Abstract
Fat and bone have a complicated relationship. Although obesity has been associated with low fracture risk, there is increasing evidence that some of the factors that are released by peripheral fat into the circulation may also have a deleterious effect on bone mass, thus, predisposing to fractures. More importantly, the local interaction between fat and bone within the bone marrow seems to play a significant role in the pathogenesis of age-related bone loss and osteoporosis. This “local interaction” occurs inside the bone marrow and is associated with the autocrine and paracrine release of fatty acids and adipokines, which affect the cells in their vicinity including the osteoblasts, reducing their function and survival. In this review, we explore the particularities of the fat and bone cell interactions within the bone marrow, their significance in the pathogenesis of osteoporosis, and the potential therapeutic applications that regulating marrow fat may have in the near future as a novel pharmacologic treatment for osteoporosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a major public health problem that affects nearly 75 million people around the world and causes more than 2 million fractures annually [1]. This creates a major health burden by costing billions annually and causing significant morbidity and mortality within the older population.
The pathophysiology of osteoporosis has been associated with a misbalance between bone formation and resorption [2]. During the menopause, bone resorption by the osteoclasts is increased, thus inducing a significant bone loss [3], whereas with aging there is a significant reduction in bone formation due to low number and function of the bone forming osteoblasts [4]. More recently, a third pathophysiological mechanism for osteoporosis has been proposed involving the increasing presence of fat within the bone marrow, which is known to affect osteoblast differentiation and function, while increasing osteoclastic activity and also affecting mineralization [5, 6].
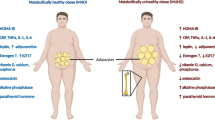
In fact, the relationship between fat and bone is complex. Several studies have differentiated this relationship into either systemic (endocrine) or local (auto and paracrine) [7, 8•]. The systemic interaction between fat and bone refers to those factors that are released by peripheral fat (subcutaneous, visceral, etc) and affect bone metabolism either in a negative or positive manner [4, 9]. In contrast, the local relationship refers to the activity of fat within the bone marrow milieu and its interaction with other bone cells [7].
Interest in the systemic effect of fat on bone has increased in recent years mostly due to the obesity epidemic. Some studies have reported that obesity reduces the risk for osteoporosis and that low body weight is a major risk for fractures [9, 10]. However, more recent evidence indicates that obesity could be detrimental to bone and that there is an inverse relationship between body mass index, bone mineral density and bone formation [11•, 12, 13]. Although this negative systemic effect of fat on bone metabolism has been associated with circulating adipokines, the mechanism of this deleterious effect remains unclear.
In contrast, the local relationship between fat and bone has been better understood and extensively explored in the last years. In this review, we summarize the current understanding on the role of marrow fat in bone metabolism, its interaction with other cells in the bone marrow milieu and the potential therapeutic applications that regulating marrow fat volume and activity would have on bone formation (Fig. 1).
Fat and bone relationship within the bone marrow milieu. MSCs differentiate toward osteogenic and adipogenic lineage. MSCs are stimulated by either osteogenic or adipogenic factors at each stage of differentiation. Furthermore, fatty acids and adipokines released by adipocytes are toxic and block the osteoblast differentiation pathway. BMP Bone morphogenic protein, C/EBPαβ CCAAT/enhancer binding protein alpha and beta, ECM extracellular matrix, OSX Osterix
The Multicellular Bone Marrow Milieu: Cell Differentiation and Their Interactions
The bone marrow is a complex environment, in which a variety of cell types share a common space locally releasing cytokines and growth factors that could affect the cells in their vicinity. Major cellular groups within the bone marrow include blood cells, bone mass-regulating cells (osteoblasts and osteoclasts), and marrow adipocytes [14••].
In terms of their origin, mesenchymal precursors give rise to osteoblast, adipocytes and chondrocytes whereas blood cells are derived from hematopoietic stem cells. On the other hand, osteoclasts are derived from hematopoietic monocytes or macrophages [15]. Although both hematopoietic and mesenchymal precursors are present during the embryonic and early stages of life, marrow fat (yellow fat) only acquire significant levels during the second decade of life [16] in a process of progressive infiltration of the bone marrow space, which finally occupies a significant proportion of the bone marrow [17, 18•]. In addition, this increase in adipocyte number and volume is associated with reduced hematopoietic function and decreased osteogenesis [19].
The first local linkage between bone and fat relies on their cellular origin. Osteoblasts and marrow adipocytes derive from bone marrow mesenchymal stem cells (MSCs), which must not only differentiate but also proliferate in order to reach the appropriate cell numbers required for tissue regeneration, growing, and repair. Human MSCs fulfill the following characteristics: (1) have a specific antigenic profile that includes CD9+, CD54+, CD73+, CD90+, CD105+, CD166+, CD29+, CD44+, CD14-, CD19-, CD31-, CD34-, CD45-, HLA-DR-, and Nestin + [20•]; (2) show a fibroblast-like morphology in culture with significant adherence to tissue culture plastic; (3) are isolated from specific niches in postnatal tissues, principally from bone marrow; (4) can remain undifferentiated and have the multipotent in vitro capacity to differentiate into mesenchymal lineage such as osteoblasts, adipocytes, chondrocytes and myoblasts [21–24, 25••]. Finally, MSCs show low immunogenicity and have pro-angiogenic and anti-inflammatory properties, which made them attractive not only for preventing the graft-versus-host disease and modulating the immune system after transplantation [26], but also to be used in regenerative medicine [21] and antitumor therapy [27].
