Abstract
Hypothyroidism is a condition that becomes more prevalent with age. Patients with untreated hypothyroidism have consistently reported symptoms of severe cognitive impairments. In patients suffering hypothyroidism, thyroid hormone supplementation offers the prospect to alleviate the cognitive consequences of hypothyroidism; however, the therapeutic value of TH supplementation remains at present uncertain and the link between cellular modifications associated with hypothyroidism and neurodegeneration remains to be elucidated. In the present study, we therefore evaluated the molecular and behavioral consequences of T3 hormone replacement in an animal model of hypothyroidism. We have previously reported that the antithyroid molecule propylthiouracil (PTU) given in the drinking water favors cerebral atrophy, brain neuroinflammation, Aβ production, Tau hyperphosphorylation, and altered plasticity-related cell-signaling pathways in the hippocampus in association with hippocampal-dependent spatial memory deficits. In the present study, our aim was to explore, in this model, the effect of hippocampal T3 signaling normalization on various molecular mechanisms involved in learning and memory that goes awry under conditions of hypothyroidism and to evaluate its potential for recovery of hippocampal-dependent memory deficits. We report that T3 supplementation can alleviate hippocampal-dependent memory impairments displayed by hypothyroid rats and normalize key markers of thyroid status in the hippocampus, of neuroinflammation, Aβ production, and of cell-signaling pathways known to be involved in synaptic plasticity and memory function. Together, these findings suggest that normalization of hippocampal T3 signaling is sufficient to reverse molecular and cognitive dysfunctions associated with hypothyroidism.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid hormones (THs), particularly the main cellular active forms, triiodothyronine (T3) and thyroxin (T4), are powerful neuromodulators of brain functions throughout life. In the brain T3, the main transcriptionally active form, has a double origin: a fraction is available directly from the circulation (mainly produced from T4 by a type-1 iodothyronine deiodinases D1), and another is produced locally from T4 in astrocytes by a type-2 iodothyronine deiodinases D2. The fetal brain depends almost entirely on T3 generated locally. The contribution of systemic T3 increases subsequently during development to account for approximately 50% of total brain T3 in the late postnatal and adult stages [1]. Rapid non-genomic TH actions have been described; however, TH effects are predominantly mediated by their binding to nuclear thyroid hormone receptors (TRs), which act as transcriptional factors regulating the expression of specific thyroid hormone-responsive genes [2, 3]. Thus, slight variations from the normal/homeostatic range of TH may have wide-ranging effects on multiple organ systems, including the central nervous system. It has been shown that adult-onset dysthyroidism, which become more prevalent with age, is closely related to neuropsychiatric and cognitive disorders [4]. Epidemiological studies have in particular suggested a compelling relationship between both hypo- and hyperthyroidism and the risk for Alzheimer’s disease (AD), the most common cause of dementia in the elderly [5,6,7,8].
Hypothyroidism is a condition that becomes more prevalent with age and patients with untreated hypothyroidism have consistently reported symptoms of severe cognitive impairment including learning and memory impairments [9]. Clinical reports show variable results as to whether TH replacement therapy can fully restore hypothyroidism-induced impairments in learning and memory in the adult. It has been reported that 15% of L-T4-treated hypothyroid patients complain of psychological symptoms and/or cognitive dysfunction despite normal blood TSH level [10]. Accumulating evidence suggest that there is tissue-specific regulation of TH contents in target tissues via differential expression of thyroid hormone transporters and iodothyronine deiodinases [11]. Serum thyroid hormones may thus not always accurately reflect the hormonal status of target tissues. This has brought into question the ability of L-T4 monotherapy in hypothyroid patients with persistent complaints, to fully restore T3 content in target tissues, especially in the brain. So far, the link between cellular modifications associated with hypothyroidism and neurodegeneration as well as the cell-signaling mechanisms by which hormone replacement therapy can alleviate certain cognitive deficits remain to be elucidated.
The hippocampus, a key structure for several forms of learning and memory, is highly sensitive to the actions of thyroid hormones due to a high expression of thyroid hormone receptor. A decrease in hippocampal volume in adult patients with untreated overt hypothyroidism has been described [12]. Moreover, recent studies in adult rats with hypothyroidism have reported deficits in hippocampal-dependent spatial learning and memory [13, 14] and, at the molecular level, impairments of long-term potentiation (LTP) in area CA1 of the hippocampus [15]. Several authors have shown that spatial memory deficits and altered CA1 LTP in hypothyroid animals are associated with an alteration of neurogranin (RC3) expression in neurons, a target gene of TH [16,17,18,19]. RC3 is involved in synaptic plasticity and memory via the modulation of Ca2+/calmodulin-dependent signaling [20, 21]. This signaling pathway interacts with the MAPK/ERK-CREB pathway, also involved in synaptic plasticity and hippocampal functions [22,23,24]. Our recent studies showed that 5-week treatment with the antithyroid molecule, propylthiouracyl (PTU), induces hypothyroidism in adult rats. This antithyroid molecule blocks the activity of thyroid peroxidases that are essential for thyroid hormone synthesis and inhibits D1, which produces T3 by deiodination of T4 in peripheral tissues such as blood [25, 26]. PTU treatment is associated with a reduction of cerebral and hippocampal volume and an alteration in hippocampal expression of signaling molecules important for synaptic plasticity and memory, including RC3, CaM, CaMKII, CaMKIV, ERK, CREB, and EGR1/ZIF268, associated with spatial memory deficits [27, 28]. PTU-treated rats also showed increased levels of Aβ peptide production, abnormal Tau phosphorylation, and high levels of several pro-inflammatory cytokines in the hippocampus, biochemical changes generally associated with neurodegenerative pathology, in particular with AD. Altogether, the above-mentioned data support the hypothesis that adult-onset hypothyroidism is prone to produce a wide range of hippocampal molecular dysfunctions converging towards plasticity and memory impairments, which ultimately may favor the development of AD.
To address this question, in the present study, we aim at exploring to which extent reinstating T3 signaling in the hippocampus impacts on various molecular mechanisms involved in learning and memory that goes awry under conditions of hypothyroidism and leads to a subsequent recovery of hippocampal-dependent memory deficits. For this purpose, we evaluated the hippocampal molecular consequences of T3 replacement therapy in our model of PTU-induced spatial memory deficits with a special focus on Aβ42 generation, neuroinflammation occurrence, and synaptic plasticity markers.
Material and Methods
Animals and Treatment
The experiments were performed with 8-week-old male Wistar rats (Janvier, Le Genest Saint Isle, France). Animals were housed two per cage in a colony room with a constant airflow system, controlled temperature (21–23 °C), and light (12:12 h light/dark cycle) with food and water ad libitum. The experimental design is summarized in Fig. 1. Rats were randomly assigned to one of two groups: the control group (N = 18) or the hypothyroid group (N = 30). Hypothyroidism was induced by adding 0.05% propylthiouracyl (6-n-propyl-2-thiouracyl, PTU; Sigma Chemicals, St Louis, MO, USA) to their drinking water for 7 weeks as described by Ghenimi et al. (2010) [27]. Knowing that in the adult, the contribution of systemic T3 accounts for approximately 50% of total brain T3, we used T3 supplementation in a group of PTU-treated rats to better control the thyroid hormone replacement in hypothyroid animals and to bypass the necessary conversion of T4 to T3 by D1. Thus, after 5 weeks, a group of PTU-treated rats (N = 12) were injected daily (i.p.) with 150 μg/kg/day T3 (Sigma) until the end of behavioral testing. A similar T3 replacement has been used in several studies in hypothyroid models induced by PTU treatment [29,30,31]. T3 was dissolved in a vehicle mixture containing NaOH 0.1 N/NaCl 0.9% (1 V/4 V). Control and PTU-untreated rats were given similar vehicle injections. In our laboratory, we have shown in various experimental models of brain T3 hyposignalling that 4 days of this treatment can normalize mRNA levels of T3 target genes [17, 32, 33]. Thus, rats were administrated with T3 for 4 days before the start of the behavioral tasks. The half-life of T3 does not exceed 24 h [34]; therefore, rats were injected daily, 12 h before starting behavioral testing, during 2 weeks.
