Opinion statement
Colorectal cancer (CRC) is the third leading cancer diagnosed globally and an important cause of cancer-related mortality. Of interest, while we have witnessed a declining incidence trend over the past few decades in the older population, incidence rates for adolescents and young adults have been increasing steadily. Several factors may well explain this apparent epidemic in the young, namely a lack of routine screening and emerging lifestyle issues such as obesity, lack of exercise, and dietary factors. It is known that both environmental and genetic factors can increase the likelihood of developing CRC. Although inherited susceptibility is associated with the most striking increases in risk, and must always be considered in a young patient with CRC, the majority of CRCs are in fact sporadic rather than familial. Early-onset CRC is a truly heterogeneous disease, with mounting evidence to suggest that this patient population has a distinctive molecular profile, very different to late-onset CRC cases. Currently, both younger and older patients with CRC are treated in essentially the same manner, but with a better understanding of the molecular mechanisms underlying CRC in the young, we will have the opportunity to specifically tailor screening and clinical management strategies in this unique patient population in an effort to improve outcomes. The aim of this review is to outline our current knowledge of the distinguishing features of early-onset CRC, the ongoing research efforts, and the evolving evidence in this field.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
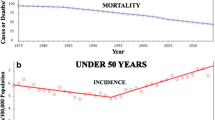
Colorectal cancer remains a common cancer worldwide and a significant public health burden. The estimated annual incidence is 1.2 million new cases per year [1]. While there has been a progressive steady decline of CRC among the older population in recent decades, this contrasts sharply with a rising incidence in young adults (Fig. 1). Early-onset CRC is a highly heterogeneous disease, with hereditary genetic syndromes accounting for only a minority of cases while the vast majority of patients have so-called sporadic disease [2]. CRC in the young tends to be associated with more advanced disease at presentation, adverse histologic features, and a variability in molecular characteristics resulting in a distinct tumor biology compared to their older counterparts. Despite this, studies have shown that the prognosis of patients with early-onset CRC, matched for stage, is identical to and even surpasses that of older patients [3]. Currently, all patients with CRC are treated in a homogeneous fashion in terms of cytotoxic regimens, regardless of the age of disease onset, with a trend towards overtreatment in the young [4]. Efforts are ongoing to advance our understanding of the molecular landscape of this early-onset disease, with the aim of impacting how prevention, screening, and treatment strategies are designed in the future to optimize outcomes for this novel patient population.
Incidence of colorectal cancer in the population younger and older than 50 years of age according to the SEER database from 1973 to 2013 [158].
Epidemiology
Although recent decades have witnessed steady declines in both incidence and mortality rates from CRC overall [5, 6], the latest evidence points towards an alarming rise in its occurrence among individuals younger than 50 years old [6,7,8,9,10,11,12]. CRC is the second most common cancer and the third leading cause of cancer-related death (1.51 per 100,000 in females and 1.67 per 100,000 in males) in the USA, when assessed only in the population younger than 50 years [10].
An analysis of the Surveillance, Epidemiology and End Results (SEER) database from 1973 to 1999 indicated that incidences of colon and rectal cancer among young adults (20 to 40 years) increased by 17% and 75%, respectively [13]. From 1992 to 2005, the incidence rates for CRC increased 1.5% per year in men and 1.6% per year in women. For rectal cancer, the average increase was 3.5% per year in men and 2.9% per year in women [14]. A more recent assessment of the SEER Database (from 1975 to 2010) analyzed 393,241 patients with pathologically confirmed CRC and found annual percentage changes of 1.99, 0.41, −0.97, and −1.15, in the age groups of 20–34, 35–49, 50–74, and >74 years, respectively. Despite a 0.92% global decline in overall CRC incidence, the incidence rate in individuals aged 20–34 years is predicted to increase by up to 90% for colon cancer and 124% for rectal cancer, by the year 2030 [9•].
Approximately three quarters of early-onset CRC occur between ages 40 and 49 years [15]. Both sexes are equally affected, as revealed in a retrospective analysis (SEER Database, 1992 to 2005), which detected increased annual incidence rates per 100,000 young adults of 1.5% in men and 1.6% in women. However, another study highlighted a slight male predominance. In this study, incidence rates were 4.9, 9.9, 16.4, and 30.8 in men and 4.2, 7.6, 15.3, and 25.9 in women, for age groups of 30–34, 35–39, 40–44, and 45–49 years, respectively [10].
Racial disparities in the diagnosis and outcomes of CRC in the young have been identified through observational studies [15,16,17]. CRC incidence in young adults (20–44 years) was higher in African-Americans (7.9 per 100,000 individuals) when compared to non-Hispanic Whites (6.7 per 100,000 individuals) [18]. A retrospective analysis of the SEER Database found that African-Americans with colon cancer had an increased hazard of cancer-specific death (HR = 1.35, 95% CI 1.26 to 1.45), with an overall 5-year survival of 54.9% among non-Hispanic Blacks versus 68.1% among Non-Hispanic Whites [19•]. The causal factors of these disparities are still a matter of debate but may result from biological, cultural, or socioeconomic distinctions.
Young patients diagnosed with CRC more commonly have symptomatic, later stage, mucinous, and poorly differentiated tumors [20,21,22]. Teng et al. analyzed 11,071 CRC cases in the adolescent and young adult population (15–39 years) from 17 registries of the SEER program (1998 to 2011) and found that the rectum was the most common primary tumor site (25%) and 66.6% were left-sided. Moreover, 72% were diagnosed with regional or metastatic disease, although disease-specific and overall survival were comparable to the general population (10 years = 57.3 and 52.4%, respectively) [23]. Accordingly, a retrospective study by Abdelsattar et al. found that younger patients achieved longer stage-adjusted disease-specific survival, although their disease was more advanced [24]. In a retrospective study from Stanford Cancer Institute, 253 patients with young-onset CRC were compared with 232 patients diagnosed at 50 years or older. Advanced-stage tumors (72% vs. 63%), family history (25% vs. 17%), and confirmed hereditary syndromes (7% vs. 1%) were observed in higher proportions within the younger group [25].
Hereditary syndromes
Although the majority of CRCs are sporadic, up to 20–30% are thought to have a hereditary component. Of those, only 3–5% have a well-characterized genetic basis [26]. Lynch syndrome (LS) and familial adenomatous polyposis (FAP) are the most common of the known hereditary CRC syndromes, with well-characterized physiopathology (Table 1).
Lynch syndrome is the most common CRC hereditary syndrome, estimated to account for 2–5% of CRC cases [27]. It is inherited in an autosomal dominant fashion and results from germline mutations in four DNA mismatch repair genes (MMR)—MLH1, MSH2, PMS2, and MSH6 [28]—or the EPCAM gene and confers an estimated 50–80% lifetime risk of CRC development [29]. Clinically, these tumors are diagnosed on average between 40 and 45 years of age, are most likely proximal in location, often with numerous synchronous and metachronous lesions, have a lower stage at diagnosis, and better prognosis than sporadic CRC [30, 31]. LS also predisposes to a wide range of other primary cancers, including endometrial, gastric, small bowel, hepatobiliary and urinary tract, and ovarian and CNS tumors.
The cumulative risk of developing cancer varies according to the different mutations. MSH6 and PMS2 mutations, for example, have an overall lower CRC risk as compared to MLH1 and MSH2 and possibly an attenuated phenotype with later age of cancer development and lower penetrance [32]. The CRC risk appears to be similar in MLH1, MSH2, and EPCAM mutation carriers but the risk of endometrial and other cancers seems to be higher in MSH2 mutated individuals [33]. Genetic evaluation for LS should be considered for individuals with synchronous and metachronous CRC, those diagnosed at an age younger than 50 years, with multiple Lynch-associated cancers, and also in cases of familial clustering of Lynch-associated tumors.
FAP is the second most common hereditary CRC syndrome, accounting for less than 1% of all CRC cases. It is characterized by the presence of multiple colorectal adenomatous polyps (typically more than 100) and occurs in 1/10,000 to 1/30,000 live births [34]. Classic FAP has an autosomal dominant inheritance pattern, resulting from a germline mutation in the adenomatous polyposis coli (APC) gene, with almost complete penetrance of colonic manifestations but variable penetrance of the extra-colonic features, which include duodenal adenoma, gastric polyps, desmoid tumors, dental osteomas, soft tissue tumors, and extra-intestinal cancers [35].
The age of onset of adenomas is variable, but by age 30, it is estimated that 90% of mutation carriers present with FAP [36]. Individuals with germline APC gene mutations generally have an exceedingly strong penetrance, with an estimated 100% cancer risk by a median age of 39, if left without medical follow-up or treatment [37, 38]. Very young onset of CRCs can also occur, with 7% developing CRCs by age 21 [39]. Attenuated FAP is a phenotypically distinct and less severe entity, presenting with fewer than 100 adenomas, typically 20–30, and occurring at a later age. The mean age at diagnosis is 56 years [40]. Regular, systematic follow-up and supportive care should be offered to all patients. Patients should also be considered for prophylactic CRC surgery by their early twenties. Upper endoscopy is necessary for surveillance to reduce the risk of ampullary and duodenal cancer.