Indeed, the main and most studied source of MSCs is still the bone marrow [28] with other diverse sources such as peripheral blood and subcutaneous fat being tested as alternative sources, which would facilitate their collection and culture in a less invasive way. However, the plasticity of MSCs from those extra medullar sources compared as bone marrow MSCs is limited [29••]. In vitro, non-bone marrow MSCs have a reduced capacity to proliferate and differentiate and also show variable characteristics changing according to the culture conditions [20•, 30].
Although present in a very low numbers under physiological conditions, minimal quantities of MSCs are required to support bone formation during development and adulthood. However, their numbers normally decrease after estrogen withdraw and during ageing [22, 31]. These changes in MSC number within the bone marrow environment would contribute to a shifting of MSC differentiation into an adipogenic lineage instead of an osteogenic one, which has been a common finding in in vivo and ex vivo studies [22, 31].
In contrast, in vitro studies have been less successful in mimicking the fat and bone interaction. This is due to the fact that in vitro models, although allowing the control of several factors such as the cell number and conditioning media, critically impede to simulate the marrow microenvironment where cells and their products interact in a reciprocal crosstalk. With regard to these limitations, biomedical engineers have developed 3D systems of co- and triculture with artificial mineral-coated scaffolds, thus, mimicking the mineralized extracellular matrix and allowing a paracrine multiple-way cellular interaction [32, 33]. Others have replaced the usual conditioning media with supernatants of other bone marrow cells in culture, thus, exposing MSCs to factors present in the bone marrow milieu [32]. Our group has used a different approach by testing the interaction between fat and bone cells in vitro separated by a porous membrane, which allows growth factors and cytokines to unidirectionally flow into the other cell group [34].
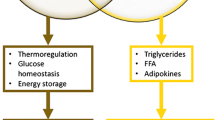
Indeed, there is enough evidence to suggest that, in the process of osteogenic differentiation of MSCs, an inverse relationship is established, in which mechanisms that promote osteoblastogenesis prevent adipogenesis and vice versa [35, 36]. Certain states such as ageing [7], metabolic diseases such as diabetes mellitus [37], estrogen withdrawal [38], immobilization [39], and glucocorticoid treatment [40] favor fat accumulation at the expense of bone formation. Overall, these risk factors induce the MSC to switch into its default lineage, which is considered to be adipocytic. In addition to high levels of adipogenesis observed in these conditions, it has been demonstrated that adipocytes products (fatty acids and adipokines) potentiate this negative scenario in a vicious circle, which has been termed as lipotoxicity [8]. Finally, other cellular and molecular changes associated with ageing such as bigger MSC size, diminished differentiation potential, proliferation and growth rate as well as shortened telomeres could affect the capacity of MSCs to differentiate into osteoblasts while increase their adipocytic differentiation [22].
Molecular Mechanisms of Adipogenesis vs Osteoblastogenesis
The ultimate major controllers of the switching of a MSC toward either osteogenic or adipogenic lineages are runt-related transcription factor 2 (RUNX2) [41] for osteogenesis and the peroxisome proliferator-activated receptor-γ (PPARγ) [42] for adipogenesis, with many regulating routes and epigenetic factors being directly or indirectly involved [43•]. To reach the nucleus and to form their DNA-binding complex, RUNX2 and PPARγ should interact with a set of elements of osteogenic and adipogenic pathways, respectively. The most important pathway involved in these 2 differentiation processes is known as canonical Wnt/β-Catenin pathway (Fig. 1). Pro-osteogenic Wnts such as Wnt10b, Wnt1, Wnt6, Wnt7a, and Wnt10a are soluble proteins that prevent β-Catenin degradation and ultimately allow its nuclear translocation to form transcriptional complexes along with Tcf/Lef (T-cell factor/lymphoid enhancer-binding factor) and RUNX2, thus, stimulating osteogenic commitment of MSCs [44]. This process stimulates mineralization and alkaline phosphatase (ALP) activity in pre-osteoblasts [45] while inducing osteoprotegerin (OPG) expression, thus, indirectly downregulating bone resorption.
Considering that this is a highly regulated pathway, the exact mechanism by which the Wnt ligands and β-Catenin regulate MSCs differentiation within the bone marrow remains partially understood. Mutations in several up or down stream components and controllers of the Wnt/β-Catenin signaling pathway have been associated with bone-related diseases either by up- or downregulating osteogenic genes, thus, causing sclerosteosis or osteoporosis [46–49]. During osteogenesis, several pro-osteogenic Wnt proteins crosstalk and then bind to low-density lipoprotein (LDL) receptor–related proteins 5 and 6 (LRP5/6). This communication, which is followed by β-Catenin translocation, promotes osteoblastogenesis while blocks adipogenesis [50•]. In contrast, the presence of other group of Wnt proteins such as Wnt4, Wnt5a, and Wnt5b blocks these interactions, facilitate the degradation of β-Catenin and induce adipogenesis [51].