Two cohorts of rats were used. The first cohort was used for behavioral testing in the radial-arm water maze (RAWM) task (controls: N = 12, PTU: N = 12 and PTU + T3: N = 6). The second cohort (N = 6 per group) was tested in the elevated Plus-Maze task. After completion of the behavioral tasks, rats were sacrificed and their hippocampi were collected: 6 per group were used for western blotting, 6 for qRT-PCR, and 11 per group for Aβ42-ELISA.
All efforts were made to minimize the number of animals and their suffering throughout the experiments. Experiments were performed in accordance with the European Communities Council Directive of 24 November 1986 (86/609/EEC), EU Directive 2010/63/EU and the French National Committee (87/848).
Behavioral Tasks
Behavioral testing was undertaken between 8 a.m. and 7 p.m. after daily handling for 1 week. A video camera was mounted on the ceiling above each testing apparatus and rats’ behavior was monitored and analyzed using the ANY-maze™ video-tracking system and software (version 4.5, Stoelting Co., USA).
Elevated Plus-Maze
To assess anxiety, rats (N = 6 per group) were tested in an elevated plus-maze (black opaque Plexiglas, 50 cm above the floor) that consisted of four arms (50 cm × 10 cm) connected by a common 10 cm × 10 cm center area. Two opposite facing arms were open, while the other two facing arms were enclosed by high walls (40 cm in height). Each rat was placed onto the central area facing an open arm and observed for 10 min. The maze was cleaned with 100% ethanol between each animal. Total number of entries and time spent in open and enclosed arms were recorded to evaluate anxiety-like behavior.
Radial Arm Water Maze
Spatial learning and memory performance was tested in a radial-arm water maze (RAWM) as described by Diamond et al. (1999) and Chaalal et al. (2014) [28, 35]. The RAWM is a navigational paradigm in which rats learn to find a submerged platform to escape from swimming. Several large extra-maze visual cues were placed on the walls of the room. The apparatus consisted of a white circular tank (150 cm in diameter, 40 cm height) filled with water (22 °C) made opaque by adding a white, nontoxic opacifier (Acusol OP301 Opacifier, Rohm and Haas). Six V-shaped Plexiglass inserts (39 cm height, 50 cm length) placed into the tank produced six swim arms that radiated from an open central area. A hidden platform (11 cm in diameter) was located 2 cm below the water surface at the far end of one arm (designated as the “goal arm”). For each rat, the platform remained in the same arm during all learning and memory trials of a given day but was moved to a new arm each day. Each day, rats were given four consecutive learning trials (max 60 s). For each learning trial, the rat was placed into one arm (designated as the “start arm”) facing the wall of the water tank, with start locations varying pseudo-randomly. After reaching the platform, rats were allowed to remain on it for 30 s. If a rat did not locate the hidden platform within 1 min, it was gently guided to the platform. Each day, after the fourth learning trial, two probe tests (memory trials) were performed, respectively, 15 min and 5 h later. A third probe test was performed the following day (24 h after each learning day). These probe tests consisted of a single 60-s trial. Total duration of the task was 11 days. Using the video tracking system, we registered arm entry errors, described as every time a rat entered an arm other than the goal arm or entered the goal arm without reaching the platform.
T3 Enzyme-Linked Immunosorbent Assay
Blood was collected during sacrifice, about 12 h after the last T3 or vehicle injection. Serum was immediately separated by centrifugation and stored at − 20 °C until analysis. Serum total T3 was measured (N = 6 per group) using an ELISA Complete Kit (NovaTec Immundiagnostica, Germany) according to the manufacturer’s instruction sheet.
Aβ42 Enzyme-Linked Immunosorbent Assay
Hippocampal tissue samples (N = 11 per group) were homogenized with 400 μl of extraction buffer containing a protease inhibitor cocktail (T-PER, Pierce). Homogenates were centrifuged at 15,000 rpm for 5 min. The resultant supernatant was collected. Endogenous rat hippocampus Aβ42 was quantified with the Wako ELISA system as described in the manufacturer’s instruction sheet.
Real-Time Quantitative PCR
RNA extraction from hippocampal tissue samples (N = 6 per group) was conducted using an extraction kit (Trizol reagent, Invitrogen, France) according to the manufacturer’s instructions. The quality and the concentration of RNA were determined by spectrophotometry. Using OligodT and random primers (Promega, France), cDNA were synthetized with SuperScript II reverse transcriptase (Invitrogen, France). The real-time polymerase chain reaction (PCR) was performed in a LightCycler system (CFX96 TouchTM, Bio-Rad, France) using a qPCR SsoAdvancedTM SYBR® Green Supermix (Bio-Rad, France). Forward and reverse primer sequences were designed in accordance with published sequences available in Lin et al. (2009) for TNFα, CRP, IL-1β, IL-6 and in Ghenimi et al. (2010) for cyclophilin B (PPIB, the housekeeping gene), TR isoforms (TRα and TRβ), RC3, APP695, and APP770–751 [27, 36]. Quantification was monitored by measuring the increase in fluorescent signal from the samples due to SYBR® Green dye binding to double-stranded DNA at the end of elongation step. The threshold cycle (Ct), defined as the cycle at which an increase in fluorescence above a defined baseline is first detected, was determined for each sample. The results were expressed as the ratio of the concentration of the target to that of PPIB within the same sample. We have verified that the expression level of PPIB was unaffected by the treatments and thus could be used to normalize data from target mRNA expression: standard curves (a plot of the crossing point (Cp) versus the amount of the initial cDNA used for amplification) of PPIB were comparable under all different experimental conditions (controls, PTU, and PTU + T3) indicating that the Cp was always the same for a given dilution of cyclophilin cDNA.
Western Blotting
Hippocampal tissue samples (N = 6 per group) were prepared for western blotting as described previously [37]. Each sample was loaded onto SDS-acrylamide gels (9–12%) and transferred onto a nitrocellulose membrane (0.2 μm for CaM, CaMKII, CaMKIV, CaN, RC3, IL1β proteins and 0.45 μm for CREB, EGR1, ERK, P38-MAPK, CRP proteins) by electro-blotting. Membranes were pre-blocked with TBST-milk (5%) and incubated overnight at 4 °C with primary antibody. The next-day membranes were washed and incubated in a horseradish peroxidase-conjugated anti-rabbit IgG (Amersham, GE Healthcare, France) or anti-mouse IgG (Amersham, GE Healthcare, France) or anti-goat IgG (Santa Cruz Biotechnology, France) for 1 h at room temperature. Membranes were washed with TBST buffer and proteins were visualized using the enhanced chemiluminescence (ECL) solution (Amersham, GE Healthcare, France). After development and fixation, the films were scanned. Staining intensity of the protein bands was determined using Totallab software (Nonlinear dynamics, UK). Membranes were then subsequently stripped of antibodies and re-probed with other antibodies using the same procedure. Antibodies used are against β-actin (Sigma-Aldrich, 1:10000), Calmodulin (Millipore, 1:5000), CaMKII (Santa Cruz Biotechnology, 1:750), phospho-CaMKIIα (Santa Cruz Biotechnology, 1:1000), CaMKIV (Millipore, 1:2000), CREB (Cell signaling Technology, 1:1000), phospho-CREB (Cell signaling Technology, 1:1000), CRP (R&D Systems, 1:1000), EGR1 (Cell signaling Technology, 1:500), ERK (Cell signaling Technology, 1:4000), phospho-ERK (Cell signaling Technology, 1:2000), IL-1β (R&D Systems, 1:1000), P38-MAPK (Cell signaling Technology, 1:1000), phospho-P38-MAPK (Cell signaling Technology, 1:1000), CaN (Millipore, 1:1000), RC3 (Chemicon, 1:3000), phospho-RC3 (Merck Millipore, 1:3000). For each protein studied, the experimental conditions for western blot analysis were first setup as follows, to avoid saturation of the signal, allowing reliable quantification. A standard curve was plotted between the intensity of the signal against the amount of sample loaded. To ensure reliable quantification, for a given antibody dilutions, ECL incubation/revelation time, a linear relation is needed between the signal (which corresponds to the quantity of proteins) and the quantity of total proteins loaded. In the subsequent experiments, for each individual protein studies, we then loaded a quantity of protein (10 μg to 20 μg) leading to an intensity of the signal localized in the middle of the linear plot. In addition, we verified that β-actin remained constant regardless of experimental conditions to ensure that this constituted a correct control for all the proteins of interest studied. The relative levels in proteins in hypothyroid and hypothyroid + T3-treated rats were expressed as a percentage of the same proteins in control rats. For pERK, pP38-MAPK, pCREB, pRC3, pCaMKII, data are presented as the ratio of phospho-proteins to total proteins, after being normalized to β-actin.