Multiple colorectal adenomas can also be caused by mutations in the human MutY homolog (MYH) gene, in an autosomal recessive condition referred to as MutYH-associated polyposis (MAP). It causes a recessively inherited polyposis condition, usually diagnosed between 40 and 60 years, with a mean age of 45, which is characterized by a slightly increased risk of developing CRC and polyps/adenomas in both the upper and lower gastrointestinal tract [41, 42]. Both biallelic and monoallelic mutations have been described in MAP, and it appears that biallelic mutations carry an estimated CRC risk of 80% [43]. The risk attributed to monoallelic mutations is still controversial.
Other rare conditions include the hamartomatous syndromes, which include Peutz-Jeghers syndrome (PJS), juvenile polyposis syndromes (JPS), hereditary mixed polyposis syndrome (HMPS), and PTEN hamartomatous tumor syndrome. They are inherited in an autosomal dominant fashion and increase the risk of young-onset CRC. PJS is a rare autosomal dominant syndrome characterized by the presence of gastrointestinal polyps and mucocutaneous pigmentation. Hamartomatous polyps are more frequently found in the small intestine but may occur anywhere in the gastrointestinal tract [35]. CRC appears to be the most common PJS-associated malignancy with a mean age at diagnosis of 42 years [44]. Juvenile polyposis syndrome is characterized by multiple juvenile polyps (inflammatory hamartomatous polyps seen in childhood) throughout the digestive tract. The risk of CRC is estimated to be 17–22% by age 35, and almost 68% by 60, with a median age of CRC diagnosis of 42 years [45]. Germline PTEN mutations are also responsible for another rare group of hamartoma syndromes. The two most frequently described are Cowden syndrome (CS) and Bannayan-Riley-Ruvalcaba syndrome (BRRS). It has been suggested that they are part of a spectrum of the same disease, with an age-related penetrance [46].
Serrated polyposis syndrome (SPS) is a rare condition where patients present with multiple polyps with serrated architecture in the colorectum The overall cumulative risk of CRC is still unclear as well as the age of onset of CRC. In a multicenter report, the average age of CRC diagnosis was 48 years, and there was an increase in the risk of CRC for first-degree relatives if the index case was diagnosed under the age of 50, suggesting that there is an inherited component [47]. The genetic basis for SPS has not yet been clarified.
Nonhereditary risk factors
Genetic predisposition alone is not a sufficient explanation as to why CRC incidence is increasing in the young. Possible reasons could involve general lifestyle changes. Sedentary habit, obesity, and diabetes mellitus, for example, have risen in the general population over the past decades and may well have influenced CRC rates [48, 49].
There is sufficient evidence to support a role for physical activity in preventing cancers of the colon and breast and also strong links between obesity and CRC risk [50]. Diet may play a significant role in young patients who develop CRC [51,52,53]. It appears that for each 5-unit increase in body mass index, there is an estimated 13% to 18% associated increase in CRC risk. A systematic review and meta-analysis including data from 13 studies showed that a weight gain between early adulthood and midlife was associated with a significant increase in CRC risk [54]. Similarly, a meta-analysis study suggested that regular physical activity is associated with a 24% to 31% reduction in CRC risk when comparing the most versus the least active individuals [55]. Diabetes mellitus has been associated with increased CRC risk [56]. A meta-analysis including data from 14 studies estimated that the risk of CRC among diabetics was between 20% and 38% higher than nondiabetics, even when the analysis was limited to studies that either controlled for smoking and obesity or for smoking, obesity, and physical exercise [56]. The notable increased frequency of obesity and diabetes seen in young adults for the past three decades is precisely in parallel with the increase in CRC incidence in this age group.
Cigarette smoking has been linked to increased risk of CRC diagnosis and mortality, with stronger association for rectal rather than colon cancer [57]. Moreover, smoking is also a risk factor for serrated, hyperplastic, and adenomatous colonic polyps [58, 59]. Several studies have also described an association between alcohol consumption and CRC, with increased risk for moderate (two to three drinks per day) and heavy drinkers (≥4 drinks per day) but not for light drinkers (≤1 drink per day) [60,61,62].
However, all the of the listed risk factors alone do not fully explain the observed trends in young-onset CRC since they are also common or increasing in older age groups in which CRC incidence has decreased. Furthermore, they are also highly influenced by ethnicity and related cultures, and on this matter, it is known that African-Americans have high CRC rates with a 20% greater mortality than Whites [63]. They tend to be diagnosed at a younger age with higher frequency of CRC diagnosis under age 50. It is clear therefore that additional epidemiologic research is warranted to better explain these trends.
Screening
Young adults at increased risk for CRC
The presence of a first-degree relative diagnosed with CRC or adenomas increases the lifetime risk for CRC by up to fourfold [64,65,66,67]. Therefore, the occurrence of CRC in ages younger than 60 years in a first-degree relative may prompt screening of asymptomatic young adults either at age 40 or 10 years earlier than the youngest age at CRC diagnosis in the index case [68, 69]. A retrospective study found that the prevalence of adenomas and advanced adenomas in 40- to 49-year-olds undergoing colonoscopies due to family history of CRC was 15.4% and 3.9%, respectively [70]. However, the adherence rate of physicians to colonoscopy recommendations for first-degree relatives of young patients diagnosed with CRC was previously reported as only 62.9% in a cross-sectional study [71]. Another potential issue for adequate screening is low patient adherence to family screening due to poor awareness of greater risk among first-degree relatives of CRC patients [72, 73]. Conversely, there is still uncertainty if screening first-degree relatives of patients with adenomas without CRC history is cost-effective [74].
Patients with hereditary syndromes, such as LS, FAP, or any other, are at an even higher risk for CRC development at earlier ages. Clinical follow-ups, screening tests, and genetic counseling are fundamental pillars for the appropriate management of these hereditary conditions. Individuals with confirmed or suspected Lynch syndrome should undergo periodical colonoscopies for CRC screening every 1 to 2 years beginning at age 20 to 25 years [75,76,77], as appropriate screening is associated with decreased mortality [78,79,80]. Because colorectal adenomas and CRC occur later and at a lower risk in families with MSH6 or PMS2 mutations, screening may be started at 30 to 35 years or 5 years before the earliest CRC case in a first-degree relative [75]. Physicians should also pay attention to the possible development of other primary cancers, such as endometrial, ovarian, gastric, small bowel, and others, and additional screening should be carried out with pelvic examination, endometrial biopsy, and gastroduodenoscopies [75, 81].
Patients with diagnosed FAP or at high-risk for FAP (first-degree relatives and individuals diagnosed with ≥10 to 20 adenomas or adenomas in the presence of extra-colonic characteristics of FAP) should start annual surveillance with sigmoidoscopy or colonoscopy at 10 to 11 years. Due to the large number of polyps and high CRC risk, virtually all individuals with classic FAP will ultimately undergo colectomy in adulthood. Physicians should continue periodic surveillance of the reminiscent rectal or ileal pouch every 6 to 12 months or every 6 months to 5 years, respectively, depending on the polyp burden. Families with attenuated FAP may begin surveillance at 18 to 20 years [76, 82,83,84].
Additionally, young patients with inflammatory bowel disease (IBD), such as Crohn’s colitis and ulcerative colitis (UC), may develop CRC at a young age due to accelerated carcinogenesis resulting from chronic inflammation [85]. In a cohort of IBD patients, the incidence ratio of CRC was 2.1 for Crohn’s colitis and 5.6 for UC [86]. As expected, the higher risk for CRC is related to uncontrolled disease and early-onset of colitis [87]. Approximately two-thirds of patients with IBD are aware of an increased CRC risk [88]. However, there is an absence of prospective studies evaluating the role of surveillance for CRC in this scenario and evidence to support this indication relies on case-controls and retrospective cohorts [85]. Individuals with left-sided UC and Crohn’s disease affecting at least one-third of the colon should perform periodic examinations. According to the severity of colitis, societies have recommend colonoscopies at intervals of 1 to 5 years [89,90,91]. Literature evaluating the role of chromoendoscopy with targeted biopsies for detection of neoplasia in patients with intestinal bowel disease is still controversial [92, 93]. Random surveillance biopsies have a low yield and should not be routinely indicated [94].
Young adults at average risk
Screening for CRC has been recommended for the average-risk population between 50 and 74 years and has been shown to reduce CRC incidence and mortality in up to 26% [95, 96]. Due to the recent increase in incidence of early-onset CRC, questions have been raised if screening should be initiated earlier [97].
Even though 10.9% to 15% of CRC cases are diagnosed in patients too young for average-risk screening, current evidence is scarce and does not support a wide-scale recommendation to screen individuals younger than 50 years, as the incidence of pre-neoplastic lesions is low in this age group and does not justify the associated risks and costs [15, 24, 97]. However, considering possible disparities in racial characteristics in CRC incidence, the consensus opinion of the American College of Gastroenterology and American College of Gastrointestinal Endoscopy is to recommend initiating screening after 45 years in non-Hispanic African-Americans [98, 99].
