Abstract
The aim of this study was to evaluate the change in serum levels of C-reactive protein (CRP) in patients with obstructive sleep apnea (OSA) before and after expansion sphincter pharyngoplasty (ESP) and continuous positive airway pressure (CPAP) treatment. Fifty-one patients with newly diagnosed OSA were prospectively enrolled in this study. We performed ESP in twenty-three patients in the surgery group and twenty-eight patients were included in the CPAP group. Serum levels of high-sensitivity CRP (hs-CRP) were analyzed by enzyme-linked immunosorbent assays before and 3 months after treatment. The relations between CRP and the apnea hypopnea index (AHI), visual analog scale (VAS), the Epworth Sleepiness Scale (ESS), and saturation parameters were evaluated. Both surgical and CPAP treatments caused significant improvements in the clinical and laboratory parameters. However, only the patients whose postoperative AHI levels improved to final AHI of <5 (n = 6) after ESP, had significant decrease in their serum CRP levels (p = 0.028). CPAP group and the rest of the patients in the surgery group did not show statistically significant difference in CRP levels after treatment. We suggest that the successful surgical treatment for OSA—ESP in this study—, which provides OSA cure, can decrease serum levels of CRP and reduce possible cardiovascular morbidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
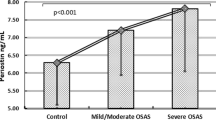
Obstructive sleep apnea (OSA) is an important risk factor for endothelial dysfunction and associated with cardiovascular diseases [1, 2]. Systemic inflammation is one of the main reasons of the cardiovascular morbidity and mortality in patients with OSA [3]. C-reactive protein (CRP) is considered an important indicator of systemic inflammation that can predict many cardiovascular diseases such as myocardial infarction, stroke, coronary heart disease, atherosclerosis, and sudden cardiac death [4]. There are growing published data demonstrating serum CRP levels are independently correlated with the severity of OSA [5–7].
Known since 1930, CRP is, a kind of polypeptide, which consists of five subunits and contains 206 amino acids, encoded by the gene region on the first chromosome [8]. It is synthesized by the liver cells in response to tissue damage, infection and inflammation [9]. CRP not only causes the expression of adhesion molecules from endothelial cells, but also mediates low density lipoprotein (LDL) to be taken in by macrophages. Moreover, it induces monocytes for synthesis of tissue factor, which is a powerful procoagulant substance. It may connect to activated complement. All these effects contribute to endothelial dysfunction [10–12]. There is a reliable evidence that CRP directly reflects the severity of inflammation, thus, some studies have demonstrated more significant findings that CRP may predict cardiovascular risk at the specific serum levels [13, 14]. Besides a strong association was detected between serum CRP levels and cardiovascular disease, patients with OSA had higher CRP levels, were noted [15]. Even in patients with no cardiovascular disease, CRP may show the predicted risk for cardiovascular disease in patients diagnosed with OSA.
In recent decades, the number of studies investigating serum levels of inflammatory markers before and after treatment in patients with OSA has gradually increased. Besides CPAP treatment, the effect of surgical treatment on systemic inflammation in OSA has been also examined previously, however, the number of these studies is poor [16, 17]. In parallel to developments in understanding the inflammation component of OSA, surgical techniques for treatment of OSA have evolved, too. Surgeons have established new ways to find the most successful surgical technique and still continue to try to find a radical solution for treatment of OSA. Expansion sphincter pharyngoplasty (ESP) is one of these new techniques which was first described by Pang and Woodson [18]. Since its introduction 9 years ago, many authors have used and some modified the ESP technique and published their surgical results [19–22]. The recent meta-analysis revealed that the overall success rate of the ESP was 86.3 % and the ESP has been shown to have significantly better clinical and statistical outcome compared to other traditional pharyngoplasty methods of treating OSA [23].
We hypothesized that if an OSA patient undergoes an effective surgical therapy, as confirmed by postoperative polysomnography, then the inflammatory process ought to be interrupted as well. Based on this hypothesis, we aimed to assess the effect of the ESP, which seems an objectively effective and relatively new surgical technique for treatment of OSA, on inflammatory process by evaluating the serum levels of CRP.
