Abstract
Thyroid hormone (TH) is essential for brain development, and hypothyroidism induces cognitive deficits in children and young adults. However, the participating mechanisms remain less explored. Here, we examined the molecular mechanism, hypothesizing the involvement of a deregulated autophagy and apoptosis pathway in hippocampal neurons that regulate cognitive functions. Therefore, we used a rat model of developmental hypothyroidism, generated through methimazole treatment from gestation until young adulthood. We detected that methimazole stimulated the autophagy mechanism, characterized by increased LC3B-II, Beclin-1, ATG7, and ATG5–12 conjugate and decreased p-mTOR/mTOR and p-ULK1/ULK1 autophagy regulators in the hippocampus of developing and young adult rats. This methimazole-induced hippocampal autophagy could be inhibited by thyroxine treatment. Subsequently, probing the upstream mediators of autophagy revealed an increased hippocampal neuroinflammation, marked by upregulated interleukin (IL)-1alpha and beta and activated microglial marker, Iba1, promoting neuronal IL-1 receptor-1 expression. Hence, IL-1R-antagonist (IL-1Ra), which reduced hippocampal neuronal IL-1R1, also inhibited the enhanced autophagy in hypothyroid rats. We then linked these events with hypothyroidism-induced apoptosis and loss of hippocampal neurons, where we observed that like thyroxine, IL-1Ra and autophagy inhibitor, 3-methyladenine, reduced the cleaved caspase-3 and TUNEL-stained apoptotic neurons and enhanced Nissl-stained neuronal count in methimazole-treated rats. We further related these molecular results with cognition through Y-maze and passive avoidance tests, demonstrating an IL-1Ra and 3-methyladenine-mediated improvement in learning-memory performances of the hypothyroid rats. Taken together, our study enlightens the critical role of neuroinflammation-dependent autophagy mechanism in TH-regulated hippocampal functions, disrupted in developmental hypothyroidism.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid hormones (TH), triiodothyronine (T3) and thyroxine (T4), are crucial for development and maturation of the central nervous system, playing a key role in prenatal, postnatal, and adult brain functioning [1, 2]. Conversely, TH deficiency, or hypothyroidism, which is prevalent in severely iodine-deficient population or as an autoimmune response of the body, alters neuronal functions, including cognition [3,4,5,6]. The hippocampus is integral to cognitive performances [7], and increased apoptosis and loss of hippocampal neurons and decreased synaptic plasticity appear as key factors for hypothyroidism-induced learning-memory impairments [8, 9]. On the other hand, T4 supplementation improved working memory in terms of cognitive performance scores, particularly during brain development [10, 11]. However, the fundamental mechanisms for hypothyroidism-induced learning-memory deficits and T4-mediated protection at the postnatal stages are less studied.
Autophagy that involves the delivery and degradation or recycling of cytoplasmic material at the lysosomes is important for removing dysfunctional and inessential components from the body. Hence, autophagy has been generally considered to play an intricate balance between cell survival and cell death [12, 13]. At the same time, a dysregulated and uncontrolled autophagy process elicits pathological responses, reported in the brain as well [14, 15]. Particularly, an altered expression of Beclin-1 and microtubule-associated protein 1A/1B-light chain 3 (LC3), which mediate the genesis of autophagosome formation and prompt degradation of autophagic cargo, induces hippocampal neuronal dysfunction. This may also associate with modulated ATG5–12 and ATG7 levels in the hippocampus [16, 17]. Additionally, a deregulated hippocampal autophagy via mammalian target of rapamycin (mTOR) and Unc-51 like autophagy-activating kinase (ULK1) reduced cognitive ability [18].
A distinct link between hippocampal neuronal autophagy and apoptosis-mediated learning and memory decline has been reported, where autophagy protected hippocampal neurons against synaptic impairment and apoptosis [19, 20]. On the contrary, an increased autophagy via reduced p-mTOR/mTOR signaling led to cognitive impairment, involving mitochondrial loss and caspase-3 activation [16]. However, whether TH deficiency affected hippocampal neuronal autophagy and if that correlated with apoptosis and learning-memory loss remain unknown.
The hippocampus of an immature brain is vulnerable to inflammatory insults, with detrimental consequences on cognitive performances. Owing to the significant expression of receptors for inflammatory mediators in the hippocampus, the pro-inflammatory cytokines negatively influence the normal cellular signaling mechanisms, and influence apoptosis as well [21, 22]. With regard to hypothyroidism, there have been reports on the participation of inflammation in hippocampal neurodegeneration and spatial memory impairments at early ages and even after maturation [23,24,25]. However, to the best of knowledge, a direct link between the pro-inflammatory cytokines, apoptosis, and learning-memory loss, along with autophagy, particularly at the developmental stages of TH deficiency awaits investigation.
By using a methimazole-induced rat model of perinatal hypothyroidism through maternal exposure [26, 27], we determined the hippocampal autophagy mechanism in the developing brain. Continuing the methimazole treatment post weaning, we also evaluated the effects on autophagy in young adult rats. We measured neuroinflammation and apoptosis and correlated them with autophagy pathway and ultimate hypothyroidism-induced learning-memory impairment. We also assessed the recovery mechanism through T4 treatment, and overall, identified a novel TH deficiency–induced pathway that reduces hippocampal neuronal cell survival and cognitive functions during development and young adulthood.
Materials and Method
Chemicals and Reagents
Methimazole, l-thyroxine (T4), paraformaldehyde, CelLytic™ MT cell lysis reagent, sodium orthovanadate, protease inhibitor cocktail, DL-dithiothreitol (DTT), sodium dodecyl sulphate, Trizma® base, acrylamide, bis-acrylamide, ammonium sulphate, N,N,N′,N′-tetramethylethylenediamine, bovine serum albumin, TWEEN® 20, sodium citrate, picric acid, in situ cell death detection kit fluorescein for terminal deoxynucleotidyl transferase dUTP nick end labelling (TUNEL), cresyl violet acetate, (3-aminopropyl) triethoxysilane, and TRI Reagent® were procured from Sigma-Aldrich Chemicals Co. (St. Louis, MO). 3-Methyladenine (3-MA), ethanol, glycerol, methanol, acetone, acetic acid, xylene, isopropanol, chloroform, Immobilon-P PVDF membrane, and Immobilon Western Chemiluminescent HRP Substrate were purchased from MilliporeSigma (Burlington, MA). Maxima SYBR Green/ROX qPCR master mix (2×), and horse serum were bought from Thermo Fischer Scientific (Waltham, MA). Superscript™ III first-strand synthesis kit and nuclease free water were purchased from Invitrogen (Carlsbad, CA). Sucrose and DPX mountant were purchased from SRL Pvt. Ltd. (Mumbai, India). Prestained protein ladder was bought from Genetix Biotech Asia Pvt. Ltd. (New Delhi, India). VECTASHIELD antifade mounting medium with DAPI was bought from Vector Laboratories (Burlingame, CA). Interleukin-1receptor antagonist (1IL-1Ra) was procured from R&D systems (Minneapolis, MN).
Antibodies
Rabbit polyclonal ATG7 (cat no. 2631) and ATG5 (cat no. 2630) and rabbit monoclonal phospho-ULK1 (Ser757) (cat no. 14202), ULK1 (cat no. 8054), and cleaved caspase-3 (cat no. 9664) antibodies were from Cell Signaling Technology (Danvers, MA). Rabbit monoclonal phospho-mTOR (S2448) (cat no. ab109268) and mTOR (cat no. ab134903) and rabbit polyclonal IL-1α (cat no. ab7632) and IL-1β (cat no. ab9722) antibodies were from Abcam (Cambridge, UK). Mouse monoclonal Iba1 (cat no. MABN92) antibody was from MilliporeSigma. Rabbit polyclonal LC3B (cat no. L7543), Beclin-1 (cat no. PRS3613) and SQSTM1/p62 (cat no. P0067), mouse monoclonal β-tubulin III (cat no. T8578), and horseradish peroxidase (HRP)-conjugated secondary anti-rabbit (cat no. A0545) antibodies were from Sigma-Aldrich Chemical Co. Rabbit polyclonal IL-1R1 (cat no. sc-689) and HRP-conjugated mouse monoclonal β-Actin (cat no. sc-47778) antibodies were from Santa Cruz Biotechnology, Inc. (Dallas, TX). Alexa Fluor®546 goat anti-rabbit IgG (cat no. A-11010), Alexa Fluor®488 goat anti-rabbit IgG (cat no. A-11008), Alexa Fluor®546 goat anti-mouse IgG (cat no. A-11030), and Alexa Fluor®488 goat anti-mouse IgG (cat no. A-11001) were from Invitrogen.