Previous work demonstrated that delayed diagnosis was a potential problem in the scenario of symptomatic CRC in young patients, possibly contributing to diagnosis at more advanced stages and with less favorable outcomes [100, 101]. For instance, a recently published case-control study including 1514 patients treated at University of Vermont Medical Center showed the median time to treatment from symptom onset in rectal cancer was 217 days for patients under 50 years versus 29.5 days for patients older than 50 years [102]. Educational strategies to improve awareness of patients, primary care physicians, and gastroenterologists on the increasing incidence of early-onset CRC should perhaps prevail over universal recommendations for screening asymptomatic patients to address this issue. Such an approach would lead to better identification of high-risk families and red flag symptoms (such as anemia without apparent cause, rectal bleeding, change in bowel habits, and weight loss) and ultimately would trigger diagnostic investigation and appropriate, timely curative interventions.
Molecular characteristics
From a molecular perspective, early-onset CRCs represent a highly heterogeneous disease group. Marked biological diversity is evident not only when comparing early- to late-onset CRC cases [103] but a divergence in molecular features is also an inherent component within the early-onset group itself, which includes known hereditary syndromes, familial cases, as well as sporadic CRC.
The pathogenesis of early-onset CRC is well characterized in those individuals with inherited CRC syndromes, in which an identifiable germline mutation is present in a cancer susceptibility gene. Knowledge, however, regarding genetic alterations and molecular mechanisms of sporadic early-onset CRC remains somewhat limited, although it is increasing. Recent studies suggest that sporadic young-onset CRC may have a unique molecular profile and is likely attributed to the cumulative effect of multiple common/rare genetic variants displaying variable penetrance [104].
Three critical mutational pathways implicated in CRC carcinogenesis include chromosomal instability (CIN), microsatellite instability (MSI), and the CpG island methylator phenotype (CIMP). Each pathway is distinctive in terms of its respective clinicopathological, familial, and prognostic features. While these pathways are not mutually exclusive, whichever is the dominant pathway determines the final phenotype in the individual patient [105].
The majority of sporadic CRC cases (80–85%) involve the CIN pathway, which is associated with chromosomal number and structural alterations, and loss of heterozygosity. CIN has also been found in cases of FAP with a germline APC mutation. These tumors are microsatellite stable (MSS). Other molecular characteristics include activation of the proto-oncogenes, KRAS and C-MYC; inactivation of tumor suppressor genes, APC and p53; and loss of heterozygosity for the long arm of chromosome 18 as well as TGFBR and PIK3CA mutations [106,107,108,109,110]. The CIN pathway is the main driver in most early-onset tumors, which are characterized by a lower right colon prevalence, fewer synchronous and metachronous tumors, higher rate of adverse histologic features, absence of other primary neoplasms, and typically later stage at diagnosis [111, 112]. Compared with late-onset cases, early-onset tumors differ by the substantial rate of left colon location and a significant familial component.
The MSI pathway is implicated in 10–15% of all CRCs. Here, the MMR system is unable to correct DNA replication errors, which is under the control of several genes (including MLH1, MSH2, MSH6, and PMS2). Other genes affected in this CRC subgroup include the tumor suppressor genes, TGF-BRII, IGFIIR, MSH3, and BAX [113]. Single nucleotide mutations accumulate and alterations in the lengths of repetitive microsatellite nucleotide sequences also occur [28, 114]. MSI tumors are present both in the hereditary form such as Lynch syndrome, due to a germline MMR gene mutation, and also sporadic CRC cases, as a result of MLH1 hypermethylation [115]. Most Lynch syndrome tumors (>90%) are MSI-high [116]. As mentioned previously, inactivation of one of the MMR genes, MLH1, MSH2, MSH6, and PMS2, secondary to a germline mutation, is the underlying mechanism. MLH1 and MSH2 mutations account for ∼90%, MSH6 mutations for ∼10%, and PMS2 mutations for 6% of all Lynch syndrome tumors [117]. EPCAM gene deletions can also result in Lynch syndrome, with high risk of CRC, through epigenetic silencing of MSH2 in tissues expressing EPCAM [118].
A higher rate of microsatellite instability (MSI-H) has been demonstrated in younger CRC patients [119]. In a series by Gryfe et al. of 607 CRC patients aged ≤50 years, high frequency MSI was found in 17% of cases [120]. Furthermore, multivariate analysis identified a significant survival advantage independent of all standard prognostic factors, including tumor stage (HR, 0.42; 95% CI, 0.27 to 0.67; p < 0.001) with reduced likelihood of regional lymph node and distant metastasis (odds ratio, 0.33; 95% CI, 0.21 to 0.53; p < 0.001 and odds ratio, 0.49; 95% CI, 0.27 to 0.89; p = 0.02, respectively). Several other case series of early-onset CRC indicate MSI-H rates ranging between 29.4 and 73%, with clear evidence that MSI frequency is inversely proportional to age at diagnosis and directly proportional to the Lynch syndrome component [2, 121,122,123,124,125,126,127].
MSI-H tumors correlate with improved survival, as shown in the study by Gryfe et al. among others [120, 128]. Moreover, presence of a BRAF mutation in the setting of MSI-H tumors does not infer a poor prognosis, unlike microsatellite stable or low tumors (MSS/MSI-L) [129]. Younger adults with CRC have almost identical or even better survival when matched stage for stage to older patients, which likely relates to this higher MSI-H frequency [100, 130].
A third pathway involved in CRC pathogenesis is CIMP which leads to gene silencing and is responsible for ∼40% of all CRCs [131]. CIMP-high tumors are typically found in a proximal colonic location, are poorly differentiated, with higher frequency of MSI, and BRAF mutations, and also association with p53 mutations [112, 132, 133]. A higher rate of CIMP-low cases has been observed in the early-onset CRC population. One caveat to this is an increased frequency of CIMP-high tumors within Lynch syndrome patients with early-onset compared to late-onset CRC. Perea et al. evaluated early-onset CRC relative to late-onset cases according to these three main carcinogenic pathways [131]. This study reinforced an association between early-onset CIMP-high CRCs and germline MMR gene mutations. On the other hand, late-onset CIMP-high CRCs were more likely to be sporadic MSI tumors, with high BRAF mutation rates. Predominant left colon location for early-onset CRCs, with an increased frequency of CIMP-low cases and an important familial component, was noted.
Another subset of CRCs identified most commonly in younger patients is so-called microsatellite and chromosome stable CRC (MACS). These tumors are most frequently located in the distal colon and rectum, have histologic features correlated with poor prognosis, present with metastases at diagnosis, recur early, and have some familial aggregation for Lynch syndrome neoplasms [134,135,136]. Understanding of the molecular landscape of MACS is limited. Various studies reveal that MACS tumors are CIMP-low, have rare BRAF mutations, absent MLH1 expression, and a different hypomethylation pattern compared to CIN and MSI CRC. One possible explanation is that LINE-1 hypomethylation, a marker of genome-wide hypomethylation and a unique feature of early-onset CRC, is related to MACS [137,138,139,140]. LINE-1 hypomethylation is also associated with a family history of CRC. CIMP-high and MSI-high tumors are inversely correlated, while MSS tumors are associated with LINE-1 hypomethylation [141].
Early-onset CRCs have been categorized into four molecular subtypes according to age of onset: early-onset MSS, early-onset MSI/CIMP-high, early-onset MSS/CIMP-high, and early-onset MSS/CIMP-low [131]. Each subtype differs in tumor location, BRAF mutation status, and family history. The first subtype, early-onset MSS, is characterized by CRCs more commonly located in the left colon and proven family history as compared with older patients. In the second subtype, MSI/CIMP-high early-onset CRC cases are chiefly related to Lynch syndrome, whereas BRAF V600E mutations were present in the late-onset cases. In the third subtype, early-onset MSS/CIMP-high CRCs had increased frequency of mucinous subtype and right-sided tumors compared to elderly cases. Finally, the early-onset MSS/CIMP-low subgroup contrasted with the older patients in terms of location, stage, incidence of primary neoplasms, and family history.
Regarding other hereditary syndromes involved in early-onset CRC, knowledge about the dominant underlying mutations is in general better characterized than in sporadic cases. FAP, as mentioned previously, is caused by a germline mutation in the APC tumor suppressor gene [142]. Most commonly, a nonsense or frameshift mutation occurs which leads to premature truncation of the APC protein [143]. A link between the APC mutation location and the phenotype in FAP patients has been documented [144]. MUTYH-associated polyposis is defined by an MUTYH gene mutation, most frequently Y179C and G396D. Homozygous Y179C mutation status is characterized by more severe phenotype compared with the G396D allele [145]. Germline mutation of the STK11/LKB1 tumor suppressor gene is known to be the underlying defect in Peutz-Jeghers Syndrome, found in 70–80% of affected families, with multiple mutations in STK11/LKB1 leading to phenotypic variability [146, 147]. Juvenile polyposis syndrome is related to germline mutations in SMAD4 and BMPR1A [148]. Cowden syndrome is caused by germline alterations in the PTEN tumor suppressor gene found in chromosome 10q23 [149].
