Abstract
The aim of this study was to determine the associated factors affecting the outcome of uvulopharyngopalatoplasty (UPPP) in patients with severe obstructive sleep apnea hypopnea syndrome (OSAHS), and to investigate whether cephalometric measurements were predictive of the therapeutic response to UPPP in patients with severe OSAHS. We retrospectively studied 51 consecutive patients who underwent revised UPPP with uvula preservation (H-UPPP), or Z-palatopharyngoplasty (ZPPP) for severe OSAHS [apnea–hypopnea index (AHI) >30]. All patients were evaluated using physical examination, Epworth Sleepiness Scale (ESS), cephalometry, and nocturnal polysomnography (PSG) before surgery and at 6–12 months after surgery. Based on the success criteria defined as an AHI of <20 and a decrease >50 %, the overall success rate was 45.1 %. The preoperative distance from the posterior border of the uvula to the middle pharyngeal wall (U-MPW) was significantly longer in the responder group than in the nonresponder group, when considering the whole group or the H-UPPP group alone. Among all study subjects, U-MPW and change in body mass index (△BMI) were the significant predictors of surgical success. U-MPW was the key predictor for H-UPPP surgical success, whereas mandibular plane angle (MPA) and Friedman stage were the key predictors for ZPPP surgical success. In conclusion, U-MPW was a significant predictor of UPPP surgical success. Patients with U-MPW >10 mm who are unwilling to receive nasal continuous positive airway pressure (CPAP) therapy might be suitable candidates for UPPP surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea hypopnea syndrome (OSAHS) is the intermittent cessation of breathing during sleep due to the collapse of the pharyngeal airway. Although nasal continuous positive airway pressure (nCPAP) is the primary treatment for OSAHS, compliance is limited, varying from 28 to 80 % [1, 2].
For decades, surgical modifications of the upper airway have been performed as a principal treatment for OSAHS [3]. Because OSAHS is incurable, the aim of surgery is to control the symptoms and minimize ongoing multisystem damage. Uvulopalatopharyngoplasty (UPPP) remains the most commonly utilized surgical procedure for treating OSAHS. Unfortunately, the success rate of this surgery is lower in unselected patients with obstructive sleep apnea (OSA, 40.8 %) [4] and in patients with Friedman OSA stages II (37.9 %) and III (8.1 %) [5]. Technical modifications of UPPP include the Z-plastypharyngoplasty [6], revised UPPP with uvula preservation (H-UPPP) [7], and palatal advancement. In a recent study, Z-palatopharyngoplasty (ZPPP) combined the Z-palatoplasty (ZPP) technique with concurrent tonsillectomy and pharyngoplasty to achieve a success rate of 64.7 % in patients who had Friedman stage II/III OSAHS [8]. However, our previous study demonstrated that although the success rate of the ZPPP group was higher than that of the H-UPPP group, these did not differ significantly between the two surgical groups [9].
Multiple techniques have been employed to predict UPPP effectiveness, but no consensus is available on whether any of these are significantly predictive of surgical success [4]. Identification of the upper airway (UA) occlusion sites inpatients with OSAHS may increase surgical success by contributing information that suggests which surgical choice is appropriate [10]. Identification of the precise UA obstruction localization sites has been attempted by a number of techniques including nasopharyngoscopy, pressure measurements, X-ray cephalometry, computed tomography (CT) scanning, and magnetic resonance imaging (MRI), and each technique has its unique advantages and disadvantages.
Over the years, cephalometric radiographic analysis has become one of the standard diagnostic tools for patients with OSAHS, particularly during the preoperative evaluation of the craniofacial skeletal anatomy before maxillomandibular advancement (MMA) surgery. However, the predictive value of X-ray cephalometry for UPPP remains questionable. Millman et al. [11] concluded that the distance from the hyoid to the mandibular plane (MP-H) <20 mm, the presence of a baseline apnea hyponea index (AHI) <38, and the absence of retrognathia were predictors of improvement after UPPP. Conversely, Doghramji et al. [12] reported that a preoperative cephalometry cannot be reliably used to predict surgical success following UPPP.