Materials and methods
Subjects
Fifty-one patients with newly diagnosed OSA, who had no history of previous OSA surgery or CPAP therapy, were prospectively included in this study. The Ethical Committee of Ankara Kecioren Education and Research Hospital approved the study protocol. All subjects were advised CPAP as a first-line treatment choice. The patients who could not tolerate or were unwilling to use CPAP were evaluated for surgical treatment if suitable and indicated. Only the patients undergoing ESP as a surgical treatment modality were included in the surgery group. All subjects were evaluated with a history review, a detailed otorhinolaryngologic examination, blood tests (liver enzymes, glucose, renal functions, lipid levels, and thyroid functions), electrocardiography, and chest radiography. We excluded the subjects if they had any inflammatory disease, chronic heart disease, pulmonary disease, rheumatological disease, renal disease, diabetes mellitus, hypertension, dyslipidemia, long-term use of medications, history of OSA surgery, central sleep apnea predominance in polysomnography, body mass index (BMI) >35 kg/cm2, and age <18 or >65 years. As clinical indicators of OSA, we used a visual analog scale (VAS) for the evaluation of snoring and the Epworth Sleepiness Scale (ESS) to measure daytime sleepiness symptoms.
Surgical technique
The technique was performed as Pang and Woodson have described [18, 24]. First, a bilateral tonsillectomy was performed if the patient did not have a prior tonsillectomy. The palatopharyngeus muscle was identified; its inferior end was transected horizontally, rotated supero-laterally, isolated inferior to superior direction by monopolar cautery, and left with its superior part attached to the posterior horizontal pharyngeal constrictor muscles. For the rotation of the palatopharyngeus muscle, a tunnel was prepared through an incision made on the anterior surface of soft palate medial to the hamulus. The first suture for attachment of the muscle was a submucosal, horizontal mattress suture, and the second one was a vertical mattress suture to the fibrous tissues. Finally, the anterior and posterior tonsillar pillars were then apposed with vicryl sutures.
Sleep study
The guidelines of the American Academy of Sleep Medicine 2012 was followed when performing and scoring polysomnography (COMET AS40-Plus Amplifier System, Grass Technologies, Astro-Med, Inc. Subsidiary, USA) [25]. Postoperative polysomnography was performed 3 months after surgery in the surgery group. Also, we obtained the 3 months of data recorded during CPAP treatment period to determine PAP compliance in the CPAP group (% days of at least 4 hours in a day). The patients were excluded if they could not present this data for any reason. Besides the apnea hypopnea index (AHI), four important saturation parameters were especially recorded: the lowest oxygen saturation (minO2), the mean oxygen saturation (meanO2), oxygen desaturation index (ODI), and the percentage of sleep time with SaO2 below 90 % (SaO2 <90). The definition of surgical success was defined as: a ≥50 % reduction in AHI to a final AHI of <20, <15, <10, and <5 events/hour [26]. An OSA cure was defined as a postoperative AHI of fewer than 5 events/hour.
High-sensitivity C-reactive protein
Blood samples were taken from the patients two times in 3-months period, between 8 and 9 am in the morning: (1) before the surgery/CPAP treatment at baseline, (2) after the surgery and at the end of the 3-month recording with the PAP device. After blood was collected into tubes and centrifuged at 3000 rpm for 10 minutes, the supernatant serum was separated and then stored at −80 °C in the laboratory until analysis. The levels of CRP were determined by enzyme-linked immunosorbent assays (ELISAs) using the kit Human hs-CRP (DIA Source, Louvain-la-Neuve, Belgium).
Statistical analysis
Statistical analyses were performed using SPSS for Win.Ver.15.0 (SPSS Inc., Chicago, IL., USA). The values were expressed as mean(s) and standard deviation(s) (mean ± SD). The Mann–Whitney U test was used for the comparison of continuous variables between two independent groups and the Wilcoxon test was used for the comparison of continuous variables of dependent groups. Correlations between variables were explored using the Spearman correlation test. Significance was defined as p < 0.05.