Finally, a distinct subset of early-onset CRCs exists which have notably more aggressive tumor biology, with resultant inferior outcomes [150,151,152]. These tumors are typically mucin-producing, poorly differentiated, with signet ring histology. The rate of mucin-producing tumors is inversely proportional to the age at diagnosis. The underlying mechanisms responsible for the more aggressive tumor biology among young patients remain unknown [103, 122, 153].
Implications for treatment
As outlined, early-onset CRC is characterized by more advanced stage, poorly differentiated tumors, mucinous neoplasms, more distal location, and a unique biomarker profile. Yet despite this, survival outcomes for young patients, stage for stage, consistently match or even exceed that of older patients [3]. Given this conflict, optimal treatment for early-onset CRC remains unclear.
A study by Kneuertz et al. explored treatment patterns and prognosis in young CRC patients [4]. This review reinforced that younger age at onset correlated with both advanced presentation and worse histologic characteristics. Increased use of systemic chemotherapy in younger patients, especially multi-agent regimens, was observed at all disease stages compared to those with late-onset CRC. Despite more intensive treatment, young patients experienced only minimal survival gain relative to older patients who received less treatment. In the absence of clear superiority regarding efficacy, a considerable portion of young patients are receiving unnecessary treatments with potential long-term toxicity.
A better understanding of the underlying molecular landscape is critical to help tailor prevention strategies and treatment options in this distinct subset of patients with early-onset CRC. It is known that MMR-deficient tumors, both sporadic and inherited, do not benefit from fluorouracil-based chemotherapy, and stage II patients with MMR-deficient tumors may, in fact, have impaired survival when treated with adjuvant therapy rather than surgery alone [154]. In addition, MSI-H status, which as we know is more common in early-onset CRC, has relatively good prognosis, so chemotherapy is generally discouraged. NCCN guidelines recommend that MSI/MMR testing be performed on stage II patients if chemotherapy is being considered to avoid overtreatment [155].
In this new era of next-generation sequencing, we are learning more about the molecular make-up of tumors, but further work is needed. Recent studies have highlighted key differences in terms of somatic gene mutations and DNA methylation in early-onset CRC cases relative to older patients [156•, 157]. Such ongoing efforts, with increased focus on tissue banking and multigene assays, provide us with the opportunity to expand our understanding of the molecular biology underlying these tumors. Currently, early-onset CRC patients are treated in a similar fashion to late-onset cases, but with fundamental differences in tumor biology, it is clear that continued research is critical to translate knowledge of unique molecular alterations into new, meaningful treatment options and provide individualized therapies in this novel patient population to truly impact survival outcomes.
Conclusion
The rising incidence of CRC in younger patients, with consequent increasing mortality, over the past few decades is well documented. This is a patient population where use of screening is limited and often critical symptoms go unrecognized. While we are continuing to learn and understand more about the epidemiologic, clinicopathologic, genetic, and molecular factors leading to this apparent epidemic, there remains a huge dearth of knowledge. Furthermore, marked heterogeneity in the underlying mechanisms of early-onset CRC has significant implications for the prevention, diagnosis, and management of these individuals.
From recent clinical studies, we appreciate more and more that early-onset CRC is a separate entity to late-onset CRC, with a distinct tumor biology. While current treatment paradigms do not differentiate based on age of disease onset, it is clear that moving forward there is a need to focus on tissue banking and tumoral mutational sequencing to untangle the hidden pieces of the puzzle to refine therapies for this patient group. With a lack of evidence base currently to inform us on whether certain molecular alterations merit a more specific treatment approach, there is a definite role for clinical trials in this patient population to adequately address this.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi:10.3322/caac.20107.
Perea J, Rodríguez Y, Rueda D, Marín JC, Díaz-Tasende J, Álvaro E, et al. Early-onset colorectal cancer is an easy and effective tool to identify retrospectively Lynch syndrome. Ann Surg Oncol. 2011;18:3285–91. doi:10.1245/s10434-011-1782-4.
Wang M-J, Ping J, Li Y, Adell G, Arbman G, Nodin B, et al. The prognostic factors and multiple biomarkers in young patients with colorectal cancer. Sci Rep. 2015;5:10645. doi:10.1038/srep10645.
Kneuertz PJ, Chang GJ, Hu C-Y, Rodriguez-Bigas MA, Eng C, Vilar E, et al. Overtreatment of young adults with colon cancer: more intense treatments with unmatched survival gains. JAMA Surg. 2015;150:402–9. doi:10.1001/jamasurg.2014.3572.
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–86. doi:10.1002/ijc.29210.
Howlader N, Noone A, Krapcho M, Miller D, K Bishop, SF Altekruse, et al. SEER cancer statistics review, 1975–2013. In: SEER web site [Internet]. 2016. Available: http://seer.cancer.gov/csr/1975_2013/.
Singh KE, Taylor TH, Pan C-JG, Stamos MJ, Zell JA. Colorectal cancer incidence among young adults in California. J Adolesc Young Adult Oncol. 2014;3:176–84. doi:10.1089/jayao.2014.0006.
Young JP, Win AK, Rosty C, Flight I, Roder D, Young GP, et al. Rising incidence of early-onset colorectal cancer in Australia over two decades: report and review. J Gastroenterol Hepatol. 2015;30:6–13. doi:10.1111/jgh.12792.
• Bailey CE, Hu C-Y, You YN, Bednarski BK, Rodriguez-Bigas MA, Skibber JM, et al. Increasing disparities in the age-related incidences of colon and rectal cancers in the United States, 1975-2010. JAMA Surg. 2015;150:17–22. doi:10.1001/jamasurg.2014.1756. This retrospective cohort study based on the SEER CRC registry confirms the apparent increase in the incidence of CRC in young adults and a decline in older patients
Bhandari A, Woodhouse M, Gupta S. Colorectal cancer is a leading cause of cancer incidence and mortality among adults younger than 50 years in the USA: a SEER-based analysis with comparison to other young-onset cancers. J Investig Med. 2016; doi:10.1136/jim-2016-000229.
Meyer JE, Narang T, Schnoll-Sussman FH, Pochapin MB, Christos PJ, Sherr DL. Increasing incidence of rectal cancer in patients aged younger than 40 years: an analysis of the surveillance, epidemiology, and end results database. Cancer. 2010;116:4354–9. doi:10.1002/cncr.25432.
Austin H, Henley SJ, King J, Richardson LC, Eheman C. Changes in colorectal cancer incidence rates in young and older adults in the United States: what does it tell us about screening. Cancer Causes Control. 2014;25:191–201. doi:10.1007/s10552-013-0321-y.
O’Connell JB, Maggard MA, Liu JH, Etzioni DA, Livingston EH, Ko CY. Rates of colon and rectal cancers are increasing in young adults. Am Surg. 2003;69:866–72. Available: http://www.ncbi.nlm.nih.gov/pubmed/14570365
Siegel RL, Jemal A, Ward EM. Increase in incidence of colorectal cancer among young men and women in the United States. Cancer Epidemiol Biomark Prev. 2009;18:1695–8. doi:10.1158/1055-9965.EPI-09-0186.
You YN, Xing Y, Feig BW, Chang GJ, Cormier JN. Young-onset colorectal cancer: is it time to pay attention? Arch Intern Med. 2012;172:287–9. doi:10.1001/archinternmed.2011.602.
Griffin PM, Liff JM, Greenberg RS, Clark WS. Adenocarcinomas of the colon and rectum in persons under 40 years old. A population-based study. Gastroenterology. 1991;100:1033–40. Available: http://www.ncbi.nlm.nih.gov/pubmed/2001800
Rahman R, Schmaltz C, Jackson CS, Simoes EJ, Jackson-Thompson J, Ibdah JA. Increased risk for colorectal cancer under age 50 in racial and ethnic minorities living in the United States. Cancer Med. 2015;4:1863–70. doi:10.1002/cam4.560.
Ashktorab H, Vilmenay K, Brim H, Laiyemo AO, Kibreab A, Nouraie M. Colorectal cancer in young African Americans: is it time to revisit guidelines and prevention? Dig Dis Sci. 2016;61:3026–30. doi:10.1007/s10620-016-4207-1.
• Holowatyj AN, Ruterbusch JJ, Rozek LS, Cote ML, Stoffel EM. Racial/ethnic disparities in survival among patients with young-onset colorectal cancer. J Clin Oncol. 2016;34:2148–56. doi:10.1200/JCO.2015.65.0994. Using the SEER database, the survival of patients with young-onset CRC (aged <50 years) was assessed. It was observed that the survival for CRC diagnosed at a young age is significantly worse among non-Hispanic Black patients compared to non-Hispanic White patients, even in the setting of early-stage disease
Dozois EJ, Boardman LA, Suwanthanma W, Limburg PJ, Cima RR, Bakken JL, et al. Young-onset colorectal cancer in patients with no known genetic predisposition: can we increase early recognition and improve outcome? Medicine (Baltimore). 2008;87:259–63. doi:10.1097/MD.0b013e3181881354.
