Abstract
A new palatal procedure for snoring/obstructive sleep apnea (OSA) is described. The procedure was named as barbed reposition pharyngoplasty (BRP). The technique is described step by step. The new surgical technique was carried out in ten adult OSA patients with mean age of 53.4 ± 12.4 years (average 30–70) with confirmed retropalatal obstruction. In this pilot study; we assessed the feasibility by calculating the number of cases that failed to be operated and converted to other palatal technique during the same surgical setting, safety was assessed by evaluating both intra-operative and post-operative complications, teachability measured by the learning curve of our team members (the time of surgical procedure). In this study, the technique is proved to be feasible in all cases. There were no significant intra-operative or post-operative complications. Objective clinical improvement was confirmed by polysomnography 6 months post-operative with significant decrease in mean AHI from 43.65 ± 26.83 to 13.57 ± 15.41 (P = 0.007), daytime sleepiness assessed by Epworth Sleepiness Scale from 11.6 ± 4.86 to 4.3 ± 2 (P < 0.01), ODI from 44.7 ± 27.3 to 12.9 ± 16.3 (P = 0.004). Operative time decreased over the course of the study with an initial steep ascent in technical skill acquisition followed by more gradual improvement, and a steady decrease in operative time to as short as 20 min. Our preliminary results suggest that BRP technique is feasible, safe and effective in management of OSA patients. Moreover, it is easy to learn even for not experienced surgeons, less time consuming and with no significant complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The main mechanism of the most classic palatal techniques for snoring/obstructive sleep apnea syndrome (OSAS) was basically the shortening of the soft palate by trimming the free edge (UPPP and LAUP) or pulling up the uvula and the soft palate (UPF). In the last years, many new palatal surgical techniques for snoring and OSAS were devised to address mainly the lateral pharyngeal wall and to enlarge laterally the oropharyngeal inlet (lateral pharyngoplasty [1], Z-palatoplasty [2], uvulopalatoplasty (UP2) [3], expansion sphincter pharyngoplasty (ESP) [4] and relocation pharyngoplasty [5]). In our hands, ESP proved to be in more than 250 cases a significant step forward after a previous experience of more than 1000 uvulopalatopharyngoplasty (UPPP). As the palate component of our multilevel procedure, ESP proved to be superior to UPPP [6]. Furthermore, systematic retrospective review of literature with the analysis of our cases and a targeted cadaver dissection study prompted us to modify our approach to lateral pharyngeal wall/retropalatal airway switching from ESP to the relocation pharyngoplasty according to Li [5], with some modifications inspired to different solutions of experienced surgeons. We introduced:
-
1.
“Barbed” which refers to the use of knotless bidirectional reabsorbable sutures introduced for similar purposes by Mantovani et al. [7].
-
2.
“Reposition pharyngoplasty” because it displaces the posterior pillar (palatopharyngeal muscle) in a more lateral and anterior position to enlarge the oropharyngeal inlet as well as the retropalatal space.
-
3.
Suspension of the posterior pillar to the pterygomandibular raphe.
-
4.
Initial weakening of the inferior aspect of the palatopharyngeal muscle.
The multiple lateral sustaining suture loops of BRP proved to be more stable than the single pulling tip suture of ESP, with no risk of tearing the muscle fibers losing the entire pulling force.
Patients and methods
This preliminary prospective study was conducted at the Otolaryngology, Head and Neck Surgery Department, G.B. Morgagni-L. Pierantoni Hospital, ASL of Romagna, Forli, Italy, starting from February 2014 until January 2015. Prior to conduction of the study, informed detailed consent was taken from patients. Patients were enrolled in conformance with the following inclusion/exclusion criteria:
Inclusion criteria included
Patients diagnosed with mild to severe OSA (AHI ≥5), having the main site of obstruction at the retropalatal level with or without retrolingual obstruction, patients not accepting or unwilling to use CPAP treatment, failures of previous surgery, age between 21 and 70 years, body mass index (BMI) ≤35, patients fit for general anesthesia (ASA ≤2).
Exclusion criteria included
Patients >70 years and/or with severe medical illness, patients with significant craniofacial anomalies affecting airway, BMI >35, patients with limited mouth opening (interincisive distance <1.5 cm) and patients unfit for general anesthesia (ASA >2).
