apnea. ORL J Otorhinolaryngol Relat Spec. 2004;66:119–23.
Li HY, Chen NH, Shu YH, Wang PC. Changes in quality of life and respiratory disturbance after extended uvulopalatal flap surgery in patients with obstructive sleep apnea. Arch Otolaryngol Head Neck Surg. 2004;130:195–200.
Li HY, Huang YS, Chen NH, et al. Mood improvement after surgery for obstructive sleep apnea. Laryngoscope. 2004;114:1098–102.
Han DM, Ye JY, Lin ZH, et al. Revised uvulopalatopharyngoplasty with uvula preservation and its clinical study. ORL J Otorhinolaryngol Relat Spec. 2005;67:213–9.
Li HY, Wang PC, Hsu CY, et al. Combined nasal-palatopharyngeal surgery for obstructive sleep apnea: simultaneous or staged? Acta Otolaryngol. 2005;125:298–303.
Hofmann T, Schwantzer G, Reckenzaun E, et al. Radiofrequency tissue volume reduction of the soft palate and UPPP in the treatment of snoring. Eur Arch Otorhinolaryngol. 2006;263:164–70.
Li HY, Wang PC, Lee LA, et al. Prediction of uvulopalatopharyngoplasty outcome: anatomy-based staging system versus severity-based staging system. Sleep. 2006;29:1537–41.
Lin SW, Chen NH, Li HY, et al. A comparison of the long-term outcome and effects of surgery or continuous positive airway pressure on patients with obstructive sleep apnea syndrome. Laryngoscope. 2006;116:1012–6.
Huang TW, Cheng PW. Microdebrider-assisted extended uvulopalatoplasty: an effective and safe technique for selected patients with obstructive sleep apnea syndrome. Arch Otolaryngol Head Neck Surg. 2008;134:141–5.
Li HY, Lee LA. Relocation pharyngoplasty for obstructive sleep apnea. Laryngoscope. 2009;119:2472–7.
Lundkvist K, Januszkiewicz A, Friberg D. Uvulopalatopharyngoplasty in 158 OSAS patients failing non-surgical treatment. Acta Oto-Laryngological. 2009;129:1280–6.
Pang KP, Tan R, Puraviappan P, Terris DJ. Anterior palatoplasty for the treatment of OSA: three-year results. Otolaryngol Head Neck Surg. 2009;141:253–6.
Lee LA, Huang CG, Chen NH, et al. Severity of obstructive sleep apnea syndrome and high-sensitivity C-reactive protein reduced after relocation pharyngoplasty. Otolaryngol Head Neck Surg. 2010;144:632–8.
Neruntarat C. Uvulopalatal flap for obstructive sleep apnea: short-term and long-term results. Laryngoscope. 2011;121:683–7.
Mantovani M, Minetti A, Torretta S, et al. The velo-uvulo-pharyngeal lift or “roman blinds” technique for treatment of snoring: a preliminary report. Acta Otorhinolaryngol Ital. 2012;32:48–53.
Choi JH, Jun YJ, Kim TH, et al. Effect of isolated uvulopalatopharyngoplasty on subjective obstructive sleep apnea symptoms. Clin Exp Otorhinolaryngol. 2013;6:161–5.
Li HY, Cheng WN, Chuang LP, et al. Positional dependency and surgical success of relocation pharyngoplasty among patients with severe obstructive sleep apnea. Otolaryngol Head Neck Surg. 2013;149:506–12.
Browaldh N, Nerfeldt P, Lysdahl M, et al. SKUP3 randomised controlled trial: polysomnographic results after uvulopalatopharyngoplasty in selected patients with obstructive sleep apnoea. Thorax. 2013;68:846–53.
Kim MJ, Kim BY, Lee DC, et al. A modified uvulopalatal flap with lateral pharyngoplasty for treatment in 92 adults with obstructive sleep apnoea syndrome. Clin Otolaryngol. 2013;38:381–442.
Liu SR, Yi HL, Yin SK, et al. Associated predictors of therapeutic response to uvulopharyngopalatoplasty for severe obstructive sleep apnea hypopnea syndrome. Eur Arch Otorhinolaryngol. 2013;270:1411–7.
Marzetti A, Tedaldi M, Passali FM. Preliminary findings from our experience in anterior palatoplasty for the treatment of obstructive sleep apnea. Clin Exp Otorhinolaryngol. 2013;6:18–22.
Sorrenti G, Piccin O. Functional expansion pharyngoplasty in the treatment of obstructive sleep apnea. Laryngoscope. 2013;123:2905–8.
Yousuf A, Beigh Z, Khursheed RS, et al. Clinical predictors for successful uvulopalatopharyngoplasty in the management of obstructive sleep apnea. Int J Otolaryngol. 2013;2013:290265.
Sep Cho KS, Koo SK, Lee JK, et al. Limited palatal muscle resection with tonsillectomy: a novel palatopharyngoplasty technique for obstructive sleep apnea. Auris Nasus Larynx. 2014;41:558–62.
de Paula Soares CF, Cavichio L, Cahali MB. Lateral pharyngoplasty reduces nocturnal blood pressure in patients with obstructive sleep apnea. Laryngoscope. 2014;124:311–6.