Animal Treatment
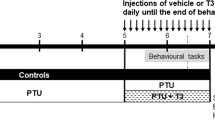
All animal experimental procedures were prior approved (Institutional Animal Ethics Committee of CSIR-CDRI (approval no. IAEC/2020/58/RENEW0) and CSIR-IITR (approval no. IITR/IAEC/75/17–53/19)) and conducted as per the guidelines laid by the Committee for the Purpose of Control and Supervision of Experiments on Animals (CPCSEA), Ministry of Environment and Forests, Government of India. Wistar rat dams were housed under standard conditions of 12 h light/dark at 24 ± 2 °C and 40–60% relative humidity, with ad libitum availability of chow diet and reverse osmosis (R. O.) water. To induce hypothyroidism, methimazole (MZ) (0.025%) in R. O. water [27] was fed to rat dams from gestational day 5 (G05) until weaning, and MZ treatment was continued in the post-weaning rats (mixed gender) until postnatal day (PND) 60. Control rats (CT) received R. O. water. To study the effect of MZ, tissue samples were isolated from the CT and MZ rat sets at PND0, PND08, PND16, PND30, and PND60.
To study the effect of thyroxine supplementation, MZ rats were injected (intraperitoneal route) with T4 (15μg/Kg body weight) or normal saline as the vehicle (V) [26] daily from PND08 to PND16 or PND30 to PND60.
To study whether inflammation and autophagy participated in the hypothyroidism-induced effects, IL-1Ra (5 μl, 350 ng/ml in vehicle, PBS) and autophagy inhibitor 3-MA (5 μl, 300 nM in vehicle, normal saline) respectively were used. They were delivered, once, by the intrahippocampal route, through stereotaxic surgery in MZ rats at PND12 (stereotaxic coordinates: − 2.6 mm from bregma, 2.5 mm (medial-lateral), and 2.5 mm (dorsal-ventral)) [28] or PND50 (stereotaxic coordinates: − 4 mm (anterior-posterior), 2.6 mm (medial-lateral), and 3.5 mm (doral-ventral)) [29] for dissection at PND16 and PND60, respectively, following the protocol described earlier [16, 30]. The corresponding control groups received PBS or normal saline as vehicle (V). Tissue samples were then isolated from the V, MZ, MZ + T4, MZ + IL-1Ra, and MZ + 3-MA rat sets at PND16 and PND60.
Detection of Serum TH Levels
Blood was collected from the heart of anesthetized rats by cardiac puncture, and then centrifuged at 1500g for 10 min to isolate serum. Total T3 and T4 levels in the serum were assessed through radio-immuno assay (RIA) method by the Diagnostic Products Corporation kits (DPC, New York, NY) as done before [27].
Western Blotting
Rats were sacrificed and their brain dissected out. The hippocampal tissues were isolated, snap frozen in liquid nitrogen and stored at − 80 °C until analysis. For western blotting, hippocampal tissues were homogenized in lysis buffer containing protease inhibitor cocktail and DTT, and sodium orthovanadate and sodium fluoride were added for phosphorylated proteins. The lysates were centrifuged (4 °C, 20,000g, 30 min), and protein content in the supernatant estimated by Bradford assay. Protein samples were prepared and equal amount of protein (30–50 μg) was loaded onto each lane. Samples were then run on SDS-PAGE and transferred onto PVDF membrane as described earlier [31]. Blots were blocked with 5% BSA, probed overnight with LC3B, Beclin-1, ATG7, ATG5–12, p62, p-mTOR, mTOR, p-ULK1, ULK1, IL-1α, IL-1β, and IL-1R1 (1:1000) primary antibodies and HRP-conjugated β-actin antibody (1:5000, 2 h). After washing in TBST, the blots (other than β-actin) were probed with HRP-conjugated secondary antibody (1:5000) for 2 h. The blots were then developed in Amersham Imager 600 system (GE Healthcare; Chicago, IL) using Immobilon Western Chemiluminescent HRP Substrate. The protein bands were quantified by Quantity One software (Bio-Rd laboratories; Hercules, CA).
Real-time PCR
RNA was isolated from the hippocampal tissues of rats using the TRI reagent (TRIzol), and cDNA was synthesized using Superscript™ III First-Strand Synthesis kit as described earlier [32]. Real-time PCR was performed using p62 and GAPDH primers (Table 1) and SYBR Green dye following 40 cycles of denaturation (95 °C, 15 s), annealing (60 °C, 30 s), and extension (72 °C, 30 s) steps in real-time PCR Instrument (Applied Biosystems; Foster City, CA). Relative mRNA expression was calculated using RQ = 2−ΔΔCT Method.
Cryosectioning
Towards sample isolation for cryosectioning, rats were anesthetized and trans-cardially perfused with 0.2% picric acid in 4% paraformaldehyde, as described earlier [33]. The whole brain was isolated, cryoprotected in 30% sucrose solution and coronal sections were prepared using a cryomicrotome (Leica Biosystems, Wetzlar, Germany) and taken onto silane-coated slides.
Immunofluorescence
The 10-μm cryosections of the brain from age-matched rats were fixed in acetone and antigen retrieved in citrate buffer, as described earlier [34]. Sections were then blocked in horse serum and probed overnight with IL-1α, IL-1β, IL-1R1, Iba1, β-tubulin III, LC3B, Beclin-1, or cleaved caspase-3 (1:300) primary antibodies, followed by Alexa Fluor secondary antibodies (1:600) for 2 h. The sections were then mounted in mounting medium containing DAPI, and the dentate gyrus region of the hippocampus that plays a key role in memory formation [35] was photographed using a fluorescent microscope (Nikon Instruments Inc.; Minato, Tokyo, Japan). Images from different slides were captured with the same software and constant settings, and processed using the ImageJ software (Wayne Rasband, NIH).
TUNEL Assay
TUNEL assay was performed to detect apoptosis, following the protocol described earlier [33]. The 10-μm cryosections of the brain were fixed in acetone, antigen retrieved in citrate buffer and probed with TdT and fluorescein-labeled dUTP at 37 °C for 2–4 h, while using DNAse I-incubated sections (data not shown) as positive control [36]. Sections were then blocked with horse serum, probed overnight with β-tubulin III antibody (1:300), followed by secondary antibody, and mounted with antifade mounting media containing DAPI. Photomicrographs of the dentate gyrus region of hippocampus were captured under × 10 objective in fluorescent microscope (Nikon Instruments Inc.; Minato, Tokyo, Japan), and images were processed using the ImageJ software (Wayne Rasband, NIH). The % apoptotic index was calculated as number of TUNEL positive nuclei per100 nuclei in β-tubulin III expressing neurons.
Nissl Staining
The 30-μm cryosections of the brain were taken and Nissl staining performed, following the protocol described earlier [37]. Sections were kept in chloroform-ethanol (1:1) mixture for 2–3 h and then in 100% ethanol for 2–3 min. Sections were then stained in cresyl violet (0.1%) solution for 10–15 min, rinsed in water and serially dehydrated in 50, 75, 95, and 100% ethanol. The sections were cleared in xylene, mounted in DPX mounting media and photomicrographs of the dentate gyrus region of hippocampus were captured under × 10 objectives using a Leica DMi1 microscope (Leica Microsystems). The images were exported to the ImageJ software and the number of neurons counted manually from five different random fields per section using Cell counter plugin.
Y-Maze and Passive Avoidance Tests
A Y-maze test was performed to check the learning-memory performance of rats, as described earlier [38]. The Y-maze apparatus consists of three arms, two of which were dark and had foot shock (1–5 mA) (unsafe arms), while the third one had a light cue and was without foot shock (safe arm). On day 1, during learning trials (thirty trials), rats were trained to identify the safe arm, and then memory was checked 24 h, 48 h, and 7 days post learning trials. The apparatus was cleaned between trials. Movement of rats to the unsafe arm was counted as error, and % memory was calculated as (Etraining − Etest) × 100/Etraining.
A separate set of rats was made to undergo passive avoidance test for learning-memory, following an earlier protocol with slight modification [38]. Rats were placed in a gated light-dark chamber, where they were subjected to acquisition in the light chamber (120 s) followed by a foot shock (0.5 mA, 10 s) in the dark chamber. Shock-free retention trials (R1, R2, and R3) after 24 h, 48 h, and 72 h post acquisition were performed and transfer latency time (TLT) was recorded as the time needed by rats to move from light to dark chamber. The chambers were cleaned between trials. Higher TLT indicated better learning-memory ability.