A careful general, ear nose and throat (ENT) history of each patient was taken with particular attention given to sleep history.
For all cases, the following data were recorded: (1) age, (2) sex, (3) date of diagnosis, (4) pre-operative and 6 months post-operative apnea–hypopnea index (AHI) and lowest oxygen saturation (all the sleep studies were carried out in an unattended way by means of a Polymesam Unattended Device 8-channel; reviewed and scored by the same expert in sleep medicine according to the American Academy of Sleep Medicine Guidelines 2007 [8], (5) pre-operative and post-operative Epworth Sleepiness Scale (ESS) using the Italian version of the Epworth test that was adapted and tested for the Italian-speaking population [9], (6) post-operative dysphagia [10], (7) pain visual analog scale (VAS; 0–10) post-operatively, (8) operative times for BRP surgical technique, as measured by our electronic system, (9) discharge date, (10) complication types and rate, and (11) fiber-optic examination of retropalatal space 6 months post-operative.
Surgical technique
All the procedures were performed with patients under general anesthesia and orally intubated, exposed by a Boyle–Davis mouth gag together with lateral cheek retractors to give wide access to the surgical field. The patient was positioned in supine position with under shoulder inflatable bag to keep the head extended. In most of the cases, as reported into details in Table 1, BRP was a step of a single access multisite procedure including if required a nasal procedure, a thyro-hyoid pexy, a transoral robotic tongue base reduction and supraglottoplasty.
Surgical steps
The first step was bilateral tonsillectomy with identification and meticulous sparing of the palatoglossus and palatopharyngeus muscles; the most important trick was to spare as much as possible the mucosal covering of both anterior and posterior pillars.
Two weakening or releasing partial incisions were done by a pinpoint bowie (Colorado®) at the inferior (caudal) part of the palatopharyngeal muscle. A full thickness (mucosa and muscle) triangle was removed at the superolateral corner of the tonsil to obtain a wider and most squared oropharyngeal inlet.
The center of the palate was marked at palatal spine (Fig. 1a), also the pterygomandibular raphe in both sides were located by digital palpation and marked. We used a single barbed suture, bidirectional polydioxanone absorbable monofilament, size 0, with transition zone in the middle. One needle was introduced at the center point then passed laterally within the palate, turning around pterygomandibular raphe till it comes out at the most superior part of the raphe at one side; the thread is pulled until it hangs at the central transition zone which is a free zone present between the two directions of the thread (Fig. 1b). The needle again is re-introduced close to point of exit, passing around the pterygomandibular raphe, till it comes out into the tonsillectomy bed, then through the upper part of the palatopharyngeus muscle and comes out near to mucosa of posterior pillar not through it (Fig. 1c). The posterior pillar is entered at the junction between the upper third and the lower two-thirds. Then, again the needle is passed back through the tonsillectomy bed and then this suture will be suspended around the raphe again; a gentle traction is then applied on the thread only and no knots are taken (Fig. 1d). This leads to a stable repositioning of the posterior pillar to more lateral and anterior location without any knot, then this stitch is repeated at least three times between raphe and muscle till the lower pole of the muscle is reached. The opposite side is done by the same way. Finally, each thread comes out at the raphe of the same side, for locking of the stitches and looseness prevention; a superficial stitch in the opposite direction is taken, and then the thread is cut while bushing the tissue downward for more traction. Further explanation of surgical steps is presented in Fig. 2.
a Marking the center of palate, pterygomandibular raphe and squaring of anterior pillars. b The barbed suture around the upper part of the right raphe and it hangs at the central transition zone. c The needle is passed through the upper part of the palatopharyngeus muscle and comes out near to mucosa of posterior pillar not through it. d The needle is passed through the upper pole and suspended around the raphe, pulling of barbed suture without taking of knots
The tip of uvula is not removed if it is short, instead a small island of the mucosa is removed from its anterior aspect by monopolar diathermy, and then coagulation of submucosal tissue is done by bipolar diathermy, after suturing this mucosal gap the uvula will bend forward. If the uvula is too long its tip is trimmed.
