Abstract
Objectives
The aim of this study was to investigate of salivary gland dysfunction with single-photon emission computed tomography/computed tomography (SPECT/CT), especially the relationship between maximum standardized uptake value (SUVmax) of salivary glands and their dysfunction.
Methods
Five patients (2 submandibular sialolithiasis, 2 Sjögren's syndrome, and 1 parotitis) who underwent SPECT/CT were included in this study. The salivary gland excretion function was defined as A (pre-stimulatory 20 min after injection of Tc-99m pertechnetate)/B (post-stimulatory 40 min after injection of Tc-99m pertechnetate) using SUVmax of parotid and submandibular glands.
Results
SUVmax before stimulation of the submandibular gland with sialoliths in a patient was lower than that in the opposite submandibular gland without sialoliths (5.81 vs 51.37). Furthermore, the A/B using SUVmax in the other patient of submandibular glands with sialoliths was lower than that in the opposite submandibular glands without sialoliths (0.70 vs 1.85). The A/B using SUVmax of right and left parotid gland in a patient with Sjögren's syndrome was 1.06 and 0.74, respectively. Furthermore, the A/B using SUVmax of right and left parotid glands in the other patient with Sjögren's syndrome was 3.20 and 4.32, respectively. The A/B using SUVmax of right and left parotid glands in a patient with left parotitis was 2.26 and 1.58, respectively.
Conclusion
The results of the present study indicate that SUVmax using SPECT/CT seems a useful tool for evaluation of the salivary gland dysfunction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sialolithiasis is one of the most prevalent large obstructive disorders of the major salivary glands [1]. The submandibular gland is the most frequently involved [2]. The main clinical features are pain and swelling associated with eating and subsequent sialoadenitis [3].
Sjögren's syndrome is a chronic, progressive, autoimmune disease, of unknown aetiology, characterized by focal lymphocytic infiltration of exocrine glands with a significant functional impairment, leading to Sicca symptoms, such as the salivary and lachrymal glands, resulting in dry mouth and dry eyes [4].
Different physical and chemical examinations, including ultrasonography, sialography, computed tomography (CT), and magnetic resonance (MR) imaging, are commonly used to diagnose various salivary gland diseases [5]. 99mTc-pertechnetate salivary gland scintigraphy is useful for the diagnosis of diseases that affect the salivary glands through the use of radionuclide-labeled compounds. This easy, noninvasive, and accurate method assesses the functional state and degree of injury to the gland, resulting in highly valuable clinical information [6]. Furthermore, we indicated the relationship between CT value of submandibular gland with/without sialolithiasis and salivary gland excretion using salivary gland scintigraphy [7].
In recent years, thanks to the development of tomographic imaging with a three-dimensional image reconstruction algorithm, planar nuclear imaging has evolved to single-photon emission computed tomography (SPECT). Integration of SPECT with CT, producing a hybrid scanner of SPECT/CT, was the next step, following the successful clinical application of positron emission tomography (PET)/CT [8]. These scanners provide fusion images of CT and SPECT and also produce attenuation correction maps that are necessary for quantitative analyses using the standardized uptake value (SUV). SUV is defined as the tissue concentration of tracer as measured by a scanner divided by the activity injected divided usually by body weight [9]. Quantitative salivary gland SPECT/CT holds promise as an objective imaging modality for assessment of salivary dysfunction [10]. However, to the best of our knowledge, the relationship between SUV of salivary glands and their dysfunction has not been reported in the literature. The aim of this study was to investigate of salivary gland dysfunction with SPECT/CT, especially the relationship between maximum SUV (SUVmax) of salivary glands and their dysfunction.
Materials and methods
Patient population
This study was approved by the ethics committee of our institution (ECNG-R-280). After providing written informed consent, 5 patients (3 male, 2 female; age 23–79 years, mean age 59.8 years; 2 submandibular sialolithiasis, 2 Sjögren's syndrome, and 1 parotitis) underwent SPECT/CT at our university hospital from November 2018 to January 2019.
Image acquisition
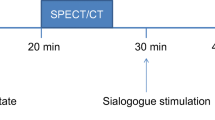
The radiopharmaceutical used in this study was 99mTc-pertechnetate (Technescinti, Nihon Medi-Physics, Tokyo, Japan). Serial salivary gland images were obtained with a dual-head gamma camera (Optima NM/CT 640, GE Healthcare Japan, Tokyo, Japan) using a low-energy, high-resolution collimator, and the 140 keV photo energy peak for 99mTc. Each patient was administered the agent at 370 MBq with a rapid intravenous injection. Anterior sequential salivary gland images were obtained with a 256 × 256 matrix of 2.1 mm pixel size, at 20 s per frame for 20 min. Twenty minutes after the injection, SPECT scans were acquired using a 128 × 128 matrix of 4.2 mm pixel size, and a total of 60 projections (30 stops) over 360° with a dwell time of 10 s/stop. Subsequent to the SPECT acquisition, a low-dose CT scan was acquired with 120 kV, 20 mA, and a 512 × 512 matrix. Furthermore, serial salivary gland images were obtained at 20 s frames for 10 min. At the 40 min, we added 0.5 mL citric acid as an oral salivary stimulant. Finally, the second SPECT scans and the second CT scan were acquired.