Statistics
Statistical analysis was performed using GraphPad Prism version 6.01 GraphPad Software (La Jolla, CA). Unpaired Student’s t test was performed for analyzing two groups. For analyzing more than two groups, one-way ANOVA was performed, followed by the Tukey’s post hoc multiple-comparisons test. For analyzing more than two groups and more than one parameter, two-way ANOVA followed by the Tukey’s post hoc multiple-comparisons test was carried out.
Results
Effect of MZ Treatment on Hippocampal LC3B and p-mTOR/mTOR in Postnatal Rats
We treated rats with MZ from G05 to PND60 and assessed serum T3 and T4 levels at PND0, PND08, PND16, PND30 and PND60. We detected an MZ-mediated reduction in serum T3 and T4 in the postnatal rats, at almost all the ages (Table 2). We then investigated the effect of MZ on hippocampal autophagy, and detected an increased LC3B-II level (Fig. 1a). We also observed an MZ-mediated decrease in autophagy regulator, p-mTOR/mTOR (Fig. 1b). Our data here indicate a TH deficiency–induced hippocampal autophagy in the postnatal rats.
Hypothyroidism induces hippocampal autophagy in postnatal rats. Hippocampal tissues of PND0, PND08, PND16, PND30, and PND60 rats from control (CT) and methimazole (MZ) sets were isolated. a, b Representative western blots and densitometry relative to CT-PND0 of LC3B-II (16 kDa) normalized with β-actin (42 kDa) (a) and p-mTOR (289 kDa) normalized with mTOR (289 kDa) (b). ***p < 0.001, **p < 0.01, and *p < 0.05 compared with CT of respective age. Data represent means ± SE from three rats of three different litters
Effect of TH Deficiency and T4-Supplementation on Hippocampal Autophagy in Postnatal Rats
To further validate autophagy, we examined the effect of MZ on other important autophagy proteins (besides LC3B), viz. Beclin-1, ATG7, and ATG5–12, and then checked whether T4 treatment had any impact on the hippocampal autophagy. We found that MZ caused an increase in the hippocampal Beclin-1, ATG7, and ATG5–12 levels (Fig. 2a), and T4 treatment not only induced recovery in serum T3 and T4 levels (Table 3) but also reduced the MZ-induced autophagy markers, viz. LC3B-II, Beclin-1, ATG7, and ATG5–12 at both PND16 and PND60, signifying developmental and young adult stages respectively (Fig. 2a). Corroborating the changes in autophagy regulation (as seen in Fig. 1b, showing decreased p-mTOR/mTOR), we observed a reduction in hippocampal p-ULK1/ULK1 in MZ-treated rats and T4-mediated recovery in p-mTOR/mTOR and p-ULK1/ULK1 (Fig. 2b). We next examined the effect of MZ and MZ + T4 on autophagic flux by determining p62 that undergoes degradation in the autophagosomes [39]. We detected an MZ-mediated decrease in hippocampal p62 protein level and its T4-mediated recovery (Fig. 2c). However, we observed an unchanged hippocampal p62 mRNA level following MZ treatment (Fig. 2d), suggesting autophagic degradation rather than a reduced p62 expression for causing P62 protein loss. Thus, our results suggest a hypothyroidism-induced hippocampal autophagy and autophagic flux, and their T4-mediated protection at the postnatal stages.
Hypothyroidism-induced hippocampal autophagy is reduced by T4. Hippocampal tissues of PND16 and PND60 rats from vehicle control (V), MZ or MZ+T4 sets were isolated. a–c Representative western blots and densitometry relative to V of LC3B-II, Beclin-1 (60 kDa), ATG7 (78 kDa), and ATG5–12 (55 kDa) normalized with β-actin (a), p-mTOR normalized with mTOR and p-ULK1 (150 kDa) normalized with ULK1 (150 kDa) (b), and p62 (62 kDa) normalized with β-actin (c) for PND16 (left panel) and PND60 (Right Panel) sets. d mRNA levels relative to V of p62 normalized with GAPDH. ***p < 0.001 and **p < 0.01 compared with V and $$$p < 0.001, $$p < 0.01, and $p < 0.05 compared with MZ. Data represent means ± SE from three rats of three different litters
Effect of TH Deficiency and T4-Supplementation on Hippocampal Neuroinflammation and Its Link with Autophagy in Postnatal Hypothyroid Rats
We then explored the mechanism promoting hippocampal autophagy in the hypothyroid postnatal rats.
It has been reported that the inflammatory cytokine, IL-1, participates in hypothyroidism-induced hippocampal dysfunction, studied in adult rats [23,24,25]. Consistent with the observation, we detected an MZ-induced hippocampal IL-1α (Fig. 3a) and IL-1β (Fig. 3b) in the PND16 and PND60 rats. We also detected a T4-mediated reduction in the MZ-induced IL-1α (Fig. 3a) and IL-1β (Fig. 3b). Activated microglia mediate neuroinflammatory responses [40, 41], and hence, we examined whether MZ affected the microglial activation marker, Iba1. MZ appeared to enhance the hippocampal Iba1 and also caused an increased co-immunolocalization of IL-1α (Fig. 3c) and IL-1β (Fig. 3d) with Iba1, which could be reduced by T4 (Fig. 3c, d). IL-R1 transmits IL-1-induced neuroinflammatory signals [42, 43], and we examined the effect of MZ on hippocampal IL-1R1. We found that MZ upregulated IL-1R1 levels in the hippocampus (Fig. 4a), and also appeared to enhance the co-immunolabeling of IL-1R1 with neuronal marker, β-tubulin III (Fig. 4b), which could be reduced by T4 (Fig. 4a, b). Thus, our results appear to indicate hypothyroidism-induced hippocampal neuroinflammation and T4-mediated protection at the postnatal stages.
Hypothyroidism increases hippocampal IL-1α, IL-1β and microglial activation. Hippocampal tissues of PND16 and PND60 rats from V, MZ, and MZ + T4 sets were isolated. a, b Representative western blots and densitometry relative to V of IL-1α (17 kDa) (a) and IL-1β (17 kDa) (b) normalized with β-actin. **p < 0.01 compared with V and $$p < 0.01 and $p < 0.05 compared with MZ. Data represent means ± SE from three rats of three different litters. Immunofluorescence was performed on brain sections from PND16 and PND60 rats of V, MZ, and MZ + T4 sets. c, d Representative fluorescence photomicrographs (× 40) of the dentate gyrus region of hippocampus in sections co-immuno-stained for IL-1α (c) or IL-1β (d) with Iba1 and co-stained with DAPI. Scale bar: 20 μm. Enlarged: inset area of the merged image. Bar diagrams represent the dual IL-1α (c) or IL-1β (d) and Iba1 + ve counts in the merged photomicrographs, relative to V. **p < 0.01 and *p < 0.05 compared with V and $$p < 0.01 and $p < 0.05 compared with MZ. Data represent means ± SE from three rats of three different litters
Hypothyroidism increases hippocampal neuronal IL-1R1 levels. Hippocampal tissues of PND16 and PND60 rats from V, MZ and MZ + T4 sets were isolated. a Representative western blots and densitometry relative to V of IL-1R1 (80 kDa) normalized with β-actin. ***p < 0.001 and **p < 0.01 compared with V and $$p < 0.01 compared with MZ. Data represent means ± SE from three rats of three different litters. Immunofluorescence was performed on brain sections from PND16 and PND60 rats of V, MZ, and MZ + T4 sets. b Representative fluorescence photomicrographs (× 10) of the dentate gyrus region of hippocampus in sections immuno-stained for IL-1R1 and β-tubulin III, and co-stained with DAPI. Scale bar: 200 μm. Photomicrographs represent brain sections from three rats of three different litters
We then investigated whether this increased IL-1 participated in autophagy mechanism, for which we carried out intrahippocampal infusion of IL-1Ra in the MZ-treated rats. We found that IL-1Ra, which reduced IL-1R1 (Suppl. 1), downregulated hippocampal LC3B-II, Beclin-1, ATG7, and ATG5–12 (Fig. 5a) and increased the p62 (Fig. 5a), p-mTOR/mTOR, and p-ULK1/ULK1 levels (Fig. 5b) in MZ-treated rats, indicating an IL-1-dependent hippocampal autophagy in the postnatal hypothyroid rats.
