Abstract
The objective of the study is to assess the correlation between outpatient department (OPD) assessment and sleep nasendoscopy (SNE) in treatment planning for sleep related breathing disorders. The study design includes a blinded, cohort study comparing the treatment prediction based on OPD clinical evaluation with SNE in consecutive, adult patients by a single clinician with a specialist interest in snoring related disorders. Patients with moderate to severe obstructive sleep apnoea and those who had undergone previous treatment were excluded. The study was conducted in Royal National Throat, Nose and Ear Hospital, London and Queen’s Hospital, Romford. Ninety-four patients were recruited as participants for the study. The main outcome measures include site of obstruction and treatment planning. The results show no significant correlation between the two groups with SNE recommending less surgical intervention and a choice of surgical and non-surgical management in greater number of patients. In conclusion, even in experienced hands, clinical prediction is significantly modified by SNE findings. The addition of SNE to the diagnostic pathway, to assess the three-dimensional dynamic anatomy of the upper airway, provides a valuable adjunct to the OPD assessment of upper airway collapse. This affords the clinician a greater accuracy of diagnosis and the patient a more focussed management strategy with increased choice of modality of treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The perfect diagnostic tool for the investigation and subsequent evaluation of upper airway dynamics has yet to be described. There are multiple methods that purport to achieve the most accurate diagnosis and management strategy. These include out-patient (OPD) based clinical assessments, haematological investigation, polysomnography, acoustic evaluation [1, 2], sleep nasendoscopy (SNE) [3–6], X-ray cephalometry, magnetic resonance scanning, spontaneous sleep videoendoscopy and multi-channel pressure measurements. Considerable controversy exists as to which method or combination of methods represents the gold-standard investigation.
The technique of SNE, developed in the late 1980s and further modified during the 1990s, has been the focus of both positive and negative opinion [6–8]. In our eyes it represents a repeatable, cost effective, and reliable adjunct to OPD findings. SNE provides two assessments of the upper airway which are not possible to evaluate in the OPD setting: firstly, a dynamic, three-dimensional, real time evaluation of the anatomical sites of upper airway collapse during sleep; and secondly, the effect of mandibular advancement on the airway and snoring [3]. In our institution this is essential in the development of a management strategy that incorporates surgical and non-surgical options allowing the patient to make the best available informed choice [9]. It is important to note that SNE, since its inception, represents an adjunct to clinical evaluation and is not designed to displace this.
This study aims to examine and compare the information derived from clinical evaluation with that derived from SNE in a blinded prospective study. By doing this we hope to establish whether SNE contributes to the diagnosis of snoring.
Method
The subjects for this prospective, blinded, cohort study were recruited at Queen’s Hospital, Oldchurch and the Royal National Throat, Nose and Ear Hospital. They represent 94 consecutive patients, referred between May 2005 and August 2006 with sleep disordered breathing, to a single ENT consultant surgeon with a special interest in snoring related disorders. Patients who had the suspicion of OSA were sent for formal polysomnography and if proven excluded as were those who had had previous treatment. All patients underwent OPD evaluation and SNE by the same clinician. A diagnosis of anatomical site of obstruction and a subsequent prediction of treatment was made after OPD evaluation, and again after SNE with the clinician being blinded to the previous conclusions.
Clinical evaluation
In our department, OPD evaluation has been standardized using a set proforma recording detailed patient information broadly categorized as follows (see Appendix)
Patient demographics, patient history and, when present, partner history (nocturnal symptoms inter alia: restless sleep, sleep disruptions, choking, oesophageal reflux, nocturia, night sweats, morning headaches, mood alterations, sexual dysfunction, autonomic behaviour, short term memory loss); Epworth Sleepiness Scale [10]; the measurement of height and weight with the calculation of body mass index (BMI) [1, 11]; measurement of blood pressure; anthropomorphic measurement of neck circumference (collar size); examination of the architecture of the nose (inter alia, nasal septum deviations, inferior turbinate size and nasal polyposis), the oropharynx (inter alia, the size of the tonsils, uvula and soft palate, degree of overbite and nature of dentition), and the larynx and pharynx with a combination of flexible nasendoscopy, endoscopy and direct visualisation in combination with Müller’s manoeuvre [12] and simulated snoring techniques [13]; haematological investigation including thyroid function tests and full blood count.
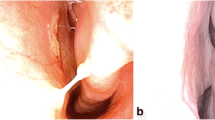
Sleep nasendoscopy
All subjects underwent SNE, performed by the senior author who was not made aware of the previous conclusions reached. This was made possible by the nature of the time delay between OPD assessment and SNE imposed by the hospital waiting list for elective surgery. In accordance with the technique described by Croft and Pringle [7], subjects lay supine with a representation of their usual size of pillow. A light phase of sleep was induced, by the same anaesthetist in each case, using intravenous midazolam (0.05 mg/kg) and propofol (1.5 mg/kg), titrated individually with the subjects heart rate, blood pressure and blood oxygen saturations being continuously monitored. The desired level of sedation, with all reflexes present, was maintained with further boluses of Propofol [4].