Image analysis
To calculate the SUV, the SPECT/CT system had been first calibrated to the dose calibrator for determination of the system sensitivity, the converting factor for radioactivity from measured counts. SUV in a given volume of interest (VOI) was indirectly calculated from the percentage injected dose, which was obtained using the dosimetry software (Q. Metrix; GE Healthcare Japan). To derive percentage injected dose in a certain VOI using the dosimetry software, we entered the following information into the software in advance: the pre-injection radioactivity in the syringe and the measurement time, the post-injection residual radioactivity in the syringe and the measurement time, the time of injection to the patient, body weight, and the system sensitivity. On a dedicated workstation (GEniE Xeleris; GE Healthcare Japan), CT, SPECT, and SPECT/CT images were displayed with the dosimetry software. Using the transaxial and coronal CT images as the anatomic reference, a VOI was drawn over the parotid and submandibular glands, which was automatically reflected on the SPECT/CT fusion images. Then, the dosimetry software provided multiple quantitative data for a given VOI. The mean SUV (SUVmean) in a given VOI was calculated as follows: SUVmean = (total radioactivity/VOI volume)/(injected radioactivity/body weight). The maximum SUV (SUVmax) in a given VOI was calculated as follows: SUVmax = (maximum radioactivity/voxel volume)/(injected radioactivity/body weight). The salivary gland excretion function was defined as A (pre-stimulatory 20 min after injection of Tc-99m pertechnetate)/B (post-stimulatory 40 min after injection of Tc-99m pertechnetate) using SUVmax of parotid and submandibular glands. The SPECT/CT parameters SUVmax were compared for the parotid and submandibular glands.
Results
Table 1 shows SPECT/CT SUVmax in the parotid and submandibular glands. SUVmax before stimulation of the submandibular gland with sialoliths in a patient (Case 2, Fig. 1) was lower than that in the opposite submandibular gland without sialoliths (5.81 vs 51.37). Furthermore, the A/B using SUVmax in the same patient of submandibular glands with sialoliths was lower than that in the opposite submandibular glands without sialoliths (1.55 vs 2.96).
SUVmax before stimulation of the submandibular gland with sialoliths in the other patient of submandibular glands with sialoliths (Case 1) was higher than that in the opposite submandibular gland without sialoliths (23.32 vs 20.28). However, the A/B using SUVmax in the same patient of submandibular glands with sialoliths was lower than that in the opposite submandibular glands without sialoliths (0.70 vs 1.85).
The A/B using SUVmax of right and left parotid glands in a patient with Sjögren's syndrome (Case 3) was 1.06 and 0.74, respectively. Furthermore, The A/B using SUVmax of right and left parotid glands in the other patient with Sjögren's syndrome (Case 4) was 3.20 and 4.32, respectively. The A/B using SUVmax of right and left parotid glands in a patient with left parotitis (Case 5) was 2.26 and 1.58, respectively.
Discussion
Sialolithiasis is diagnosed using clinically and radiographically methods [11]. 99mTc-pertechnetate salivary gland scintigraphy is useful for the diagnosis of diseases that affect the salivary glands, such as noninvasive and accurate method assesses the functional state and degree of injury to the gland. Wu et al. [6] indicated that uptake and excretion by the glands were substantially decreased in patients with sialolithiasis. Ogura et al. [7] showed that the A [before stimulation test (counts/frame)]/B [after stimulation test (counts/frame)] of submandibular gland with sialoliths (1.09 ± 0.23) was lower than that of submandibular gland without sialoliths (1.99 ± 0.57, P = 0.000). Furthermore, Chen et al. [12] established a point-scoring diagnostic system for Sjögren's syndrome based on quantified SPECT imaging of salivary gland.
Despite the wide array of clinical applications in many fields of nuclear medicine, SPECT/CT has been considered not quantitative but qualitative, because there have been no reports regarding the proven clinical utility of quantitative SPECT/CT [8]. Kim et al. [10] evaluated the salivary gland dysfunction in Sjögren's syndrome patients using quantitative salivary SPECT/CT data, such as % parotid uptake, % submandibular uptake, % parotid excretion, and % submandibular excretion. SPECT/CT scanners provide fusion images of CT and SPECT and also produce attenuation correction maps that are necessary for quantitative analyses using the SUV. However, the quantitative information from the SPECT/CT, such as SUV, has not been well investigated in any disease model yet. Araz et al. [13] showed that SUVmax of the hyperfunctioning parathyroid gland seems to be predictive of disease severity in terms of serum parathormone and bone mineral densitometry results. We evaluated the salivary gland dysfunction in sialolithiasis patients using the SUVmax. In this study, SUVmax before stimulation of the submandibular gland with sialoliths was lower than that in the opposite submandibular gland without sialoliths (5.81 vs 51.37). Furthermore, the A/B in the other patient of submandibular glands with sialoliths was lower than that in the opposite submandibular glands without sialoliths (0.70 vs 1.85). We consider that sialoliths is a factor of salivary gland excretion in the submandibular gland.