IL-1Ra reduces hypothyroidism-induced hippocampal autophagy. Hippocampal tissues of PND16 and PND60 rats from V, MZ and MZ + IL-1Ra sets were isolated. a, b Representative western blots and densitometry relative to V of LC3B-II, Beclin-1, ATG7, ATG5–12, and p62 normalized with β-actin (a), and p-mTOR and p-ULK1 normalized with mTOR and ULK1 respectively (b). ***p < 0.001 and **p < 0.01 compared with V and $$$p < 0.001 and $p < 0.05 compared with MZ. Data represent means ± SE from three rats of three different litters. Immunofluorescence was performed on brain sections from PND16 and PND60 rats of V, MZ, MZ + T4, and MZ + IL-1Ra sets. c, d Representative fluorescence photomicrographs (× 10) of the dentate gyrus region of hippocampus in sections co-immuno-stained for LC3B (c) or Beclin-1 (d) with β-tubulin III and co-stained with DAPI. Scale bar: 200 μm. Photomicrographs represent brain sections from three rats of three different litters
We further correlated the increased neuroinflammation with autophagy in the hippocampal neurons, where MZ appeared to enhance the co-immunolabeling of LC3B (Fig. 5c) and Beclin-1 (Fig. 5d) with β-tubulin III, which could be reduced by T4, as well as IL-1Ra (Fig. 5c, d). Thus, our results appear to indicate an IL-1-dependent autophagy in the hippocampal neurons during TH deficiency and T4- or IL-1Ra-mediated protection at postnatal stages.
Effect of T4, IL-1Ra, and 3-MA on Hippocampal Neuronal Apoptosis and Neuronal Density in Postnatal Hypothyroid Rats
Hypothyroidism induces hippocampal neuronal damage [9, 44,45,46], and using IL-1Ra and the autophagy inhibitor, 3-MA, we examined whether the inflammation-dependent autophagy pathway affected the hippocampal neurons of hypothyroid rats. We first verified the effect of 3-MA on hippocampal neurons of MZ-treated rats, showing a reduced LC3B expression (Suppl. 2). We then examined the effect on apoptosis, where MZ appeared to enhance the c-caspase-3 co-immunolabeling with β-tubulin III, which could be reduced by T4, IL-1Ra, and 3-MA (Fig. 6a). Corroborating these findings, we observed an MZ-mediated increased apoptotic TUNEL staining and % apoptotic index in the hippocampal neurons, and their T4, IL-1Ra, and 3-MA-mediated reduction (Fig. 6b).
Hypothyroidism-induced hippocampal neuronal apoptosis is reduced by T4, IL-1Ra, and 3-MA. Immunofluorescence and TUNEL staining were performed on sections from PND16 and PND60 rat brain of V, MZ, MZ + T4, MZ + IL-1Ra, and MZ + 3-MA sets. a Representative fluorescence photomicrographs (× 10) of the dentate gyrus region of hippocampus in sections co-immuno-stained for cleaved caspase-3 with β-tubulin III and co-stained with DAPI. Scale bar: 200 μm. Photomicrographs represent brain sections from three rats of three different litters. b Representative fluorescence photomicrographs (× 10) of the dentate gyrus region of hippocampus in sections stained for TUNEL and β-tubulin III antibody, and co-stained with DAPI. Scale bar: 200 μm. Enlarged: inset area of the merged image. Bar diagram represents Apoptotic index. ***p < 0.001 compared with V and $$p < 0.01 and $p < 0.05 compared with MZ. Data represent means ± SE from three rats of three different litters
Through Nissl staining, we further detected an MZ-mediated decrease in hippocampal neuronal count (%), which (like T4) could be inhibited by IL-1Ra and 3-MA (Fig. 7). Thus, our results indicate a neuroinflammation- and autophagy-dependent increased apoptosis and loss of hippocampal neurons in TH-deficient postnatal rats.
Hypothyroidism-induced hippocampal neuronal loss is reduced by T4, IL-1Ra, and 3-MA. Nissl staining was performed on brain sections from PND16 and PND60 rats of V, MZ, MZ + T4, MZ + IL-1Ra, and MZ + 3-MA sets. Figure shows representative photomicrograph of Nissl-stained dentate gyrus region of hippocampus (× 10). Enlarged: inset area. Bar diagrams represent Neuronal count (%) relative to V. Scale bar: 200 μm. ***p < 0.001 and **p < 0.01 compared with V and $$$p < 0.001 and $$p < 0.01 compared with MZ. Data represent means ± SE from three rats of three different litters
Effect of T4 Supplementation, IL-1Ra, and 3-MA on Learning-Memory Functions in Postnatal Hypothyroid Rats
Hypothyroidism triggers impairment in learning-memory functions that are regulated by hippocampal neurons [9]. Hence, through Y-maze and passive avoidance tests, we assessed whether the MZ-induced hippocampal neuroinflammation and autophagy participated in the learning-memory dysfunctions. We found that like T4, IL-1Ra and 3-MA reduced the error (%) and enhanced the saving memory (%) in Y-maze test (Fig. 8a), and caused significant recovery of the transfer latency time in passive avoidance test (Fig. 8b) in the MZ-treated rats. Thus, our data indicate an increased hippocampal inflammation and autophagy-dependent learning-memory impairment in TH-deficient postnatal stages.
Hypothyroidism-induced learning-memory impairment is reduced by T4, IL-1Ra and 3-MA. Y-maze and passive avoidance tests were performed on PND60 rats of V, MZ, MZ + T4, MZ + IL-1Ra, and MZ + 3-MA sets. a Y-maze data representing the number of errors (%) during learning and the memory retained (% saving memory) at 24 h, 48 h, and 7 days post learning trial. ***p < 0.001 compared with V and $$$p < 0.001, $$p < 0.01, and $p < 0.05 compared with MZ. b Passive avoidance data representing transfer latency time in the first (R1), second (R2), and third (R3) retention trials (24 h, 48 h, and 72 h post acquisition (Aq) trial, respectively). ***p < 0.001 compared with V and $$$p < 0.001 compared with MZ for a particular trial, and ###p < 0.001 compared with acquisition trial. Data represent means ± SE from ten rats of ten different litters
Discussion
The present study reveals a novel mechanism of hypothyroidism-induced cognitive decline during brain development and maturation. We distinctively identified that TH deficiency stimulated hippocampal neuronal autophagy via an inflammation-dependent mechanism, which ultimately emerged as the key reason for neuronal apoptosis and learning-memory loss. TH replenishment or a reduction of the hypothyroidism-induced hippocampal neuroinflammation and autophagy suppressed hippocampal neuronal damage and restored cognitive functions (Fig. 9).
Proposed schematic depicting hypothyroidism-induced hippocampal neuroinflammation and autophagy leading to increased neuronal apoptosis, neuronal loss, and learning-memory dysfunction. Hypothyroidism induces microglial activation, which generates IL-1α and IL-1β and induces neuronal IL-1R1 expression in the hippocampus. This in turn stimulates autophagy and subsequent apoptosis and loss in hippocampal neurons, ultimately resulting in cognitive decline. Inhibition of IL-1 and autophagy pathway, like T4 treatment, reduced the hypothyroidism-induced hippocampal neuronal damage. (The schematic diagram has been created with BioRender.com)
Thyroid hormones have a vital role in influencing neurological and cognitive functions [47, 48], and the current study for the first time reveals the need for a regulated autophagy mechanism in TH-mediated neuroprotection. The findings appeared relevant for both early stages and young adulthood. Our study specifically indicated that TH deficiency stimulates the autophagy process, marked by upregulated Beclin-1 and LC3B-II that are central proteins in the autophagy pathway. Delving into the regulatory components demonstrated an inhibited mTOR1 and ULK1 as important nodes through which the TH deficiency-induced stress responses transmit to the autophagy machinery. Our findings showing increased ATG5–12 conjugate and ATG7 levels (suggestive of upregulated ubiquitin-proteasome system and the extension of phagophoric membrane in autophagic vesicles [17, 49]) corroborated that TH deficiency truly deregulates autophagy via increased cell degradation and recycling within the hippocampus. Additionally, hypothyroidism-mediated reduction in protein and not mRNA levels of the cargo adaptor protein, P62, hints at its own degradation in the process of autophagic flux. It also suggests the delivery of autophagy substrates to autophagosomes for degradation. In the concept of TH-dependent functions, a link between subclinical hypothyroidism and abnormal skeletal development has been reported. The changes associated with a reduced expression of Beclin-1 and LC3-II, upregulated mTOR and decreased autophagosome and p62 accumulation in the chondrocytes [50]. Likewise, in the hypothyroid state, muscle nerve stimulation modulated the autophagy process, conferring TH as a critical predictor of exercise-related muscle conditions [51]. Within the brain, although the involvement of TH-targeted genes in autophagy-related cellular events has been shown for neurological and psychiatric disorders [52], to the best of knowledge, the current study appeared first in identifying the effect of TH deficiency on autophagy in the brain, or more specifically hippocampal neurons. Notably, although we detected that T4 replenishment reduced hypothyroidism-induced hippocampal autophagy, we found that T4 treatment in control rats promoted LC3B-II and beclin-1 levels and decreased mTOR phosphorylation in the hippocampus (Suppl. 3). The latter corresponds with earlier findings demonstrating a hyperthyroidism-induced autophagy in the skeletal muscle [53] and liver [54]. Nonetheless, the differential impact of T4 on the hippocampal autophagy process in control compared with hypothyroidism warrants further investigation, which may be carried out as a separate study. Irrespective of thyroid hormones, there also have been contradictory observations on the role of autophagy in hippocampal functions. On the one hand, hippocampal injections of genetic and pharmacological modulators of autophagy showed that autophagy induction promoted short-term synaptic functions and plasticity, and reduced the age-dependent memory deficits [55]. Contrarily, hippocampal injury in transient hypoxia, long-term ischemia [56, 57], chronic cerebral hypoperfusion [58], and early stages of aging [18] involved an increased autophagy. Matching the current findings, our recent study also demonstrated an augmented autophagy-dependent cognitive impairment in estrogen-deficient females [16], and another report claimed impaired insulin signaling as an inducer of hippocampal autophagy and spatial working memory deficits [59]. Thus, the above studies point to the non-specific or rather situation and condition-dependent pattern in which autophagy participates in hippocampal functions, of which few also strongly express the vital link between hippocampal neuronal autophagy and hormone physiology [16, 59].