Statistical Analyses
Values are given as mean ± S.E.M. Statistical analyses were performed with Statview 5.0 software. Data were analyzed by a one-way ANOVA or repeated-measures ANOVA followed by Scheffe or Tukey’s post hoc test respectively for behavioral and biochemical data. For analysis of performance in the RAWM task, we used repeated-measures ANOVA comparing errors on successive trials across the three groups for the learning phase and successive probe tests. Days 1–3, 4–6, 7–9, and 10–11 were averaged for simplification and clarity of figures. For the Plus-Maze task and all biochemical assays, data were analyzed by one-way ANOVA. P values of less than 0.05 were considered statistically significant.
Results
Behavioral Consequences of T3 Supplementation
Anxiety-Like Behavior
The influence of T3 status on anxiety-like behavior was evaluated in the elevated plus-maze. No significant difference was observed between controls, PTU-treated, and PTU + T3-treated rats in the percentage of time spent in open arms (F (2, 15) = 0.71, NS) or in the number of entries into open arms (F (2, 15) = 1.19, NS), indicating no effect of thyroid status on anxiety-related responses (Fig. 2).
Thyroid status and anxiety-like behavior. Effect of PTU treatment and T3 supplementation on the time spent in open arms and the number of entries in open arms in the elevated plus-maze. No difference was observed between controls, PTU, and PTU + T3-treated rats in the percent time spent in open arms or the number of entries into open arms, indicating no effect of thyroid status on anxiety-related responses. Values are mean ± SEM (N = 6 per group)
Radial-Arm Water Maze
Using the radial-arm water maze task (RAWM) with the escape platform placed in a different arm on each training day, we have previously shown that PTU treatment impairs spatial learning and memory [28]. In this study, we tested the effect of T3 replacement on the memory deficits induced by PTU hypothyroidism. During the first 3 days of the behavioral task, for all groups, the mean number of errors between trial 1 and trial 4 of the acquisition phase decreased, revealing a modest but significant improvement of performance (Fig. 3a, trial effect: F(3, 81) = 17.192; p < 0.0001; group effect: F(2, 27) = 0.549; NS; trial × group interaction: F(6, 81) = 1.23; NS). Analyses of the three probe tests following the first 3 days of training indicate that all groups still showed relatively poor performance with an average of between 2.4 and 4.2 errors and no significant difference between the three groups (group effect: F(2, 27) = 2.29; NS; time effect: F(2, 54) = 0.36; NS; group × time interaction: F(4, 54) = 0.58; NS). Over the following training days, as the position of platform was changed each day, the mean number of errors on trial 1 was always important but, from trial 2, the number of errors decreased rapidly. However, on days 4–6 and days 7–9, PTU treatment alone resulted in a significant delay in learning (Fig. 3b, c; repeated-measures ANOVA; days 4–6: trial effect: F (3, 81) = 51.845; p < 0.0001; group effect: F(2, 27) = 1.184; NS; group × trial interaction: F(6, 81) = 2.99; p = 0.01; days 7–9: trial effect: F(3, 81) = 39.258; p < 0.0001; group effect: F(2, 27) = 1.369; NS; group × trial interaction: F(6, 81) = 3.311; p < 0.01). We notably observed that, on the second trial of the learning phase, at both days 4–6 and 7–9, hypothyroid rats made more errors than controls (factorial ANOVA, trial 2, days 4–6: group effect: F(2, 27) = 3.495, p < 0.05, post hoc PTU vs controls: p < 0.05; days 7–9: F(2, 27) = 5.661, p < 0.001; post hoc PTU vs controls p < 0.01). T3 administration in PTU-treated rats completely reversed this delay in learning and our analyses showed no significant difference between controls and PTU + T3 groups, the two learning curves being closely superposed (Fig. 3b, c; days 4–6: trial effect: F(3, 48) = 44.277; p < 0.0001; group effect: F(1, 16) = 2.008; NS; group × trial interaction: F(3, 48) = 1.83; NS; days 7–9: trial effect: F(3, 48) = 44.406; p < 0.0001; group effect: F(1, 16) = 0.088; NS; group × trial interaction: F(3, 48) = 0.212; NS). For the three probe tests following training days 4–6 and 7–9, animals from the PTU group made significantly more spatial memory errors than those from other groups (days 4–6: Fig. 3b, group effect: F(2, 27) = 8.707; p < 0.005; time effect: F(2, 54) = 0.992; NS; group × time interaction: F(4, 54) = 0.552; NS); days 7–9: Fig. 3c, group effect: F(2, 27) = 6.996; p < 0.005; time effect: F(2, 54) = 0.642; NS; group × time interaction: F(4, 54) = 0.601; NS). Thus, PTU-treated rats displayed significant short- and long-term memory impairments compared to controls (post hoc PTU vs controls: days 4–6, p < 0.001; days 7–9, p < 0.05) and these deficits were also reversed by T3 treatment (post hoc PTU + T3 vs PTU: days 4–6 and days 7–9, p < 0.05; post hoc control vs PTU + T3: days 4–6 and days 7–9, NS). Finally, at days 10–11, even if rats of all groups now showed a similar learning rate (trial effect: F(3, 81) = 65.482; p < 0.0001; group effect: F(2, 27) = 1.334; NS; group × trial interaction: F(6, 81) = 1.672; NS), short-term and long-term retention performance remained significantly affected in PTU-treated rats (Fig. 3d, group effect: F(2, 27) = 5.738; p < 0.01; time effect: F(2, 54) = 1.413; NS; group × time interaction: F(4, 54) = 0.575; NS). These memory deficits were again reversed by T3 administration (post hoc PTU vs controls: p < 0.05; PTU + T3 vs PTU: p < 0.05; control vs PTU + T3: NS).
Learning and memory deficits in PTU-treated rats in the radial-arm water maze task and recovery after T3 supplementation. Each panel represents the mean number of errors made during the learning phases (with a change in goal arm every day, left panels) and the short- (15 min) and long-term (5 h, 24 h) memory retention tests (right panels) for days 1 to 3 (a), 4 to 6 (b), 7 to 9 (c), and 10 to 11(d). PTU rats showed a transient delay in learning and both short- and long-term spatial memory deficits. T3 rescued learning and memory performance in PTU-treated rats. Values are mean ± SEM (controls: N = 12 rats, PTU: N = 12 rats, PTU + T3: N = 6 rats). Main statistical results from repeated-measures ANOVA for learning and probe tests are indicated in boxes above the curves. Asterisks and number signs indicate post hoc statistical analyses. *p < 0.05; **p < 0.005; ***p < 0.01; ****p < 0.001 mean values significantly different between PTU-treated and control rats on learning trial 2 and probe tests. #p < 0.05, mean values significantly different between PTU + T3 and PTU-treated rats on probe tests
Thyroid Status
Body weight was used as a general indicator of the efficiency of PTU treatment, known to arrest growth in young adult rats [29]. Body weights were not significantly different at the beginning of the experiment (288.89 ± 1.78 and 293.00 ± 2.47 g respectively for controls (N = 18) and hypothyroid rats (N = 30)). As described in our previous work, body weight gain of PTU-treated rats slowed down significantly after 2 weeks of PTU treatment (337.17 ± 1.30 and 305.10 ± 4.68 g, respectively for controls (N = 18) and hypothyroid rats (N = 18); p < 0.001) and reached a plateau until the end of the experiment [27, 28]. T3 administration to PTU-treated rats had no effect on body weight.
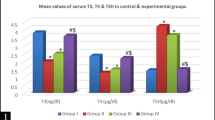
Peripheral thyroid status was evaluated by measuring T3 serum levels after completion of the behavioral tasks. Hypothyroidism was confirmed by the significant 42% reduction in serum T3 levels after 7 weeks of PTU treatment, compared to controls rats (controls 0.68 ± 0.04 ng/ml; PTU 0.39 ± 0.06 ng/ml; p < 0.01). T3 serum level was largely increased in PTU-treated rats that received T3 administration (PTU + T3 2.85 ± 0.28 ng/ml, p < 0.0001 compared to PTU alone).
