Abstract
Purpose
To investigate the outcomes and risk factors of patients treated with stereotactic ablative radiotherapy (SABR) delivered by image-guided helical tomotherapy (HT) for extracranial oligometastases.
Methods
From August 2006 through July 2011, 42 consecutive patients (median age 69 years [range 16–87]) with oligometastases (≤3) received HT to all known cancer sites (lung, n = 28; liver, n = 12; adrenal, n = 2). Prognostic factors were assessed by Cox’s proportional hazards regression analysis.
Results
A total of 60 lesions were treated with hypofractionated HT (median dose 39 Gy [range 36–72.5]; median dose per fraction 12 Gy [range 5–20]). Complete or partial response was observed in 40 (54 %) patients. With a median follow-up period of 15 months, 1- and 2-year overall survival (OS) was 84 and 63 %, respectively; and 1- and 2-year local control (LC) was 92 and 86 %, respectively. Four patients had pneumonitis Grade ≥2 and two patients had lower gastrointestinal toxicity Grade ≥2. Only the lack of complete/partial response was associated with higher risk of mortality on univariate (HR = 3.8, P = 0.04) and multivariate (HR = 6.6, P = 0.01) analyses.
Conclusions
SABR delivered by image-guided HT is well tolerated and offers adequate LC with low acute morbidity in patients with extracranial oligometastatic disease. We found that the response to HT was the only predictor for OS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Definitive radiation therapy (RT) can cause significant acute and chronic adverse effects. Therefore, radical RT has historically been reserved for patients with stage I−III disease, and the most common indication for RT to the metastatic site has been palliation for pain or other symptoms directly resulting from the tumor metastases. However, metastatic patients are a very broad category [1], and prior studies have suggested that some patients with only a few distant metastases (‘oligometastases’) [2] may benefit from local therapy to the distant sites of disease [3, 4].
With the advent of image-guided RT [5] and stereotactic ablative radiotherapy (SABR), it has become possible to ablate tumors using high radiation doses to limited target volumes with surprisingly minimal morbidity [6–9]. Using these treatment techniques, high rates of durable local tumor control (LC) are achievable in oligometastatic tumors [10]. These outcomes represent a significant improvement compared with historical controls treated with conventionally fractionated regimens.
In this context, we have investigated the outcomes and risk factors for a single-institution series of patients with extracranial oligometastases who received SABR delivered by image-guided helical tomotherapy (HT).
Methods and materials
Selection criteria
This research project was approved by the institutional review board and was in compliance with the Health Insurance Portability and Accountability Act regulations. Subjects were identified by searching a database of patients with extracranial oligometastases treated with SABR delivered by image-guided HT between October 2006 and June 2011.
Inclusion criteria were having a Karnofsky performance status ≥70, having extracranial oligometastatic disease (≤3 metastases) with a locally controlled primary tumor, no Child B or C liver cirrhosis and functional liver volume of >1,000 cc in those patients with oligometastatic tumors in the liver, and lung diffusion capacity for carbon monoxide >30 % in the case of lung metastases. Ultimately, 42 patients met these criteria.
Chemotherapy
Treatment patterns were analyzed by line of therapy. Each treatment regimen was defined by the chemotherapy and/or biologic agents given to a patient within a 4-day period starting from the date of the first chemotherapy or biologic administration. The treatment was considered advanced to the next line of therapy when an addition or substitution of chemotherapy or biologic agent was observed and the resulting drug regimen lasted 28 days and was administered for two or more cycles.