Results
Ten adult male patients were included in this preliminary study (3 patients underwent BRP as well as TORS with tongue base reduction, 7 BRP with nasal and/or hyoid surgery) with mean age 53.4 ± 12.4 (range 30–70), mean BMI 28.5 ± 3.6 (range 22.6–33.9), pre-operative AHI (43.65 ± 26.83), pre-operative ODI (44.7 ± 27.32), pre-operative ESS (11.6 ± 4.8); the pre and post operative results are shown in Table 2 and Fig. 3.
The technique was feasible in all patients; there were no significant intra-operative or post-operative complications. The main complaint was foreign body sensation at the palate which spontaneously disappeared in a period ranging from 2 weeks to 1 month. Two patients felt the extrusion of short piece of suture, without any additional problems.
The stability of the new wide retropalatal space was confirmed by fiber-optic examination 6 months post-operative (Fig. 4).
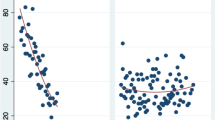
With regard to teachability, operative time decreased over the course of the study with an initial steep ascent in technical skill acquisition followed by more gradual improvement, and a steady decrease in operative time to as short as 20 min now with more than 40 cases was observed by our surgical team (Fig. 5).
If we considered a widely accepted success definition as post-operative AHI <20 with a reduction <50 %, we registered a success rate of 90 %. The only patient who did not respond had the highest pre-operative BMI of 33.9.
We considered two important outcome measures related to the surgery; pain as assessed by VAS and dysphagia as assessed by MD-Anderson dysphagia questionnaire, the results are shown in detail in Tables 3, and 4.
Discussion
Barbed reposition pharyngoplasty is deeply inspired by the relocation pharyngoplasty (RP) as devised and published by Li et al. [5]. The common purpose is to use a series of sutures to widen the oropharyngeal isthmus laterally and to relocate anteriorly the lateral insertion of the soft palate to increase the retropalatal airway. The main differences between RP and BRP are:
-
1.
The anterior sustaining anatomical structure is the more stable fibrous pterygomandibular raphe instead of the weaker palatoglossus muscle; this solution is inspired to Mantovani technique [7]. Pterygomandibular raphe is a fibrous band joining the pterygoid hamulus to the mandible relatively variable in the different subjects; it is always easy to locate during surgery by inspection or, may be better, by palpation. It lies anteriorly and laterally to the posterior pillar, in the best position for an effective pulling direction to increase the transversal oropharyngeal dimension and to widen the retropalatal anteroposterior distance. Its anatomical location is far from significant nerves and vessels preventing undesired complications during suturing. Anyway parotid duct opening must be located and kept far from the suture.
-
2.
The repositioned muscle is the palatopharyngeal muscle, after a preliminary inferior release; this solution is inspired to Cahali technique [1]. The inferior muscle release is planned to allow an easier and more stable repositioning of the posterior pillar in a more lateral and anterior location without any significant tension. Moreover, if we consider the anterior and posterior pillars as two of the main legs of a tripod (the third leg is the soft palate itself), the posterior leg release shifts the anteroposterior muscle force balance moving the entire soft palate forward. No superior pharyngeal constrictor muscle section was necessary.
-
3.
The bidirectional reabsorbable barbed suture instead of a conventional series of single stitches; this solution is inspired to Mantovani technique [7]. Barbed suture proved to be much faster and easier to handle, because it is a knotless technology (knotting inside the pharynx may be not easy for the less experienced surgeons, and even for the most experienced ones, it takes obviously more time). Also, barbed suture allows running more thread loops around the muscle, creating a sort of dense net, for a better distribution of the repositioning forces over the muscle flap. In comparison to Pang–Woodson technique [4], the pulling suture works with a 90° angle on the muscle fibers array, with a much less risk to tear the flap tip.
-
4.
The tip of uvula is not trimmed, but a mucosal island is removed from its anterior aspect. After suturing of the mucosal gap the uvula is just bent forward, leaving intact the posterior surface, to reduce the risk of post-operative foreign body sensation.