Therefore, the aims of this study were to determine the associated factors affecting the success rate of UPPP, and to investigate whether cephalometric measurements could predict the therapeutic response to UPPP in patients with severe OSAHS.
Materials and methods
Study design
Between October 2009 and March 2011, we retrospectively included 51 consecutive Chinese patients (47 men and 4 women; age range, 24–64 years; mean age, 43.0 ± 9.0 years) who underwent H-UPPP [7] or ZPPP [8]. H-UPPP was performed on Friedman stage I/IIOSA patients. ZPPP was performed on Friedman stage II/IIIOSA patients with a posterior airway space (PAS) >11 mm. Of the 51 patients, 31 were in the H-UPPP group, and 20 were in the ZPPP group. All patients experienced significant clinical symptoms of snoring and/or daytime sleepiness, were diagnosed by polysomnography (PSG) with severe OSAHS (AHI >30/h), were examined with Friedman stages I–III, and could not tolerate or were unwilling to receive lifelong nCPAP therapy. Informed written consent was obtained from all participants, and the study protocol was approved by the hospital institutional review board.
A detailed physical examination of the head and neck, such as tonsil size and Friedman palate position, was performed for each patient, and each patient was assigned a Friedman stage based on morphologic findings. The Friedman staging system was judged by the Friedman palate position, tonsil size, and body mass index (BMI) [5]. Of the 51 patients, 4 patients belonged to Friedman OSA stage I, 20 to stage II, and 27 to stage III. All patients underwent preoperative and postoperative physical examination, Epworth Sleepiness Scale (ESS) evaluation, cephalometry, and nocturnal polysomnography (PSG) before surgery and at 6–12 months after surgery.
Surgical procedure
All patients underwent H-UPPP or ZPPP under general anesthesia. The H-UPPP procedure was first described by Han et al. [7]. The characteristics of H-UPPP are as follows: bilateral tonsillectomy was performed, and the redundant bilateral pharyngeal mucosa and submucosal tissue were resected; the uvula was completely preserved; larger portion of the soft palate was resected; the adipose tissue in the space of the velum palati was removed.
The ZPPP procedure was performed as described by Yi et al. [8]. First, a tonsillectomy was performed with a cold instrument or radiofrequency ablation (Evac 70; ArthroCare, Sunnyvale, CA). Then, the ZPPP surgical technique was employed using the following key procedures [13]: two adjacent flaps were outlined on the palate, the mucosa and fat tissue of the anterior aspect of the two flaps were removed, the two flaps were separated from each other by splitting the palatal segment down the midline, and a two-layer closure bringing the midline all the way to the anterolateral margin of the palate was accomplished. Finally, a two-layer closure of the palatopharyngeal pillar and palatoglossal pillar was performed.
Polysomnography
Polysomnographic recordings were made and scored using the Alice four system (Philips Respironics, Murrysville, PA, USA). Data were recorded for the stages of sleep, oxygen saturation, and number of hypopneas and apneas per hour. Obstructive apnea was defined as the absence of airflow with respiratory effort for at least 10 s. Hypopnea was defined as a greater than 50 % reduction in airflow accompanied by oxygen desaturation of more than 4 % or arousal from sleep. AHI was defined as the number of apneas and hypopneas per hour. Surgical response was defined as a decrease of AHI of 50 % or more and a postoperative AHI below 20.
Cephalometric analyses
Standard lateral cephalometric radiographs were obtained in 51 patients by a senior examiner using a standardized technique before surgery and at 6–12 months after surgery. The patients were seated in the natural head position at the end-expiration phase and were instructed not to swallow. The landmarks and reference lines for the conventional cephalometric analysis have been defined previously [14]. The preoperative and postoperative cephalograms were digitized by a single investigator using the Nemoceph NX 2006 software (Nemotec SL, Madrid, Spain).