Radiation therapy
RT was carried out using the TomoTherapy Hi-Art II System (TomoTherapy Inc., Madison, WI), which fully integrates image-guided RT by means of mega voltage computed tomography (MVCT) scanning and intensity modulated RT (IMRT) via dynamic rotational therapy. Before each treatment session, patients underwent scanning using the integrated MVCT scan modality and were repositioned after co-registration of these images with the planning kilovoltage CT scan. Target delineation was performed using the Pinnacle treatment planning system (Philips Medical Systems, Bothell, WA). Afterwards, the planning CTs ± positron emission tomography (PET)/CTs and the contours were transferred to the HT Hi-Art II planning system using the digital imaging and communications in medicine RT protocol. The gross tumor volume (GTV), defined only as the solid abnormality on CT ± PET, was not expanded in the traditional fashion to form a clinical target volume (CTV). The GTV was expanded to a planning treatment volume (PTV) which accounts for set-up variability and tumor motion. Individualized assessment of tumor mobility (ITVs) was derived using a multiple CT scan (patients received CT scanning during free breathing, maximal inspiration, and maximal expiration) [11]. The PTV was obtained by uniformly expanding the ITV not more than 0.5 cm in the axial plane (left, right, anterior, and posterior), and 1.0 cm in the craneocaudal plane (superior and inferior) [12]. All planes were optimized to deliver at least 95 % of the prescribed dose to 100 % of the PTV, while keeping the maximum dose (Dmax) to the PTV below 105 % of the prescribed dose with heterogeneity corrections using the superposition/convolution algorithm.
Risk-adapted fractionation schemes were used. The majority of lung metastases underwent three fractions of 20 Gy when lesions were not adjacent to the chest wall; three to five fractions of 12 Gy for lesions showing broad contact with the chest wall; or eight fractions of 7.5 Gy for central lesions. For liver and adrenal metastases, three fractions of 12 or 20 Gy were delivered depending on tumor size and estimated risk of normal tissue toxicity.
No definitive consensus currently exists regarding constraints for thoracic or abdominal organs at risk (OARs) for SBRT [13, 14]. The linear-quadratic formula (with an assumed alpha/beta ratio of 10 for tumors) was used in dose conversions making some adjustments for fraction and was also used to determine our current set of dose constraints of OARs. For the treatment of thoracic tumors, patients were required to have 1,000 mL of tumor-free lung. For patients with chronic lung disease (i.e., chronic obstructive lung disease), 70 % of the lung or 800 mL (whichever was larger) was required to be kept under 1.7 Gy per fraction and <17 Gy total. For patients with healthy lungs, 60 % of the lung was required to be kept under 2 Gy per fraction and <20 Gy total. Generally, the maximum dose to the esophagus was kept under 3.5–4.0 Gy per fraction. For the treatment of liver tumors, the volume of liver not involved with gross tumor was required to be >1,000 mL. For patients with no history of liver failure or hepatitis, the dose to 60 % of the liver volume was required to be <30 Gy, and for patients with a history of hepatitis or cirrhosis the dose to 70 % of the liver volume was required to be <30 Gy. It was required that <50 % of the kidneys would receive >16 Gy. The dose to the small bowel was required to be <50 Gy. It was required that the dose to the center of the spinal cord be <2 Gy per fraction and <45 Gy total, whereas the surface dose was to be kept <54 Gy. Generally, the spinal cord maximum was <30 Gy in 3-Gy fractions. Chest wall dose was restricted to <30 Gy to 30 cc and <60 Gy to 3 cc. Figure 1 shows the dose distribution and dose–volume histograms relative to planning target volume and organs at risk of three patients.
Patients were evaluated at approximately 1–3 months after the completion of therapy. The Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1 was used for treatment evaluation [15]. CT ± PET scans were obtained at intervals of 3–6 months to assess for recurrence.
Statistical analysis
All data analyses were done using the SPSS (version 19.0) statistical software. The primary endpoint of the study was overall survival (OS), and progression-free survival (PFS) and toxicity were the secondary endpoints. Recurrence in the primary radiation field was defined as recurrence within the PTV. Acute toxicity was scored according to the Common Terminology Criteria for Adverse Events (CTCAE) version 3.0 [16]. The Kaplan–Meier method was used to estimate the probabilities of survival. Potential associations were assessed in univariate analyses using the Cox proportional hazards model. Multivariate Cox regression was performed to adjust for factors significant on univariate analysis, as well as any other factors that might have confounded the univariate analysis. Quantitative variables were evaluated using the median as the cut-off, except for the biological effective dose (BED), normalized to a 2 Gy fraction, which was dichotomized at 100 Gy. Survival time was measured from the start date of HT to the first occurrence of the considered event (death or recurrence).