In addition, there are also secreted antagonists of the Wnt/ β-Catenin pathway that could affect osteoblast differentiation and function. Sclerostin, which is a protein encoded by the SOST gene and is exclusively produced by the osteocytes, binds to the Wnt co-receptors LRP5/6 in osteoblasts to block the Wnt/β-Catenin signaling pathway while increases osteoblast apoptosis [52]. In contrast, mechanical loading sensed by osteocytes, and parathyroid hormone (PTH) diminish sclerostin production and favor osteoblastogenesis [53•, 54]. Furthermore, other antagonist of the Wnt/ β-Catenin pathway known as Dickkopf-related protein 1 (DKK-1) play an important role in skeletal formation since rare polymorphisms are present in patients with juvenile osteoporosis [55]. Also, the animal transgenic model Dkk-1+/- has increased osteoblast number and bone formation rate [56]. Current clinical trials are employing antibodies to neutralize these antagonists of bone formation and to increase bone formation in patients with osteoporosis [57, 58, 59••, 60].
In addition to the soluble Wnt proteins, other growth factors are involved in osteoblastogenesis. Members of the transforming growth factor-beta (TGF-β)/bone morphogenic protein (BMP) signaling pathway crosstalk along with multiple enhancers such as PTH, fibroblast growth factor (FGF), Wnts, Hedgehog, and others, integrate and amplify their signals and ultimately activate RUNX2 in an either SMAD-dependent or independent manner [61••]. Overall, most of the members of these pathways are crucial for bone formation as it is demonstrated by the critical bone impairment in genetic models lacking any of their multiple components [61••].
Additionally, vitamin D3 has been proved to be stronger than BMP-2 inducing all stages of osteogenesis in a dexamethasone-dependent manner both in vitro [62] and in vivo [63•]. Indirectly, vitamin D enhances calcium and phosphate re-absorption in kidney and intestine, which improves bone mineralization. Finally, vitamin D inhibits marrow adipogenesis by inhibition of PPARγ in vivo [63•].
Interestingly, the downstream response that determines osteoblast differentiation is dependent on the translocation of several transcription factors from the cytoplasm to the nucleus. This has allowed to the discovery that osteogenic/adipogenic transcription factors could only reach the nucleus by means of the mechanical coupling and physical interaction between these activated factors and the proteins of the inner nuclear envelope [64]. Amongst these proteins, lamin A has acquired special relevance due to its regulatory role in the nuclear translocation and DNA-binding of essential transcription factors [65, 66]. In the case of osteoblastogenesis, it has been demonstrated that lamin A integrity and function are crucial to allow its progression [67, 68], otherwise, in the presence of low levels of lamin A expression, adipogenesis would take place [69, 70].
Furthermore, the molecular mechanism linking the Wnt pathway with proteins of the nuclear envelope relay on how β-Catenin translocates into the nucleus and also on the prevention of its degradation while in the cytoplasm. Initially β-Catenin is phosphorylated [71], then it can diffuse or migrate freely through the nuclear pore complexes [72] or can interact with other proteins of the nuclear envelope while facilitates their interaction with the RUNX-related osteogenic complex [73].
In contrast to the role of RUNX2 in osteoblastogenesis, PPARγ is the master transcription factor regulating adipogenesis that affects bone mass not only by blocking RUNX2 activity and thus, bone formation but also stimulating osteoclastogenesis [74]. Activation of PPARγ has a strong adipogenic effect that is reached through the inhibition of osteogenic Wnts, degradation of beta β-Catenin and low levels of lamin A expression. Based on this antagonistic effect between RUNX2 and PPARγ activity, it is proposed that mechanisms blocking marrow adipogenesis through PPARγ inhibition would facilitate RUNX2-related response and would improve osteoblastogenesis and bone formation. This therapeutic effect was obtained by using either pharmacologic antagonists or molecular inhibitors of PPARγ in vivo [63•, 75, 76].
In addition to local release of osteogenic proteins and growth factors, systemic adipokines could also play a role in the regulation of bone marrow MSCs. Leptin, an adipocyte-specific adipokine, centrally inhibits bone formation by preventing serotonin release from the hypothalamus [77•]. In addition, absence of serotonin receptors and tryptophan hydroxylase (Tph2) deletion cause osteoporosis and anorexia [78]. On the other hand, gut-derived serotonin peripherally contributes to prevent bone formation through LRP regulation [79], thus, inhibitors of gut-serotonin have shown to be effective in rescuing osteoporosis in an animal model of bone loss [80]. In addition, Confavreux (2011) reported the relationship between energy metabolism and bone remodeling via the neuronal regulation of leptin (neuropeptide Y: NPY, neuromedin: NMU, serotonin and β2-adrenergic receptor mediated) and osteocalcin (adiponectin and insulin mediated) [81]. Finally, insulin inhibits OPG production in osteoblasts, thus, the increased OPG/RANKL ratio favors osteocalcin activation and release from the ECM toward the stimulation of insulin in the pancreas [82].
