Abstract
Objective
The value of salivary gland scintigraphy (SGS) in the evaluation of Sjögren’s syndrome (SS) remains controversial. The aim of this study was to evaluate the diagnostic efficacy of quantitative SGS in patients with xerostomia and to assess the correlation between scintigraphic parameters and pathological features of salivary glands.
Methods
Medical records of 165 patients with xerostomia who underwent [99mTc] pertechnetate SGS and labial biopsy were retrospectively reviewed. The maximum accumulation ratio (MAR), maximum secretion ratio (MSR), and time interval from stimulation to minimum count (Tmin) of the parotid glands were calculated to quantify the glandular activity. Furthermore, pre-stimulatory oral activity index (PRI) and post-stimulatory oral activity index (POI) were calculated to quantify the oral activity.
Results
All parameters except for Tmin were significantly lower in patients with SS than in those without SS. Among the five SGS parameters, PRI showed the highest areas under the curve value (0.9005; p < 0.001), and PRI > 32.75 was associated with a sensitivity of 78.5% and specificity of 86.4% for the diagnosis of SS. A decrease in MAR, MSR, PRI, and POI and an increase in Tmin correlate significantly with the histopathologic grade of labial gland biopsy and disease severity of SS. No significant differences in glandular parameters (MAR, MSR, and Tmin) were found between the non-SS and early-stage SS groups.
Conclusion
Conventional scintigraphic parameters could be used as simple, reliable, and sensitive indicators for the early diagnosis of SS and determination of disease severity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sjögren’s syndrome (SS) is a chronic autoimmune disease characterised by lymphocytic infiltration and destruction of salivary and lacrimal gland tissue, leading to dryness of the main mucosa surface. The primary type is characterised by sicca complex but systemic manifestation such as arthritis, skin vasculitis, and pulmonary, neurological, gastrointestinal, and haematological disorders may also be observed [1]. Regarding the secondary type, sicca symptoms associated with another autoimmune disease, such as systemic lupus erythematosus (SLE), systemic sclerosis, rheumatoid arthritis (RA), or dermatomyositis are observed [2]. SS overwhelmingly affects middle-aged women, and more recent studies have reported an incidence rate of 3–11 cases per 100,000 persons and a prevalence of 0.01–0.72% [3, 4].
While some treatments may improve symptoms and prevent complications of SS, currently there is no cure. The recent development of new therapeutic options for the management of autoimmune diseases has proven to be promising for patients with SS, especially for those with early-stage SS [5]. However, it may be difficult to distinguish the early stage of SS from normal clinical findings. Neither clinical characteristics nor laboratory tests are sufficient for accurate diagnosis [6]. The American–European Consensus Group criteria 2002 (AECC) are widely accepted for the diagnosis of SS [7], and these criteria include subjective ocular and oral symptoms, objective evidence of ocular and salivary gland involvement, demonstration of lymphocyte infiltration on labial salivary biopsy, and presence of antibodies anti-SS-A or anti-SS-B. According to the AECC standard, histopathology of the labial salivary gland, as determined by biopsy, facilitates the most specific and definitive diagnostic method for SS; however, it is invasive and causes some degree of patient discomfort and risk, and it must be performed and interpreted following strict criteria [8, 9]. The objective evidence of salivary gland involvement is another key criterion for the diagnosis of SS. As such, reliable method for detecting impaired salivary function will be of assistance in the diagnosis of SS, especially in the diagnosis of early SS in patients with xerostomia.
Salivary gland scintigraphy (SGS) using [99mTc] pertechnetate is a safe and non-invasive method that provides detailed functional assessment of salivation; it measures the quantity and speed of radionuclide uptake and secretion for the four salivary glands separately [10, 11]. Besides, SGS is not very expensive; it is associated with low radiation exposure and is quite widespread in both high- and low-income countries. Traditional SGS is focused on the quantitative measurements of delayed uptake, reduced concentration, or reduced secretion after provocation with a salivary stimulating agent [11, 12]. These quantitative measurements allow an objective and precise evaluation of salivary involvement in patients with SS [12]. However, conflicting views regarding the diagnostic merits of SGS with regard to SS persist. Various quantitative parameters have been investigated in the past two decades, but no consensus was reached on parameters that accurately indicate impaired parenchymatous function of salivary glands; therefore, determination of the clinical stage of SS have been problematic [13,14,15].