An anterior pillar totally sparing approach for tonsillectomy proved to be very useful for the better tensionless reconstruction of the mucosal covering at the end of the procedure. Two more remarks about the posterior pillar repositioning are given. If properly located between the upper third and the inferior two-thirds of the posterior pillar, the first suture loop will produce a sort of “posterior pillar steal”, inspired to the same concept of lateral crural steal technique in tip rhinoplasty. The meaning is that the upper part of the posterior pillar will be transposed into the soft palate free edge, which will be transversally enlarged in a very significant way. The posterior pillar mucosa is not dissected free from the flap, but follows it in its repositioning. The meaning is less surgical time, no potential mucosal damage, immediate mucosal closure, probably faster recovery and less pain.
Limitations of the study
As BRP is presented as a step in a multilevel procedure, it is quite impossible to define the single role of BRP in this complex multilevel procedure. In our study, the efficacy is just one of the minor topics; the key points are feasibility, safety and teachability. Even more, the number of patients is quite minimal for discussing efficacy, so we are working in a future study in which we will present more data about the efficacy in a larger group of patients.
Conclusion
Barbed reposition pharyngoplasty proved to be in this pilot study an easy to learn, quick, safe and effective new palatopharyngeal procedure, devised as a significant improvement of the RP by Li and Coll. The key points that must be considered are the use of a knotless reabsorbable suture technology, the minimal and targeted muscle manipulation, the use of the pterygomandibular raphe as sustaining structure. The minimal muscle and mucosa resection and the absence of knots in the pharynx are well accepted by the patients in terms of invasiveness. The minimal required manipulations and the knotless technique mean for the not experienced surgeon a technique easy to learn, quick and safe to perform, including inside a simultaneous multilevel procedure if required. A single bidirectional barbed suture economical cost is superior to a conventional suture cost, but one suture is sufficient instead of 2 or 3, also this superior cost can be balanced by the less operative time. Preliminary results seem very promising also in terms of efficacy and safety. Further studies in a significant number of patients, possibly in a multicenter setting, are strongly recommended in the future and already under evaluation.
References
Cahali MB (2003) Lateral pharyngoplasty: a new treatment for obstructive sleep apnea hypopnea syndrome. Laryngoscope 113(11):1961–1968
Friedman M, Ibrahim HZ, Vidyasagar J et al (2004) Z-palatoplasty (ZPP): a technique for patients without tonsils. Otolaryngol Head Neck Surg 131:89–100
Friedman M, Ibrahim HZ, Lowenthal S, Vidyasagar J, Joseph NJ (2004) Uvulopalatoplasty (UP2): a modified technique for selected patients. Laryngoscope 114:441–449
Pang KP, Woodson BT (2007) Expansion sphincter pharyngoplasty: a new technique for the treatment of obstructive sleep apnea. Otolaryngol Head Neck Surg 137(1):110–114
Li HY, Lee LA (2009) Relocation pharyngoplasty for obstructive sleep apnea. Laryngoscope 119:2472–2477
Vicini C, Montevecchi F, Pang K, Bahgat A, Dallan I, Frassineti S, Campanini A (2014) Combined transoral robotic tongue base surgery and palate surgery in obstructive sleep apnea–hypopnea syndrome: expansion sphincter pharyngoplasty versus uvulopalatopharyngoplasty. Head Neck 36:77–83
Mantovani M, Minetti A, Torretta S, Pincherle A, Tassone G, Pignataro L (2012) The velo-uvulo-pharyngeal lift or “roman blinds” technique for treatment of snoring: a preliminary report. Acta Otorhinolaryngol Ital 32:48–53
Morgenthaler T, Alessi C, Friedman L et al (2007) Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: an update for 2007. Sleep 30:519–529
Vignatelli L, Plazzi G, Barbato A et al (2003) Italian version of the Epworth sleepiness scale: external validity. Neurol Sci 23:295–300
Chen AY, Frankowski R, Bishop-Leone J et al (2001) The development and validation of a dysphagia-specific quality-of-life questionnaire for patients with head and neck cancer: the M. D. Anderson dysphagia inventory. Arch Otolaryngol Head Neck Surg 127:870–876
Conflict of interest
No.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vicini, C., Hendawy, E., Campanini, A. et al. Barbed reposition pharyngoplasty (BRP) for OSAHS: a feasibility, safety, efficacy and teachability pilot study. “We are on the giant’s shoulders”. Eur Arch Otorhinolaryngol 272, 3065–3070 (2015). https://doi.org/10.1007/s00405-015-3628-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-015-3628-3