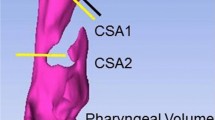
Variables analyzed included the angle from the sella to nasion to subspinale (SNA); the angle from the sella to nasion to supramentale (SNB); the angle between the maxilla and mandible (ANB); the angle of mandibular plane to Frankfort Horizontal (MPA); the distance from the sella to nasion (SN); the distance from anterior nasal spine to posterior nasal spine (ANS–PNS); the distance from the gonion (Go) to gnathion (Gn) (Go–Gn); the distance from the mandibular plane to hyoid bone (MP-H); the length of the soft palate (SPL); the sagittal area of the soft palate (SPA); the distance from posterior nasal spine to the posterior nasopharyngeal wall (PNS–UPW); the distance from the posterior border of the soft palate to the posterior nasopharyngeal wall (P-MPW); and the distance between the base of the tongue and the posterior pharyngeal wall (PAS; Fig. 1).
Diagram of cephalometric analysis: S sella, N nasion, A subspinale, B supramental, ANS anterior nasal spine, PNS, posterior nasal spine, CV cervical vertebrae, Or orbitale, Po porion, FH Frank fort horizontal plane, Go gonion, Me menton, Ge genial tubercle, Gn gnathion, UPW upper pharyngeal wall, MPW middle pharyngeal wall, U uvula, H anterior hyoid, MP mandibular plane, SNA maxillary protrusion angle, SNB mandibular protrusion angle, ANB angle between the maxilla and mandible, MPA mandibular plane angle, Go–Gn mandibular body length, MP-H distance from the hyoid to the mandibular plane, PNS-UPW width ofthe nasopharynx, U-MPW width of the oropharynx, PAS posterior airway space, SN distance from the sella to nasion, ANS–PNS length of the hard palate, SPL(P–PNS) length of the soft palate, SPA sagittal area of the soft palate
Data analysis
All statistical analyses were performed using SPSS, version 13 (SPSS Inc, Chicago, IL, USA). Continuous data are expressed as the mean ± SD, and a P value <0.05 was deemed to be statistically significant. Paired t-tests were used to compare preoperative and postoperative mean values. Unpaired t-tests were used to determine the statistical significance of relevant variables between responders and nonresponders. The χ 2 test was used to compare the frequency of response vs. nonresponse.
Logistic regression analysis was used to determine the factors associated with a successful surgery. The dependent variable was success of surgical intervention. Independent variables with a P value <0.20 when comparing responders and nonresponders were enrolled for logistic regression.
Results
Curative effect
A total of 23 patients met the success criteria, and the overall success rate was 45.1 % in this series. According to the Friedman OSA stages, the success rate was 50.0, and 40.7 % for patients with Friedman OSA stage I, II, and III, respectively. No significant differences appeared among the three stage groups (P = 0.80). Of the 51 patients, 31 were in the H-UPPP group, with a success rate of 35.5 %, and 20 were in the ZPPP group, with a success rate of 60.0 %. Although the success rate of the ZPPP group was higher than that of the H-UPPP group, no significant differences appeared between the two surgical groups (P = 0.09). In the ZPPP group, the success rate was 85.7 % for Friedman OSA stage II and 53.8 % for stage III, but no significant differences appeared between the two stage groups (P = 0.32).