O’Connell JB, Maggard MA, Liu JH, Etzioni DA, Livingston EH, Ko CY. Do young colon cancer patients have worse outcomes? World J Surg. 2004;28:558–62. Available: http://www.ncbi.nlm.nih.gov/pubmed/15366745
Taggarshe D, Rehil N, Sharma S, Flynn JC, Damadi A. Colorectal cancer: are the “young” being overlooked? Am J Surg. 2013;205:312–6. discussion 316 doi:10.1016/j.amjsurg.2012.10.016.
Teng A, Lee DY, Cai J, Patel SS, Bilchik AJ, Goldfarb MR. Patterns and outcomes of colorectal cancer in adolescents and young adults. J Surg Res. 2016;205:19–27. doi:10.1016/j.jss.2016.05.036.
Abdelsattar ZM, Wong SL, Regenbogen SE, Jomaa DM, Hardiman KM, Hendren S. Colorectal cancer outcomes and treatment patterns in patients too young for average-risk screening. Cancer. 2016;122:929–34. doi:10.1002/cncr.29716.
Chen FW, Sundaram V, Chew TA, Ladabaum U. Advanced stage colorectal cancer in persons younger than 50 years not associated with longer duration of symptoms or time to diagnosis. Clin Gastroenterol Hepatol. 2016; doi:10.1016/j.cgh.2016.10.038.
Lisa A, Boardman EB. Genetics of young onset colorectal cancer. J Bone Marrow Res. 2014;3 doi:10.4172/2161-1041.1000124.
Aarnio M. Clinicopathological features and management of cancers in Lynch syndrome. Patholog Res Int. 2012;2012:350309. doi:10.1155/2012/350309.
Peltomäki P. Role of DNA mismatch repair defects in the pathogenesis of human cancer. J Clin Oncol. 2003;21:1174–9. doi:10.1200/JCO.2003.04.060.
Stoffel E, Mukherjee B, Raymond VM, Tayob N, Kastrinos F, Sparr J, et al. Calculation of risk of colorectal and endometrial cancer among patients with Lynch syndrome. Gastroenterology. 2009;137:1621–7. doi:10.1053/j.gastro.2009.07.039.
Lynch HT, de la Chapelle A. Hereditary colorectal cancer. N Engl J Med. 2003;348:919–32. doi:10.1056/NEJMra012242.
Watson P, Lin KM, Rodriguez-Bigas MA, Smyrk T, Lemon S, Shashidharan M, et al. Colorectal carcinoma survival among hereditary nonpolyposis colorectal carcinoma family members. Cancer. 1998;83:259–66. Available: http://www.ncbi.nlm.nih.gov/pubmed/9669808
Senter L, Clendenning M, Sotamaa K, Hampel H, Green J, Potter JD, et al. The clinical phenotype of Lynch syndrome due to germ-line PMS2 mutations. Gastroenterology. 2008;135:419–28. doi:10.1053/j.gastro.2008.04.026.
Bonadona V, Bonaïti B, Olschwang S, Grandjouan S, Huiart L, Longy M, et al. Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. JAMA. 2011;305:2304–10. doi:10.1001/jama.2011.743.
Wennstrom J, Pierce ER, McKusick VA. Hereditary benign and malignant lesions of the large bowel. Cancer. 1974;34:850–7. Available: http://www.ncbi.nlm.nih.gov/pubmed/4604530
Kastrinos F, Syngal S. Inherited colorectal cancer syndromes. Cancer J. 2011;17:405–15. doi:10.1097/PPO.0b013e318237e408.
Galiatsatos P, Foulkes WD. Familial adenomatous polyposis. Am J Gastroenterol. 2006;101:385–98. doi:10.1111/j.1572-0241.2006.00375.x.
Cruz-Correa M, Giardiello FM. Familial adenomatous polyposis. Gastrointest Endosc. 2003;58:885–94. Available: http://www.ncbi.nlm.nih.gov/pubmed/14652558
Patel SG, Ahnen DJ. Familial colon cancer syndromes: an update of a rapidly evolving field. Curr Gastroenterol Rep. 2012;14:428–38. doi:10.1007/s11894-012-0280-6.
Jasperson KW, Tuohy TM, Neklason DW, Burt RW. Hereditary and familial colon cancer. Gastroenterology. 2010;138:2044–58. doi:10.1053/j.gastro.2010.01.054.
Half E, Bercovich D, Rozen P. Familial adenomatous polyposis. Orphanet J Rare Dis. 2009;4:22. doi:10.1186/1750-1172-4-22.
Lubbe SJ, Di Bernardo MC, Chandler IP, Houlston RS. Clinical implications of the colorectal cancer risk associated with MUTYH mutation. J Clin Oncol. 2009;27:3975–80. doi:10.1200/JCO.2008.21.6853.
Sampson JR, Dolwani S, Jones S, Eccles D, Ellis A, Evans DG, et al. Autosomal recessive colorectal adenomatous polyposis due to inherited mutations of MYH. Lancet (London, England). 2003;362:39–41. doi:10.1016/S0140-6736(03)13805-6.
Jenkins MA, Croitoru ME, Monga N, Cleary SP, Cotterchio M, Hopper JL, et al. Risk of colorectal cancer in monoallelic and biallelic carriers of MYH mutations: a population-based case-family study. Cancer Epidemiol Biomark Prev. 2006;15:312–4. doi:10.1158/1055-9965.EPI-05-0793.
van Lier MGF, Wagner A, Mathus-Vliegen EMH, Kuipers EJ, Steyerberg EW, van Leerdam ME. High cancer risk in Peutz–Jeghers syndrome: a systematic review and surveillance recommendations. Am J Gastroenterol. 2010;105:1258–64. doi:10.1038/ajg.2009.725.
Jass JR, Williams CB, Bussey HJ, Morson BC. Juvenile polyposis—a precancerous condition. Histopathology. 1988;13:619–30. Available: http://www.ncbi.nlm.nih.gov/pubmed/2853131
Lachlan KL. Cowden syndrome and the PTEN hamartoma tumor syndrome: how to define rare genetic syndromes. J Natl Cancer Inst. 2013;105:1595–7. doi:10.1093/jnci/djt290.
Win AK, Walters RJ, Buchanan DD, Jenkins MA, Sweet K, Frankel WL, et al. Cancer risks for relatives of patients with serrated polyposis. Am J Gastroenterol. 2012;107:770–8. doi:10.1038/ajg.2012.52.
Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002;288:1723–7. Available: http://www.ncbi.nlm.nih.gov/pubmed/12365955
Centers for Disease Control and Prevention (CDC). Trends in leisure-time physical inactivity by age, sex, and race/ethnicity—United States, 1994-2004. MMWR Morb Mortal Wkly Rep. 2005;54:991–4. Available: http://www.ncbi.nlm.nih.gov/pubmed/16208312
Pan SY, DesMeules M. Energy intake, physical activity, energy balance, and cancer: epidemiologic evidence. Methods Mol Biol. 2009;472:191–215. doi:10.1007/978-1-60327-492-0_8.
Slattery ML, Sorenson AW, Mahoney AW, French TK, Kritchevsky D, Street JC. Diet and colon cancer: assessment of risk by fiber type and food source. JNCI J Natl Cancer Inst. 1988;80:1474–80. doi:10.1093/jnci/80.18.1474.
Crosara Teixeira M, Braghiroli MI, Sabbaga J, Hoff PM. Primary prevention of colorectal cancer: myth or reality? World J Gastroenterol. 2014;20:15060–9. doi:10.3748/wjg.v20.i41.15060.
Lin J. Dietary fat and fatty acids and risk of colorectal cancer in women. Am J Epidemiol. 2004;160:1011–22. doi:10.1093/aje/kwh319.
Karahalios A, English DR, Simpson JA. Weight change and risk of colorectal cancer: a systematic review and meta-analysis. Am J Epidemiol. 2015;181:832–45. doi:10.1093/aje/kwu357.
Wolin KY, Yan Y, Colditz GA, Lee I-M. Physical activity and colon cancer prevention: a meta-analysis. Br J Cancer. 2009;100:611–6. doi:10.1038/sj.bjc.6604917.
Yuhara H, Steinmaus C, Cohen SE, Corley DA, Tei Y, Buffler PA. Is diabetes mellitus an independent risk factor for colon cancer and rectal cancer? Am J Gastroenterol. 2011;106:1911–21. doi:10.1038/ajg.2011.301.
Botteri E, Iodice S, Bagnardi V, Raimondi S, Lowenfels AB, Maisonneuve P. Smoking and colorectal cancer: a meta-analysis. JAMA. 2008;300:2765–78. doi:10.1001/jama.2008.839.
Wallace K, Grau MV, Ahnen D, Snover DC, Robertson DJ, Mahnke D, et al. The association of lifestyle and dietary factors with the risk for serrated polyps of the colorectum. Cancer Epidemiol Biomark Prev. 2009;18:2310–7. doi:10.1158/1055-9965.EPI-09-0211.