In this study, we retrospectively evaluated a series of semi-quantitative parameters from SGS in patients with xerostomia, and we correlated SGS parameters with histopathologic grades of labial gland biopsy specimens. Unlike previous studies which compared scintigraphic parameters between patients with SS and healthy subjects, the current study compares these parameters within a more relevant group of patients (i.e., patients with xerostomia). The aim of this study was to evaluate the efficiency of SGS in the diagnosis of SS in patients with xerostomia and to assess the relationship between scintigraphic parameters and pathological features of salivary glands. Through this investigation, we would like to identify the most simple, reliable, and sensitive scintigraphic parameters for the diagnosis and determination of the disease severity of SS.
Materials and methods
Patients
This single-centre retrospective study was performed in the First Affiliated Hospital of Xiamen University. Between 2012 and 2018, 174 patients (29 men, 145 women; mean age, 48 years; range 17–76 years) with xerostomia were reviewed in our department of rheumatology. Exclusion criteria were as follows: (1) active hepatitis C injection, (2) acquired immunodeficiency syndrome (AIDS), (3) sarcoidosis, (4) amyloidosis, (5) graft-versus-host disease, (6) IgG4-related disease, and (7) history of head and neck radiation treatment. All patients underwent SGS and labial salivary gland biopsy. Symptom data, results of the Schirmer’s test, and antibody test (anti-SS-A and anti-SS-B) were available for all the patients included. To confirm the diagnosis of primary SS, two experienced rheumatologists applied the AECC [7]. The study was approved by the Clinical Research Ethics Committee of the First Affiliated Hospital of Xiamen University (ID KYZ2017-001) on June 29, 2017. Jiang Jie is the chairperson of the ethics committee. Informed consent was obtained from all the participants. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Salivary gland scintigraphy protocol
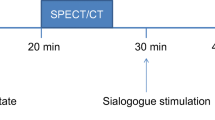
All patients underwent SGS in the department of nuclear medicine according to the same protocol. All subjects were placed in supine position, and their heads were fixed in a slightly extended position using a hemicylindrical plastic head holder with a radiolucent plastic neck-contoured head-rest during imaging. The detector field included the entire salivary gland and part of the thyroid gland. After intravenous administration of 185 MBq [99mTc] sodium pertechnetate ([99mTc]O4-), dynamic SGS was performed with single-photon emission computed tomography (dual detector; BrightView, Philips Medical Systems, Andover, MA, USA) using a low-energy, high-sensitivity, parallel-hole collimator. The images were digitally recorded in a 128 × 128 matrix with a × 2.0 magnification. The energy window around the 140-keV photopeak of 99mTc was 10%. The duration of the scan was 30 min, and the anterior salivary gland images were acquired sequentially (45 s per frame, 40 frames). After 18–20 min of acquisition, salivary gland secretion was stimulated using vitamin C drops (Shuzhong Pharmacy, China), which were administered intraorally (20 mg) avoiding patient’s head movements. We also instructed the patients to minimise swallowing during the examination.