Comparison of relevant parameters before and after surgery
A significant difference appeared in the BMI of patients before and after surgery (28.2 ± 2.4 vs. 27.7 ± 2.5, P < 0.05). The mean AHI decreased from 65.6 ± 17.2 to 29.5 ± 22.5/h (P < 0.001). The mean lowest oxygen saturation (LSAT) increased from 70.8 ± 10.9 to 79.3 ± 11.3 % (P < 0.001). The mean ESS decreased from 12.8 ± 6.1 to 5.5 ± 4.2 (P < 0.001). The mean length of soft palate (SPL) shortened from 41.3 ± 5.3 to 30.4 ± 4.4 mm (P < 0.001) after surgery. The mean area of soft palate (SPA) decreased from 349.3 ± 73.2 to 265 0 ± 58.6 mm2 (P < 0.001) after surgery. The mean distance of PNS-UPW lengthened from 22.1 ± 3.9 to 22.9 ± 3.3 mm (P = 0.051). Although the mean distance of U-MPW lengthened from 9.8 ± 3.0 to 10.4 ± 2.4 mm, this difference was not statistically significant (P = 0.13). The mean distance of PAS significantly shortened from 12.2 ± 4.0 mm to 10.0 ± 3.1 mm (P = 0.000), which was an unexpected finding. No other cephalometric and anthropometric variables differed statistically before and after surgery (Table 1).
Comparisons between responder and nonresponder groups
Overall, when patients were categorized as responders or nonresponders, we found that the U-MPW was significantly longer in the responder group than in the nonresponder group (10.7 ± 2.9 vs. 8.9 ± 2.8 mm, respectively; P = 0.05). The distance of PNS-UPW was longer in the responder group than in the nonresponder group, but the difference was not statistically significant. Although the MP-H distance was longer in the nonresponder group than in the responder group (23.3 ± 6.7 vs. 20.3 ± 5.5 mm, respectively; P = 0.12), the difference was not statistically significant. Comparisons between responder and nonresponder groups revealed no significant differences in age, Friedman stage, preoperative AHI, LSAT, ESS,and all other cephalometric parameters (P > 0.25; Table 2).
In the H-UPPP group, the preoperative U-MPW distance was significantly longer in the responder group than in the nonresponder group (12.5 ± 2.2 vs. 9.9 ± 2.8 mm, respectively; P = 0.007). No other cephalometric and anthropometric variables differed significantly between the responder and nonresponder groups. In the ZPPP group, the preoperative MPA was significantly smaller in the responder group than in the nonresponder group (27.0 ± 4.6° vs. 31.6 ± 4.7°, respectively; P = 0.04). No other cephalometric and anthropometric variables differed significantly between the responder and nonresponder groups.
All of the delta values shown in the tables were calculated by subtracting the postoperative values from the preoperative ones. The delta value of BMI (△BMI) in responders was significantly greater than that in nonresponders after surgery (0.9 ± 1.2 vs. 2 ± 1.2 kg respectively; P = 0.038). The delta values of SPA, SPL, PAS, and U-MPW did not differ significantly between responders and nonresponders (Table 3).
Logistic regression
Variables resulting in univariate P values of ≤0.2 were entered into a binary logistic regression model. Therefore, preoperative AHI (P = 0.192), △BMI (P = 0.038), U-MPW (P = 0.057), MP-H (P = 0.121), Friedman stage, and surgical method were put into a logistic regression model to determine predictive factors.
Logistic regression revealed that U-MPW and △BMI were the significant predictors of surgical success. Those with preoperative U-MPW greater than 10 mm had a higher success rate (65 %) than those with preoperative U-MPW less than or equal to 10 mm (25 %). In the H-UPPP group, preoperative U-MPW was the key predictor of H-UPPP surgical success. In the ZPPP group, MPA and Friedman stage were the key predictors of ZPPP surgical success. The success rate was 85.7 % for Friedman OSA stage II and 53.8 % for stage III, demonstrating that Friedman OSA stage is important for selecting candidates for ZPPP.