Botteri E, Iodice S, Raimondi S, Maisonneuve P, Lowenfels AB. Cigarette smoking and adenomatous polyps: a meta-analysis. Gastroenterology. 2008;134:388–95. doi:10.1053/j.gastro.2007.11.007.
Fedirko V, Tramacere I, Bagnardi V, Rota M, Scotti L, Islami F, et al. Alcohol drinking and colorectal cancer risk: an overall and dose-response meta-analysis of published studies. Ann Oncol Off J Eur Soc Med Oncol. 2011;22:1958–72. doi:10.1093/annonc/mdq653.
Cho E, Smith-Warner SA, Ritz J, van den Brandt PA, Colditz GA, Folsom AR, et al. Alcohol intake and colorectal cancer: a pooled analysis of 8 cohort studies. Ann Intern Med. 2004;140:603–13. Available: http://www.ncbi.nlm.nih.gov/pubmed/15096331
Mizoue T, Inoue M, Wakai K, Nagata C, Shimazu T, Tsuji I, et al. Alcohol drinking and colorectal cancer in Japanese: a pooled analysis of results from five cohort studies. Am J Epidemiol. 2008;167:1397–406. doi:10.1093/aje/kwn073.
Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300. doi:10.3322/caac.20073.
Lynch KL, Ahnen DJ, Byers T, Weiss DG, Lieberman DA. First-degree relatives of patients with advanced colorectal adenomas have an increased prevalence of colorectal cancer. Clin Gastroenterol Hepatol. 2003;1:96–102. doi:10.1053/cgh.2003.50018.
Lieberman DA, Prindiville S, Weiss DG, Willett W, VA Cooperative Study Group 380. Risk factors for advanced colonic neoplasia and hyperplastic polyps in asymptomatic individuals. JAMA. 2003;290:2959–67. doi:10.1001/jama.290.22.2959.
Fuchs CS, Giovannucci EL, Colditz GA, Hunter DJ, Speizer FE, Willett WC. A prospective study of family history and the risk of colorectal cancer. N Engl J Med. 1994;331:1669–74. doi:10.1056/NEJM199412223312501.
Butterworth AS, Higgins JPT, Pharoah P. Relative and absolute risk of colorectal cancer for individuals with a family history: a meta-analysis. Eur J Cancer. 2006;42:216–27. doi:10.1016/j.ejca.2005.09.023.
Lieberman DA, Rex DK, Winawer SJ, Giardiello FM, Johnson DA, Levin TR, et al. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012;143:844–57. doi:10.1053/j.gastro.2012.06.001.
Qaseem A, Denberg TD, Hopkins RH, Humphrey LL, Levine J, Sweet DE, et al. Screening for colorectal cancer: a guidance statement from the American College of Physicians. Ann Intern Med. 2012;156:378–86. doi:10.7326/0003-4819-156-5-201203060-00010.
Gupta AK, Samadder J, Elliott E, Sethi S, Schoenfeld P. Prevalence of any size adenomas and advanced adenomas in 40- to 49-year-old individuals undergoing screening colonoscopy because of a family history of colorectal carcinoma in a first-degree relative. Gastrointest Endosc. 2011;74:110–8. doi:10.1016/j.gie.2011.02.010.
Garcia GH, Riechelmann RP, Hoff PM. Adherence to colonoscopy recommendations for first-degree relatives of young patients diagnosed with colorectal cancer. Clinics (Sao Paulo). 2015;70:696–9. doi:10.6061/clinics/2015(10)07.
Akhtar S, Sinha S, McKenzie S, Sagar PM, Finan PJ, Burke D. Awareness of risk factors amongst first degree relative patients with colorectal cancer. Color Dis. 2008;10:887–90. doi:10.1111/j.1463-1318.2008.01502.x.
Hogan NM, Hanley M, Hogan AM, Sheehan M, McAnena OJ, Regan MP, et al. Awareness and uptake of family screening in patients diagnosed with colorectal cancer at a young age. Gastroenterol Res Pract. 2015;2015:194931. doi:10.1155/2015/194931.
Austin GL, Goldstein JI, Peters SL, Ahnen DJ. Are colorectal cancer screening recommendations for first-degree relatives of patients with adenomas too aggressive? Clin Gastroenterol Hepatol. 2011;9:308–13. doi:10.1016/j.cgh.2011.01.004.
Giardiello FM, Allen JI, Axilbund JE, Boland CR, Burke CA, Burt RW, et al. Guidelines on genetic evaluation and management of Lynch syndrome: a consensus statement by the US Multi-Society Task Force on Colorectal Cancer. Dis Colon Rectum. 2014;57:1025–48. doi:10.1097/DCR.000000000000000.
Stoffel EM, Mangu PB, Gruber SB, Hamilton SR, Kalady MF, Lau MWY, et al. Hereditary colorectal cancer syndromes: American Society of Clinical Oncology Clinical Practice Guideline endorsement of the familial risk-colorectal cancer: European Society for Medical Oncology Clinical Practice Guidelines. J Clin Oncol. 2015;33:209–17. doi:10.1200/JCO.2014.58.1322.
Balmaña J, Balaguer F, Cervantes A, Arnold D, ESMO Guidelines Working Group. Familial risk-colorectal cancer: ESMO Clinical Practice Guidelines. Ann Oncol Off J Eur Soc Med Oncol. 2013;24(Suppl 6):vi73–80. doi:10.1093/annonc/mdt209.
Barrow P, Khan M, Lalloo F, Evans DG, Hill J. Systematic review of the impact of registration and screening on colorectal cancer incidence and mortality in familial adenomatous polyposis and Lynch syndrome. Br J Surg. 2013;100:1719–31. doi:10.1002/bjs.9316.
Järvinen HJ, Aarnio M, Mustonen H, Aktan-Collan K, Aaltonen LA, Peltomäki P, et al. Controlled 15-year trial on screening for colorectal cancer in families with hereditary nonpolyposis colorectal cancer. Gastroenterology. 2000;118:829–34. Available: http://www.ncbi.nlm.nih.gov/pubmed/10784581
Syngal S, Weeks JC, Schrag D, Garber JE, Kuntz KM. Benefits of colonoscopic surveillance and prophylactic colectomy in patients with hereditary nonpolyposis colorectal cancer mutations. Ann Intern Med. 1998;129:787–96. Available: http://www.ncbi.nlm.nih.gov/pubmed/9841584
Giardiello FM, Allen JI, Axilbund JE, Boland CR, Burke CA, Burt RW, et al. Guidelines on genetic evaluation and management of Lynch syndrome: a consensus statement by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2014;147:502–26. doi:10.1053/j.gastro.2014.04.001.
Vasen HFA, Möslein G, Alonso A, Aretz S, Bernstein I, Bertario L, et al. Guidelines for the clinical management of familial adenomatous polyposis (FAP). Gut. 2008;57:704–13. doi:10.1136/gut.2007.136127.
Syngal S, Brand RE, Church JM, Giardiello FM, Hampel HL, Burt RW, et al. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015;110:223–62. quiz 263 doi:10.1038/ajg.2014.435.
Provenzale D, Gupta S, Ahnen DJ, Bray T, Cannon JA, Cooper G, et al. Genetic/familial high-risk assessment: colorectal version 1.2016, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2016;14:1010–30. Available: http://www.ncbi.nlm.nih.gov/pubmed/27496117
Sengupta N, Yee E, Feuerstein JD. Colorectal cancer screening in inflammatory bowel disease. Dig Dis Sci. 2016;61:980–9. doi:10.1007/s10620-015-3979-z.
Söderlund S, Brandt L, Lapidus A, Karlén P, Broström O, Löfberg R, et al. Decreasing time-trends of colorectal cancer in a large cohort of patients with inflammatory bowel disease. Gastroenterology. 2009;136:1561–7. Available: http://www.ncbi.nlm.nih.gov/pubmed/19422077
Beaugerie L, Itzkowitz SH. Cancers complicating inflammatory bowel disease. N Engl J Med. 2015;372:1441–52. doi:10.1056/NEJMra1403718.
Lopez A, Collet-Fenetrier B, Belle A, Peyrin-Biroulet L. Patients’ knowledge and fear of colorectal cancer risk in inflammatory bowel disease. J Dig Dis. 2016;17:383–91. doi:10.1111/1751-2980.12356.
Kornbluth A, Sachar DB, Practice Parameters Committee of the American College of Gastroenterology. Ulcerative colitis practice guidelines in adults: American College of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol. 2010;105:501–23. quiz 524 doi:10.1038/ajg.2009.727.
American Society for Gastrointestinal Endoscopy Standards of Practice Committee, Shergill AK, Lightdale JR, Bruining DH, Acosta RD, Chandrasekhara V, et al. The role of endoscopy in inflammatory bowel disease. Gastrointest Endosc. 2015;81:1101–21.e1-13. doi:10.1016/j.gie.2014.10.030.
Cairns SR, Scholefield JH, Steele RJ, Dunlop MG, Thomas HJW, Evans GD, et al. Guidelines for colorectal cancer screening and surveillance in moderate and high risk groups (update from 2002). Gut. 2010;59:666–89. doi:10.1136/gut.2009.179804.