Image analysis
Two experienced nuclear medicine physicians qualitatively assessed the images. Oval-shaped regions of interest (ROIs) were drawn over the oral cavity and parotid glands (on both sides) on a total of 30 frames of summation images of dynamic SGS. Background ROI was placed in the temporal and submental regions near the parotid glands (Fig. 1a). After background subtraction, time-activity curves were generated for each region. The following points were designated on the schematic presentation of the time-activity curve for the salivary glands (Fig. 1b): point A, the initial shoulder, representing a vascular perfusion peak; point B, the maximum activity point before stimulation; and point C: the minimum activity point after stimulation. The following points were designated on the schematic presentation of time-activity curve for the oral activity (Fig. 1c): point X, the initial shoulder, representing a vascular perfusion peak; point Y, the maximum activity point before stimulation; and point Z, the maximum activity point after stimulation. Meanwhile, the counts at points A, B, and C and points X, Y, and Z were shown as a, b, c, x, y, and z, respectively.
a Regions of interest on the salivary gland scintigraphy. Areas 1 and 2 are for parotid glands; area 3 is the background for parotid gland; area 4 is for oral cavity and area 5 is the background for oral cavity. Area numbers are adjacent to each ROI. b Schematic presentation of time-activity curve for glandular activity in normal pattern on salivary gland scintigraphy: point A, the initial shoulder, representing a vascular perfusion peak; point B, the maximum activity point before stimulation; and point C: the minimum activity point after stimulation. c Schematic presentation of time-activity curve for the oral activity: point X, the initial shoulder, representing a vascular perfusion peak; point Y, the maximum activity point before stimulation; and point Z, the maximum activity point after stimulation. Meanwhile, the counts at points A, B, and C and points X, Y, and Z were shown as a, b, c, x, y, and z, respectively
The following glandular parameters were calculated for each salivary gland (Table 1): maximum accumulation ratio (MAR: (b − a) / b × 100%), maximum secretion ratio (MSR: (b − c) / b × 100%), time interval from stimulation to minimum count (time interval between points B and C, Tmin). Mean values of the bilateral glands were used for data analysis. To quantify oral activity, the pre-stimulatory oral activity index (PRI: (y−x) / y × 100%), post-stimulatory oral activity index (POI: (z − x) / z × 100%) were calculated from numerical data obtained from the time-activity curves.
Labial biopsy
Labial salivary gland biopsy was performed no longer than 1 week after SGS. The minor salivary glands of the lower lip were routinely fixed, sectioned, stained with haematoxylin–eosin, and examined for the presence of lymphocytic foci or diffuse lymphocytic infiltration (or both) by an experienced pathologist. The degree of histopathologic change was graded from 0 to 4 according to Chisholm and Mason’s grading standard, and a grade of 1 or higher was considered positive [9, 16] (Table 2).
Statistical analysis
All scintigraphic parameters are expressed as mean ± standard deviation. All statistical analyses were conducted using SPSS 22.0 statistical analysis software (IBM, Armonk, NY, USA). The Mann–Whitney U test was used to analyse all mean values and to compare differences between patients with SS and non-SS. Receiver operating characteristics (ROC) were plotted for the SGS parameters to establish a cut-off value, which was used to determine the sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV) of SGS. Patients with xerostomia were divided into four groups (normal, early-stage, moderate-stage, and advanced-stage SS), and Kruskal–Wallis (to compare all) or Mann–Whitney U test (to compare any two of the four groups) were applied to analyse the scintigraphic parameters among the four groups. All tests were two-sided, and a p value of < 0.05 was considered statistically significant.
Results
Participants
Initially, 174 patients with xerostomia were included in this study. All of them underwent both SGS and labial biopsy. Nine patients were excluded because of equivocal biopsy, inadequate biopsy material, or absence of Schirmer’s test. Data of the remaining 165 patients (29 men, 136 women; mean age, 46 years; range, 17–72 years) were included for further analysis. Besides the mouth symptoms in all patients, ocular symptoms were recorded in 116 patients, positivity of Schirmer’s test was observed in 81 patients, lymphocytic infiltration on labial salivary gland biopsy (pathological grade ≥ 1 according to Chisholm and Mason’s standard) was observed in 119 patients, and presence of autoantibodies were observed in 66 patients. On the basis of the AECC standard, 121 patients could be classified as SS positive and 44 patients as SS negative.