Results
The surgery group and the CPAP group consisted of twenty-three patients and twenty-eight patients, respectively. Of the total fifty-one patients, forty-nine were male (96 %) and two were female (4 %). The patients’ ages ranged from 22 to 64 years; the mean ages for the surgery and CPAP groups were 37 ± 9.49 and 46.25 ± 10, respectively. Except the age difference (p = 0.003), no significant difference was found between the two groups in terms of BMI, AHI, ESS scores, VAS scores, serum levels of CRP, and saturation parameters at baseline (all p > 0.05) (Table 1).
The mean AHI values in the surgery group before and after treatment were 32.36 ± 20.94 and 11.79 ± 11.05 events/hour, respectively, and this difference was statistically significant (p < 0.001). The mean AHI values in the CPAP group at baseline and during treatment were 35.75 ± 13.70 and 4.08 ± 3.28, respectively, and the difference was also statistically significant (p < 0.001). The AHI improved to fewer than 5 events/hour in twenty-three patients with CPAP treatment (82.1 %). The mean compliance was 40.9 %. Besides improvements in AHI levels, both surgical and CPAP treatments caused a significant decrease in the ESS scores, VAS scores, ODI, minO2, and SaO2 <90 levels. Also, the surgical treatment significantly decreased the meanO2 levels (p = 0.041). No significant BMI changes were noted after treatment in both groups (Table 2).
The criteria of surgical success, a ≥50 % reduction in AHI to a final AHI of <20, <15, <10, and <5 as described by Kezerian et al. [26], were noted in 16 (69.6 %), 15 (65.2 %), 10 (43.5 %), and 6 (26.1 %) patients, respectively. When the change in serum CRP levels were evaluated according to this criteria, we found that the patients whose AHI levels improved to final AHI of <5 showed a significant decrease in serum CRP levels (p = 0.028). When the success rates were adapted to final AHI of <15, <10 and <5, the “p” values indicating the change of CRP improved in parallel to these, but were not statistically significant except “final AHI <5 form” (Table 3).
The improvement of CRP was somewhat provided by CPAP treatment, but this was not statistically significant (p = 0.151). The change in the ESS scores was positively correlated with the change of serum CRP levels in the CPAP group (r = 0.374, p = 0.049). Also, in the surgery group, the post-treatment serum CRP levels showed a significant correlation with the post-treatment ESS scores (r = 0.588, p = 0.003). The other significant correlations can be seen in the Table 4.
We also divided the groups into two subgroups according to whether BMI > or <28 kg/cm2. Although the change of CRP levels in patients with BMI <28 decreased more than those in BMI >28 in the surgery and CPAP groups, these improvements were not statistically significant (Table 5).
Discussion
In the pathogenesis of cardiovascular complications in OSA, the systemic inflammation is considered as a key factor [3]. This entity is thought to be arisen from intermittent hypoxia that triggers the production of proinflammatory mediators [27]. An important circulating factor of inflammation, CRP, is a valuable predictor for future cardiovascular morbidity [28]. When serum CRP levels were pharmacologically lowered, then cardiovascular risk was reduced, was shown in an interesting study [29]. Many investigators reported increased serum levels of CRP in patients with OSA and severity of OSA has been shown to be associated with CRP levels [5, 6]. However, some researchers did not identify CRP increase in OSA [30, 31]. Although the relationship between CRP and OSA is still controversial, overall evidence from studies shows OSA is associated with increased CRP levels.
In the present study, we aimed to investigate the effect of a relatively new surgical technique, ESP, on serum levels of CRP in patients with OSA. We have used the surgical success criteria as described by Kezerian et al. [26]. Of the total twenty-three patients undergoing this surgery, serum levels of CRP significantly decreased only in the subgroup consisting six patients who well responded to the surgery and had postoperative AHI of <5. However, the surgical treatment (ESP) with the overall success rate of 69.6 % in twenty-three patients did not make significant change in CRP levels. The “p”-values indicating the change of CRP were 0.028, 0.059, and 0.281, when the success criteria adapted for postoperative AHI of <5, <10, and <15, respectively. These statistical results showed that the best successful surgical treatment caused a statistically significant decrease and more successful surgery caused better improvement in serum levels of CRP. We did not observe significant CRP change in the rest of the surgery group and in the CPAP group. However, the compliance of the CPAP group was 40.9 % in this study and compliance with CPAP is an important factor for improving levels of inflammatory markers in patients with OSA [32]. Although the rate of OSA cure in the CPAP group (82.1 %) was higher than that in the surgery group (26.1 %), no significant reduction was observed in serum levels of CRP in the CPAP group. These results support the idea that compliance with CPAP treatment may be more important than improvement of AHI levels to decrease inflammation in OSA. We evaluated the CRP concentrations 3 months after the treatment, but there is no strong evidence about the evaluation time of CRP after treatment. One of the recent studies reported that hs-CRP levels were significantly higher and neurocognitive functions were significantly lower in the moderate to severe OSA group, but these factors improved after 6-months CPAP treatment [33].