Fat-Induced Osteoporosis
Both human and animal studies have demonstrated that marrow fat volumes are inversely related to bone mineral density and to bone integrity [83, 84•]. An in vitro study by Verma et al has proved that there is a clonal switch between adipocytic and osteoblastic lineages in subjects with osteoporosis [84•]. This increase in bone marrow adipogenesis could be the result from a reduction in osteoblast formation by stromal cells due to ageing or apoptosis of bone cells [85]. In addition, bone marrow adiposity may influence bone remodeling in 3 ways: (1) secretion of cytokines; (2) production of adipokines; and (3) paracrine influences on adjacent bone cells that decrease osteoblast number and increase adipocyte number while stimulating osteoclastic activity [18•].
Several lines of evidence have revealed that there is a correlation between fractures and fat marrow adipogenesis. Meunier et al studied iliac crest biopsies and found out that high bone marrow adipocytes in osteoporotic samples compares with healthy samples [86]. Wehrli et al reported MRI assessment of bone marrow in old women compared with their bone mass. They reported that increased fracture risk is associated with increased marrow fat together with lower bone mass [87].
In addition, studies have reported that lipotoxicity was detected after osteoblasts were exposed to adipocyte-secreted factors in vitro [34, 88]. This is supported by experiments using co-cultures of adipocytes and osteoblasts, which revealed that adipocytes inhibit osteoblast proliferation and function through the secretion of adipokines and fatty acids [34, 89]. When the adipocytes were treated with cerulenin (inhibitor of fatty acid synthase) osteoblasts survived longer and mineralized better than their untreated controls suggesting that the secretion of fatty acids by bone marrow adipocytes could have a lipotoxic effect on osteoblasts that can be prevented through the inhibition of fatty acid synthase [34].
Among the adipocyte-secreted factors, palmitic acid was found to be highly prevalent and very toxic to osteoblasts [5, 34]. A recent study has revealed the mechanism of lipotoxicity induced by palmitic acid on osteogenesis by demonstrating that this fatty acid affects Wnt signaling and BMP2/RUNX2 /SMADs pathways as well as mineralization [5]. Furthermore, proteomic analysis investigating changes in adipocytes has shown there is shift in ageing bone marrow in mice from pro-osteogenic, anti-adipogenic and anti-apoptotic phenotype to a toxic and pro-adipogenic one in old mice, which could be associated with adipokines production [90]. Taken together, new evidence on lipotoxicity in bone allows suggesting that yellow fat plays a toxic role within the bone marrow milieu and that inhibition of this toxicity could alleviate this negative effect on bone formation.
Clinical Translation: Fat as a Therapeutic Target for Bone-Related Diseases
From a therapeutic point of view, osteoblast differentiation and RUNX2 activation may be stimulated by using agonists of the Wnt osteogenic pathway, direct stimulation of RUNX2, or inhibition of PPARγ. However, and considering that these pathways also regulate growth and differentiation of other cell types, there is always an inherent risk of increasing the risk of malignancy [91]. For example, although LRP5 and GSK3β could be ideal targets since they have crucial roles in either promoting or blocking osteoblastogenesis, respectively, it is extremely challenging to target their activity in MSCs without affecting other cellular processes [92]. Furthermore, as an additional beneficial effect of inducing MSC differentiation into the osteogenic lineage is that myogenesis could also be facilitated while decreasing high levels of fat infiltration also observed in ageing muscle [93].
As a new therapeutic approach to osteoporosis, in addition to their role in regulating glucose and lipids metabolism, several synthetic [94] and natural PPARγ antagonists [95] are being tested as stimulators of osteoblastogenesis and bone formation. One of them, bisphenol-A-diglycidyl ether (BADGE) is a low affinity PPARγ antagonist that has been shown to have a bone anabolic effect [63•]. This effect that was potentiated when administered in combination with vitamin D in an aged animal model [63•].
As an alternative approach to regulate MSCs differentiation and stimulate osteoblastogenesis, interferon gamma (IFNγ), which we previously reported as increased together with its inducible genes during early osteoblast differentiation in vitro [96] and also to regulate osteoblastogenesis in mice, could rescue oophorectomized mice from their osteoporotic phenotype by increasing osteoblastogenesis and inhibiting adipogenesis [97]. However, the exact mechanism of this effect remains to be elucidated.
Finally, and considering that fatty acids released from adipocytes, are toxic for osteoblast differentiation [5] and that inhibition of fatty acid synthase protects osteoblasts from apoptosis, this new evidence supports the notion that regulating the fatty acid synthase (FAS) pathway could effectively prevent adipogenesis while stimulating osteoblastogenesis [34, 98], which is a hypothesis that requires further exploratory using in vivo studies.