Hippocampal thyroid-dependent signaling was evaluated by quantification of the thyroid hormone receptor (TR) isoforms (TRα and TRβ) and RC3 mRNA levels, T3 target genes usually used as biomarkers of TH tissue status [16,17,18,19, 38]. One-way ANOVA analyses comparing the three groups revealed a significant effect of T3 status on TRα (F(2, 15) = 6.35, p < 0.05), TRβ (F(2, 15) = 3.69, p < 0.05), and RC3 (F 2, 15) = 6.33, p < 0.05) mRNA levels. PTU treatment induced a significant decrease in TRα, TRβ, and RC3 hippocampal mRNA expression by 32% (post hoc PTU vs controls: p < 0.05), 25% (post hoc PTU vs controls: p < 0.05), and 18% (post hoc PTU vs controls: p < 0.01), respectively (Table 1). These reduced mRNA contents observed after 7 weeks of PTU treatment were also strongly suggestive of a reduction of T3 hippocampal tissue content. T3 administration normalized hippocampal TRα (post hoc PTU + T3 vs PTU: p < 0.001; PTU + T3 vs controls: NS) and RC3 mRNA expression (post hoc PTU + T3 vs PTU: p < 0.001; PTU + T3 vs controls: NS) and, to a lesser extent TRβ mRNA level, although not significantly (+ 18.3%, post hoc PTU + T3 vs PTU: NS) (Table 1). Together, these data indicate hypothyroidism-related decreases in T3 cellular actions in the hippocampus were substantially reversed by T3 treatment.
Cell-Signaling Pathways
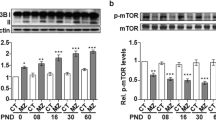
Hippocampal levels of several proteins involved in calcium signaling pathways were analyzed, targeting total and phosphorylated RC3 proteins, CaM, two Ca2+-dependent kinases (CaMKII and CaMKIV) and the Ca2+-dependent phosphatase CaN. Our results (Fig. 4) revealed a significant effect of thyroid status on hippocampal expression of several proteins, with significant changes in expression of RC3 (F(2, 15) = 25.15; p < 0.0001), pRC3 (F(2, 15) = 116.25; p < 0.0001), CaM (F(2, 15) = 7.26; p < 0.01), pCaMKII (F(2, 15) = 5.77; p < 0.05), CaMKIV (F(2, 15) = 4.93; p < 0.05), and CaN (F(2, 15) = 2.21; p < 0.01) (for each protein, post hoc PTU vs controls: p < 0.05). A small, but non-significant decrease in total CaMKII was also observed (F(2, 15) = 1.46; NS). Thus, PTU treatment alone led to the same alteration of Ca2+ signaling-related molecules than that observed previously [28]. Interestingly, T3 administration normalized the expression levels of most of these proteins. Significant increases in protein levels compared to PTU treatment alone were observed for RC3 (post hoc PTU + T3 vs PTU: p < 0.001; controls vs PTU + T3: NS), pRC3 (post hoc PTU + T3 vs PTU: p < 0.01; controls vs PTU + T3: p < 0.01), CaM (post hoc PTU + T3 vs PTU: p < 0.05; controls vs PTU + T3: NS), pCaMKII (post hoc PTU + T3 vs PTU: p < 0.05; PTU + T3 vs controls: NS), and CaN (post hoc PTU + T3 vs PTU: p < 0.01; controls vs PTU + T3: NS) (Fig. 4). Only for CaMKIV, the increase in protein level compared to PTU alone (by about 25%) did not reach statistical significance (post hoc PTU + T3 vs PTU: NS; PTU + T3 vs controls: NS). However, for all proteins examined except pRC3, which was increased above that of the controls, expression levels after T3 supplementation in PTU-treated rats were not significantly different from their levels in control rats.
Effect of thyroid status on hippocampal protein levels for RC3, p-RC3, CaM, CaMkII, pCaMkII, CaMkIV, and CaN. Values in PTU-treated rats (white bars) and PTU-treated rats receiving T3 administration (gray bars) are mean ± SEM (N = 6 per group), expressed as percent of controls (black bars). PTU rats show reduced expression of molecules involved in calcium signaling in the hippocampus. T3 administration restored normal levels of expression of these molecules. *p < 0.05; **p < 0.01 mean values significantly different from control rats. #p < 0.05; ##p < 0.01; ####p < 0.001 mean values significantly different from PTU-treated rats
We then examined expression of several components of the MAPK/ERK pathway, including total and phosphorylated ERK42, ERK44, and P38-MAPK protein kinases, total and phosphorylated CREB and EGR1/ZIF268, proteins known to play a key role in synaptic plasticity and learning and memory. Our results show no significant difference in the expression of total ERK42, ERK44, P38-MAPK, or CREB after PTU treatment compared to controls (F(2, 15) = 4.59, p < 0.05; post hoc PTU vs controls: NS; F(2, 15) = 6.24, p < 0.05; post hoc PTU vs controls: NS; F(2, 15) = 1.51, NS; F(2, 15) = 0.63, NS respectively). In contrast, several changes were induced by PTU treatment in the phosphorylated forms of these proteins, including a decrease in pERK42 (F(2, 15) = 14.84; p < 0.001; post hoc PTU vs controls: p < 0.005) and pCREB (F(2, 15) = 10.42; p < 0.01; post hoc PTU vs controls: p < 0.001) and an increase in pP38-MAPK (F(2, 15) = 7.54; p < 0.05; post hoc PTU vs controls: p < 0.005) (Fig. 5). EGR1 expression was also significantly decreased after PTU treatment (F(2, 15) = 9.76; p < 0.01, post hoc PTU vs controls: p < 0.05). T3 treatment restored normal hippocampal expression of all proteins affected by PTU treatment, increasing expression levels of pERK42 (post hoc PTU + T3 vs PTU: p < 0.001; controls vs PTU + T3: NS), pCREB (post hoc PTU + T3 vs PTU: p < 0.05; PTU + T3 vs controls: NS), and of EGR1 (post hoc PTU + T3 vs PTU: p < 0.05; PTU + T3 vs controls: NS), and decreasing back to control levels that of pP38-MAPK (post hoc PTU + T3 vs PTU: p < 0.01; PTU + T3 vs controls: NS) (Fig. 5). Thus, the altered hippocampal expression of various indicators of active MAPK signaling induced by PTU, up to the expression of the transcription factor EGR1 as described in our previous work [28], can be completely normalized by T3 supplementation.
Effect of thyroid status on hippocampal protein levels for ERK42, pERK42, ERK44, pERK44, P38-MAPK, pP38-MAPK, CREB, pCREB, and EGR1. Values in PTU-treated rats (white bars) and PTU-treated rats receiving T3 administration (gray bars) are mean ± SEM (N = 6 per group), expressed as percent of controls (black bars). Hypothyroid rats show reduced expression of molecules of the MAPK pathway in the hippocampus. T3 administration restored normal levels of expression of these molecules. *p < 0.05; ** p < 0.01; *** p < 0.005; ****p < 0.001 mean values significantly different from control rats. #p < 0.05; ##p < 0.01; ####p < 0.001 mean values significantly different from PTU-treated rats
Inflammatory Response
RT-qPCR and Western blot analyses revealed a relationship between the amount of pro-inflammatory interleukins and thyroid status in the hippocampus. Our results showed that thyroid hormone status modulates the expression of IL1β (F(2, 15) = 6.41; p < 0.01), IL6 (F(2, 15) = 13.00; p < 0.001), and TNFα (F(2, 15) = 7.42; p < 0.01) mRNA levels as well as IL1β (F(2, 15) = 9.46; p < 0.01), and CRP (F(2, 15) = 23.04; p < 0.0001) protein levels. PTU treatment for 7 weeks resulted in significant increases in the expression of IL1β, IL6, and TNFα mRNA levels as well as IL1β and CRP protein levels (for each post hoc PTU vs control: p < 0.05) (Fig. 6). T3 administration fully normalized IL6 (post hoc PTU + T3 vs PTU: p < 0.01; controls vs PTU + T3: NS) and TNFα (post hoc PTU + T3 vs PTU: p < 0.05; controls vs PTU + T3: NS) mRNA changes, as well as the protein expression of IL1β (post hoc PTU + T3 vs PTU: p < 0.01; controls vs PTU + T3: NS) and CRP (post hoc PTU + T3 vs PTU: p < 0.001; controls vs PTU + T3: NS) proteins (Fig. 6).