Discussion
Efficacy of UPPP
In this study, we analyzed our surgical results in 51 patients with severe OSAHS who had undergone H-UPPP or ZPPP. The overall success rate was 45.1 %. Historically, only patients with mild to moderate disease were considered good candidates for UPPP based on the observation of a significant difference in mean AHI between responders and nonresponders [4]. However, Senior et al. [15] found that patients with mild OSAHS did not achieve better UPPP outcomes than patients with severe disease. Caldarelli et al. [16] also reported that patients with severe disease obtained UPPP outcomes superior to those with mild disease. Moreover Li et al. [17] revealed that baseline AHI was not a determinant factor of UPPP success rates. Our study demonstrated that the UPPP success rate for severe disease was 45 %. This result is similar to the 40.7 % UPPP success rate reported by Sher et al. [4] in a systematic review of unselected patients with OSAHS. Thus UPPP was effective for some severe OSAHS patients, selecting appropriate candidates for UPPP based on disease severity (AHI) is not an effective approach.
In our study, the mean distances of preoperative P-MPW and PNS-UPW were longer in the responder group than in the nonresponder group. Of these, the mean distance from the soft palate to the posterior pharyngeal wall (P-MPW) was the single most significant predictor of surgical success. To date, no other study in the literature has identified P-MPW as a predictor of surgical success. These findings are the first systematic examination of the anatomy of the upper airways by cephalometry before and after UPPP in patients with severe OSAHS. Shepard et al. [18] found that the UPPP nonresponder group demonstrated a smaller baseline proximal retropalatal area and smaller overall retropalatal segment than responders. Additionally, Langin et al. [19] concluded that changes in the retropalatal area were correlated with UPPP response when evaluating the upper airway before and after surgery by cephalometry and pharyngeal CT scan. Responders demonstrated increased retropalatal airway size, whereas nonresponders demonstrated little or no change in retropalatal size. These findings suggest that UPPP responders have a better response if they begin with a larger and longitudinal upper airway that narrows at the level of the free margin of the soft palate. In a previous study [18], three-dimensional computed tomography was used to assess the changes of the upper airway dimension following UPPP. Thus, our results may be not comparable with those of previous studies due to the different evaluation methods employed.
Our results revealed a significant decrease of the retroglossal space (PAS) despite significant enlargement at the retropalatal space after UPPP. This finding is consistent with the results of several other studies. Li et al. [20] assessed changes in the upper airway dimension using computed tomography after extended uvulopalatal flap surgery. They found a decrease in the retroglossal space despite significant enlargement in the retropalatal space. Shepard et al. [21] also reported a similar paradoxical change. We presume that the decrease in retroglossal space results from scarring contraction of the tonsillar wound and may play a confounding factor in the unpredictability of UPPP outcomes.
In the present study, we found that the MP-H distance was not useful in predicting UPPP success, although the MP-H distance tended to be longer in nonresponders than in responders. This finding was similar to the results of some other studies. Woodson et al. [22] also reported no difference in MP-H distances between responders and nonresponders to UPPP, although nonresponders had longer posterior airways. Moreover, Doghramji et al. [12] found no relationship between MP-H distance and surgical outcome, although soft palates tended to be longer in patients in the responder group. In contrast, Millman et al. [11] concluded that a MP-H <20 mm, the presence of a baseline AHI <38, and the absence of retrognathia were significant predictors for a positive response after UPPP. However, they used more stringent criteria for surgical success (AHI <10 or AHI <20 with a 50 % reduction from baseline AHI), which could have affected their findings. Some studies [23, 24] have confirmed that the MP-H distance is positively correlated with severity of OSAHS (AHI). All patients in our study had severe OSAHS with a presurgical AHI >30. Thus, it is possible that there was no difference in the MP-H distance between responders and nonresponders to UPPP, although the MP-H distance tended to be longer in the nonresponders. Of course, the conflicting findings might be attributed to their small sample sizes.