Soetikno R, Subramanian V, Kaltenbach T, Rouse RV, Sanduleanu S, Suzuki N, et al. The detection of nonpolypoid (flat and depressed) colorectal neoplasms in patients with inflammatory bowel disease. Gastroenterology. 2013;144:1349–52. 1352–6 doi:10.1053/j.gastro.2013.04.008.
Mooiweer E, van der Meulen-de Jong AE, Ponsioen CY, Fidder HH, Siersema PD, Dekker E, et al. Chromoendoscopy for surveillance in inflammatory bowel disease does not increase neoplasia detection compared with conventional colonoscopy with random biopsies: results from a large retrospective study. Am J Gastroenterol. 2015;110:1014–21. doi:10.1038/ajg.2015.63.
Bopanna S, Roy M, Das P, Dattagupta S, Sreenivas V, Mouli VP, et al. Role of random biopsies in surveillance of dysplasia in ulcerative colitis patients with high risk of colorectal cancer. Intest Res. 2016;14:264–9. doi:10.5217/ir.2016.14.3.264.
Edwards BK, Ward E, Kohler BA, Eheman C, Zauber AG, Anderson RN, et al. Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010;116:544–73. doi:10.1002/cncr.24760.
US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW, et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2016;315:2564–75. doi:10.1001/jama.2016.5989.
Ahnen DJ, Wade SW, Jones WF, Sifri R, Mendoza Silveiras J, Greenamyer J, et al. The increasing incidence of young-onset colorectal cancer: a call to action. Mayo Clin Proc. 2014;89:216–24. doi:10.1016/j.mayocp.2013.09.006.
Williams R, White P, Nieto J, Vieira D, Francois F, Hamilton F. Colorectal cancer in African Americans: an update. Clin Transl Gastroenterol. 2016;7:e185. doi:10.1038/ctg.2016.36.
Rex DK, Johnson DA, Anderson JC, Schoenfeld PS, Burke CA, Inadomi JM, et al. American College of Gastroenterology guidelines for colorectal cancer screening 2009 [corrected]. Am J Gastroenterol. 2009;104:739–50. doi:10.1038/ajg.2009.104.
O’Connell JB, Maggard MA, Livingston EH, Yo CK. Colorectal cancer in the young. Am J Surg. 2004;187:343–8. doi:10.1016/j.amjsurg.2003.12.020.
Kim TJ, Kim ER, Hong SN, Chang DK, Kim Y-H. Long-term outcome and prognostic factors of sporadic colorectal cancer in young patients: a large institutional-based retrospective study. Medicine (Baltimore). 2016;95:e3641. doi:10.1097/MD.0000000000003641.
Scott RB, Rangel LE, Osler TM, Hyman NH. Rectal cancer in patients under the age of 50 years: the delayed diagnosis. Am J Surg. 2016;211:1014–8. doi:10.1016/j.amjsurg.2015.08.031.
Bleyer A, Barr R, Hayes-Lattin B, Thomas D, Ellis C, Anderson B, et al. The distinctive biology of cancer in adolescents and young adults. Nat Rev Cancer. 2008;8:288–98. doi:10.1038/nrc2349.
Stigliano V, Sanchez-Mete L, Martayan A, Anti M. Early-onset colorectal cancer: a sporadic or inherited disease? World J Gastroenterol. 2014;20:12420–30. doi:10.3748/wjg.v20.i35.12420.
de la Chapelle A. Microsatellite instability. N Engl J Med. 2003;349:209–10. doi:10.1056/NEJMp038099.
Sameer AS. Colorectal cancer: molecular mutations and polymorphisms. Front Oncol. 2013;3:114. doi:10.3389/fonc.2013.00114.
Armaghany T, Wilson JD, Chu Q, Mills G. Genetic alterations in colorectal cancer. Gastrointest Cancer Res. 2012;5:19–27. Available: http://www.ncbi.nlm.nih.gov/pubmed/22574233
Pino MS, Chung DC. The chromosomal instability pathway in colon cancer. Gastroenterology. 2010;138:2059–72. doi:10.1053/j.gastro.2009.12.065.
Sameer AS, Nissar S, Fatima K. Mismatch repair pathway: molecules, functions, and role in colorectal carcinogenesis. Eur J Cancer Prev. 2014;23:246–57. doi:10.1097/CEJ.0000000000000019.
Migliore L, Migheli F, Spisni R, Coppedè F. Genetics, cytogenetics, and epigenetics of colorectal cancer. J Biomed Biotechnol. 2011;2011:792362. doi:10.1155/2011/792362.
Chang DT, Pai RK, Rybicki LA, Dimaio MA, Limaye M, Jayachandran P, et al. Clinicopathologic and molecular features of sporadic early-onset colorectal adenocarcinoma: an adenocarcinoma with frequent signet ring cell differentiation, rectal and sigmoid involvement, and adverse morphologic features. Mod Pathol. 2012;25:1128–39. doi:10.1038/modpathol.2012.61.
Snover DC. Update on the serrated pathway to colorectal carcinoma. Hum Pathol. 2011;42:1–10. doi:10.1016/j.humpath.2010.06.002.
Raut CP, Pawlik TM, Rodriguez-Bigas MA. Clinicopathologic features in colorectal cancer patients with microsatellite instability. Mutat Res. 2004;568:275–82. doi:10.1016/j.mrfmmm.2004.05.025.
Cunningham D, Atkin W, Lenz H-J, Lynch HT, Minsky B, Nordlinger B, et al. Colorectal cancer. Lancet (London, England). 2010;375:1030–47. doi:10.1016/S0140-6736(10)60353-4.
Grady WM. Genomic instability and colon cancer. Cancer Metastasis Rev. 23:11–27. Available: http://www.ncbi.nlm.nih.gov/pubmed/15000146
Aaltonen LA, Peltomäki P, Leach FS, Sistonen P, Pylkkänen L, Mecklin JP, et al. Clues to the pathogenesis of familial colorectal cancer. Science. 1993;260:812–6. Available: http://www.ncbi.nlm.nih.gov/pubmed/8484121
Kovacs ME, Papp J, Szentirmay Z, Otto S, Olah E. Deletions removing the last exon of TACSTD1 constitute a distinct class of mutations predisposing to Lynch syndrome. Hum Mutat. 2009;30:197–203. doi:10.1002/humu.20942.
Kempers MJE, Kuiper RP, Ockeloen CW, Chappuis PO, Hutter P, Rahner N, et al. Risk of colorectal and endometrial cancers in EPCAM deletion-positive Lynch syndrome: a cohort study. Lancet Oncol. 2011;12:49–55. doi:10.1016/S1470-2045(10)70265-5.
Boland CR, Thibodeau SN, Hamilton SR, Sidransky D, Eshleman JR, Burt RW, et al. A National Cancer Institute Workshop on Microsatellite Instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res. 1998;58:5248–57. Available: http://www.ncbi.nlm.nih.gov/pubmed/9823339
Gryfe R, Kim H, Hsieh ET, Aronson MD, Holowaty EJ, Bull SB, et al. Tumor microsatellite instability and clinical outcome in young patients with colorectal cancer. N Engl J Med. 2000;342:69–77. doi:10.1056/NEJM200001133420201.
Losi L, Di Gregorio C, Pedroni M, Ponti G, Roncucci L, Scarselli A, et al. Molecular genetic alterations and clinical features in early-onset colorectal carcinomas and their role for the recognition of hereditary cancer syndromes. Am J Gastroenterol. 2005;100:2280–7. doi:10.1111/j.1572-0241.2005.00223.x.
Datta RV, LaQuaglia MP, Paty PB. Genetic and phenotypic correlates of colorectal cancer in young patients. N Engl J Med. 2000;342:137–8. doi:10.1056/NEJM200001133420216.
Durno C, Aronson M, Bapat B, Cohen Z, Gallinger S. Family history and molecular features of children, adolescents, and young adults with colorectal carcinoma. Gut. 2005;54:1146–50. doi:10.1136/gut.2005.066092.
Liu B, Farrington SM, Petersen GM, Hamilton SR, Parsons R, Papadopoulos N, et al. Genetic instability occurs in the majority of young patients with colorectal cancer. Nat Med. 1995;1:348–52. Available: http://www.ncbi.nlm.nih.gov/pubmed/7585065
Lukish JR, Muro K, DeNobile J, Katz R, Williams J, Cruess DF, et al. Prognostic significance of DNA replication errors in young patients with colorectal cancer. Ann Surg. 1998;227:51–6. Available: http://www.ncbi.nlm.nih.gov/pubmed/9445110
Pucciarelli S, Agostini M, Viel A, Bertorelle R, Russo V, Toppan P, et al. Early-age-at-onset colorectal cancer and microsatellite instability as markers of hereditary nonpolyposis colorectal cancer. Dis Colon rectum. 2003;46:305–12. doi:10.1097/01.DCR.0000054881.56204.F3.
Liang JT, Huang KC, Cheng AL, Jeng YM, Wu MS, Wang SM. Clinicopathological and molecular biological features of colorectal cancer in patients less than 40 years of age. Br J Surg. 2003;90:205–14. doi:10.1002/bjs.4015.