Effect of thyroid status on mRNA (a) and protein (b) levels of several inflammatory markers in the hippocampus. Values in PTU-treated rats (white bars) and PTU-treated rats receiving T3 administration (gray bars) are mean ± SEM (N = 6 per group), expressed as percent of controls (black bars). Hypothyroidism increased the expression of IL1β, IL6, TNFα, and CRP. T3 treatment restored mRNA and protein levels of pro-inflammatory cytokines and CRP. *p < 0.05, mean values significantly different from control rats. #p < 0.05, ##p < 0.01, ####p < 0.001 mean values significantly different from PTU-treated rats
Amyloid Pathway
We previously showed that adult-onset hypothyroidism can promote the amyloidogenic pathway of amyloid precursor protein processing [27]. As expected, we found that PTU treatment led to an increased expression of APP695 mRNA (F(2, 15) = 6.22, p < 0.05, post hoc PTU vs controls: p < 0.05) associated with an increased level of Aβ42 peptide (F(2, 30) = 29.97; p < 0.0001, post hoc PTU vs controls: p < 0.05) in the hippocampus. T3 administration completely reversed these effects, normalizing both the level of APP695 mRNA (post hoc PTU + T3 vs PTU: p < 0.05; PTU + T3 vs controls: NS) and that of Aβ42 (− 30% compared to PTU alone) (PTU + T3 vs PTU: p < 0.001; PTU + T3 vs controls: NS) (Table 2).
Discussion
In patients suffering hypothyroidism, TH supplementation offers the prospect to alleviate the cognitive consequences of hypothyroidism and reduce the risk of developing cognitive alterations; however, regarding hypothyroidism-induced memory deficits, the therapeutic value of TH supplementation remains unclear and underlying molecular mechanisms remain to be elucidated. We have previously reported that the antithyroid molecule propylthiouracil (PTU) given in the drinking water favors cerebral atrophy, brain neuroinflammation, Aβ production, Tau hyperphosphorylation, and altered plasticity-related cell-signaling pathways in the hippocampus in association with hippocampal-dependent spatial memory deficits [27, 28]. The pattern of changes uncovered likely underlie, at least in part, hypothyroid-related memory impairments largely documented in the literature [9, 13, 39, 40]. The present study clearly shows that hypothyroidism-induced memory deficits are associated to these molecular changes, with hippocampal normalization of T3 signaling, plasticity markers, neuroinflammation, and Aβ production together with hippocampal-dependent memory improvement displayed by PTU-treated rats supplemented with T3. Thus, this study reports that normalization of T3 signaling is associated with improved memory in a model of hypothyroidism.
Hypothyroidism in PTU-treated animals for 7 weeks was evidenced by a significant drop in serum T3 but also T3 hippocampal signaling as compared to controls rats. As expected, T3 administration led to an important increase in serum T3 levels since the analysis was done a relatively short time (12 h) after injection [41]. However, interestingly, despite a relative hyperthyroidism induced by T3 injection at the peripheral level, hypothyroidism-related TR and RC3 mRNA levels in the hippocampus were simply normalized, with no increase of these markers above control levels, the same applying for all plasticity and inflammatory markers and for Aβ production studied. These results indicate, on the one hand, that the peripheral level of T3 does not necessarily reflect brain levels of T3 [42, 43] and, on the other hand, that hippocampal T3 signaling is tightly regulated [44].
In the present work, rats showed a similar behavioral profile in the elevated plus-maze suggesting no specific anxiety-like behavior associated with peripheral or brain levels of T3. In the radial-arm water maze task, a hippocampal-dependent spatial memory task [35, 45], hypothyroid rats showed a transient delay in the early phases of learning and mainly an impairment in memory. In conditions of more extensive practice, when the animals came to perform similarly to controls in the learning phase, performance of hypothyroid rats at both short- and long-term memory tests remained deficient. T3 replacement alleviated both the delay in learning and the deficits in short- and long-term memory observed in PTU-treated rats. These results are comparable with those obtained in 2009 by Alzoubi and collaborators in thyroidectomized rats administrated with thyroxin at a dose that normalized serum T4 and TSH levels [46]. Our present findings thus consolidate the link between T3 cerebral content and hippocampal-dependent spatial memory performance and corroborate those showing a specific defect in hippocampal memory in patients with hypothyroidism. Thus, our rat model offers the possibility to investigate candidate molecular mechanisms underlying impaired memory performance associated with the thyroid status and test the potential preventive value of hormone supplementation approaches.
The MAPK/ERK-CREB and Ca2+/Calmodulin cascades are two major cell-signaling pathways involved in hippocampal synaptic plasticity and memory formation [47,48,49,50]. These pathways control activity-dependent regulation of gene programs via the regulated expression of inducible transcriptions factors such as EGR1/ZIF268, which is required for the expression of synaptic plasticity and hippocampal-dependent memories [22, 51, 52]. Our results in memory-deficient PTU-treated rats show a reduced expression of major components of both MAPK/ERK-CREB (pERK42, pCREB) and Ca2+/calmodulin (RC3, pRC3, CaM, pCaMKII, CaMKIV, and CaN protein levels) signaling pathways, associated with a decrease in EGR1/ZIF268 expression in the hippocampus. Additionally, PTU treatment also led to activation of P38-MAPK, a kinase implicated in synaptic long-term depression [53]. Crucially, T3 administration in PTU-treated rats was able to normalize the level of hippocampal expression of all these proteins. These results showing reversal to basal expression levels of proteins of these signaling pathways after hormone supplementation in our model are coherent with the finding of a restoration of normal levels of LTP-induced MAPK/ERK signaling and CREB phosphorylation in thyroidectomized rats supplemented with T4 [9, 46], and together suggest that this molecular restoration is functional in an activity-dependent context. The exact mechanisms and main target proteins via which TH hormone can lead to reversal of spatial memory deficits remain uncertain. As CREB activation acts as one major hub in the control of the expression of transcriptional regulators such as EGR1/ZIF268 that play an important role in synaptic plasticity and memory, the normalization MAPK/ERK44/42 and CaMKIV, which are reduced in hypothyroidism, and of that of the phosphatase CaN, which is elevated by hypothyroidism are likely to play an important role. In addition, the abnormal increase in active, phosphorylated P38-MAPK as consistently observed in dysthyroidism [28, 54] and, as reported here, the normalization of its expression after T3 supplementation, could also play an important role in the adjustment of pCREB levels and function. It seems at this point parsimonious to suggest that the concerted re-equilibration of several signaling cascades by TH supplementation concur in restoring the capacity for plasticity and memory performance.
Additionally, the present results provide in vivo evidence of a pro-inflammatory reaction associated with hypothyroidism in our rat model. We measured both pro-inflammatory cytokines (i.e., IL1β, IL6, and TNFα) in the hippocampus as markers of glial activation. PTU-treated rats displayed increased expression of IL1β, IL6, and TNFα in the hippocampus. T3 administration also normalized cytokines, therefore strengthening the involvement of a pro-inflammatory response in hypothyroidism. These findings are in line with a few reports suggesting that T3 is an important signaling factor that affects glial functions in the hippocampus [55,56,57]. Our results support the idea that hypothyroidism leads to activation of microglia and astrocytes in a manner sufficient to favor the production of pro-inflammatory cytokines, known to control neuronal function and in particular to impair neuronal plasticity [58, 59]. Moreover, elevated brain pro-inflammatory cytokines is associated with hippocampal-dependent memory deficits [60,61,62]. Thus, the reduction of hypothyroidism-induced brain inflammation by T3 supplementation is likely to concur, in synergy with the restoration of major plasticity-related signaling mechanisms, to the recovery of memory performance in our model. Finally, in rodents, expression of the β amyloid precursor protein (APP) gene is increased in conditions of low levels of TH, suggesting that TH may impact Aβ production [63]. Consistent with this, here, we first show that hypothyroidism favors APP695 mRNA expression associated with an increased level of Aβ42 peptide in the hippocampus, and second, that both APP695 mRNA and Aβ42 peptide levels are normalized by T3 treatment. Given that elevated Aβ42 peptide in the hippocampus can trigger some of the early-onset morphological and functional synaptic plasticity deficits that lead to memory dysfunction, as shown in mouse models of Alzheimer’s disease [64, 65], and can also induce glial cell activation and neuroinflammation, leading to the production of reactive oxygen species, TNF and IL1β [66], the beneficial effect of T3 supplementation on Aβ42 peptide level is also likely to contribute to the recovery of memory function.