Friedman et al. [5] suggested that the Friedman Staging System based on palatal position jointed with size of palatine tonsils could predict surgical outcome in OSAHS patients and is superior to the severity of disease as a predictor for successful UPPP. In the present study, the ZPPP success rate of Friedman OSA stage II was higher than that of Friedman stage III, and MPA and Friedman stage could predict the outcome of ZPPP. This result is consistent with previous findings that MPA and Friedman stage are key predictors of ZPPP surgical success [8]. Our results demonstrate that Friedman OSA stage is important for selecting candidates for ZPPP. Additionally, the MPA may affect the growth of the mandible and size of the hypopharynx; the greater the angle, the steeper the mandibular plane. In other words, the tongue base may tend to fall backwards and obstruct the hypopharynx, and affect the result of ZPPP. However, we failed to find any predictive value of Friedman stages I–III in success of UPPP. This discrepancy can presumably be explained by the different patient populations studied, because all of our patients had severe OSAHS. The majority of the patients in our study had stage II disease (39 %) and stage III disease (53 %), with only 8 % in stage I disease. Therefore, it was difficult to distinguish the differences between the responder and the nonresponder groups, and further studies are required with larger samples.
We observed a significant reduction in BMI after UPPP. Weight reduction is known to play an important role in improving treatment in OSA patients [25]. Sutherland et al. [26] found that improved sleep apnoea after weight loss was associated with an increase in velopharyngeal airway size. Additionally, weight loss decreases upper airway collapsibility during sleep because of reduced mechanical loads resulting from adiposity and/or subsequent improvements in neuromuscular control.
Conclusions
Although the success rate was unsatisfactory, uvulopalatopharyngoplasty was still an effective surgical procedure for severe OSAHS patients. U-MPW and △BMI were the significant predictors of surgical success. Those with preoperative U-MPW greater than 10 mm had a higher success rate than those with preoperative U-MPW less than or equal to 10 mm.
References
Lin HS, Zuliani G, Amjad EH, Prasad AS, Badr MS, Pan CJG, Rowley JA (2007) Treatment compliance in patients lost to follow-up after polysomnography. Otolaryngol Head Neck Surg 136:236
Haniffa M, Lasserson T, Smith I (2004) Interventions to improve compliance with continuous positive airway pressure for obstructive sleep apnoea. Cochrane Db Syst Rev 18(4):CD003531
Fujita S, Conway W, Zorick F, Roth T (1981) Surgical correction of anatomic azbnormalities in obstructive sleep apnea syndrome: uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg 89:923–934
Sher AE, Schechtman KB, Piccirillo JF (1996) The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep 19:156–177
Friedman M, Ibrahim H, Joseph NJ (2004) Staging of obstructive sleep apnea/hypopnea syndrome: a guide to appropriate treatment. Laryngoscope 114:454–459
Friedman M, Ibrahim HZ, Vidyasagar R, Pomeranz J, Joseph NJ (2004) Z-palatoplasty (ZPP): a technique for patients without tonsils. Otolaryngology-Head and Neck Surg 131:89–100
Han D, Ye J, Lin Z, Wang J, Zhang Y (2005) Revised uvulopalatopharyngoplasty with uvula preservation and its clinical study. ORL 67:213–219
Yi HL, Yin SK, Zhang YJ, Chen B, Lu WY, Sun XQ, Cao ZY, Wu HM, Guan J (2009) Z-palatopharyngoplasty for obstructive sleep apnea/hypopnea syndrome. Otolaryngol Head Neck Surg 140:640–645. doi:10.1016/j.otohns.2009.02.002