Our study results showed that initial levels of CRP and change in serum levels of CRP were not correlated either BMI or BMI change. In addition to this, when we divided the groups into subgroups according to severity of BMI (whether BMI > or <28 kg/cm2), we found that the decrease in CRP levels in patients with BMI <28 was more remarkable than those in BMI >28 in the surgery and CPAP groups, but was not statistically significant. Another point that should be taken into consideration, 3 months of follow-up time is a relatively short time to allow a change in BMI. According to some authors, the increase in serum CRP levels occurs independent of body mass index [5, 34]; in contrast, some defends obesity is the main predisposing factor for CRP increase [31, 35]. A remarkable study on this issue demonstrated that serum CRP levels did not correlate with the severity of OSA, however, only obese-OSA group had increased CRP levels, and CRP was independently associated with obesity [31]. In another study, serum CRP levels in obese patients without OSA was higher than in non-obese patients with OSA [36]. The results from our study support that CRP and BMI are independent variables in patients with OSA. However, these results were obtained from the study population with BMI <35 kg/cm2 and cannot be an objective reflection of obesity. The relationship between obesity and CRP will be again the subject of further studies.
One interesting finding from this study was the positive correlation between the change in the ESS scores and the change of serum CRP levels in the CPAP group. Also, the post-surgical serum CRP levels showed a significant correlation with the post-surgical ESS scores. These results may be incidental, but are important to predict systemic inflammation in patients with OSA by using the Epworth Scale. Forthcoming studies may investigate this possible relationship between CRP and ESS scores with larger study sample.
The surgical success rate of the ESP (69.5 %) can be considered effective but was relatively lower compared to recent meta-analysis. Some of the patients in the surgery group without OSA cure (postoperative AHI >5) may require for additional surgery due to multilevel obstructions. According to the study design, we included the patients undergoing the ESP and evaluated the serum levels of CRP after performing the ESP, but before future surgical procedures. Since we observed a significant CRP change after surgery in the patient subgroup with postoperative AHI of <5, further studies may be designed according to these results because higher success rate is needed to see an improvement in CRP. In addition to this, any other surgical technique for treatment of OSA, not only the ESP, might also make a significant decrease in CRP levels when a surgical treatment is able to provide OSA cure.
The main limitation of this study is the number of patients undergoing ESP. When we assessed the surgery group according to the success criteria described by Kezerian et al., the subgroups were supposed to consist of a relatively lower number of patients. Before the study, no power analysis was performed because the number of subgroups would be defined based on the surgical success. After the surgery, we defined the four subgroups according to postoperative AHI levels as shown in Table 3 and calculated the power. The statistical power was 81.2 % (α of 5 % corresponds to a 95 % confidence interval) when the success criteria adapted for postoperative AHI of <5. This power is also correlated with the “p”-value of 0.028 for six patients in this subgroup that confirms successful surgical treatment caused a statistically significant decrease in serum levels of CRP. Due to the surgical availability, defining the right indication for ESP and inclusion/exclusion criteria, we finally included twenty-three patients in this study in a 2-year period. To provide better power for significance and present exact results of the surgical treatment, further studies with large case series are needed.
Conclusion
More successful outcomes with the ESP significantly decreased serum levels of CRP. In this study, CPAP therapy with a low compliance could not make a significant difference on serum CRP levels. We suggest that the surgical treatment for OSA, which reduces AHI to less than 5 events/hour (OSA cure), may decrease systemic inflammation and reduce future cardiovascular diseases that can be assessed through the serum levels of CRP.