Pattern of time-activity curves
Visual evaluation of time-activity curves revealed a reciprocal relation between glandular and oral activities (Fig. 2). Parotid gland curve shows an early slow-rising uptake followed by a sharp-declining uptake after stimulation (Fig. 2a), whereas oral cavity curve shows an early slow-rising uptake followed by a fast-rising uptake after stimulation (Fig. 2b). Before stimulation, obvious reciprocal parotid uptake and oral activities were observed in 44 of 121 patients with SS (36.4%) and 34 of 44 patients with non-SS (77.3%). Meanwhile, 41 of 121 patients with SS (33.9%) and 42 of 44 patients with non-SS (95.5%) showed an obvious response to vitamin C stimulation.
Time-activity curves of parotid glands and oral cavity in a 56-year-old healthy man. a Parotid gland curve shows an early slow-rising uptake followed by a sharp-declining uptake after stimulation. b Oral cavity curve shows an early slow-rising uptake followed by a fast-rising uptake after stimulation. Arrow marks Vitamin C drop stimulation point
Diagnostic efficacy of scintigraphic parameters for SS in patients with xerostomia
The three scintigraphic parameters for the salivary glands in patients with SS and non-SS are presented using box plots in Fig. 3. As shown in Fig. 3a, b, both MAR and MSR were significantly lower in patients with SS than in patients with non-SS, whereas the Tmin in patients with SS was significantly longer than that in patients with non-SS (Fig. 3c). Regarding the overall oral activity, both PRI and POI were significantly lower in patients with SS than in patients with non-SS (Fig. 3d, e). Overall, all five scintigraphic parameters differed significantly between patients with SS and patients with non-SS, and the most discriminative cut-off value of each parameter was determined using ROC methodology which optimised the sensitivity and specificity to obtain the highest accuracy. As presented in Fig. 3f, the area under the curve (AUC) values differed significantly from 0.5 and were higher than 0.7 for all parameters. Among the five parameters from SGS, PRI showed the highest AUC value (0.9005; p < 0.001), and PRI > 32.75 were associated with a sensitivity of 78.5% and specificity of 86.4% for determining SS; POI was the most sensitive diagnostic parameter, with the optimal cut-off value of 53.5 (AUC, 0.8399; p < 0.001), and the sensitivity, specificity, PPV, and NPV for POI were 90.1%, 68.2%, 88.6%, and 71.4%, respectively; MSR showed the most specific diagnostic value, and MSR values of over 47.5 were associated with the diagnosis of SS (AUC, 0.8607; p < 0.001), with a sensitivity of 63.6%, specificity of 97.7%, PPV of 98.7%, and NPV of 49.4%. The diagnostic efficacies of all five parameters on SGS have been summarised in Table 3.
Comparing of scintigraphic parameters between patients with SS and without SS. a Maximum accumulation ratio (MAR) was significantly lower in patients with SS. b Maximum secretion ratio (MSR) was significantly lower in patients with SS. c Time interval from stimulation to minimum count (Tmin) was significantly higher in patients with SS. d Prestimulatory oral activity index (PRI) was significantly lower in patients with SS. e Poststimulatory oral activity index (POI) was significantly lower in patients with SS. f Receiver operating characteristic (ROC) curves of all scintigraphic parameters in the diagnosis of SS among patients with xerostomia (SS, Sjögren’s syndrome)
Scintigraphic parameters for determination of the severity of Sjögren’s syndrome
Among the 44 patients with non-SS, 30 showed negative histological results (grade = 0); 105 of patients with SS showed positive histological results (grade ≥ 1). To evaluate the correlation between the scintigraphic parameters and pathological features of salivary glands, the 105 patients with SS were further classified into three groups according to the pathologic grading of the labial biopsy: 30 patients with early-stage SS (grade 1–2), 39 patients with moderate-stage SS (grade 3), and 36 patients with advanced-stage SS (stage 4). Time-radioactivity curves from the parotid gland and the oral cavity for the three groups are shown in Fig. 4a, b.