A flexible nasendoscope was introduced and any snoring noted with all levels of obstruction graded according to the grading system described by Pringle and Croft [14]. In cases of multisegmental obstruction the percentage contribution of the soft palate and tongue base was noted. The jaw was then lifted by 3–5 mm to simulate the effect of a mandibular advancement splint and any changes to the snoring again and upper airway were documented [3].
Statistics
The data was recorded on to an excel spreadsheet and analysed using the Statistical package for social sciences (SPSS).
Results
Ninety-four patients (77 male and 17 female) were recruited into the study with a mean age of 45 (Fig. 1), an average Epworth Sleepiness Score of ten (standard deviation 5.3) and average BMI of 28.5 (standard deviation 4.6). Two patients with known OSA were included in the study as they declined management with continuous positive airway pressure (CPAP). On OPD evaluation one was felt to be suitable for a Laser assisted uvulopalatoplasty (LAUP) and the other CPAP. However, both subsequently went on to have CPAP based on SNE findings (Fig. 3).
Examination revealed: nasal septal deviation in 65.6%; a prominent uvula in 50%; a lax soft palate in 81%; tonsils in 69.5% of which 43.7% were Grade I, 48.4% Grade II and 7.8% Grade III; redundant oropharyngeal in 55.9% and retrognathia (Class III malocclusion) in 3.2%.
Simulated Snoring demonstrated a palatal cause in 80.9% and a tongue base cause in 2.1%. About 12.7% of patients were unable to simulate a snore.
Müllers manoeuvre attempted in all patients but only circa 46% patients were able to adequately perform the manoeuvre and these showed no correlation with the final OPD or SNE prediction.
Overall OPD evaluation predicted that a palatal intervention LAUP was indicated in 74.4% (n = 70) and mandibular advancement splint/device (MAS) in 22.3% (n = 21) (Fig. 2).
SNE predicted LAUP in 47.8% (n = 45) and a Mandibular advancement splint (MAS) in 41.4% (n = 39) and a choice of modalities in 8.5% (n = 8) (Fig. 3).
Statistical analysis of the predictions from OPD and SNE when evaluated by Pearson χ 2 test shows a statistically significant difference between the two groups with a p value of less than 0.001.
Analysis of the Correlation between OPD and SNE prediction showed a statistically significant level of disagreement (kappa = 0.199; phi = 0.0001) (Table 1; Figs. 4, 5).
Discussion
The relevance of SNE is the subject of much debate and its use remains controversial. Criticism centers on a number of points: Firstly, SNE represents a snapshot of snoring and critics would argue that this does not provide a representative picture as acoustic crest factor analysis has suggests that the dynamics of snoring change during the sleep cycle [15]. Secondly, that sedation-induced sleep, including target controlled infusion (TCI), may not correlate with natural, physiological sleep as it can cause a greater degree of muscle relaxation leading to the potential for false positive obstructive breathing [2, 16]. And thirdly, that SNE is subjective and open to inter-observer and inter-anaesthetist related error.
A study often quoted in the case against SNE is that of Badawey et al., which concluded that SNE was not of value in the assessment of the habitual snorer. However we feel that their use of intra nasal co-phenylacaine and the differing anaesthetic protocol may well account for the differences in results between our unit and theirs [17]. Not withstanding these criticisms there has been much literature published in support of the use of SNE in the identification of the site of upper airway collapse and snoring [4, 18].
This study aims to compare the diagnosis, predicted management strategy and treatment choice offered to the patient from outpatient clinical assessment and SNE.
The main finding of the study is that the information derived from SNE significantly modifies the OPD prediction of treatment option offered to the patient. OPD assessment recommends a palatal intervention in the majority of cases 74.4% (n = 70), however, if this cohort is assessed with SNE only 54% of these (n = 38/70) demonstrate a palatal cause for their obstruction. This means that potentially, unnecessary surgery is avoided 46% of patients recommended surgery by in the OPD (n = 32/70).
SNE allowed for the consideration of more than one modality of treatment for the patient so that a choice between a surgical intervention or a conservative one, such as MAS, can be offered. Based on SNE findings: six cases predicted a LAUP were offered a choice between MAS or LAUP; 25 cases predicted a LAUP were modified to a non-surgical intervention (MAS); and a non-surgical solution was offered to 32 patients (33%) who were only offered a surgical option from OPD evaluation. However, seven (7.4%) cases offered MAS at OPD were recommended to have a LAUP at SNE and two (2.1%) cases recommended a choice in OPD were recommended a MAS at SNE.
SNE also highlighted one patient, with no history of OSA, who dramatically collapsed their upper airway and desaturated to a point that a sleep study was instigated and moderate to severe OSA was subsequently diagnosed.
The analysis of the OPD Simulated Snoring test shows that it predicts a palatal cause in 81% of patients compared to 47.8% by SNE. This highlights the benefit of comparing the dynamics in the asleep versus the awake state where the muscle tone of the upper airway differs. Müllers manoeuvre was found not to correlate with prediction from OPD or SNE and only a small percentage of patients were able to perform the manoeuvre satisfactorily. This agrees with previous published literature [19].