References
Kanbay A, Ceylan E, Inonu Koseoglu H et al (2016) Endocan: a novel predictor of endothelial dysfunction in obstructive sleep apnea syndrome. Clin Respir J. doi:10.1111/crj.12487
Kokturk O, Ciftci TU, Mollarecep E et al (2005) Elevated C-reactive protein levels and increased cardiovascular risk in patients with obstructive sleep apnea syndrome. Int Heart J 46(5):801–809
Ryan S, Taylor CT, McNicholas WT (2009) Systemic inflammation: a key factor in the pathogenesis of cardiovascular complications in obstructive sleep apnoea syndrome? Thorax 64(7):631–636
Bassuk SS, Rifai N, Ridker PM (2004) High-sensitivity C-reactive protein: clinical importance. Curr Probl Cardiol 29(8):439–493
Yokoe T, Minoguchi K, Matsuo H et al (2003) Elevated levels of C-reactive protein and interleukin-6 in patients with obstructive sleep apnea syndrome are decreased by nasal continuous positive airway pressure. Circulation 107(8):1129–1134
Shamsuzzaman AS, Winnicki M, Lanfranchi P et al (2002) Elevated C-reactive protein in patients with obstructive sleep apnea. Circulation 105(21):2462–2464
Nadeem R, Molnar J, Madbouly EM et al (2013) Serum inflammatory markers in obstructive sleep apnea: a meta-analysis. J Clin Sleep Med 9(10):1003–1012
Whitehead AS, Bruns GA, Markham AF et al (1983) Isolation of human C-reactive protein complementary DNA and localization of the gene to chromosome 1. Science 221(4605):69–71
Pepys MB (1981) C-reactive protein fifty years on. Lancet 1(8221):653–657
Blake GJ, Ridker PM (2002) Inflammatory bio-markers and cardiovascular risk prediction. J Intern Med 252(4):283–294
Cleland SJ, Sattar N, Petrie JR et al (2000) Endothelial dysfunction as a possible link between C-reactive protein levels and cardiovascular disease. Clin Sci 98(5):531–535
Fichtlscherer S, Rosenberger G, Walter DH et al (2000) Elevated C-reactive protein levels and impaired endothelial vasoreactivity in patients with coronary artery disease. Circulation 102(9):1000–1006
Ridker PM, Cook N (2004) Clinical usefulness of very high and very low levels of C-reactive protein across the full range of Framingham risk scores. Circulation 109(16):1955–1959
Albert CM, Ma J, Rifai N et al (2002) Prospective study of C-reactive protein, homocysteine, and plasma lipid levels as predictors of sudden cardiac death. Circulation 105(22):2595–2599
Wu H, Yuan X, Wang L et al (2016). The relationship between obstructive sleep apnea hypopnea syndrome and inflammatory markers and quality of life in subjects with acute coronary syndrome. Respir Care (Epub ahead of print)
Kataoka T, Enomoto F, Kim R et al (2004) The effect of surgical treatment of obstructive sleep apnea syndrome on the plasma TNF-alpha levels. Tohoku J Exp Med 204(4):267–272
Constantinidis J, Ereliadis S, Angouridakis N et al (2008) Cytokine changes after surgical treatment of obstructive sleep apnoea syndrome. Eur Arch Otorhinolaryngol 265(10):1275–1279
Pang KP, Woodson BT (2007) Expansion sphincter pharyngoplasty: a new technique for the treatment of obstructive sleep apnea. Otolaryngol Head Neck Surg 137(1):110–114
Sorrenti G, Piccin O (2013) Functional expansion pharyngoplasty in the treatment of obstructive sleep apnea. Laryngoscope 123(11):2905–2908
Vicini C, Montevecchi F, Pang K et al (2014) Combined transoral robotic tongue base surgery and palate surgery in obstructive sleep apnea-hypopnea syndrome: expansion sphincter pharyngoplasty versus uvulopalatopharyngoplasty. Head Neck 36(1):77–83
Ulualp SO (2014) Modified expansion sphincter pharyngoplasty for treatment of children with obstructive sleep apnea. JAMA Otolaryngol Head Neck Surg 140(9):817–822
Carrasco-Llatas M, Marcano-Acuna M, Zerpa-Zerpa V et al (2015) Surgical results of different palate techniques to treat oropharyngeal collapse. Eur Arch Otorhinolaryngol 272(9):2535–2540