Conclusions
In conclusion, the relationship between fat and bone is complicated, especially within the marrow milieu. The inverse relationship between osteoblastogenesis and adipogenesis, the default differentiation of MSCs into adipocytes, and the age-related changes in the differentiation machinery determine that ageing bone marrow becomes fatty at expense of osteoblastogenesis and bone formation. In addition, the presence of marrow fat is associated with a toxic microenvironment that affects other marrow cells and could induce cell dysfunction and cell death. Considering that the regulatory mechanisms involved in MSCs are well known, these mechanisms could constitute novel therapeutic targets for osteoporosis, especially in older persons in whom bone formation is significantly reduced. With new regulators of adipogenesis and inhibitors of lipotoxicity being assessed in animal models, the potential development of osteoporosis treatment focusing on the fat and bone relationship could constitute the future of the pharmacologic approach to this devastating disease.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance ••Of major importance
Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser. 1994;843:1–129.
Manolagas SC. Birth and death of bone cells: basic regulatory mechanisms and implications for the pathogenesis and treatment of osteoporosis. Endocr Rev. 2000;21:115–37.
Riggs BL, Khosla S, Melton III LJ. Sex steroids and the construction and conservation of the adult skeleton. Endocr Rev. 2002;23:279–302.
Duque G, Troen BR. Understanding the mechanisms of senile osteoporosis: new facts for a major geriatric syndrome. J Am Geriatr Soc. 2008;56:935–41.
Gunaratnam K, Vidal C, Gimble JM, et al. Mechanisms of palmitate-induced lipotoxicity in human osteoblasts. Endocrinology. 2014;155:108–16.
Wauquier F, Philippe C, Leotoing L, et al. The free fatty acid receptor G protein-coupled receptor 40 (GPR40) protects from bone loss through inhibition of osteoclast differentiation. J Biol Chem. 2013;288:6542–51.
Duque G. Bone and fat connection in aging bone. Curr Opin Rheumatol. 2008;20:429–34.
Ng A, Duque G. Osteoporosis as a Lipotoxic Disease. IBMS BoneKEy. 2010;7:108–23. Comprehensive review on the mechanisms of lipotoxicity in bone.
Reid IR, Plank LD, Evans MC. Fat mass is an important determinant of whole body bone density in premenopausal women but not in men. J Clin Endocrinol Metab. 1992;75:779–82.
Albala C, Yanez M, Devoto E, et al. Obesity as a protective factor for postmenopausal osteoporosis. Int J Obes Relat Metab Disord. 1996;20:1027–32.
Cohen A, Dempster DW, Recker RR, et al. Abdominal fat is associated with lower bone formation and inferior bone quality in healthy premenopausal women: a transiliac bone biopsy study. J Clin Endocrinol Metab. 2013;98:2562–72. Important study looking at the relationship between abdominal fat and bone mass.
Bredella MA, Fazeli PK, Lecka-Czernik B, et al. IGFBP-2 is a negative predictor of cold-induced brown fat and bone mineral density in young non-obese women. Bone. 2013;53:336–9.
Gilsanz V, Chalfant J, Mo AO, et al. Reciprocal relations of subcutaneous and visceral fat to bone structure and strength. J Clin Endocrinol Metab. 2009;94:3387–93.
Gimble JM, Nuttall ME. The relationship between adipose tissue and bone metabolism. Clin Biochem. 2012;45:874–9. Excellent review on the relationship between adipose tissue and bone.
Boyle WJ, Simonet WS, Lacey DL. Osteoclast differentiation and activation. Nature. 2003;423:337–42.
Di Iorgi N, Mo AO, Grimm K, et al. Bone acquisition in healthy young females is reciprocally related to marrow adiposity. J Clin Endocrinol Metab. 2010;95:2977–82.
Gimble JM, Robinson CE, Wu X, et al. The function of adipocytes in the bone marrow stroma: an update. Bone. 1996;19:421–8.
Kawai M, de Paula FJ, Rosen CJ. New insights into osteoporosis: the bone-fat connection. J Intern Med. 2012;272:317–29. General overview of the relationship between fat and bone focused on peripheral fat.
Corre J, Planat-Benard V, Corberand JX, et al. Human bone marrow adipocytes support complete myeloid and lymphoid differentiation from human CD34 cells. Br J Haematol. 2004;127:344–7.
Mendez-Ferrer S, Michurina TV, Ferraro F, et al. Mesenchymal and haematopoietic stem cells form a unique bone marrow niche. Nature. 2010;466:829–34. Excellent review on the mechanisms of mesenchymal stem cell differentiation.
Si YL, Zhao YL, Hao HJ, et al. MSCs: biological characteristics, clinical applications and their outstanding concerns. Ageing Res Rev. 2011;10:93–103.
Sethe S, Scutt A, Stolzing A. Aging of mesenchymal stem cells. Ageing Res Rev. 2006;5:91–116.
Maurer MH. Proteomic definitions of mesenchymal stem cells. Stem Cells Int. 2011;2011:704256.
Dominici M, Le Blanc K, Mueller I, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8:315–7.
Boxall SA, Jones E. Markers for characterization of bone marrow multipotential stromal cells. Stem Cells Int. 2012;2012:975871. Comprehensive review on the mechanisms of stem cell differentiation.
Casiraghi F, Perico N, Remuzzi G. Mesenchymal stromal cells to promote solid organ transplantation tolerance. Curr Opin Organ Transplant. 2013;18:51–8.