Xiong YP, Yi HL, Yin SK, Meng LL, Tang XL, Guan J, Luo HP, Zhang WT, Chen B (2011) Predictors of surgical outcomes of uvulopalatopharyngoplasty for obstructive sleep apnea hypopnea syndrome. Otolaryngol Head Neck Surg 145:1049–1054. doi:10.1177/0194599811420811
Hudgel D, Harasick T, Katz R, Witt W, Abelson T (1991) Uvulopalatopharyngoplasty in obstructive apnea: value of preoperative localization of site of upper airway narrowing during sleep. Am Rev Respir Dis 143:942–946
Millman RP (2000) Simple Predictors of uvulopalatopharyngoplasty outcome in the treatment of obstructive sleep apnea. Chest 118:1025–1030. doi:10.1378/chest.118.4.1025
Doghramji K, Jabourian ZH, Pilla M, Farole A, Lindholm RN (1995) Predictors of outcome for uvulopalatopharyngoplasty. Laryngoscope 105:311–314
Friedman M, Ibrahim HZ, Vidyasagar R, Pomeranz J, Joseph NJ (2004) Z-palatoplasty (ZPP): a technique for patients without tonsils. Otolaryngol Head Neck Surg 131:89–100
Ricketts RM (1968) Esthetics, environment, and the law of lip relation. Am J Orthod 54:272–289
Senior BA, Rosenthal L, Lumley A, Gerhardstein R, Day R (2000) Efficacy of uvulopalatopharyngoplasty in unselected patients with mild obstructive sleep apnea. Otolaryngol Head Neck Surg 123(3):179–182
Caldarelli DD, Cartwright R, Lilie JK (1986) Severity of sleep apnea as a predictor of successful treatment by palatopharyngoplasty. Laryngoscope 96:945–947
Li HY, Wang PC, Lee LA, Chen NH, Fang TJ (2006) Prediction of uvulopalatopharyngoplasty outcome: anatomy-based staging system versus severity-based staging system. Sleep 29:1537–1541
Shepard JW Jr, Olsen KD (1990) Uvulopalatopharyngoplasty for treatment of obstructive sleep apnea. Mayo Clin Proc 65:1260–1267
Langin T, Pépin JL, Pendlebury S, Baranton-Cantin H, Ferretti G, Reyt E, Lévy P (1998) Upper airway changes in snorers and mild sleep apnea sufferers after uvulopalatopharyngoplasty (UPPP). Chest 113:1595–1603
Li HY, Li KK, Chen NH, Wang CJ, Liao YF, Wang PC (2005) Three-dimensional computed tomography and polysomnography findings after extended uvulopalatal flap surgery for obstructive sleep apnea. Am J Otolaryngol 26:7–11
Shepard JW Jr, Thawley SE (1989) Evaluation of the upper airway by computerized tomography in patients undergoing uvulopalatopharyngoplasty for obstructive sleep apnea. Am J Respir Crit Care Med 140:711
Woodson B, Conley S, Dohse A, Feroah T, Sewall S, Fujita S (1997) Posterior cephalometric radiographic analysis in obstructive sleep apnea. Ann Otol Rhinol Laryngol 106:310–313
Will MJ, Esther MS, Ramirez SG (1995) A comparison of cephalometric analysis with ethnicity in obstructive sleep apnea syndrome. South Med J 88:S79
Chang ET, Shiao GM (2008) Craniofacial abnormalities in Chinese patients with obstructive and positional sleep apnea. Sleep Med 9:403–410
Johansson K, Neovius M, Lagerros YT, Harlid R, Rössner S, Granath F, Hemmingsson E (2009) Effect of a very low energy diet on moderate and severe obstructive sleep apnoea in obese men: a randomised controlled trial. BMJ 339:b4609
Sutherland K, Lee RWW, Phillips CL, Dungan G, Yee BJ, Magnussen JS, Grunstein RR, Cistulli PA (2011) Effect of weight loss on upper airway size and facial fat in men with obstructive sleep apnoea. Thorax 66:797–803
Acknowledgments
Source of funding: program for advancing front technology of Shanghai Shenkan Center (SHDC12010209).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Liu, S.R., Yi, H.L., Yin, S.K. et al. Associated predictors of therapeutic response to uvulopharyngopalatoplasty for severe obstructive sleep apnea hypopnea syndrome. Eur Arch Otorhinolaryngol 270, 1411–1417 (2013). https://doi.org/10.1007/s00405-013-2404-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-013-2404-5