Salamanca F, Costantini F, Mantovani M, et al. Barbed anterior pharyngoplasty: an evolution of anterior palatoplasty. Acta Otorhinolaryngol Ital. 2014;34:434–8.
Li HY, Lee LA, Yu JF, et al. Changes of snoring sound after relocation pharyngoplasty for obstructive sleep apnoea: the surgery reduces mean intensity in snoring which correlates well with apnoea-hypopnoea index. Clin Otolaryngol. 2014;40:98–105.
Ugur KS, Ark N, Kurtaran H, et al. Anterior palatoplasty for selected mild and moderate obstructive sleep apnea: preliminary results. Eur Arch Otorhinolaryngol. 2014;271:1777–83.
Chen HC, Lee LA, Hsin LJ, et al. Transverse retropalatal collapsibility is associated with obstructive sleep apnea severity and outcome of relocation pharyngoplasty. Otolaryngol Head Neck Surg. 2015;153:1056–63.
Chi JC, Chiang RP, Chou TY, et al. The role of lateral pharyngoplasty in obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol. 2015;272:489–96.
Carrasco-Llatas M, Marcano-Acuña M, Zerpa-Zerpa V, Dalmau-Galofre J. Surgical results of different palate techniques to treat oropharyngeal collapse. Eur Arch Otorhinolaryngol. 2015;272:2535–40.
Dizdar D, Civelek ÇZA, et al. Comparative analysis of lateral pharyngoplasty and uvulopalatopharyngoplasty techniques with polysomnography and Epworth sleepiness scales. J Craniofac Surg. 2015;26:e647–51.
Elbassiouny AMME. Soft palatal webbing flap palatopharyngoplasty for both soft palatal and oropharyngeal lateral wall collapse in the treatment of snoring and obstructive sleep apnea: a new innovative technique without tonsillectomy. Sleep Breath. 2015;19:481–7.
Li HY, Lee LA, Kezirian EJ. Efficacy of Coblation endoscopic lingual lightening in multilevel surgery for obstructive sleep apnea. JAMA Otolaryngol Head Neck Surg. 2016;142:438–43.
Mantovani M, Rinaldi V, Torretta S, et al. Barbed Roman blinds technique for the treatment of obstructive sleep apnea: how we do it? Eur Arch Otorhinolaryngol. 2015;273:517–23.
Vicini C, Hendawy E, Campanini A, et al. Barbed reposition pharyngoplasty (BRP) for OSAHS: a feasibility, safety, efficacy and teachability pilot study. “We are on the giant’s shoulders”. Eur Arch Otorhinolaryngol. 2015;272:3065–70.
Emara TA, Hassan MH, Mohamad AS, et al. Anterolateral advancement pharyngoplasty: a new technique for treatment of obstructive sleep apnea. Otolaryngol Head Neck Surg. 2016;155:702–7.
Pang KP, Piccin O, Pang EB, et al. Combined expansion pharyngoplasty and anterior palatoplasty for the treatment of OSA. Indian J Otolaryngol Head Neck Surg. 2016;64:528–33.
Sommer JU, Heiser C, Gahleitner C, et al. Tonsillectomy with uvulopalatopharyngoplasty in obstructive sleep apnea-a two-center randomized controlled trial. Dtsch Arztebl Int. 2016;113:1–8.
Wu H, Yin Y, Ma H, et al. Outcome comparison of two methods of pharyngeal cavity reconstruction in uvulopalatopharyngoplasty. Acta Otolaryngol. 2016;136:847–51.
Adzreil B, EHC W, Saraiza AB, Raman R, Amin J. The effectiveness of combined tonsillectomy and anterior palatoplasty in the treatment of snoring and obstructive sleep apnoea (OSA). Eur Arch Otorhinolaryngol. 2017;274:2005–11.
Amali A, Motiee-Langroudi M, Saedi B, et al. A comparison of uvulopalatopharyngoplasty and modified radiofrequency tissue ablation in mild to moderate obstructive sleep apnea: a randomized clinical trial. J Clin Sleep Med. 2017;13:1089–96.
Askar SM, El-Anwar MW. Double suspension sutures: a simple surgical technique for selected cases of obstructive sleep apnoea: our experience with twenty-two patients. Clin Otolaryngol. 2018;43:753–7. https://doi.org/10.1111/coa.13056.
Atan D, Ozcan KM, Ozcan M, Dere H. The effect of anterior palatoplasty plus modified expansion sphincter pharyngoplasty on voice performance in obstructive sleep apnea syndrome. J Craniofac Surg. 2017;28:e464–7.
Binar M, Akcam T, Karakoc O, et al. A new surgical technique versus an old marker: can expansion sphincter pharyngoplasty reduce C-reactive protein levels in patients with obstructive sleep apnea? Eur Arch Otorhinolaryngol. 2017;274:829–36.
Cammaroto G, Montevecchi F, D'Agostino G, et al. Palatal surgery in a transoral robotic setting (TORS): preliminary results of a retrospective comparison between uvulopalatopharyngoplasty (UPPP), expansion sphincter pharyngoplasty (ESP) and barbed respositioning pharyngoplasty (BRP). Acta Otorhinolaryngol Ital. 2017;37:406–9.