Shah K. Mesenchymal stem cells engineered for cancer therapy. Adv Drug Deliv Rev. 2012;64:739–48.
Ramakrishnan A, Torok-Storb B, Pillai MM. Primary marrow-derived stromal cells: isolation and manipulation. Methods Mol Biol. 2013;1035:75–101.
Al-Nbaheen M, Vishnubalaji R, Ali D, et al. Human stromal (mesenchymal) stem cells from bone marrow, adipose tissue and skin exhibit differences in molecular phenotype and differentiation potential. Stem Cell Rev. 2013;9:32–43. Good review on the biology of mesenchymal stem cells.
Rastegar F, Shenaq D, Huang J, et al. Mesenchymal stem cells: molecular characteristics and clinical applications. World J Stem Cells. 2010;2:67–80.
Stolzing A, Jones E, McGonagle D, et al. Age-related changes in human bone marrow-derived mesenchymal stem cells: consequences for cell therapies. Mech Ageing Dev. 2008;129:163–73.
Hammoudi TM, Rivet CA, Kemp ML, et al. Three-dimensional in vitro tri-culture platform to investigate effects of crosstalk between mesenchymal stem cells, osteoblasts, and adipocytes. Tissue Eng A. 2012;18:1686–97.
Lu Z, Roohani-Esfahani S-I, Wang G, et al. Bone biomimetic microenvironment induces osteogenic differentiation of adipose tissue-derived mesenchymal stem cells. Nanomedicine. 2012;8:507–15.
Elbaz A, Wu X, Rivas D, et al. Inhibition of fatty acid biosynthesis prevents adipocyte lipotoxicity on human osteoblasts in vitro. J Cell Mol Med. 2010;14:982–91.
Rosen CJ, Ackert-Bicknell C, Rodriguez JP, et al. Marrow fat and the bone microenvironment: developmental, functional, and pathological implications. Crit Rev Eukaryot Gene Expr. 2009;19:109–24.
Kang S, Bennett CN, Gerin I, et al. Wnt signaling stimulates osteoblastogenesis of mesenchymal precursors by suppressing CCAAT/enhancer-binding protein alpha and peroxisome proliferator-activated receptor gamma. J Biol Chem. 2007;282:14515–24.
Kurra S, Siris E. Diabetes and bone health: the relationship between diabetes and osteoporosis-associated fractures. Diabetes Metab Res Rev. 2011;27:430–5.
Taxel P, Kaneko H, Lee SK, et al. Estradiol rapidly inhibits osteoclastogenesis and RANKL expression in bone marrow cultures in postmenopausal women: a pilot study. Osteoporos Int. 2008;19:193–9.
Lau RY, Guo X. A review on current osteoporosis research: with special focus on disuse bone loss. J Osteoporos. 2011;2011:293808.
Hayashi K, Yamaguchi T, Yano S, et al. BMP/Wnt antagonists are upregulated by dexamethasone in osteoblasts and reversed by alendronate and PTH: potential therapeutic targets for glucocorticoid-induced osteoporosis. Biochem Biophys Res Commun. 2009;379:261–6.
Gaur T, Lengner CJ, Hovhannisyan H, et al. Canonical WNT signaling promotes osteogenesis by directly stimulating Runx2 gene expression. J Biol Chem. 2005;280:33132–40.
Rosen ED, MacDougald OA. Adipocyte differentiation from the inside out. Nat Rev Mol Cell Biol. 2006;7:885–96.
Takada I, Kouzmenko AP, Kato S. Wnt and PPAR gamma signaling in osteoblastogenesis and adipogenesis. Nat Rev Rheumatol. 2009;5:442–7. Excellent review on the role of Wnt and PPAR gamma in osteoblast and adipocyte differentiation.
Komori T. Signaling networks in RUNX2-dependent bone development. J Cell Biochem. 2011;112:750–5.
Yavropoulou MP, Yovos JG. The role of the Wnt signaling pathway in osteoblast commitment and differentiation. Hormones. 2007;6:279–94.
Johnson ML, Rajamannan N. Diseases of Wnt signaling. Rev Endocr Metab Disord. 2006;7:41–9.
Johnson ML. LRP5 and bone mass regulation: where are we now? BoneKEy Rep. 2012;1:1.
Chang MK, Kramer I, Keller H, et al. Reversing LRP5-dependent osteoporosis and SOST deficiency-induced sclerosing bone disorders by altering Wnt signaling activity. J Bone Miner Res. 2014;29:29–42.
Frost M, Andersen T, Gossiel F, et al. Levels of serotonin, sclerostin, bone turnover markers as well as bone density and microarchitecture in patients with high-bone-mass phenotype due to a mutation in Lrp5. J Bone Miner Res. 2011;26:1721–8.
Cawthorn WP, Bree AJ, Yao Y, et al. Wnt6, Wnt10a and Wnt10b inhibit adipogenesis and stimulate osteoblastogenesis through a beta-catenin-dependent mechanism. Bone. 2012;50:477–89. Relevant information on the role of Wnts in osteoblastogenesis.