a Time-radioactivity curves from the parotid gland for the three groups of patients with early-stage (a), moderate-stage (b) and advanced-stage (c) SS, respectively. b Time-radioactivity curves from oral cavity for the three groups of patients with early-stage (a), moderate-stage (b) and advanced-stage (c) SS, respectively. Arrow marks Vitamin C drop stimulation point (SS, Sjögren’s syndrome)
Comparisons of scintigraphic parameters among the three groups are presented in Fig. 5. Except the Tmin value, which increased significantly, all scintigraphic parameters decreased significantly with the progression of SS stage. Additionally, with regard to the parotids, MAR, MSR, PRI, and POI were significantly lower and Tmin was significantly higher in the early-stage SS group than in the advanced-stage SS group. Furthermore, all scintigraphic parameters showed significant differences between patients with moderate-stage and advanced-stage SS.
Overall analysis of comparisons among all scintigraphic parameters in patients with early-, moderate- and advanced-stage SS. a Maximum accumulation ratio (MAR) decreased significantly with the progression of SS stage. b Maximum secretion ratio (MSR) decreased significantly with the progression of SS stage. c Time interval from stimulation to minimum count (Tmin) increased significantly with the progression of SS stage. d Prestimulatory oral activity index (PRI) decreased significantly with the progression of SS stage. e Poststimulatory oral activity index (POI) decreased significantly with the progression of SS stage (SS, Sjögren’s syndrome)
Scintigraphic parameters of the three groups of patients with SS were further compared with those of the 30 patients with non-SS (with negative histological results), as summarised in Table 4. Similar to the previous results, a decrease in MAR, MSR, PRI and POI and an increase in Tmin could also be observed in the four groups with the disease stage progression. Regarding each of the five parameters, significant differences among the four groups were observed via Kruskal–Wallis analysis. Specifically, all scintigraphic parameters the non-SS group were significantly different from those of either the moderate- or advanced-stage SS group. However, no significant differences with respect to the glandular parameters MAR (70.8 ± 3.9 vs. 67.0 ± 3.3, p = 0.719), MSR (64.7 ± 3.8 vs. 60.6 ± 3.0, p = 0.164), and Tmin (3.1 ± 0.7 vs. 3.9 ± 0.5, p = 0.322) were observed between the non-SS and early-stage SS group.
Discussion
SS is considered to be a chronic autoimmune disease characterised by diffuse lymphoid cell infiltration into the salivary and lacrimal glands, and xerostomia may occur as the most common symptom in patients with SS [5]. However, it may be difficult to distinguish the early stage of SS from normal clinical findings. Planar SGS is a relatively easy and non-invasive method used to explore the salivary gland function, and attempts have been made to use it as a substitute for labial salivary gland biopsy for the diagnosis of SS [17, 18]. In the past two decade, a wide variety of quantification methods were applied in SGS for the diagnosis of SS [19,20,21]. However, some scholars expressed concerns about the use of SGS as the first-line tool in the patients with suspected SS [17, 22], and there has been uncertainty as to which of the scintigraphic parameters are most useful diagnostically [23,24,25]. Therefore, the value of SGS in the diagnosis of SS among patients with xerostomia remains controversial, and very few quantitative SGS studies have been reported to date.
In this retrospective study, we investigated the quantitative parameters (MAR, MSR, PRI, POI) derived from salivary glandular and oral radioactivity for assessing the diagnostic efficacy of SGS in patients with xerostomia. The results of our study indicated that all scintigraphic parameters except for Tmin were significantly lower in patients with SS than in those with non-SS, which are consistent with the results from the previous studies [20, 26, 27]. However, these previous studies compared patients with SS to healthy control subjects, which does not fit with the target population usually considered for the diagnosis of SS in the routine clinical practice, and it cannot, therefore, be concluded whether the discrepancies observed were related to xerostomia or were specific to patients with SS. To address this shortcoming, our work points out the key role of SGS in the group of patients affected with xerostomia.