Despeghel AS, Mus L, Dick C, et al. Long-term results of a modified expansion sphincter pharyngoplasty for sleep-disordered breathing. Eur Arch Otorhinolaryngol. 2017;274(3):1665–70.
El-Ahl MA, El-Anwar MW. Expansion pharyngoplasty by new simple suspension sutures without tonsillectomy. Otolaryngol Head Neck Surg. 2016;155:1065–8.
Mantovani M, Carioli D, Torretta S, et al. Barbed snore surgery for concentric collapse at the velum: the Alianza technique. J Cranio Maxillo Facial Surg. 2017;45:1794–800.
Montevecchi F, Meccariello G, Firinu E, et al. Prospective multi-centre study on barbed reposition pharyngoplasty standing alone or as a part of multilevel surgery for sleep apnea. Clin Otolaryngol. 2017;43:483–8. https://doi.org/10.1111/coa.13001.
Pianta L, Bertazzoni G, Morello R, et al. Barbed expansion sphincter pharyngoplasty for the treatment of oropharyngeal collapse in obstructive sleep apnoea syndrome: a retrospective study on 17 patients. Clin Otolaryngol. 2018;43:696–700. https://doi.org/10.1111/coa.13008.
Rashwan MS, Montevecchi F, Cammaroto G, et al. Evolution of soft palate surgery techniques for obstructive sleep apnea patients: a comparative study for single level palatal surgeries. Clin Otolaryngol. 2018;43:584–90. https://doi.org/10.1111/coa.13027.
Süslü AE, Pamuk G, Pamuk AE, et al. Effects of expansion sphincter pharyngoplasty on the apnea-hypopnea index and heart rate variability. J Oral Maxillofac Surg. 2017;75:2650–7.
Plaza G, Baptista P, O’Connor-Reina C, et al. Prospective multi-center study on expansion sphincter pharyngoplasty. Acta Otolaryngol. 2019;139(2):219–22.
Hewitt RJD, Dasgupta A, Singh A, Dutta C, Kotecha BT. Is sleep nasendoscopy a valuable adjunct to clinical examination in the evaluation of upper airway obstruction? Eur Arch Otorhinolaryngol. 2009;266:691–7.
Campanini A, Canzi P, De Vito A, et al. Awake versus sleep endoscopy: personal experience in 250 OSA patients. Acta ORL Ital. 2010;30:73–7.
Eichler C, Sommer JU, Stuck BA, Hörmann K, Maurer JT. Does drug-induced sleep endoscopy change the treatment concept of patients with snoring and obstructive sleep apnea? Sleep Breath. 2013;17:63–8.
Rabelo FAW, Kupper DS, Sander HH, et al. A comparison of Fujita classification of awake and DISE. Braz J Otorhinolaryngol. 2013;79:100–5.
Gillespie MB, Reddy RP, White DR. A trial of DISE in the surgical management of SDB. Laryngoscope. 2013;123:277–82.
Fernández-Julián E, García-Pérez MÁ, García-Callejo J, Ferrer F, Martí F, Marco J. Surgical planning after sleep versus awake techniques in patients with obstructive sleep apnea. Laryngoscope. 2014;124(8):1970–4.
Zerpa Zerpa V, Carrasco Llatas M, Agostini Porras G, Dalmau GJ. Drug-induced sedation endoscopy versus clinical exploration for the diagnosis of severe upper airway obstruction in OSAHS patients. Sleep Breath. 2015;19(4):1367–72.
Certal VF, Pratas R, Guimarares L, et al. Awake examination versus DISE for surgical decision making in OSA patients: a systematic review. Laryngoscope. 2016;126:768–74.
Camacho M, Zaghi S, Piccin O, Certal V. Expansion sphincter pharyngoplasty for obstructive sleep apnea: an update to the recent meta-analysis. Eur Arch Otorhinolaryngol. 2016;273:2857–8.
Elshaug AG, Moss JR, Southcott AM, Hiller JE. Redefining success in airway surgery for obstructive sleep apnea: a meta analysis and synthesis of the evidence. Sleep. 2007;30:461–7.
Rotenberg BW, Murariu D, Pang KP. Trends in CPAP adherence over twenty years of data collection: a flattened curve. J Otolaryngol Head Neck Surg. 2016;45:43.
Acknowledgment
There are no financial disclosures and no conflict of interest for all the above authors.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Pang, K.P., Guillermo, P., Baptista, P.M., O’Connor Reina, C., Pang, E.B., Pang, S.B. (2022). The New Generation of Palate Surgery for Obstructive Sleep Apnea. In: Vicini, C., Salamanca, F., Iannella, G. (eds) Barbed Pharyngoplasty and Sleep Disordered Breathing. Springer, Cham. https://doi.org/10.1007/978-3-030-96169-5_2
Download citation
DOI: https://doi.org/10.1007/978-3-030-96169-5_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-96168-8
Online ISBN: 978-3-030-96169-5
eBook Packages: MedicineMedicine (R0)