Cristancho AG, Lazar MA. Forming functional fat: a growing understanding of adipocyte differentiation. Nat Rev Mol Cell Biol. 2011;12:722–34.
Lin C, Jiang X, Dai Z, et al. Sclerostin mediates bone response to mechanical unloading through antagonizing Wnt/beta-catenin signaling. J Bone Miner Res. 2009;24:1651–61.
Duque G, Li W, Yeo LS, et al. Attenuated anabolic response to exercise in lamin A/C haploinsufficient mice. Bone. 2011;49:412–8. Initial report on the role of the proteins of the nuclear envelope in osteoblastogenesis.
Piemonte S, Romagnoli E, Bratengeier C, et al. Serum sclerostin levels decline in post-menopausal women with osteoporosis following treatment with intermittent parathyroid hormone. J Endocrinol Invest. 2012;35:866–8.
Korvala J, Löija M, Mäkitie O, et al. Rare variations in WNT3A and DKK1 may predispose carriers to primary osteoporosis. Eur J Med Genet. 2012;55:515–9.
Morvan F, Boulukos K, Clement-Lacroix P, et al. Deletion of a single allele of the Dkk1 gene leads to an increase in bone formation and bone mass. J Bone Miner Res. 2006;21:934–45.
Padhi D, Jang G, Stouch B, et al. Single-dose, placebo-controlled, randomized study of AMG 785, a sclerostin monoclonal antibody. J Bone Miner Res. 2011;26:19–26.
Glantschnig H, Hampton RA, Lu P, et al. Generation and selection of novel fully human monoclonal antibodies that neutralize Dickkopf-1 (DKK1) inhibitory function in vitro and increase bone mass in vivo. J Biol Chem. 2010;285:40135–47.
Canalis E. Wnt signalling in osteoporosis: mechanisms and novel therapeutic approaches. Nat Rev Endocrinol. 2013;9:575–83. Excellent overview of the role of Wnt signaling in osteoporosis.
Ling L, Nurcombe V, Cool SM. Wnt signaling controls the fate of mesenchymal stem cells. Gene. 2009;433:1–7.
Chen G, Deng C, Li YP. TGF-beta and BMP signaling in osteoblast differentiation and bone formation. Int J Biol Sci. 2012;8:272–88. Comprehensive assessment of the role of BMPs in bone formation.
Piek E, Sleumer LS, van Someren EP, et al. Osteo-transcriptomics of human mesenchymal stem cells: accelerated gene expression and osteoblast differentiation induced by vitamin D reveals c-MYC as an enhancer of BMP2-induced osteogenesis. Bone. 2010;46:613–27.
Duque G, Li W, Vidal C, et al. Pharmacological inhibition of PPARgamma increases osteoblastogenesis and bone mass in male C57BL/6 mice. J Bone Miner Res. 2013;28:639–48. Most recent report on the therapeutic applications of PPAR gamma inhibition in osteoporosis.
Swift J, Ivanovska IL, Buxboim A, et al. Nuclear lamin-A scales with tissue stiffness and enhances matrix-directed differentiation. Science. 2013;341:1240104.
Crisp M, Burke B. The nuclear envelope as an integrator of nuclear and cytoplasmic architecture. FEBS Lett. 2008;582:2023–32.
Andres V, Gonzalez JM. Role of A-type lamins in signaling, transcription, and chromatin organization. J Cell Biol. 2009;187:945–57.
Akter R, Rivas D, Geneau G, et al. Effect of lamin A/C knockdown on osteoblast differentiation and function. J Bone Miner Res. 2009;24:283–93.
Rauner M, Sipos W, Goettsch C, et al. Inhibition of lamin A/C attenuates osteoblast differentiation and enhances RANKL-dependent osteoclastogenesis. J Bone Miner Res. 2009;24:78–86.
Duque G, Rivas D. Age-related changes in lamin A/C expression in the osteoarticular system: laminopathies as a potential new aging mechanism. Mech Ageing Dev. 2006;127:378–83.
Rivas D, Li W, Akter R, et al. Accelerated features of age-related bone loss in zmpste24 metalloproteinase-deficient mice. J Gerontol A Biol Sci Med Sci. 2009;64:1015–24.
Wu X, Tu X, Joeng KS, et al. Rac1 activation controls nuclear localization of beta-catenin during canonical Wnt signaling. Cell. 2008;133:340–53.
Kumeta M, Yoshimura SH, Hejna J, et al. Nucleocytoplasmic shuttling of cytoskeletal proteins: molecular mechanism and biological significance. Int J Cell Biol. 2012;2012:494902.
Tilgner K, Wojciechowicz K, Jahoda C, et al. Dynamic complexes of A-type lamins and emerin influence adipogenic capacity of the cell via nucleocytoplasmic distribution of beta-catenin. J Cell Sci. 2009;122:401–13.
Wan Y. PPARγ in bone homeostasis. Trends Endocrinol Metab. 2010;21:722–8.
Vidal C, Bermeo S, Li W, et al. Interferon gamma inhibits adipogenesis in vitro and prevents marrow fat infiltration in oophorectomized mice. Stem Cells. 2012;30:1042–8.