The main aim of the present work was to explore the effect of brain T3 signaling replacement on various molecular mechanisms involved in learning and memory. We showed that T3 supplementation in PTU-treated rat model restores hippocampal T3 signaling which associate with normalized hippocampal levels of synaptic plasticity markers, inflammatory mediators, and Aβ peptides. Our data thus supports the proof-of-concept that normalizing T3 hippocampal signaling is sufficient to improve molecular markers signing memory deficits but also memory deficits themselves. The strategy clinically used for the treatment of hypothyroidism generally aims at normalizing the rate of thyroid-stimulating hormone (TSH) production by administration of T4. However, in conditions of overt hypothyroidism, characterized by elevated level of TSH and low levels of serum T3 and T4, thyroid hormone replacement is not always efficient at alleviating cognitive impairments. For instance, Bjerke et al. (2001) found that impaired mood and short-term memory in four cases of hypothyroidism could be only partially improved by TH [67]. Further, Samuels et al. (2007) reported that a group of 34 T4-treated hypothyroid subjects still suffer from decrements in psychological functions, working memory, and motor learning compared to euthyroid subjects [68]. Finally, Correia et al. (2009) reported that spatial memory and associative memory deficits could persist in an overt hypothyroid cohort after L-T4 replacement [69]. Interestingly, recent data showed that combined L-T4 and L-T3 administration, by normalizing all TH-dependent measures including tissue T3 levels, benefits to hypothyroid patients with psychological symptoms, and/or cognitive dysfunction [10, 70, 71]. Further, previous data obtained by Escobar-Morreale and collaborators showed that elevated plasma T3 levels is required for normal cerebral cortex T3 levels in thyroidectomized rats [72]. These authors reported that only the combined treatment with thyroxine and triiodothyronine ensures euthyroidism in all tissues of thyroidectomized rats [73]. These findings strengthen the hypothesis that normalization of TSH by T4 in patients with hypothyroidism that still suffer irreversible cognitive impairments could be due to insufficient brain thyroid hormone replenishment and therefore insufficient molecular compensation, calling attention to the importance of developing approaches to restore a full thyroid-signaling status in the brain, especially in patients with TH metabolism alterations. In turn, our present data are in line with the hypothesis of an ineffectiveness of L-T4 monotherapy treatment in hypothyroid patients with persistent complaints and suggest that brain T3-related signaling is crucial with regard to cognitive impairments, thus adding to the debate concerning the prospect of a T4 + T3 combination therapy in some hypothyroid patients. Finally, our data, by emphasizing the importance of hippocampal-dependent T3 signaling regarding memory deficits, also suggest that beyond TH replacement therapies, the search of alternative molecules able to restore this pathway in patients with hypothyroidism will be of great therapeutic interest in the future.
In conclusion, in the present work, we show that T3 supplementation in hypothyroid rats, which is associated with indicators of normalization of T3 signaling in the hippocampus, reversed the memory deficits and improved neurobiological functions by normalizing both the altered plasticity-related signaling pathways, Aβ42 peptide and pro-inflammatory markers, supporting the importance of brain TH signaling in cognitive abilities. Further, given hypothyroidism represents one important factor influencing the risk for developing AD, that the occurrence of hypothyroidism is recognized in several pathological conditions recognized as risk factors for AD such as aging, obesity, or diabetes, [5,6,7, 74,75,76,77] and that T3 replacement improves pathways impaired in AD, the characterization of the mechanism by which TH level can improve neural functions and alleviate cognitive impairments becomes also critical for the development of preventive approaches in Alzheimer’s disease.
References
Morte B, Bernal J (2014) Thyroid hormone action: astrocyte-neuron communication. Front Endocrinol 5:82. https://doi.org/10.3389/fendo.2014.00082
Raymaekers SR, Darras VM (2017) Thyroid hormones and learning-associated neuroplasticity. Gen Comp Endocrinol 247:26–33. https://doi.org/10.1016/j.ygcen.2017.04.001
Schroeder AC, Privalsky ML (2014) Thyroid hormones, t3 and t4, in the brain. Front Endocrinol 5:40. https://doi.org/10.3389/fendo.2014.00040
Ritchie M, Yeap BB (2015) Thyroid hormone: influences on mood and cognition in adults. Maturitas 81(2):266–275. https://doi.org/10.1016/j.maturitas.2015.03.016
Aggarwal N, Razvi S (2013) Thyroid and aging or the aging thyroid? An evidence-based analysis of the literature. J Thyroid Res 2013:481287–481288. https://doi.org/10.1155/2013/481287
Tan ZS, Vasan RS (2009) Thyroid function and Alzheimer’s disease. J Alzheimers Dis 16(3):503–507
Ganguli M, Burmeister LA, Seaberg EC, Belle S, DeKosky ST (1996) Association between dementia and elevated TSH: a community-based study. Biol Psychiatry 40(8):714–725. https://doi.org/10.1016/0006-3223(95)00489-0
van Osch LA, Hogervorst E, Combrinck M, Smith AD (2004) Low thyroid-stimulating hormone as an independent risk factor for Alzheimer disease. Neurology 62(11):1967–1971
Alzoubi KH, Alkadhi KA (2014) Levothyroxin replacement therapy restores hypothyroidism induced impairment of L-LTP induction: critical role of CREB. Brain Res Bull 100:29–37. https://doi.org/10.1016/j.brainresbull.2013.10.011
McAninch EA, Bianco AC (2016) The history and future of treatment of hypothyroidism. Ann Intern Med 164(1):50–56. https://doi.org/10.7326/M15-1799
Freitas BC, Gereben B, Castillo M, Kallo I, Zeold A, Egri P, Liposits Z, Zavacki AM et al (2010) Paracrine signaling by glial cell-derived triiodothyronine activates neuronal gene expression in the rodent brain and human cells. J Clin Invest 120(6):2206–2217. https://doi.org/10.1172/JCI41977
Cooke GE, Mullally S, Correia N, O'Mara SM, Gibney J (2014) Hippocampal volume is decreased in adults with hypothyroidism. Thyroid 24(3):433–440. https://doi.org/10.1089/thy.2013.0058
Gerges NZ, Alzoubi KH, Park CR, Diamond DM, Alkadhi KA (2004) Adverse effect of the combination of hypothyroidism and chronic psychosocial stress on hippocampus-dependent memory in rats. Behav Brain Res 155(1):77–84. https://doi.org/10.1016/j.bbr.2004.04.003
Artis AS, Bitiktas S, Taskin E, Dolu N, Liman N, Suer C (2012) Experimental hypothyroidism delays field excitatory post-synaptic potentials and disrupts hippocampal long-term potentiation in the dentate gyrus of hippocampal formation and Y-maze performance in adult rats. J Neuroendocrinol 24(3):422–433. https://doi.org/10.1111/j.1365-2826.2011.02253.x
Alzoubi KH, Gerges NZ, Alkadhi KA (2005) Levothyroxin restores hypothyroidism-induced impairment of LTP of hippocampal CA1: electrophysiological and molecular studies. Exp Neurol 195(2):330–341. https://doi.org/10.1016/j.expneurol.2005.05.007
Iniguez MA, Rodriguez-Pena A, Ibarrola N, Aguilera M, Munoz A, Bernal J (1993) Thyroid hormone regulation of RC3, a brain-specific gene encoding a protein kinase-C substrate. Endocrinology 133(2):467–473. https://doi.org/10.1210/endo.133.2.8344193