Conclusion
Even in experienced hands, clinical prediction is significantly modified by SNE findings. SNE has been proven to be a reliable assessment tool in snoring evaluation in some studies and disputed in others [14, 20–22]. Clearly, the dynamics of the upper airway cannot be fully assessed in the clinical setting. The addition of SNE to the diagnostic pathway, to assess the three-dimensional dynamic anatomy of the upper airway, provides a valuable adjunct to the OPD assessment of upper airway collapse in spite of its additional cost. Whilst the gold standard assessment tool is yet to be defined, we believe that SNE affords the clinician a greater accuracy of diagnosis and the patient a more focussed management strategy with increased choice of modality of treatment.
References
Browman CP, Sampson MG, Yolles SF (1984) Obstructive sleep apnea and body weight. Chest 85(3):435–438
Jones TM, Ho MS, Earis JE, Swift AC, Charters P (2006) Acoustic parameters of snoring sound to compare natural snores with snores during ‘steady-state’ propofol sedation. Clin Otolaryngol 31(1):46–52
Battagel JM, Johal A, Kotecha BT (2005) Sleep nasendoscopy as a predictor of treatment success in snorers using mandibular advancement splints. J Laryngol Otol 119(2):106–112
Berry S, Roblin G, Williams A, Watkins A, Whittet HB (2005) Validity of sleep nasendoscopy in the investigation of sleep related breathing disorders. Laryngoscope 115(3):538–540
Georgalas C, Kotecha B (2004) Predictive value of sleep nasendoscopy in the management of habitual snorers. Ann Otol Rhinol Laryngol 113(5):420 Comment
Camilleri AE, Ramamurthy L, Jones PH (1995) Sleep nasendoscopy: what benefit to the management of snorers? J Laryngol Otol 109(12):1163–1165
Croft CB, Pringle MB (1991) Sleep nasendoscopy: a technique of assessment in snoring and obstructive sleep apnoea. Clin Otolaryngol 16:504–509
Counter P, Wilson JA (2004) The Management of Simple Snoring. Sleep Med Rev 8(6):433–441
American Academy of Sleep Medicine Task Force (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 22:667–689
Johns MW (1993) Daytime sleepiness, snoring and obstructive sleep apnoea: the Epworth Sleepiness Scale. Chest 103:30–36
Quetelet LAJ (1842) A treatise on man and the development of his faculties. Scholars Facsimilies and Reprint. ISBN 0820110612
Li W, Ni D, Jiang H, Zhang L (2003) Predictive value of sleep nasendoscopy and the Müller maneuver in uvulopalatopharyngoplasty for the obstructive sleep apnea syndrome. J clin otorhinolaryngol 17(3):145–146 Lin Chuang Er Bi Yan Hou Ke Za Zhi
Liistro G, Stanescu D, Veriter C (1991) Pattern of simulated snoring is different through mouth and nose. J Appl Physiol 70:2736–2741
Pringle MB, Croft CB (1993) A grading system for patients with obstructive sleep apnoea-based on sleep nasendoscopy. Clin Otolaryngol 18:480–484
Hill PD, Osman EZ, Osbourne JE, Lee BWV (2000) Changes in snoring during natural sleep identified by acoustic crest factor analysis at different times of night. Clin Otolaryngol 25:507–510
Agrawal S, Stone P, McGuinness K, Morris J, Cameilleri AE (2002) Sound Frequency analysis and the site of snoring in natural and induced sleep. Clin Otolaryngol 27:162–166
Badawey MR, McKee G, Heggie N, Marshall H, Wilson JA (2003) Predictive value of sleep nasendoscopy in the management of hjabitual snorers. Ann Otol rhino Laryngol 112(1):40–44
Saunders NC, Tassone P, Wood G, Norris A, Harries M, Kotecha B (2004) Is acoustic analysis of snoring an alternative to sleep nasendoscopy? Clin Otolaryngol Allied Sci 29(3):242–246
Ritter CT, Trudo FJ, Goldberg AN, Welch KC, Maislin G, Schwab RJ (1999) Quantative evaluation of the upper airway during nasopharyngoscopy with the Muller manouevre. Laryngoscope 109(6):954–963
Johal A, Battagel JM, Kotecha BT (2005) Sleep nasendoscopy: a diagnostic tool for predicting treatment success with mandibular advancement splints in obstructive sleep apnoea. Eur J Orthod 27(6):607–614
Kotecha BT, Hannan A, Khalil HMB, Georgalas C, Bailey P (2007) Sleep nasendoscopy: a 10 year retrospective audit study. Eur Arch Otorhinolaryngol 264:1361–1367
Stuck BA, Maurer JT (2007) Airway evaluation in obstructive sleep apnea. Sleep Med Rev (Epub ahead of print)
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix


Rights and permissions
About this article
Cite this article
Hewitt, R.J.D., Dasgupta, A., Singh, A. et al. Is sleep nasendoscopy a valuable adjunct to clinical examination in the evaluation of upper airway obstruction?. Eur Arch Otorhinolaryngol 266, 691–697 (2009). https://doi.org/10.1007/s00405-008-0831-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-008-0831-5