In continuation with the concept of endocrine-related effects, studies from a group showed both altered apoptosis and autophagy in relation to neuronal damage [60, 61]. Few studies demonstrated an apoptosis-independent autophagic flux or a switch between apoptotic and autophagic cell death within the hippocampus in situations like withdrawal of insulin hormones, etc. [62,63,64,65]. However, supporting our earlier study, demonstrating estrogen deficiency–induced autophagy and subsequent neuronal apoptosis [16], the current study delineated a strong causal relationship between autophagy and TH deficiency–induced apoptotic hippocampal neuronal cell death. More specifically, it showed enhanced autophagy induction as a requisite for caspase-3-dependent apoptosis, which then critically governed cognitive dysfunction. Moreover, our data showing a decrease in surviving hippocampal neurons using autophagy inhibitor, 3MA, also sustained the concept of an interplay between autophagy and apoptotic pathways in the pathogenesis of neurodegeneration, or the need for an intermediate apoptosis in autophagy-induced neuronal cell death [66, 67].
Corroborating findings from earlier reports [23,24,25], we spotted a hypothyroidism-induced hippocampal interleukin-1 activation and microglial activation, which could be reduced by TH supplementation. Subsequently, delving deeper into the hypothyroidism-induced mechanism revealed neuroinflammation as the pivotal regulator of the autophagy mechanism and its downstream hippocampal neuronal damage. Thyroid hormones have been shown to suppress hepatocellular inflammation and ultimate carcinogenesis involving selective autophagy process [68], while another study, without linking the inflammation and autophagy mechanisms, demonstrated the protective role of T3 in combination with docosahexaenoic acid against inflammasome activation and via enhanced hepatic bioenergetics and lipid homeostasis in ischemia-reperfusion [69]. Thus, an inverse relation between inflammation and autophagy had been generally shown in terms of thyroid hormone functioning, and opposed to that, the current study appears first in linking the thyroid hormone levels with both hippocampal inflammation and autophagy by showing a positive association between the two mechanisms in hypothyroidism or TH-mediated hippocampal recovery. Putting aside thyroid hormone functioning and considering hippocampal inflammation and autophagy as such, studies showed that mutations within the lysosomal-associated membrane protein type-2 (LAMP2) gene, which participates in autophagy and lysosomal degradation of accumulated proteins in neurodegeneration [70], led to inflammation alteration and memory loss [71]. Similarly, drugs activating the autophagy process inhibited the PI3K/AKT/mTOR/ULK1 signaling pathway with a concomitant clearance of hippocampal amyloid beta (Aβ) and reduction in inflammation [72]. Moreover, inhibition of the inflammatory response in the transgenic Alzheimer’s disease (AD) mice models not only reinstated a normal LC3-II and p62 level but also inhibited Aβ accumulation [73]. On the other hand, a decreased cell death and reduced cerebral expression of pro-inflammatory cytokines or autophagy markers in the ATG7 KO mice, as well as upon rosiglitazone or chloroquine treatments and toll-like receptor 4 knockdown following ischemia/reperfusion, traumatic brain injury or radiotherapy-induced neural stem cell and progenitor cell death closely matched our observations in hypothyroidism [74,75,76,77,78,79]. The expression of inflammatory factors at par with the increased Beclin-1, caspase-3 and LC3II/I in focal cerebral ischemia-reperfusion injury [80] also showed a direct link between inflammation and autophagy. Thus, it may be postulated that hippocampal autophagy and inflammation bear an inverse relationship in some situations of neurodegeneration, where the former is essential for clearance of protein oligomers. On the other hand, autophagy and hippocampal inflammation bear a direct relationship in situations, such as hypothyroidism (as observed by us here), etc., culminating in hippocampal neuronal death and damage. Increased hippocampal autophagy downstream of neuroinflammation in the hypothyroid conditions could also be indicative of a defense mechanism for impending neurodegeneration. This may be more relevant for situations like hypothyroidism-induced AD-like pathology [25, 81], marked by hippocampal neurodegeneration. This draws support from earlier studies that indicate an activated autophagy or inhibited mTOR-mediated alleviation in neuronal cell death and memory impairment [82, 83]. Nonetheless, the condition or situation-dependent relationship between hippocampal autophagy, inflammation, and apoptosis, and how thyroid hormones interact in the recovery against neurodegeneration await investigation as an extension to this study.
In conclusion, the present study showed that thyroid hormones play a critical contributory role in sustaining a normal hippocampal autophagy mechanism, which undergoes disruption via interleukin activation, culminating in hippocampal neuronal loss and learning-memory impairment. Moreover, our study proposes microglia and autophagy as important partners in hypothyroidism-induced hippocampal neuronal damage. Accordingly, as suggested earlier [84], it is possible that the aberrant microglial activation has functional consequences in microglial phagocytosis, leading to abnormal engulfment of hippocampal neurons, together with autophagy-induced flux dysregulation and the subsequent apoptotic neuronal cell death. Thus, the crossroads of inflammation, autophagy, apoptosis, and neuronal survival are critical points, which may serve as appropriate targets for reducing cognitive dysfunction in juveniles and adults hypothyroids. Exploring the hypothyroidism-induced dysregulation of glia-neuron communication involving microglial phagocytosis and neuronal autophagy may be a future direction of research to understand the pathophysiological mechanisms associated with hypothyroidism-induced decline in cognitive function.