Husson M, Enderlin V, Alfos S, Boucheron C, Pallet V, Higueret P (2004) Expression of neurogranin and neuromodulin is affected in the striatum of vitamin A-deprived rats. Brain Res Mol Brain Res 123(1-2):7–17. https://doi.org/10.1016/j.molbrainres.2003.12.012
Guadano-Ferraz A, Escamez MJ, Morte B, Vargiu P, Bernal J (1997) Transcriptional induction of RC3/neurogranin by thyroid hormone: differential neuronal sensitivity is not correlated with thyroid hormone receptor distribution in the brain. Brain Res Mol Brain Res 49(1–2):37–44
Piosik PA, van Groenigen M, Baas F (1996) Effect of thyroid hormone deficiency on RC3/neurogranin mRNA expression in the prenatal and adult caprine brain. Brain Res Mol Brain Res 42(2):227–235
Marambaud P, Dreses-Werringloer U, Vingtdeux V (2009) Calcium signaling in neurodegeneration. Mol Neurodegener 4:20. https://doi.org/10.1186/1750-1326-4-20
Koromilas C, Liapi C, Schulpis KH, Kalafatakis K, Zarros A, Tsakiris S (2010) Structural and functional alterations in the hippocampus due to hypothyroidism. Metab Brain Dis 25(3):339–354. https://doi.org/10.1007/s11011-010-9208-8
Bozon B, Davis S, Laroche S (2002) Regulated transcription of the immediate-early gene Zif268: mechanisms and gene dosage-dependent function in synaptic plasticity and memory formation. Hippocampus 12(5):570–577. https://doi.org/10.1002/hipo.10100
Davis S, Bozon B, Laroche S (2003) How necessary is the activation of the immediate early gene zif268 in synaptic plasticity and learning? Behav Brain Res 142(1–2):17–30
Besnard A, Laroche S, Caboche J (2014) Comparative dynamics of MAPK/ERK signalling components and immediate early genes in the hippocampus and amygdala following contextual fear conditioning and retrieval. Brain Struct Funct 219(1):415–430. https://doi.org/10.1007/s00429-013-0505-y
Bianco AC, Salvatore D, Gereben B, Berry MJ, Larsen PR (2002) Biochemistry, cellular and molecular biology, and physiological roles of the iodothyronine selenodeiodinases. Endocr Rev 23(1):38–89
Cooper DS (2005) Antithyroid drugs. N Engl J Med 352(9):905–917
Ghenimi N, Alfos S, Redonnet A, Higueret P, Pallet V, Enderlin V (2010) Adult-onset hypothyroidism induces the amyloidogenic pathway of amyloid precursor protein processing in the rat hippocampus. J Neuroendocrinol 22(8):951–959. https://doi.org/10.1111/j.1365-2826.2010.02002.x
Chaalal A, Poirier R, Blum D, Gillet B, Le Blanc P, Basquin M, Buee L, Laroche S et al (2014) PTU-induced hypothyroidism in rats leads to several early neuropathological signs of Alzheimer’s disease in the hippocampus and spatial memory impairments. Hippocampus 24(11):1381–1393. https://doi.org/10.1002/hipo.22319
Sui L, Wang F, Li BM (2006) Adult-onset hypothyroidism impairs paired-pulse facilitation and long-term potentiation of the rat dorsal hippocampo-medial prefrontal cortex pathway in vivo. Brain Res 1096(1):53–60
Weiss RE, Forrest D, Pohlenz J, Cua K, Curran T, Refetoff S (1997) Thyrotropin regulation by thyroid hormone in thyroid hormone receptor beta-deficient mice. Endocrinology 138(9):3624–3629. https://doi.org/10.1210/endo.138.9.5412
Weiss RE, Murata Y, Cua K, Hayashi Y, Seo H, Refetoff S (1998) Thyroid hormone action on liver, heart, and energy expenditure in thyroid hormone receptor beta-deficient mice. Endocrinology 139(12):4945–4952. https://doi.org/10.1210/endo.139.12.6412
Feart C, Pallet V, Boucheron C, Higueret D, Alfos S, Letenneur L, Dartigues JF, Higueret P (2005) Aging affects the retinoic acid and the triiodothyronine nuclear receptor mRNA expression in human peripheral blood mononuclear cells. Eur J Endocrinol 152(3):449–458
Vallortigara J, Alfos S, Micheau J, Higueret P, Enderlin V (2008) T3 administration in adult hypothyroid mice modulates expression of proteins involved in striatal synaptic plasticity and improves motor behavior. Neurobiol Dis 31(3):378–385
Sapin R, Schlienger JL (2003) Thyroxine (T4) and tri-iodothyronine (T3) determinations: techniques and value in the assessment of thyroid function. Ann Biol Clin (Paris) 61(4):411–420
Diamond DM, Park CR, Heman KL, Rose GM (1999) Exposing rats to a predator impairs spatial working memory in the radial arm water maze. Hippocampus 9(5):542–552. https://doi.org/10.1002/(SICI)1098-1063(1999)9:5<542::AID-HIPO8>3.0.CO;2-N
Lin HB, Yang XM, Li TJ, Cheng YF, Zhang HT, Xu JP (2009) Memory deficits and neurochemical changes induced by C-reactive protein in rats: implication in Alzheimer’s disease. Psychopharmacology 204(4):705–714. https://doi.org/10.1007/s00213-009-1499-2
Kelly A, Laroche S, Davis S (2003) Activation of mitogen-activated protein kinase/extracellular signal-regulated kinase in hippocampal circuitry is required for consolidation and reconsolidation of recognition memory. J Neurosci 23(12):5354–5360
Iniguez MA, Rodriguez-Pena A, Ibarrola N, Morreale de Escobar G, Bernal J (1992) Adult rat brain is sensitive to thyroid hormone. Regulation of RC3/neurogranin mRNA. J Clin Invest 90(2):554–558. https://doi.org/10.1172/JCI115894
Ge JF, Peng L, Hu CM, Wu TN (2012) Impaired learning and memory performance in a subclinical hypothyroidism rat model induced by hemi-thyroid electrocauterisation. J Neuroendocrinol 24(6):953–961. https://doi.org/10.1111/j.1365-2826.2012.02297.x
Rivas M, Naranjo JR (2007) Thyroid hormones, learning and memory. Genes Brain Behav 6(Suppl 1):40–44. https://doi.org/10.1111/j.1601-183X.2007.00321.x
Yu D, Zhou H, Yang Y, Jiang Y, Wang T, Lv L, Zhou Q, Yang Y et al (2015) The bidirectional effects of hypothyroidism and hyperthyroidism on anxiety- and depression-like behaviors in rats. Horm Behav 69:106–115. https://doi.org/10.1016/j.yhbeh.2015.01.003
Gustafson C (2014) Antonio C. Bianco, md, phd: is T4 enough for patients with hypothyroid dysfunction? Integr Med (Encinitas) 13(3):20–22
Bocco BM, Werneck-de-Castro JP, Oliveira KC, Fernandes GW, Fonseca TL, Nascimento BP, McAninch EA, Ricci E et al (2016) Type 2 deiodinase disruption in astrocytes results in anxiety-depressive-like behavior in male mice. Endocrinology 157(9):3682–3695. https://doi.org/10.1210/en.2016-1272
Boelen A, Kwakkel J, Alkemade A, Renckens R, Kaptein E, Kuiper G, Wiersinga WM, Visser TJ (2005) Induction of type 3 deiodinase activity in inflammatory cells of mice with chronic local inflammation. Endocrinology 146(12):5128–5134
Park CR, Zoladz PR, Conrad CD, Fleshner M, Diamond DM (2008) Acute predator stress impairs the consolidation and retrieval of hippocampus-dependent memory in male and female rats. Learn Mem 15(4):271–280. https://doi.org/10.1101/lm.721108
Alzoubi KH, Gerges NZ, Aleisa AM, Alkadhi KA (2009) Levothyroxin restores hypothyroidism-induced impairment of hippocampus-dependent learning and memory: behavioral, electrophysiological, and molecular studies. Hippocampus 19(1):66–78. https://doi.org/10.1002/hipo.20476
Bourtchuladze R, Frenguelli B, Blendy J, Cioffi D, Schutz G, Silva AJ (1994) Deficient long-term memory in mice with a targeted mutation of the cAMP-responsive element-binding protein. Cell 79(1):59–68
Sweatt JD (2001) The neuronal MAP kinase cascade: a biochemical signal integration system subserving synaptic plasticity and memory. J Neurochem 76(1):1–10
Davis S, Vanhoutte P, Pages C, Caboche J, Laroche S (2000) The MAPK/ERK cascade targets both Elk-1 and cAMP response element-binding protein to control long-term potentiation-dependent gene expression in the dentate gyrus in vivo. J Neurosci 20(12):4563–4572