Results
Patient characteristics are listed in Table 1. All patients were considered inoperable by the number, dimension or location of the metastases (n = 34), or due to being medically unfit for surgical resection (n = 6). In addition, two patients refused surgery. The median length of follow-up at the time of analysis was 15 months (range 2–57). The total radiation dose to the metastatic site for all patients ranged from 36 to 72.5 Gy (median 39 Gy) with a median dose per fraction of 12 Gy (range 5–20). The most common fractionations used were 36 Gy at 12 Gy/fraction (n = 20) and 60 Gy at 12 Gy/fraction (n = 10). Median radiation therapy oncology group (RTOG) homogeneity index [17] and Paddick conformity index [18] values were 1.15 and 1.25, respectively. Thirty-eight patients (90 %) received at least one line of chemotherapy before HT. Fourteen patients (33 %) received two lines and four patients (9.5 %) three. For first-line therapy, the most common chemotherapy backbone regimens were infused fluorouracil, leucovorin, and oxaliplatin (FOLFOX; n = 16, 38 % of patients), and gemcitabine plus cisplatin (GemCis; n = 6, 14 %). The most common treatment regimen was FOLFOX plus bevacizumab (n = 15, 35.7 %). For second-line therapy, fluorouracil, leucovorin, and irinotecan (FOLFIRI) were the most common chemotherapy backbones (n = 7, 16.7 %), and FOLFIRI plus bevacizumab was the most common treatment regimen (n = 5, 11.9 %). Across the study period, 47.6 % (n = 20) and 16.7 % (n = 7) of patients received bevacizumab and cetuximab, respectively.
The sites of metastatic disease were the lung (n = 28), liver (n = 7) and adrenal glands (n = 2). Sixteen (36 %) patients had more than one metastases in the same organ and 4 (9.5 %) patients had metastases in more than one site. All lesions underwent radiation therapy. The most common primary sites were colon/rectum (64 %) and lung (14 %; Table 1).
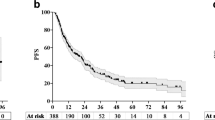
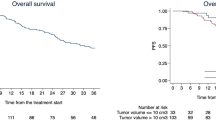
At the time of reporting, 12 patients had died. A complete and partial response was observed in 9 and 14 patients, respectively. Seventeen patients had stable disease and 2 patients progressed. The local relapse rate was 9.5 % (n = 4), and 22 of the original 42 patients had new sites of distant metastases (lung, n = 13; liver, n = 6; brain, n = 3). For all patients, the 1- and 2-year OS rates were 92 and 86 %; the 1- and 2-year PFS was 83 and 65 %; and the 1- and 2-year local control (LC) rates were 92 and 86 % (Fig. 2). Univariate Cox proportional hazard analyses showed that having a longer time from the primary tumor diagnosis date to the oligometastases was associated with a lower risk of mortality (hazard ratio [HR] = 0.2; P = 0.03). In contrast, the lack of complete/partial response (HR = 3.8; P = 0.04) or having a greater oligometastases size (HR = 4.5; P = 0.01) were associated with a higher risk of mortality (Table 2). On multivariate analysis (Table 3), only the response to the HT retained significance (HR = 6.6; P = 0.01; Fig. 3). We did not find a significant risk factor for PFS on univariate analysis (Table 2).
With regard to toxicity, grades 1, 2, and 3 radiation pneumonitis were experienced in 11, 3, and 1 patient, respectively. Six patients had grade 1 chest wall pain. Grade 1 skin toxicity was observed in 6 patients. Finally, gastrointestinal toxicity was observed in 8 patients: esophagitis grade 1 in 3 patients; diarrhea grade 1 and 2 in 3 and 1 patient, respectively, and lower gastrointestinal hemorrhage grade 3 in 1 patient.