References
Salazar P, Cisternas P, Martinez M, Inestrosa NC (2019) Hypothyroidism and cognitive disorders during development and adulthood: implications in the central nervous system. Mol Neurobiol 56(4):2952–2963. https://doi.org/10.1007/s12035-018-1270-y
Bernal J (2000) Thyroid hormones in brain development and function. In: Feingold KR, Anawalt B, Boyce A et al. (eds) Endotext. South Dartmouth
Lazarus JH (2002) Epidemiology and prevention of thyroid disease in pregnancy. Thyroid 12(10):861–865. https://doi.org/10.1089/105072502761016485
Vanderpump MP (2011) The epidemiology of thyroid disease. Br Med Bull 99:39–51. https://doi.org/10.1093/bmb/ldr030
Korevaar TI, Muetzel R, Medici M, Chaker L, Jaddoe VW, de Rijke YB, Steegers EA, Visser TJ et al (2016) Association of maternal thyroid function during early pregnancy with offspring IQ and brain morphology in childhood: a population-based prospective cohort study. Lancet Diabetes Endocrinol 4(1):35–43. https://doi.org/10.1016/S2213-8587(15)00327-7
Modesto T, Tiemeier H, Peeters RP, Jaddoe VW, Hofman A, Verhulst FC, Ghassabian A (2015) Maternal mild thyroid hormone insufficiency in early pregnancy and attention-deficit/hyperactivity disorder symptoms in children. JAMA Pediatr 169(9):838–845. https://doi.org/10.1001/jamapediatrics.2015.0498
Sweatt JD (2004) Hippocampal function in cognition. Psychopharmacology 174(1):99–110. https://doi.org/10.1007/s00213-004-1795-9
Salazar P, Cisternas P, Codocedo JF, Inestrosa NC (2017) Induction of hypothyroidism during early postnatal stages triggers a decrease in cognitive performance by decreasing hippocampal synaptic plasticity. Biochim Biophys Acta Mol basis Dis 1863(4):870–883. https://doi.org/10.1016/j.bbadis.2017.01.002
Huang XW, Yin HM, Ji C, Qin YF, Yang RW, Zhao ZY (2008) Effects of perinatal hypothyroidism on rat behavior and its relation with apoptosis of hippocampus neurons. J Endocrinol Investig 31(1):8–15. https://doi.org/10.1007/BF03345560
Ma C, Xie J, Huang X, Wang G, Wang Y, Wang X, Zuo S (2009) Thyroxine alone or thyroxine plus triiodothyronine replacement therapy for hypothyroidism. Nucl Med Commun 30(8):586–593. https://doi.org/10.1097/MNM.0b013e32832c79e0
Sangun O, Demirci S, Dundar N, Pirgon O, Koca T, Dogan M, Dundar B (2015) The effects of six-month L-thyroxine treatment on cognitive functions and event-related brain potentials in children with subclinical hypothyroidism. J Clin Res Pediatr Endocrinol 7(2):102–108. https://doi.org/10.4274/jcrpe.1684
Bossy B, Perkins G, Bossy-Wetzel E (2008) Clearing the brain’s cobwebs: the role of autophagy in neuroprotection. Curr Neuropharmacol 6(2):97–101. https://doi.org/10.2174/157015908784533897
Doherty J, Baehrecke EH (2018) Life, death and autophagy. Nat Cell Biol 20(10):1110–1117. https://doi.org/10.1038/s41556-018-0201-5
Wong E, Cuervo AM (2010) Autophagy gone awry in neurodegenerative diseases. Nat Neurosci 13(7):805–811. https://doi.org/10.1038/nn.2575
Zhu J, Chen X, Song Y, Zhang Y, Zhou L, Wan L (2016) Deficit of RACK1 contributes to the spatial memory impairment via upregulating BECLIN1 to induce autophagy. Life Sci 151:115–121. https://doi.org/10.1016/j.lfs.2016.02.014
Pandey R, Shukla P, Anjum B, Gupta HP, Pal S, Arjaria N, Gupta K, Chattopadhyay N et al (2020) Estrogen deficiency induces memory loss via altered hippocampal HB-EGF and autophagy. J Endocrinol 244(1):53–70. https://doi.org/10.1530/JOE-19-0197
Wesselborg S, Stork B (2015) Autophagy signal transduction by ATG proteins: from hierarchies to networks. Cell Mol Life Sci 72(24):4721–4757. https://doi.org/10.1007/s00018-015-2034-8
Yu Y, Feng L, Li J, Lan X, Lixiang A, Lv X, Zhang M, Chen L (2017) The alteration of autophagy and apoptosis in the hippocampus of rats with natural aging-dependent cognitive deficits. Behav Brain Res 334:155–162. https://doi.org/10.1016/j.bbr.2017.07.003
Li Z, Hao S, Yin H, Gao J, Yang Z (2016) Autophagy ameliorates cognitive impairment through activation of PVT1 and apoptosis in diabetes mice. Behav Brain Res 305:265–277. https://doi.org/10.1016/j.bbr.2016.03.023
Guo HD, Zhu J, Tian JX, Shao SJ, Xu YW, Mou FF, Han XJ, Yu ZH et al (2016) Electroacupuncture improves memory and protects neurons by regulation of the autophagy pathway in a rat model of Alzheimer’s disease. Acupunct Med 34(6):449–456. https://doi.org/10.1136/acupmed-2015-010894
Hagberg H, Gressens P, Mallard C (2012) Inflammation during fetal and neonatal life: implications for neurologic and neuropsychiatric disease in children and adults. Ann Neurol 71(4):444–457. https://doi.org/10.1002/ana.22620
Guo LL, Wang DS, Xu YY, Cui KG (2018) Effects of IL-1beta on hippocampus cell apoptosis and learning ability of vascular dementia rats. Eur Rev Med Pharmacol Sci 22(18):6042–6048. https://doi.org/10.26355/eurrev_201809_15941
Chaalal A, Poirier R, Blum D, Laroche S, Enderlin V (2019) Thyroid hormone supplementation restores spatial memory, hippocampal markers of Neuroinflammation, plasticity-related signaling molecules, and beta-amyloid peptide load in hypothyroid rats. Mol Neurobiol 56(1):722–735. https://doi.org/10.1007/s12035-018-1111-z
Nam SM, Kim JW, Yoo DY, Jung HY, Chung JY, Kim DW, Hwang IK, Yoon YS (2018) Hypothyroidism increases cyclooxygenase-2 levels and pro-inflammatory response and decreases cell proliferation and neuroblast differentiation in the hippocampus. Mol Med Rep 17(4):5782–5788. https://doi.org/10.3892/mmr.2018.8605
Chaalal A, Poirier R, Blum D, Gillet B, Le Blanc P, Basquin M, Buee L, Laroche S et al (2014) PTU-induced hypothyroidism in rats leads to several early neuropathological signs of Alzheimer's disease in the hippocampus and spatial memory impairments. Hippocampus 24(11):1381–1393. https://doi.org/10.1002/hipo.22319
Kumar A, Sinha RA, Tiwari M, Pal L, Shrivastava A, Singh R, Kumar K, Kumar Gupta S et al (2006) Increased pro-nerve growth factor and p75 neurotrophin receptor levels in developing hypothyroid rat cerebral cortex are associated with enhanced apoptosis. Endocrinology 147(10):4893–4903. https://doi.org/10.1210/en.2006-0027
Sinha RA, Khare P, Rai A, Maurya SK, Pathak A, Mohan V, Nagar GK, Mudiam MK et al (2009) Anti-apoptotic role of omega-3-fatty acids in developing brain: perinatal hypothyroid rat cerebellum as apoptotic model. Int J Dev Neurosci 27(4):377–383. https://doi.org/10.1016/j.ijdevneu.2009.02.003
Khazipov R, Zaynutdinova D, Ogievetsky E, Valeeva G, Mitrukhina O, Manent JB, Represa A (2015) Atlas of the postnatal rat brain in stereotaxic coordinates. Front Neuroanat 9:161. https://doi.org/10.3389/fnana.2015.00161
Paxinos G, Watson C (2007) The rat brain in stereotaxic coordinates, 6th edn. Academic Press/Elsevier, Amsterdam
Ashok A, Rai NK, Tripathi S, Bandyopadhyay S (2015) Exposure to As-, Cd-, and Pb-mixture induces Abeta, amyloidogenic APP processing and cognitive impairments via oxidative stress-dependent neuroinflammation in young rats. Toxicol Sci 143(1):64–80. https://doi.org/10.1093/toxsci/kfu208
Tripathi S, Kushwaha R, Mishra J, Gupta MK, Kumar H, Sanyal S, Singh D, Sahasrabuddhe AA et al (2017) Docosahexaenoic acid up-regulates both PI3K/AKT-dependent FABP7-PPARγ interaction and MKP3 that enhance GFAP in developing rat brain astrocytes. J Neurochem 140(1):96–113. https://doi.org/10.1111/jnc.13879
Maurya SK, Rai A, Rai NK, Deshpande S, Jain R, Mudiam MK, Prabhakar YS, Bandyopadhyay S (2012) Cypermethrin induces astrocyte apoptosis by the disruption of the autocrine/paracrine mode of epidermal growth factor receptor signaling. Toxicol Sci 125(2):473–487. https://doi.org/10.1093/toxsci/kfr303