Lisman J, Schulman H, Cline H (2002) The molecular basis of CaMKII function in synaptic and behavioural memory. Nat Rev Neurosci 3(3):175–190. https://doi.org/10.1038/nrn753
Jones MW, Errington ML, French PJ, Fine A, Bliss TV, Garel S, Charnay P, Bozon B et al (2001) A requirement for the immediate early gene Zif268 in the expression of late LTP and long-term memories. Nat Neurosci 4(3):289–296. https://doi.org/10.1038/85138
Veyrac A, Besnard A, Caboche J, Davis S, Laroche S (2014) The transcription factor Zif268/Egr1, brain plasticity, and memory. Prog Mol Biol Transl Sci 122:89–129. https://doi.org/10.1016/B978-0-12-420170-5.00004-0
Thomas GM, Huganir RL (2004) MAPK cascade signalling and synaptic plasticity. Nat Rev Neurosci 5(3):173–183. https://doi.org/10.1038/nrn1346
Bitiktas S, Kandemir B, Tan B, Kavraal S, Liman N, Dursun N, Donmez-Altuntas H, Aksan-Kurnaz I et al (2016) Adult-onset hyperthyroidism impairs spatial learning: possible involvement of mitogen-activated protein kinase signaling pathways. Neuroreport 27(11):802–808. https://doi.org/10.1097/WNR.0000000000000612
Mancini A, Di Segni C, Raimondo S, Olivieri G, Silvestrini A, Meucci E, Curro D (2016) Thyroid hormones, oxidative stress, and inflammation. Mediat Inflamm 2016:6757154. https://doi.org/10.1155/2016/6757154 12
Noda M (2015) Possible role of glial cells in the relationship between thyroid dysfunction and mental disorders. Front Cell Neurosci 9:194. https://doi.org/10.3389/fncel.2015.00194
Cortes C, Eugenin E, Aliaga E, Carreno LJ, Bueno SM, Gonzalez PA, Gayol S, Naranjo D et al (2012) Hypothyroidism in the adult rat causes incremental changes in brain-derived neurotrophic factor, neuronal and astrocyte apoptosis, gliosis, and deterioration of postsynaptic density. Thyroid 22(9):951–963. https://doi.org/10.1089/thy.2010.0400
Yirmiya R, Goshen I (2011) Immune modulation of learning, memory, neural plasticity and neurogenesis. Brain Behav Immun 25(2):181–213. https://doi.org/10.1016/j.bbi.2010.10.015
Delpech JC, Madore C, Nadjar A, Joffre C, Wohleb ES, Laye S (2015) Microglia in neuronal plasticity: influence of stress. Neuropharmacology 96(Pt A):19–28. https://doi.org/10.1016/j.neuropharm.2014.12.034
Barrientos RM, Higgins EA, Sprunger DB, Watkins LR, Rudy JW, Maier SF (2002) Memory for context is impaired by a post context exposure injection of interleukin-1 beta into dorsal hippocampus. Behav Brain Res 134(1–2):291–298
Labrousse VF, Costes L, Aubert A, Darnaudery M, Ferreira G, Amedee T, Laye S (2009) Impaired interleukin-1beta and c-Fos expression in the hippocampus is associated with a spatial memory deficit in P2X(7) receptor-deficient mice. PLoS One 4(6):e6006. https://doi.org/10.1371/journal.pone.0006006
Sparkman NL, Buchanan JB, Heyen JR, Chen J, Beverly JL, Johnson RW (2006) Interleukin-6 facilitates lipopolysaccharide-induced disruption in working memory and expression of other proinflammatory cytokines in hippocampal neuronal cell layers. J Neurosci 26(42):10709–10716. https://doi.org/10.1523/JNEUROSCI.3376-06.2006
O'Barr SA, Oh JS, Ma C, Brent GA, Schultz JJ (2006) Thyroid hormone regulates endogenous amyloid-beta precursor protein gene expression and processing in both in vitro and in vivo models. Thyroid 16(12):1207–1213
Jacobsen JS, Wu CC, Redwine JM, Comery TA, Arias R, Bowlby M, Martone R, Morrison JH et al (2006) Early-onset behavioral and synaptic deficits in a mouse model of Alzheimer’s disease. Proc Natl Acad Sci U S A 103(13):5161–5166. https://doi.org/10.1073/pnas.0600948103
Brouillette J, Caillierez R, Zommer N, Alves-Pires C, Benilova I, Blum D, De Strooper B, Buee L (2012) Neurotoxicity and memory deficits induced by soluble low-molecular-weight amyloid-beta1–42 oligomers are revealed in vivo by using a novel animal model. J Neurosci 32(23):7852–7861. https://doi.org/10.1523/JNEUROSCI.5901-11.2012
Cai Z, Liu N, Wang C, Qin B, Zhou Y, Xiao M, Chang L, Yan LJ et al (2016) Role of RAGE in Alzheimer’s disease. Cell Mol Neurobiol 36(4):483–495. https://doi.org/10.1007/s10571-015-0233-3
Bjerke SN, Bjoro T, Heyerdahl S (2001) Psychiatric and cognitive aspects of hypothyroidism. Tidsskr Nor Laegeforen 121(20):2373–2376
Samuels MH, Schuff KG, Carlson NE, Carello P, Janowsky JS (2007) Health status, psychological symptoms, mood, and cognition in L-thyroxine-treated hypothyroid subjects. Thyroid 17(3):249–258. https://doi.org/10.1089/thy.2006.0252
Correia N, Mullally S, Cooke G, Tun TK, Phelan N, Feeney J, Fitzgibbon M, Boran G et al (2009) Evidence for a specific defect in hippocampal memory in overt and subclinical hypothyroidism. J Clin Endocrinol Metab 94(10):3789–3797. https://doi.org/10.1210/jc.2008-2702
Escobar-Morreale HF, Botella-Carretero JI, Escobar del Rey F, Morreale de Escobar G (2005) REVIEW: treatment of hypothyroidism with combinations of levothyroxine plus liothyronine. J Clin Endocrinol Metab 90(8):4946–4954. https://doi.org/10.1210/jc.2005-0184
Wiersinga WM (2017) Therapy of endocrine disease: T4+T3 combination therapy: is there a true effect? Eur J Endocrinol 177:R287–R296. https://doi.org/10.1530/EJE-17-0645
Escobar-Morreale HF, Obregon MJ, Escobar del Rey F, Morreale de Escobar G (1999) Tissue-specific patterns of changes in 3,5,3′-triiodo-L-thyronine concentrations in thyroidectomized rats infused with increasing doses of the hormone. Which are the regulatory mechanisms? Biochimie 81(5):453–462
Escobar-Morreale HF, del Rey FE, Obregon MJ, de Escobar GM (1996) Only the combined treatment with thyroxine and triiodothyronine ensures euthyroidism in all tissues of the thyroidectomized rat. Endocrinology 137(6):2490–2502. https://doi.org/10.1210/endo.137.6.8641203
Davis JD, Podolanczuk A, Donahue JE, Stopa E, Hennessey JV, Luo LG, Lim YP, Stern RA (2008) Thyroid hormone levels in the prefrontal cortex of post-mortem brains of Alzheimer’s disease patients. Curr Aging Sci 1(3):175–181
Johansson P, Almqvist EG, Johansson JO, Mattsson N, Hansson O, Wallin A, Blennow K, Zetterberg H et al (2013) Reduced cerebrospinal fluid level of thyroxine in patients with Alzheimer’s disease. Psychoneuroendocrinology 38(7):1058–1066. https://doi.org/10.1016/j.psyneuen.2012.10.012
Luo L, Stopa EG (2004) Thyrotropin releasing hormone inhibits tau phosphorylation by dual signaling pathways in hippocampal neurons. J Alzheimers Dis 6(5):527–536
Sampaolo S, Campos-Barros A, Mazziotti G, Carlomagno S, Sannino V, Amato G, Carella C, Di Iorio G (2005) Increased cerebrospinal fluid levels of 3,3′,5′-triiodothyronine in patients with Alzheimer’s disease. J Clin Endocrinol Metab 90(1):198–202
Acknowledgements
We would like to thank Pascale Gisquet-Verrier for her help with behavioral equipment and Fabien Lhericel for animal care.
Funding
This work was supported by Centre National de la Recherche Scientifique (France), University Paris-Sud (France) and by the France Alzheimer/Fédération pour la Recherche sur le Cerveau (AAP France Alzheimer 2013) to V Enderlin. A Chaalal was supported by a doctoral fellowship from the French Ministry of Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Chaalal, A., Poirier, R., Blum, D. et al. Thyroid Hormone Supplementation Restores Spatial Memory, Hippocampal Markers of Neuroinflammation, Plasticity-Related Signaling Molecules, and β-Amyloid Peptide Load in Hypothyroid Rats. Mol Neurobiol 56, 722–735 (2019). https://doi.org/10.1007/s12035-018-1111-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-018-1111-z