To identify the most useful scintigraphic parameter for the diagnosis of SS among patients with xerostomia, we determined the diagnostic efficacy of these parameters via ROC analysis and subsequently established a threshold that could assist the diagnosis of SS in patients with xerostomia. As a matter of fact, very few of the previous studies that we found in the literature used as many quantitative parameters as we did and compared the diagnostic efficacy of different parameters in patients with SS. Interestingly, the oral activity index PRI showed the highest AUC value (AUC = 0.9005, p < 0.0001) among all parameters, suggesting that PRI may be a more useful SGS parameter than the others. Patients with a PRI greater than 32.75, who were assigned to the negative group, were associated with a sensitivity of 78.5%, the specificity of 86.4%, PPV of 85.6%, and NPV of 59.4% for the determination of SS among patients with xerostomia. Regarding the remaining four scintigraphic parameters, POI > 53.5 showed a higher sensitivity of 90.1% (AUC = 0.8399, p < 0.0001) while MSR > 47.5 showed a higher specificity of 97.7% (AUC = 0.8607, p < 0.0001) than that of PRI, which suggested that the three scintigraphic parameters PRI, POI, and MSR play complementary roles in the diagnosis of SS among patients with xerostomia.
To further evaluate the correlation between the scintigraphic parameters and pathological features of salivary glands, the overall analysis of comparisons among all quantitative glandular and oral parameters was conducted in patients with SS who showed positive histological results (grade ≥ 1). The results demonstrated that a decrease in MAR, MSR, PRI, and POI and an increase in Tmin correlate significantly with the histopathologic grade of labial gland biopsy and disease severity of SS. Comparisons of scintigraphic parameters and overall analysis revealed that the three groups of patients (early-stage, moderate-stage, and advanced-stage SS) could be clearly distinguished by decreased MAR, MSR, PRI, and POI and increased Tmin. Moreover, when the patients with non-SS (patients who showed negative histological results, grade = 0) were analysed together with the three SS groups, the decreasing trend in MAR, MSR, PRI, and POI and an increasing trend in Tmin could still be observed in the four groups with an increase in the disease severity. However, no significant differences regarding glandular parameters (MAR, MSR, and Tmin) were found between the non-SS group and the early-stage SS group (grade 1–2), whereas the decrease in oral activity indices (PRI and POI) was statistically significant when the non-SS group was compared to the early-stage SS group. This indicated that the decrease in glandular parameters may be less helpful in the early diagnosis and evaluation of the severity of glandular involvement, reduction of oral activity may be more relevant to salivary gland function and plays an important role in disease stage identification. Since the oral activity mainly comes from the spontaneous secretion of the salivary glands, we could speculate that decrease in spontaneous secretion function of the salivary gland was the main indication of SS in the early stage and that will allow the diagnosis of early form of SS when pathological features of salivary gland are not already present. Therefore, we extended our observation to include that the conventional scintigraphic parameters, especially the oral activity indices PRI and POI, which could be used as simple, reliable, and sensitive indicators to determine the early diagnosis and distinguish the disease severity of SS. Overall, quantitative SGS is a valuable tool in the diagnostic management of patients with xerostomia. This method is straightforward and can be implemented in any nuclear medicine department; it is worth gaining experience in this underused nuclear medicine technology. Future studies are necessary to harmonise the rules for the preparation of patients and acquisition protocol and to optimise quantification parameters and normal values.
A limitation of this study is that the time-activity curve analysis from submandibular glands was not performed, due to following considerations: The submandibular glands are sometimes not well visualized and are easily affected by the oral activity (especially after the Vitamin C stimulation). This is because the unstimulated spontaneous secretion mainly comes from the submandibular glands and less frequently from the parotid glands [28]. As a result, the parotid glands normally exhibit a higher 99mTc-pertechnetate uptake than the submandibular glands do. In order for representing the salivary gland function, it may be more reliable and accurate to analyze the time-activity curves from parotid glands than those from submandibular glands. However, we noticed that the quantitative analysis from submandibular glands are still performed in many other studies, adding of analysis of parameters of the submandibular salivary gland in our further investigations may be more meaningful and insightful.