Pang KP, Pang EB, Win MT et al (2015) Expansion sphincter pharyngoplasty for the treatment of OSA: a systemic review and meta-analysis. Eur Arch Otorhinolaryngol (Epub ahead of print)
Woodson BT, Karakoc O (2011) The expansion sphincter pharyngoplasty for obstructive sleep apnea. In: Yaremchuk KL, Wardrop PA (eds) Sleep medicine. Plural Publishing, San Diego, pp 301–309
Berry RB, Budhiraja R, Gottlieb DJ et al (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions task force of the American Academy of Sleep Medicine. J Clin Sleep Med 8(5):597–619
Kezirian EJ, Weaver EM, Criswell MA et al (2011) Reporting results of obstructive sleep apnea syndrome surgery trials. Otolaryngol Head Neck Surg 144(4):496–499
Htoo AK, Greenberg H, Tongia S et al (2006) Activation of nuclear factor kappaB in obstructive sleep apnea: a pathway leading to systemic inflammation. Sleep Breath 10(1):43–50
Duchna HW, Orth M, Schultze-Werninghaus G et al (2005) Long-term effects of nasal continuous positive airway pressure on vasodilatory endothelial function in obstructive sleep apnea syndrome. Sleep Breath 9(3):97–103
Ridker PM, Danielson E, Fonseca FA et al (2009) Reduction in C-reactive protein and LDL cholesterol and cardiovascular event rates after initiation of rosuvastatin: a prospective study of the JUPITER trial. Lancet 373(9670):1175–1182
Taheri S, Austin D, Lin L et al (2007) Correlates of serum C-reactive protein (CRP)—no association with sleep duration or sleep disordered breathing. Sleep 30(8):991–996
Ryan S, Nolan GM, Hannigan E et al (2007) Cardiovascular risk markers in obstructive sleep apnoea syndrome and correlation with obesity. Thorax 62(6):509–514
Ishida K, Kato M, Kato Y et al (2009) Appropriate use of nasal continuous positive airway pressure decreases elevated C-reactive protein in patients with obstructive sleep apnea. Chest 136(1):125–129
Wu SQ, Liao QC, Xu XX et al (2016) Effect of CPAP therapy on C-reactive protein and cognitive impairment in patients with obstructive sleep apnea hypopnea syndrome. Sleep Breath (Epub ahead of print)
Punjabi NM, Beamer BA (2007) C-reactive protein is associated with sleep disordered breathing independent of adiposity. Sleep 30(1):29–34
Barcelo A, Barbe F, Llompart E et al (2004) Effects of obesity on C-reactive protein level and metabolic disturbances in male patients with obstructive sleep apnea. Am J Med 117(2):118–121
Sharma SK, Mishra HK, Sharma H et al (2008) Obesity, and not obstructive sleep apnea, is responsible for increased serum hs-CRP levels in patients with sleep-disordered breathing in Delhi. Sleep Med 9(2):149–156
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research is supported by Gulhane Military Medical Academy Research grant (AR-2013/49).
Conflict of interest
Author MURAT BINAR declares that he has no conflict of interest. Author MURAT TIMUR ACAM declares that he has no conflict of interest. Author OMER KARAKOC declares that he has no conflict of interest. Author RAHSAN ILIKCI SAGKAN declares that he has no conflict of interest. Author UGUR MUSABAK declares that he has no conflict of interest. Author MUSTAFA GEREK declares that he has no conflict of interest. None of the authors has any conflict of interest, financial or otherwise.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study. Each of the authors has contributed to, read and approved this manuscript.
Rights and permissions
About this article
Cite this article
Binar, M., Akcam, T., Karakoc, O. et al. A new surgical technique versus an old marker: can expansion sphincter pharyngoplasty reduce C-reactive protein levels in patients with obstructive sleep apnea?. Eur Arch Otorhinolaryngol 274, 829–836 (2017). https://doi.org/10.1007/s00405-016-4290-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-4290-0