Fournier C, Perrier A, Thomas M, et al. Reduction by strontium of the bone marrow adiposity in mice and repression of the adipogenic commitment of multipotent C3H10T1/2 cells. Bone. 2012;50:499–509.
Driessler F, Baldock PA. Hypothalamic regulation of bone. J Mol Endocrinol. 2010;45:175–81. Original evidence on hypothalamic regulation of bone.
Yadav VK, Oury F, Tanaka KF, et al. Leptin-dependent serotonin control of appetite: temporal specificity, transcriptional regulation, and therapeutic implications. J Exp Med. 2011;208:41–52.
Mason JJ, Williams BO. SOST and DKK: antagonists of LRP family signaling as targets for treating bone disease. J Osteoporos. 2010;2010:460120.
Inose H, Zhou B, Yadav VK, et al. Efficacy of serotonin inhibition in mouse models of bone loss. J Bone Miner Res. 2011;26:2002–11.
Confavreux CB. Bone: from a reservoir of minerals to a regulator of energy metabolism. Kidney Int. 2011;79 Suppl 121:S14–9.
Chen X, Tian HM, Yu XJ. Bone delivers its energy information to fat and islets through osteocalcin. Orthop Surg. 2012;4:114–7.
Fazeli PK, Horowitz MC, MacDougald OA, et al. Marrow fat and bone–new perspectives. J Clin Endocrinol Metab. 2013;98:935–45.
Verma S, Rajaratnam JH, Denton J, et al. Adipocytic proportion of bone marrow is inversely related to bone formation in osteoporosis. J Clin Pathol. 2002;55:693–8. Original paper demonstrating the inverse relationship between marrow fat and bone mass in humans.
Jilka RL, Weinstein RS, Parfitt AM, et al. Quantifying osteoblast and osteocyte apoptosis: challenges and rewards. J Bone Miner Res. 2007;22:1492–501.
Meunier P, Aaron J, Edouard C, et al. Osteoporosis and the replacement of cell populations of the marrow by adipose tissue. A quantitative study of 84 iliac bone biopsies. Clin Orthop Relat Res. 1971;80:147–54.
Wehrli FW, Hopkins JA, Hwang SN, et al. Cross-sectional study of osteopenia with quantitative MR imaging and bone densitometry. Radiology. 2000;217:527–38.
Kim JE, Ahn MW, Baek SH, et al. AMPK activator, AICAR, inhibits palmitate-induced apoptosis in osteoblast. Bone. 2008;43:394–404.
Maurin AC, Chavassieux PM, Frappart L, et al. Influence of mature adipocytes on osteoblast proliferation in human primary co-cultures. Bone. 2000;26:485–9.
Gasparrini M, Rivas D, Elbaz A, et al. Differential expression of cytokines in subcutaneous and marrow fat of aging C57BL/6 J mice. Exp Gerontol. 2009;44:613–8.
Reya T, Clevers H. Wnt signaling in stem cells and cancer. Nature. 2005;434:843–50.
Moon RT, Kohn AD, De Ferrari GV, et al. WNT and beta-catenin signaling: diseases and therapies. Nat Rev Genet. 2004;5:691–701.
Tong J, Li W, Vidal C, et al. Lamin A/C deficiency is associated with fat infiltration of muscle and bone. Mech Ageing Dev. 2011;132:552–9.
Shearer BG, Billin AN. The next generation of PPAR drugs: do we have the tools to find them? Biochim Biophys Acta. 2007;1771:1082–93.
Goto T, Kim Y-I, Takahashi N, et al. Natural compounds regulate energy metabolism by the modulating the activity of lipid-sensing nuclear receptors. Mol Nutr Food Res. 2013;57:20–33.
Duque G, Huang DC, Macoritto M, et al. Autocrine regulation of interferon gamma in mesenchymal stem cells plays a role in early osteoblastogenesis. Stem Cells. 2009;27:550–8.
Duque G, Huang DC, Dion N, et al. Interferon-gamma plays a role in bone formation in vivo and rescues osteoporosis in ovariectomized mice. J Bone Miner Res. 2011;26:1472–83.
Schmid B, Rippmann JF, Tadayyon M, et al. Inhibition of fatty acid synthase prevents preadipocyte differentiation. Biochem Biophys Res Commun. 2005;328:1073–82.
Acknowledgement
The authors’ research cited in this review has been funded by project grants from the National Health and Medical Research Council (NHMRC) of Australia (Grants 632766 and 632767) and the Nepean Medical Research Foundation. The authors would like to thank PR Ebeling of the University of Melbourne and EF Eriksen of Oslo University Hospital for their review of the manuscript.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
S. Bermeo declares no conflicts of interest.
K. Gunaratnam declares no conflicts of interest.
G. Duque declares no conflicts of interest.
Human and Animal Rights and Informed Consent
All studies by the authors involving animal subjects were performed after approval by the appropriate institutional review boards.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bermeo, S., Gunaratnam, K. & Duque, G. Fat and Bone Interactions. Curr Osteoporos Rep 12, 235–242 (2014). https://doi.org/10.1007/s11914-014-0199-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-014-0199-y