Conclusion
The straightforward quantitative analysis of SGS carried out in this study could be used for early diagnosis, disease severity determination, and therapy response monitoring in patients with SS.
References
Ramos-Casals M, Brito-Zeron P, Siso-Almirall A, Bosch X. Primary Sjogren syndrome. BMJ. 2012;344:e3821.
Gonzalez LA, Toloza SM, McGwin G Jr, Alarcon GS. Ethnicity in systemic lupus erythematosus (SLE): its influence on susceptibility and outcomes. Lupus. 2013;22(12):1214–24.
Maldini C, Seror R, Fain O, Dhote R, Amoura Z, De Bandt M, et al. Epidemiology of primary Sjogren’s syndrome in a French multiracial/multiethnic area. Arthritis Care Res (Hoboken). 2014;66(3):454–63.
Qin B, Wang J, Yang Z, Yang M, Ma N, Huang F, et al. Epidemiology of primary Sjogren’s syndrome: a systematic review and meta-analysis. Ann Rheum Dis. 2015;74(11):1983–9.
Brito-Zeron P, Acar-Denizli N, Zeher M, Rasmussen A, Seror R, Theander E, et al. Influence of geolocation and ethnicity on the phenotypic expression of primary Sjogren’s syndrome at diagnosis in 8310 patients: a cross-sectional study from the Big Data Sjogren Project Consortium. Ann Rheum Dis. 2017;76(6):1042–50.
Shiboski CH, Shiboski SC, Seror R, Criswell LA, Labetoulle M, Lietman TM, et al. 2016 American College of Rheumatology/European League Against Rheumatism classification criteria for primary Sjogren’s syndrome: a consensus and data-driven methodology involving three international patient cohorts. Ann Rheum Dis. 2017;76(1):9–16.
Shiboski CH, Shiboski SC, Seror R, Criswell LA, Labetoulle M, Lietman TM, et al. 2016 American College of Rheumatology/European League Against Rheumatism Classification Criteria for Primary Sjogren’s Syndrome: a consensus and data-driven methodology involving three international patient cohorts. Arthritis Rheumatol. 2017;69(1):35–45.
Vitali C, Moutsopoulos HM, Bombardieri S. The European Community Study Group on diagnostic criteria for Sjogren’s syndrome. Sensitivity and specificity of tests for ocular and oral involvement in Sjogren’s syndrome. Ann Rheum Dis. 1994;53(10):637–47.
Chisholm DM, Mason DK. Labial salivary gland biopsy in Sjogren’s disease. J Clin Pathol. 1968;21(5):656–60.
Nishiyama S, Miyawaki S, Yoshinaga Y. A study to standardize quantitative evaluation of parotid gland scintigraphy in patients with Sjogren’s syndrome. J Rheumatol. 2006;33(12):2470–4.
Klutmann S, Bohuslavizki KH, Kroger S, Bleckmann C, Brenner W, Mester J, et al. Quantitative salivary gland scintigraphy. J Nucl Med Technol. 1999;27(1):20–6.
Umehara I, Yamada I, Murata Y, Takahashi Y, Okada N, Shibuya H. Quantitative evaluation of salivary gland scintigraphy in Sjorgen’s syndrome. J Nucl Med. 1999;40(1):64–9.
Xue L, Sun P, Ou D, Chen P, Chen M, Yan B. Diagnosis of pathological minor salivary glands in primary Sjogren’s syndrome by using Raman spectroscopy. Lasers Med Sci. 2014;29(2):723–8.
Vivino FB, Hermann GA. Role of nuclear scintigraphy in the characterization and management of the salivary component of Sjogren’s syndrome. Rheum Dis Clin North Am. 2008;34(4):973–986 ix.
Vinagre F, Santos A, Santos M, Prata A, Oliveira A, Silva JC. Salivary gland scintigraphy in the evaluation of patients with sicca complaints. Acta Reumatol Port. 2008;33(4):422–8.