Regarding Sjögren's syndrome, Ogura et al. [4] showed the relationship between MR sialographic stages and salivary gland excretion in patients with Sjögren's syndrome. In this study, the A/B using SUVmax of right and left parotid glands in a patient with Sjögren's syndrome was 1.06 and 0.74, respectively. Furthermore, The A/B using SUVmax of right and left parotid glands in the other patient with Sjögren's syndrome was 3.20 and 4.32, respectively. We consider that the A/B using SUVmax of parotid gland with Sjögren's syndrome can evaluate stages of Sjögren's syndrome.
The limitations of this study were as follows: the number of patients with SPECT/CT was too small and logistic multivariate regression analysis was not used to determine the relationship between SUVmax of salivary glands and their excretion function. Therefore, further research is necessary to validate these results.
Conclusions
The aim of this study was to investigate of salivary gland dysfunction with SPECT/CT, especially the relationship between SUVmax of salivary glands and their dysfunction. The results of the present study indicate that SUVmax using SPECT/CT seems a useful tool for evaluation of the salivary gland dysfunction.
References
Kim JH, Aoki EM, Cortes AR, Abdala-Junior R, Asaumi J, Arita ES. Comparison of the diagnostic performance of panoramic and occlusal radiographs in detecting submandibular sialoliths. Imaging Sci Dent. 2016;46:87–92.
Lustmann J, Regev E, Melamed Y. Sialolithiasis. A survey on 245 patients and a review of the literature. Int J Oral Maxillofac Surg. 1990;19:135–8.
Schwarz D, Kabbasch C, Scheer M, Mikolajczak S, Beutner D, Luers JC. Comparative analysis of sialendoscopy, sonography, and CBCT in the detection of sialolithiasis. Laryngoscope. 2015;125:1098–101.
Ogura I, Sasaki Y, Oda T, Sue M, Hayama K. Magnetic resonance sialography and salivary gland scintigraphy of parotid glands in Sjögren's syndrome. Chin J Dent Res. 2018;21:63–8.
Gulati A, Scott J, Blythe JN, Southorn B, Brennan PA. Review of salivary papers published in the British Journal of Oral and Maxillofacial Surgery during 2009–2010. Br J Oral Maxillofac Surg. 2011;49:627–9.
Wu CB, Xi H, Zhou Q, Zhang LM. The diagnostic value of technetium 99m pertechnetate salivary gland scintigraphy in patients with certain salivary gland diseases. J Oral Maxillofac Surg. 2015;73:443–50.
Ogura I, Hayama K, Sue M, Oda T, Sasaki Y. Submandibular sialolithiasis with CT and scintigraphy: CT values and salivary gland excretion in the submandibular glands. Imaging Sci Dent. 2017;47:227–31.
Suh MS, Lee WW, Kim YK, Yun PY, Kim SE. Maximum standardized uptake value of 99mTc hydroxymethylene diphosphonate SPECT/CT for the evaluation of temporomandibular joint disorder. Radiology. 2016;280:890–6.
Kaneta T, Ogawa M, Daisaki H, Nawata S, Yoshida K, Inoue T. SUV measurement of normal vertebrae using SPECT/CT with Tc-99m methylene diphosphonate. Am J Nucl Med Mol Imaging. 2016;22:262–8.
Kim J, Lee H, Lee H, Bang JI, Kang YK, Bae S, et al. Quantitative single-photon emission computed tomography/computed tomography for evaluation of salivary gland dysfunction in Sjögren's syndrome patients. Nucl Med Mol Imaging. 2018;52:368–76.
Jardim EC, Ponzoni D, de Carvalho PS, Demetrio MR, Aranega AM. Sialolithiasis of the submandibular gland. J Craniofac Surg. 2011;22:1128–31.
Chen J, Zhao X, Liu H, Zhou S, Yang Y, Li S, et al. A point-scoring system for the clinical diagnosis of Sjögren's syndrome based on quantified SPECT imaging of salivary gland. PLoS ONE. 2016;11:e0155666.
Araz M, Soydal C, Ozkan E, Kir MK, Ibis E, Gullu S, et al. The efficacy of fluorine-18-choline PET/CT in comparison with 99m Tc-MIBI SPECT/CT in the localization of a hyperfunctioning parathyroid gland in primary hyperparathyroidism. Nucl Med Commun. 2018;39:989–94.
Acknowledgements
This work was supported by JSPS KAKENHI Grant Number JP 18K09754.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kazunori Ninomiya, Shuji Toya, and Ichiro Ogura declare that they have no conflict of interest.
Human rights statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ninomiya, K., Toya, S. & Ogura, I. Single-photon emission computed tomography/computed tomography for evaluation of salivary gland dysfunction: preliminary study on diagnostic ability of maximum standardized uptake value. Oral Radiol 36, 163–167 (2020). https://doi.org/10.1007/s11282-019-00393-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11282-019-00393-2