Discussion
Oligometastatic disease represents a hypothesized state of metastatic progression in which a limited systemic spread of disease is potentially curable with local therapy [19–21]. We present one of the largest published studies on outcomes in patients with extracranial oligometastases treated with HT, with specific assessment of the effect of aggressive local radiation on survival. Our pertinent findings can be summarized as follows. First, oligometastatic patients treated with HT had an excellent OS and LC, having a 2-year OS rate of 86 % and only a 9.5 % rate of local recurrence. Second, we found that only the lack of complete/partial response was associated with a higher risk of mortality. Patients who had a complete/partial response experienced prolonged OS compared with those who had not. However, neither the treatment response nor other factors were associated with PFS. Finally, image-guided HT was well tolerated in the majority of patients, with only 2 cases experiencing severe (grade 3) toxicity.
The number of studies assessing patients with extracranial oligometastatic disease treated with SABR is limited and the aggregate results are inconclusive [6, 9, 22]. For example, a recent systematic literature search performed by Silva et al. [9] evaluated the outcomes, techniques, radiobiology, and scientific rigor of SABR for the treatment of pulmonary oligometastatic cancer. There was insufficient evidence to recommend a consensus view for optimal tumor parameters, dose fractionation, and technical delivery of treatment. However, high LC rates that could potentially lead to a survival benefit justifies the consideration of stereotactic radiotherapy for patients with limited pulmonary oligometastases. Milano et al. [20] found that lesions originating from primary pancreatic, biliary or liver cancer exhibited significantly poorer LC, as did lesions from colorectal cancer. They also observed that lesions from breast cancer were better controlled. Therefore, one should notice the careful selection based on localization and dimension in most of these SABR series. In addition, a standard SABR regimen for metastatic lesions is still unclear. For instance, Iwata et al. [23] used 34 and 36 Gy for lung metastasis, while a French group [24] used a median fractionation scheme of three fractions of 15 Gy (range, 9–20 Gy). Our study mainly used risk-adapted fractionation schemes according to the metastatic lesion location.
The number of distant metastatic sites was not associated with survival outcomes in this study, probably because most of the patients had only a single site of metastatic disease, thus making it difficult to detect an advantage among patients with fewer sites of disease. To this end, several studies have shown that when distant metastases are limited in number and location, sterilization or LC of the metastases may improve both PFS and OS [19, 21]. For example, the University of Florence [19] reported a substantial LC benefit for patients with adrenal gland metastases who received SABR, with a control rate of 90 % at 2 years. Consistently, we observed a similar LC rate in our series. In addition, a multi-institutional phase I/II trial of SABR for lung metastases [21] reported a series of 38 patients with one to three lung metastases and a cumulative maximum tumor diameter smaller than 7 cm. With a median follow-up of 15 months, LC at 1 and 2 years after SABR was 100 and 96 %, respectively. There was no grade 4 toxicity and the incidence of any grade 3 toxicity was 8 %. The high rates of OS and LC observed in these studies as well as in ours could be explained due to the patient’s selection. In our study, the vast majority of patients had a good performance status (KPS ≥ 70), only 1–2 sites of metastatic disease, and approximately 2-year median interval (21 months) between diagnosis and time to metastasis.
With regard to toxicity outcomes, the rate of severe (grade ≥3) acute toxicity in our study was lower to that in published series of patients with metastatic disease [21]. There are several potential reasons that could explain this divergence. First, the relatively short follow-up period (15 months for all 42 patients) may have led to an underestimation of toxicity. Second, the use of SABR allows optimization between tumor control probability and normal tissue complication probability [22]. For those patients, toxicity has ceased to be a dose-limiting issue since the introduction and availability of HT [25]. Hence, the combination of dose sculpting by IMRT with image guidance techniques is mandatory for these indications [26]. Finally, in a considerable number of patients of our series, metastases were localized far from the proximity of OARs (i.e., 82 % of lung metastases were located peripherally), and therefore there was not an overlap with the PTV in these patients, which would make the delivery of curative doses to the tumor impossible with regard to normal tissue toxicity.