Carubbi F, Alunno A, Cipriani P, Bartoloni E, Baldini C, Quartuccio L, et al. A retrospective, multicenter study evaluating the prognostic value of minor salivary gland histology in a large cohort of patients with primary Sjogren’s syndrome. Lupus. 2015;24(3):315–20.
Kim HA, Yoon SH, Yoon JK, Lee SJ, Jo KS, Lee DH, et al. Salivary gland scintigraphy in Sjogren’s syndrome. Comparison of the diagnostic performance of visual and semiquantitative analysis. Nuklearmedizin. 2014;53(4):139–45.
Geitung JT, Jonsson MV. Imaging Technology in Sjögren’s Syndrome: non-invasive evaluation of the salivary glands. In: Fox IR, Fox MC, editors. Sjögren’s Syndrome: Practical Guidelines to Diagnosis and Therapy. New York: Springer; 2012. p. 83–89.
Loy F, Diana M, Isola R, Solinas P, Isola M, Conti G, et al. Morphological evidence that pentagastrin regulates secretion in the human parotid gland. J Anat. 2012;220(5):447–53.
Zou Q, Jiao J, Zou MH, Xu JH, Pan YF, Chen JN, et al. Semi-quantitative evaluation of salivary gland function in Sjogren’s syndrome using salivary gland scintigraphy. Clin Rheumatol. 2012;31(12):1699–705.
Shizukuishi K, Nagaoka S, Kinno Y, Saito M, Takahashi N, Kawamoto M, et al. Scoring analysis of salivary gland scintigraphy in patients with Sjogren’s syndrome. Ann Nucl Med. 2003;17(8):627–31.
Adams BK, Al Attia HM, Parkar S. Salivary gland scintigraphy in Sjogren’s syndrome: are quantitative indices the answer? Nucl Med Commun. 2003;24(9):1011–6.
Angusti T, Pilati E, Parente A, Carignola R, Manfredi M, Cauda S, et al. Semi-quantitative analysis of salivary gland scintigraphy in Sjogren’s syndrome diagnosis: a first-line tool. Clin Oral Investig. 2017;21(7):2389–95.
Nadal M, Levy M, Bakhsh A, Joly A, Maruani A, Vaillant L, et al. Salivary scintigraphy for Sjogren’s syndrome in patients with xerostomia: a retrospective study. Oral Dis. 2018;24(4):552–60.
Kaldeway HP, Ter Borg EJ, van de Garde EMW, Habraken JBA, van Buul MMC. Validation of quantitative salivary gland scintigraphy in relation to the American-European concensus criteria for Sjogren’s syndrome. Nucl Med Commun. 2019;40(4):343–8.
Gune S, Yilmaz S, Karalezli A, Aktas A. Quantitative and visual evaluation of salivary and thyroid glands in patients with primary Sjogren’s syndrome using salivary gland scintigraphy: relationship with clinicopathological features of salivary, lacrimal and thyroid glands. Nucl Med Commun. 2010;31(7):666–72.
Aung W, Murata Y, Ishida R, Takahashi Y, Okada N, Shibuya H. Study of quantitative oral radioactivity in salivary gland scintigraphy and determination of the clinical stage of Sjogren’s syndrome. J Nucl Med. 2001;42(1):38–433.
Hermann GA, Vivino FB, Shnier D, Krumm RP, Mayrin V, Shore JB. Variability of quantitative scintigraphic salivary indices in normal subjects. J Nucl Med. 1998;39(7):1260–3.
Funding
This study was supported by the National Natural Science Foundation of China (Grant number 81701736) and Fujian Middle-aged Backbone Talents Program (2017-ZQN-82).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest in this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, J., Wu, J., Zhao, L. et al. Quantitative evaluation of salivary gland scintigraphy in Sjögren’s syndrome: comparison of diagnostic efficacy and relationship with pathological features of the salivary glands. Ann Nucl Med 34, 289–298 (2020). https://doi.org/10.1007/s12149-020-01448-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-020-01448-9