Popat S, Hubner R, Houlston RS. Systematic review of microsatellite instability and colorectal cancer prognosis. J Clin Oncol. 2005;23:609–18. doi:10.1200/JCO.2005.01.086.
Roth AD, Tejpar S, Delorenzi M, Yan P, Fiocca R, Klingbiel D, et al. Prognostic role of KRAS and BRAF in stage II and III resected colon cancer: results of the translational study on the PETACC-3, EORTC 40993, SAKK 60-00 trial. J Clin Oncol. 2010;28:466–74. doi:10.1200/JCO.2009.23.3452.
Hubbard J, Thomas DM, Yothers G, Green E, Blanke C, O’Connell MJ, et al. Benefits and adverse events in younger versus older patients receiving adjuvant chemotherapy for colon cancer: findings from the Adjuvant Colon Cancer Endpoints data set. J Clin Oncol. 2012;30:2334–9. doi:10.1200/JCO.2011.41.1975.
Perea J, Rueda D, Canal A, Rodríguez Y, Álvaro E, Osorio I, et al. Age at onset should be a major criterion for subclassification of colorectal cancer. J Mol Diagn. 2014;16:116–26. doi:10.1016/j.jmoldx.2013.07.010.
Silla IO, Rueda D, Rodríguez Y, García JL, de la Cruz VF, Perea J. Early-onset colorectal cancer: a separate subset of colorectal cancer. World J Gastroenterol. 2014;20:17288–96. doi:10.3748/wjg.v20.i46.17288.
Nazemalhosseini Mojarad E, Kuppen PJ, Aghdaei HA, Zali MR. The CpG island methylator phenotype (CIMP) in colorectal cancer. Gastroenterol Hepatol from bed to bench. 2013;6:120–8. Available: http://www.ncbi.nlm.nih.gov/pubmed/24834258
Hawkins NJ, Tomlinson I, Meagher A, Ward RL. Microsatellite-stable diploid carcinoma: a biologically distinct and aggressive subset of sporadic colorectal cancer. Br J Cancer. 2001;84:232–6. doi:10.1054/bjoc.2000.1554.
Chan TL, Curtis LC, Leung SY, Farrington SM, Ho JW, Chan AS, et al. Early-onset colorectal cancer with stable microsatellite DNA and near-diploid chromosomes. Oncogene. 2001;20:4871–6. doi:10.1038/sj.onc.1204653.
Banerjea A, Hands RE, Powar MP, Bustin SA, Dorudi S. Microsatellite and chromosomal stable colorectal cancers demonstrate poor immunogenicity and early disease recurrence. Color Dis. 2009;11:601–8. doi:10.1111/j.1463-1318.2008.01639.x.
Ogino S, Nosho K, Kirkner GJ, Kawasaki T, Chan AT, Schernhammer ES, et al. A cohort study of tumoral LINE-1 hypomethylation and prognosis in colon cancer. J Natl Cancer Inst. 2008;100:1734–8. doi:10.1093/jnci/djn359.
Cai G, Xu Y, Lu H, Shi Y, Lian P, Peng J, et al. Clinicopathologic and molecular features of sporadic microsatellite- and chromosomal-stable colorectal cancers. Int J Color Dis. 2008;23:365–73. doi:10.1007/s00384-007-0423-7.
Silver A, Sengupta N, Propper D, Wilson P, Hagemann T, Patel A, et al. A distinct DNA methylation profile associated with microsatellite and chromosomal stable sporadic colorectal cancers. Int J Cancer. 2012;130:1082–92. doi:10.1002/ijc.26104.
Antelo M, Balaguer F, Shia J, Shen Y, Hur K, Moreira L, et al. A high degree of LINE-1 hypomethylation is a unique feature of early-onset colorectal cancer. PLoS One. 2012;7:e45357. doi:10.1371/journal.pone.0045357.
Baba Y, Huttenhower C, Nosho K, Tanaka N, Shima K, Hazra A, et al. Epigenomic diversity of colorectal cancer indicated by LINE-1 methylation in a database of 869 tumors. Mol Cancer. 2010;9:125. doi:10.1186/1476-4598-9-125.
Stoffel EM, Kastrinos F. Familial colorectal cancer, beyond Lynch syndrome. Clin Gastroenterol Hepatol. 2014;12:1059–68. doi:10.1016/j.cgh.2013.08.015.
Nagase H, Nakamura Y. Mutations of the APC (adenomatous polyposis coli) gene. Hum Mutat. 1993;2:425–34. doi:10.1002/humu.1380020602.
Nieuwenhuis MH, Vasen HFA. Correlations between mutation site in APC and phenotype of familial adenomatous polyposis (FAP): a review of the literature. Crit Rev Oncol Hematol. 2007;61:153–61. doi:10.1016/j.critrevonc.2006.07.004.
Terdiman JP. MYH-associated disease: attenuated adenomatous polyposis of the colon is only part of the story. Gastroenterology. 2009;137:1883–6. doi:10.1053/j.gastro.2009.10.017.
Campos FG, Figueiredo MN, Martinez CAR. Colorectal cancer risk in hamartomatous polyposis syndromes. World J Gastrointest Surg. 2015;7:25–32. doi:10.4240/wjgs.v7.i3.25.
Chen H-M, Fang J-Y. Genetics of the hamartomatous polyposis syndromes: a molecular review. Int J Color Dis. 2009;24:865–74. doi:10.1007/s00384-009-0714-2.
Schreibman IR, Baker M, Amos C, McGarrity TJ. The hamartomatous polyposis syndromes: a clinical and molecular review. Am J Gastroenterol. 2005;100:476–90. doi:10.1111/j.1572-0241.2005.40237.x.
Zbuk KM, Eng C. Cancer phenomics: RET and PTEN as illustrative models. Nat Rev Cancer. 2007;7:35–45. doi:10.1038/nrc2037.
LaQuaglia MP, Heller G, Filippa DA, Karasakalides A, Vlamis V, Wollner N, et al. Prognostic factors and outcome in patients 21 years and under with colorectal carcinoma. J Pediatr Surg. 1992;27:1085–9. Available: http://www.ncbi.nlm.nih.gov/pubmed/1403541
Chiang J-M, Chen M-C, Changchien CR, Chen J-S, Tang R, Wang J-Y, et al. Favorable influence of age on tumor characteristics of sporadic colorectal adenocarcinoma: patients 30 years of age or younger may be a distinct patient group. Dis Colon rectum. 2003;46:904–10. doi:10.1097/01.DCR.0000075210.01797.11.
Tricoli JV, Seibel NL, Blair DG, Albritton K, Hayes-Lattin B. Unique characteristics of adolescent and young adult acute lymphoblastic leukemia, breast cancer, and colon cancer. J Natl Cancer Inst. 2011;103:628–35. doi:10.1093/jnci/djr094.
Hill DA, Furman WL, Billups CA, Riedley SE, Cain AM, Rao BN, et al. Colorectal carcinoma in childhood and adolescence: a clinicopathologic review. J Clin Oncol. 2007;25:5808–14. doi:10.1200/JCO.2007.12.6102.
Sargent DJ, Marsoni S, Monges G, Thibodeau SN, Labianca R, Hamilton SR, et al. Defective mismatch repair as a predictive marker for lack of efficacy of fluorouracil-based adjuvant therapy in colon cancer. J Clin Oncol. 2010;28:3219–26. doi:10.1200/JCO.2009.27.1825.
National Comprehensive Cancer Network. NCCN guidelines—colon cancer [Internet]. Available: https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf.
• Ben-Aharon R, Pelossof R, Elkabets M. Early-onset colorectal cancer—does the difference lie in epigenetics? Eur Cancer Congr. 2015:Abstract 2189. doi:10.1016/S0959-8049(16)31108-X. This exploratory study investigated differences between somatic gene expression in cohorts of patients younger and older than age 50 years
Kirzin S, Marisa L, Guimbaud R, De Reynies A, Legrain M, Laurent-Puig P, et al. Sporadic early-onset colorectal cancer is a specific sub-type of cancer: a morphological, molecular and genetics study. PLoS One. 2014;9:e103159. doi:10.1371/journal.pone.0103159.
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat database: incidence—SEER 9 Regs Research Data, Nov 2015 Sub (1973–2013)<Katrina/Rita Population Adjustment>−Linked To County Attributes - Total U.S., 1969–2014 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch, released April 2016, based on the November 2015 submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Louise C. Connell, José Mauricio Mota, Maria Ignez Braghiroli, and Paulo M. Hoff declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Lower Gastrointestinal Cancers
Rights and permissions
About this article
Cite this article
Connell, L.C., Mota, J.M., Braghiroli, M.I. et al. The Rising Incidence of Younger Patients With Colorectal Cancer: Questions About Screening, Biology, and Treatment. Curr. Treat. Options in Oncol. 18, 23 (2017). https://doi.org/10.1007/s11864-017-0463-3
Published:
DOI: https://doi.org/10.1007/s11864-017-0463-3