Our finding that complete/partial response was associated with improved outcome is consistent with prior studies [7, 27, 28]. However, an association between response and PFS was not observed. Langenhoff et al. [28] reported outcomes for 23 patients with unresectable colorectal liver metastases which were treated with SABR. None of the treatment responders developed a local recurrence during a mean follow-up period of 16 months.
We acknowledge several limitations of our study. First, the population was heterogeneous (different primary tumors and metastases location), having been treated with HT over 5 years and receiving different combinations of radio(chemo)therapy regimens rather than being treated prospectively on a well-defined treatment protocol. In addition, a systematic method of follow-up, including imaging, would be optimal to evaluate patterns of failure after radiotherapy. For example, patients with “distant only” recurrences may not have undergone optimal imaging of the prior metastatic site at the time of recurrence. Thus, some local failures might not have been detected. Future studies that include larger numbers of patients with oligometastases treated with and without radical RT would be useful for further elucidating the effect of local therapy on these subgroups and may also identify additional risk factors, which were not able to be identified in the current study due to a small sample size. Finally, it must be emphasized that systemic therapy plays an important role in the management of metastatic patients, including in the oligometastatic setting. Up-front chemotherapy followed by either switch/continuation maintenance or observation remains the standard of care in this context, and local therapy to metastatic sites should be performed in the scenario of a clinical trial, if possible.
In conclusion, we found that patients with oligometastatic disease who were treated with hypofractionated HT could be treated safely and had improved rates of LC and OS. We also found that those who experienced complete/partial response were associated with a lower risk of mortality. Our results suggest that a subgroup of patients with stage IV disease can benefit from aggressive treatment to the metastatic site. Further investigation should focus on patient selection and in the use of peri/concomitant systemic therapy to decrease the distant relapse rate in patients undergoing local treatment.
References
Greene FL, Page DL, Fleming ID et al (2002) Lung. In: AJCC cancer staging manual, 6th edn. Springer, New York
Weichselbaum RR, Hellman S (2011) Oligometastases revisited. Nat Rev Clin Oncol 8:378–382
Lopes JC, Navarro A, Solé JM, Martínez M, Guedea F (2010) Stereotactic body radiation therapy for spinal metastases. Clin Transl Oncol 12:639–642
Norihisa Y, Nagata Y, Takayama K et al (2008) Stereotactic body radiotherapy for oligometastatic lung tumors. Int J Radiat Oncol Biol Phys 72:398–403
Tomita N, Soga N, Ogura Y et al (2012) Preliminary results of intensity-modulated radiation therapy with helical tomotherapy for prostate cancer. J Cancer Res Clin Oncol. doi:10.1007/s00432-012-1277-0
Hoyer M, Swaminath A, Bydder S et al (2012) Radiotherapy for liver metastases: a review of evidence. Int J Radiat Oncol Biol Phys 82:1047–1057
Cárdenes HR, Price TR, Perkins SM et al (2010) Phase I feasibility trial of stereotactic body radiation therapy for primary hepatocellular carcinoma. Clin Transl Oncol 12:218–225
Oshiro Y, Aruga T, Tsuboi K et al (2010) Stereotactic body radiotherapy for lung tumors at the pulmonary hilum. Strahlenther Onkol 186:274–279
Siva S, MacManus M, Ball D (2010) Stereotactic radiotherapy for pulmonary oligometastases: a systematic review. J Thorac Oncol 5:1091–1099