Kushwaha R, Mishra J, Tripathi S, Khare P, Bandyopadhyay S (2018) Arsenic, cadmium, and Lead like troglitazone trigger PPARgamma-dependent poly (ADP-ribose) polymerase expression and subsequent apoptosis in rat brain astrocytes. Mol Neurobiol 55(3):2125–2149. https://doi.org/10.1007/s12035-017-0469-7
Kushwaha R, Mishra J, Gupta AP, Gupta K, Vishwakarma J, Chattopadhyay N, Gayen JR, Kamthan M et al (2019) Rosiglitazone up-regulates glial fibrillary acidic protein via HB-EGF secreted from astrocytes and neurons through PPARγ pathway and reduces apoptosis in high-fat diet-fed mice. J Neurochem 149(5):679–698. https://doi.org/10.1111/jnc.14610
Jonas P, Lisman J (2014) Structure, function, and plasticity of hippocampal dentate gyrus microcircuits. Front Neural Circuits 8:107. https://doi.org/10.3389/fncir.2014.00107
Ohyama K, Farquharson C, Whitehead CC, Shapiro IM (1997) Further observations on programmed cell death in the epiphyseal growth plate: comparison of normal and dyschondroplastic epiphyses. J Bone Miner Res 12(10):1647–1656. https://doi.org/10.1359/jbmr.1997.12.10.1647
Pandey R, Rai V, Mishra J, Mandrah K, Kumar Roy S, Bandyopadhyay S (2017) From the cover: arsenic induces hippocampal neuronal apoptosis and cognitive impairments via an up-regulated BMP2/Smad-dependent reduced BDNF/TrkB signaling in rats. Toxicol Sci 159(1):137–158. https://doi.org/10.1093/toxsci/kfx124
Maurya SK, Mishra J, Abbas S, Bandyopadhyay S (2016) Cypermethrin stimulates GSK3β-dependent Aβ and p-tau proteins and cognitive loss in young rats: reduced HB-EGF signaling and downstream Neuroinflammation as critical regulators. Mol Neurobiol 53(2):968–982. https://doi.org/10.1007/s12035-014-9061-6
Bjorkoy G, Lamark T, Pankiv S, Overvatn A, Brech A, Johansen T (2009) Monitoring autophagic degradation of p62/SQSTM1. Methods Enzymol 452:181–197. https://doi.org/10.1016/S0076-6879(08)03612-4
Dong Y, Xu M, Kalueff AV, Song C (2018) Dietary eicosapentaenoic acid normalizes hippocampal omega-3 and 6 polyunsaturated fatty acid profile, attenuates glial activation and regulates BDNF function in a rodent model of neuroinflammation induced by central interleukin-1beta administration. Eur J Nutr 57(5):1781–1791. https://doi.org/10.1007/s00394-017-1462-7
Ho YH, Lin YT, Wu CW, Chao YM, Chang AY, Chan JY (2015) Peripheral inflammation increases seizure susceptibility via the induction of neuroinflammation and oxidative stress in the hippocampus. J Biomed Sci 22:46. https://doi.org/10.1186/s12929-015-0157-8
Friedman WJ (2001) Cytokines regulate expression of the type 1 interleukin-1 receptor in rat hippocampal neurons and glia. Exp Neurol 168(1):23–31. https://doi.org/10.1006/exnr.2000.7595
Zhang K, Xu H, Cao L, Li K, Huang Q (2013) Interleukin-1beta inhibits the differentiation of hippocampal neural precursor cells into serotonergic neurons. Brain Res 1490:193–201. https://doi.org/10.1016/j.brainres.2012.10.025
Huang XW, Zhao ZY, Ji C (2005) Effects of hypothyroidism on apoptosis and the expression of Bcl-2 and Bax gene in the neonatal rat hippocampus neurons. Zhonghua Er Ke Za Zhi 43(1):48–52
Huang XW, Yang RL, Zhao ZY, Ji C, Yang RW (2005) Mechanism for apoptosis of hippocampus neuron induced by hypothyroidism in perinatal rats. Zhejiang Da Xue Xue Bao Yi Xue Ban 34(4):298–303
Dong J, Liu W, Wang Y, Hou Y, Xi Q, Chen J (2009) Developmental iodine deficiency resulting in hypothyroidism reduces hippocampal ERK1/2 and CREB in lactational and adolescent rats. BMC Neurosci 10:149. https://doi.org/10.1186/1471-2202-10-149
Accorroni A, Chiellini G, Origlia N (2017) Effects of thyroid hormones and their metabolites on learning and memory in normal and pathological conditions. Curr Drug Metab 18(3):225–236. https://doi.org/10.2174/1389200218666170116112407
Raymaekers SR, Darras VM (2017) Thyroid hormones and learning-associated neuroplasticity. Gen Comp Endocrinol 247:26–33. https://doi.org/10.1016/j.ygcen.2017.04.001
Kocaturk NM, Gozuacik D (2018) Crosstalk between mammalian autophagy and the ubiquitin-proteasome system. Front Cell Dev Biol 6:128. https://doi.org/10.3389/fcell.2018.00128
Xin W, Yu Y, Ma Y, Gao Y, Xu Y, Chen L, Wan Q (2017) Thyroid-stimulating hormone stimulation downregulates autophagy and promotes apoptosis in chondrocytes. Endocr J 64(7):749–757. https://doi.org/10.1507/endocrj.EJ16-0534
Zhou J, Parker DC, White JP, Lim A, Huffman KM, Ho JP, Yen PM, Kraus WE (2019) Thyroid hormone status regulates skeletal muscle response to chronic motor nerve stimulation. Front Physiol 10:1363. https://doi.org/10.3389/fphys.2019.01363
Napolitano F, D'Angelo L, de Girolamo P, Avallone L, de Lange P, Usiello A (2018) The thyroid hormone-target gene Rhes a novel crossroad for neurological and psychiatric disorders: new insights from animal models. Neuroscience 384:419–428. https://doi.org/10.1016/j.neuroscience.2018.05.027
Lesmana R, Sinha RA, Singh BK, Zhou J, Ohba K, Wu Y, Yau WW, Bay BH et al (2016) Thyroid hormone stimulation of autophagy is essential for mitochondrial biogenesis and activity in skeletal muscle. Endocrinology 157(1):23–38. https://doi.org/10.1210/en.2015-1632
Sinha RA, You SH, Zhou J, Siddique MM, Bay BH, Zhu X, Privalsky ML, Cheng SY et al (2012) Thyroid hormone stimulates hepatic lipid catabolism via activation of autophagy. J Clin Invest 122(7):2428–2438. https://doi.org/10.1172/JCI60580
Glatigny M, Moriceau S, Rivagorda M, Ramos-Brossier M, Nascimbeni AC, Lante F, Shanley MR, Boudarene N et al (2019) Autophagy is required for memory formation and reverses age-related memory decline. Curr Biol 29(3):435–448 e438. https://doi.org/10.1016/j.cub.2018.12.021
Li L, Zhang Q, Tan J, Fang Y, An X, Chen B (2014) Autophagy and hippocampal neuronal injury. Sleep Breath 18(2):243–249. https://doi.org/10.1007/s11325-013-0930-4
Sun L, Gao J, Zhao M, Cui J, Li Y, Yang X, Jing X, Wu Z (2015) A novel cognitive impairment mechanism that astrocytic p-connexin 43 promotes neuronic autophagy via activation of P2X7R and down-regulation of GLT-1 expression in the hippocampus following traumatic brain injury in rats. Behav Brain Res 291:315–324. https://doi.org/10.1016/j.bbr.2015.05.049
Zou W, Song Y, Li Y, Du Y, Zhang X, Fu J (2018) The role of autophagy in the correlation between neuron damage and cognitive impairment in rat chronic cerebral Hypoperfusion. Mol Neurobiol 55(1):776–791. https://doi.org/10.1007/s12035-016-0351-z
Woo H, Hong CJ, Jung S, Choe S, Yu SW (2018) Chronic restraint stress induces hippocampal memory deficits by impairing insulin signaling. Mol Brain 11(1):37. https://doi.org/10.1186/s13041-018-0381-8
Chung H, Kim E, Lee DH, Seo S, Ju S, Lee D, Kim H, Park S (2007) Ghrelin inhibits apoptosis in hypothalamic neuronal cells during oxygen-glucose deprivation. Endocrinology 148(1):148–159. https://doi.org/10.1210/en.2006-0991
Chung H, Choi J, Park S (2018) Ghrelin protects adult rat hippocampal neural stem cells from excessive autophagy during oxygen-glucose deprivation. Endocr J 65(1):63–73. https://doi.org/10.1507/endocrj.EJ17-0281
Yu SW, Baek SH, Brennan RT, Bradley CJ, Park SK, Lee YS, Jun EJ, Lookingland KJ et al (2008) Autophagic death of adult hippocampal neural stem cells following insulin withdrawal. Stem Cells 26(10):2602–2610. https://doi.org/10.1634/stemcells.2008-0153
Baek SH, Kim EK, Goudreau JL, Lookingland KJ, Kim SW, Yu SW (2009) Insulin withdrawal-induced cell death in adult hippocampal neural stem cells as a model of autophagic cell death. Autophagy 5(2):277–279. https://doi.org/10.4161/auto.5.2.7641
Ha S, Ryu HY, Chung KM, Baek SH, Kim EK, Yu SW (2015) Regulation of autophagic cell death by glycogen synthase kinase-3beta in adult hippocampal neural stem cells following insulin withdrawal. Mol Brain 8:30. https://doi.org/10.1186/s13041-015-0119-9