Ohtakara K, Hayashi S, Mizuta K et al (2012) Clinical outcomes of single or oligo-fractionated stereotactic radiotherapy for head and neck tumors using micromultileaf collimator-based dynamic conformal arcs. J Cancer Res Clin Oncol 138:1511–1522
Lagerwaard FJ, Van Sornsen de Koste JR, Nijssen-Visser MR et al (2001) Multiple “slow” CT scans for incorporating lung tumor mobility in radiotherapy planning. Int J Radiat Oncol Biol Phys 51:932–937
Timmerman R, Galvin J, Michalski J et al (2006) Accreditation and quality assurance for radiation therapy oncology group: multicenter clinical trials using stereotactic body radiation therapy in lung cancer. Acta Oncol 45:779–786
Timmerman RD (2008) An overview of hypofractionation and introduction to this issue of seminars in radiation oncology. Semin Radiat Oncol 18:215–222
Bentzen SM, Constine LS, Deasy JO et al (2010) Quantitative analyses of normal tissue effects in the clinic (QUANTEC): an introduction to the scientific issues. Int J Radiat Oncol Biol Phys 76:S3–S9
Eisenhauer EA, Therasse P, Bogaerts J et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247
Cancer Therapy Evaluation Program (2003) Common terminology criteria for adverse events VB, MD, National Cancer Institute
Feuvret L, Noel G, Mazeron JJ, Bey P (2006) Conformity index: a review. Int J Radiat Oncol Biol Phys 64:333–342
Paddick I (2000) A simple scoring ratio to index the conformity of radiosurgical treatment plans. Technical note. J Neurosurg 93:219–222
Casamassima F, Livi L, Masciullo S et al (2012) Stereotactic radiotherapy for adrenal gland metastases: university of Florence experience. Int J Radiat Oncol Biol Phys 82:919–923
Milano MT, Katz AW, Schell MC et al (2008) Descriptive analysis of oligometastatic lesions treated with curative-intent stereotactic body radiotherapy. Int J Radiat Oncol Biol Phys 72:1516–1522
Rusthoven KE, Kavanagh BD, Burri SH et al (2009) Multi-institutional phase I/II trial of stereotactic body radiation therapy for lung metastases. J Clin Oncol 27:1579–1584
Chi A, Jang SY, Welsh JS et al (2011) Feasibility of helical tomotherapy in stereotactic body radiation therapy for centrally located early stage nonsmall-cell lung cancer or lung metastases. Int J Radiat Oncol Biol Phys 81:856–862
Iwata H, Shibamoto Y, Baba F et al (2011) Correlation between the serum KL-6 level and the grade of radiation pneumonitis after stereotactic body radiotherapy for stage I lung cancer or small lung metastasis. Radiother Oncol 101(267–270):22
Fumagalli I, Bibault JE, Dewas S et al (2012) A single-institution study of stereotactic body radiotherapy for patients with unresectable visceral pulmonary or hepatic oligometastases. Radiat Oncol 7:164
Engels B, Gevaert T, Everaert H et al (2012) Phase II study of helical tomotherapy in the multidisciplinary treatment of oligometastatic colorectal cancer. Radiat Oncol 7:34
Verellen D, De Ridder M, Linthout N et al (2007) Innovations in image-guided radiotherapy. Nat Rev Cancer 7:949–960
Engels B, Everaert H, Gevaert T et al (2011) Phase II study of helical tomotherapy for oligometastatic colorectal cancer. Ann Oncol 22:362–368
Langenhoff BS, Oyen WJ, Jager GJ et al (2002) Efficacy of fluorine-18-deoxyglucose positron emission tomography in detecting tumor recurrence after local ablative therapy for liver metastases: a prospective study. J Clin Oncol 20:4453–4458
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sole, C.V., Lopez Guerra, J.L., Matute, R. et al. Stereotactic ablative radiotherapy delivered by image-guided helical tomotherapy for extracranial oligometastases. Clin Transl Oncol 15, 484–491 (2013). https://doi.org/10.1007/s12094-012-0956-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-012-0956-2