Chung KM, Park H, Jung S, Ha S, Yoo SJ, Woo H, Lee HJ, Kim SW et al (2015) Calpain determines the propensity of adult hippocampal neural stem cells to autophagic cell death following insulin withdrawal. Stem Cells 33(10):3052–3064. https://doi.org/10.1002/stem.2082
Chung Y, Lee J, Jung S, Lee Y, Cho JW, Oh YJ (2018) Dysregulated autophagy contributes to caspase-dependent neuronal apoptosis. Cell Death Dis 9(12):1189. https://doi.org/10.1038/s41419-018-1229-y
Ginet V, Spiehlmann A, Rummel C, Rudinskiy N, Grishchuk Y, Luthi-Carter R, Clarke PG, Truttmann AC et al (2014) Involvement of autophagy in hypoxic-excitotoxic neuronal death. Autophagy 10(5):846–860. https://doi.org/10.4161/auto.28264
Chi HC, Chen SL, Tsai CY, Chuang WY, Huang YH, Tsai MM, Wu SM, Sun CP et al (2016) Thyroid hormone suppresses hepatocarcinogenesis via DAPK2 and SQSTM1-dependent selective autophagy. Autophagy 12(12):2271–2285. https://doi.org/10.1080/15548627.2016.1230583
Videla LA (2019) Combined docosahexaenoic acid and thyroid hormone supplementation as a protocol supporting energy supply to precondition and afford protection against metabolic stress situations. IUBMB Life 71(9):1211–1220. https://doi.org/10.1002/iub.2067
Xilouri M, Brekk OR, Landeck N, Pitychoutis PM, Papasilekas T, Papadopoulou-Daifoti Z, Kirik D, Stefanis L (2013) Boosting chaperone-mediated autophagy in vivo mitigates alpha-synuclein-induced neurodegeneration. Brain 136(Pt 7):2130–2146. https://doi.org/10.1093/brain/awt131
Rothaug M, Stroobants S, Schweizer M, Peters J, Zunke F, Allerding M, D'Hooge R, Saftig P et al (2015) LAMP-2 deficiency leads to hippocampal dysfunction but normal clearance of neuronal substrates of chaperone-mediated autophagy in a mouse model for Danon disease. Acta Neuropathol Commun 3:6. https://doi.org/10.1186/s40478-014-0182-y
Fan L, Qiu XX, Zhu ZY, Lv JL, Lu J, Mao F, Zhu J, Wang JY et al (2019) Nitazoxanide, an anti-parasitic drug, efficiently ameliorates learning and memory impairments in AD model mice. Acta Pharmacol Sin 40(10):1279–1291. https://doi.org/10.1038/s41401-019-0220-1
Alvarez-Arellano L, Pedraza-Escalona M, Blanco-Ayala T, Camacho-Concha N, Cortes-Mendoza J, Perez-Martinez L, Pedraza-Alva G (2018) Autophagy impairment by caspase-1-dependent inflammation mediates memory loss in response to beta-amyloid peptide accumulation. J Neurosci Res 96(2):234–246. https://doi.org/10.1002/jnr.24130
Wang Y, Zhou K, Li T, Xu Y, Xie C, Sun Y, Zhang Y, Rodriguez J et al (2017) Inhibition of autophagy prevents irradiation-induced neural stem and progenitor cell death in the juvenile mouse brain. Cell Death Dis 8(3):e2694. https://doi.org/10.1038/cddis.2017.120
Cui CM, Gao JL, Cui Y, Sun LQ, Wang YC, Wang KJ, Li R, Tian YX et al (2015) Chloroquine exerts neuroprotection following traumatic brain injury via suppression of inflammation and neuronal autophagic death. Mol Med Rep 12(2):2323–2328. https://doi.org/10.3892/mmr.2015.3611
Shao ZQ, Liu ZJ (2015) Neuroinflammation and neuronal autophagic death were suppressed via rosiglitazone treatment: new evidence on neuroprotection in a rat model of global cerebral ischemia. J Neurol Sci 349(1–2):65–71. https://doi.org/10.1016/j.jns.2014.12.027
Li J, Yang F, Guo J, Zhang R, Xing X, Qin X (2015) 17-AAG post-treatment ameliorates memory impairment and hippocampal CA1 neuronal autophagic death induced by transient global cerebral ischemia. Brain Res 1610:80–88. https://doi.org/10.1016/j.brainres.2015.03.051
Xu M, Pirtskhalava T, Farr JN, Weigand BM, Palmer AK, Weivoda MM, Inman CL, Ogrodnik MB et al (2018) Senolytics improve physical function and increase lifespan in old age. Nat Med 24(8):1246–1256. https://doi.org/10.1038/s41591-018-0092-9
Jiang H, Wang Y, Liang X, Xing X, Xu X, Zhou C (2018) Toll-like receptor 4 knockdown attenuates brain damage and neuroinflammation after traumatic brain injury via inhibiting neuronal autophagy and astrocyte activation. Cell Mol Neurobiol 38(5):1009–1019. https://doi.org/10.1007/s10571-017-0570-5
Zhu Y, Li S, Liu J, Wen Q, Yu J, Yu L, Xie K (2019) Role of JNK signaling pathway in Dexmedetomidine post-conditioning-induced reduction of the inflammatory response and autophagy effect of focal cerebral ischemia reperfusion injury in rats. Inflammation 42(6):2181–2191. https://doi.org/10.1007/s10753-019-01082-2
Ghenimi N, Alfos S, Redonnet A, Higueret P, Pallet V, Enderlin V (2010) Adult-onset hypothyroidism induces the amyloidogenic pathway of amyloid precursor protein processing in the rat hippocampus. J Neuroendocrinol 22(8):951–959. https://doi.org/10.1111/j.1365-2826.2010.02002.x
Srivastava IN, Shperdheja J, Baybis M, Ferguson T, Crino PB (2016) mTOR pathway inhibition prevents neuroinflammation and neuronal death in a mouse model of cerebral palsy. Neurobiol Dis 85:144–154. https://doi.org/10.1016/j.nbd.2015.10.001
Pan J, He L, Li X, Li M, Zhang X, Venesky J, Li Y, Peng Y (2017) Activating autophagy in hippocampal cells alleviates the morphine-induced memory impairment. Mol Neurobiol 54(3):1710–1724. https://doi.org/10.1007/s12035-016-9735-3
Plaza-Zabala A, Sierra-Torre V, Sierra A (2017) Autophagy and microglia: novel partners in neurodegeneration and aging. Int J Mol Sci 18(3):598. https://doi.org/10.3390/ijms18030598
Acknowledgments
The first author was supported by the fellowship from Council of Scientific and Industrial Research (CSIR), New Delhi. Dr. Rohit A. Sinha, Assistant Prof & Wellcome Trust/DBT Fellow, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, provided valuable suggestions for the autophagy experiments. CSIR-IITR manuscript number is 3640.
Funding
This study was supported by the Science and Engineering Research Board, Govt. of India (GAP340).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
: IL-1Ra reduces hypothyroidism-induced hippocampal IL-R1. Hippocampal tissues of PND16 and PND60 rats from V, MZ and MZ+IL-1Ra sets were isolated. Figure shows representative western blots and densitometry relative to V of IL-1R1 normalized with β-actin. **p<0.01 compared to V and $$p<0.01 and $p<0.05 compared to MZ. Data represent means ± SE from three rats of three different litters. (PNG 427 kb)
ESM 2
: 3-MA reduces hypothyroidism-induced LC3B levels in hippocampal neurons. Immunofluorescence was performed on sections from PND16 and PND60 rat brain of V, MZ and MZ+3-MA sets. Figure shows representative fluorescence photomicrographs (10x) of the dentate gyrus region of hippocampus in sections co-immuno-stained for LC3 with β-tubulin III, and co-stained with DAPI. Scale bar: 200 μm. Photomicrographs represent brain sections from three rats of three different litters. (PNG 320 kb)
ESM 3
: T4 treatment induces hippocampal autophagy in postnatal rats. Hippocampal tissues of PND16 and PND60 rats from V and T4 sets were isolated. Figure shows representative western blots and densitometry relative to V of LC3B-II and Beclin-1 normalized with β-actin, and p-mTOR normalized with mTOR for PND16 (Left Panel) and PND60 (Right Panel) sets. ***p<0.001, **p<0.01 and *p<0.05 compared to V. Data represent means ± SE from three rats of three different litters (PNG 484 kb)
Rights and permissions
About this article
Cite this article
Mishra, J., Vishwakarma, J., Malik, R. et al. Hypothyroidism Induces Interleukin-1-Dependent Autophagy Mechanism as a Key Mediator of Hippocampal Neuronal Apoptosis and Cognitive Decline in Postnatal Rats. Mol Neurobiol 58, 1196–1211 (2021). https://doi.org/10.1007/s12035-020-02178-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-020-02178-9