Abstract
Background
There is little robust data on weight regain (WR) after bariatric surgery making it difficult to counsel patients regarding long-term outcomes of different bariatric procedures. The purpose of this study was to see WR in medium and long term after SG, RYGB, and OAGB in Indian population.
Methods
In a multicentre study, data on preoperative and postoperative weights over 5 years were collected. Multiple definitions were applied to find the proportion of patients with significant WR increase of 25% of lost weight from nadir (definition 1), weight gain of > 10 kg from nadir (definition 2), and BMI gain of > 5 kg/m2 from nadir (definition 3). The proportion of those with significant WR was compared across sub-groups.
Results
A total of 9617 patients were included. Median WR at 5 years was 14.1% of lost weight, 1.92 kg/m2, and 5 kg. Significant WR using definition 1 was 35.1%, 14.6%, and 3% after sleeve gastrectomy (SG), Roux-en-Y gastric bypass (RYGB), and mini-one anastomosis gastric bypass (OAGB) respectively. Severe albumin deficiency was highest in OAGB (5.9%) patients followed by SG (2.9%) and RYGB (2.2%) at 5 years(p = 0.023). Haemoglobin levels < 10 g/dL were seen in 8.2%, 9.0%, and 13.9% of SG, RYGB, and OAGB patients respectively (p = 0.041).
Conclusions
In the first comparative study of WR, OAGB had lesser WR in comparison to SG and RYGB but had the most impact on Hb and albumin levels in the long term. Definition selection for reporting WR has a significant impact on the results. There is a need for standardising the reporting of WR in bariatric literature.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery is now recognised to be the best treatment strategy for sustained weight loss. The data on medium and long-term outcomes is scarce with only very few studies reporting on ≥ 5-year results and most have relatively small numbers [1]. Studies that compare different bariatric procedures in the mid and long term are even fewer [2]. There are further very few studies [3,4,5,6,7] that have patients with ≥ 5-year outcomes after one anastomosis gastric bypass (OAGB), a relatively common procedure in India [8]. A recent review by the American Society for Metabolic and Bariatric Surgery [9] identified lack of 5-year outcomes a significant problem with published data on this procedure.
Most of the weight loss after bariatric surgery happens within the first year [10], and most patients experience some loss of clinical response in terms of weight loss and resolution of co-morbidities in the medium to long term. This loss of clinical response, often loosely labelled as weight regain (WR), is an Achilles’ heel of bariatric surgery and may lead to a patient seeking revisional bariatric procedures that are recognised to be riskier and less efficacious [11]. Despite this being such an important problem, there is no consensus on the definition of WR. Multiple definitions of WR have been used in the scientific literature further making any comparisons difficult [12].
It is also known that a proportion of patients undergoing bariatric surgery become anaemic and that certain procedures are associated with a higher risk of anaemia than the others [13]. Similarly, hypoalbuminaemia, often used as a surrogate of nutritional status of patients, is often associated with OAGB [14]. This makes understanding long-term weight loss, WR, anaemia rates, and albumin levels with different bariatric procedures a subject of significance.
The purpose of this study was to understand medium and long-term weight loss outcomes, WR, anaemia rates, and albumin deficiency with SG, RYGB, and OAGB in high-volume bariatric surgery centres in India.
Material and Methods
This retrospective study was part of a data collection exercise conducted by the Indian Bariatric Surgery Outcome Reporting Group. High-volume bariatric surgery centres in India were requested to share information on medium and long-term outcomes (weight loss, anaemia rates, and hypoalbuminaemia rates) after sleeve gastrectomy (SG), Roux-en-Y gastric bypass (RYGB), and one anastomosis gastric bypass (OAGB).
Surgeons reported a variation in the basic anatomical details of different procedures. For SG, the bougie sizes ranged between 34 and 38 Fr, and the distance from the pylorus ranged from 2 to 6 cm. For RYGB, the approximate pouch size ranged from 20 to 60 mL. The length of the biliopancreatic limb ranged from 50 to 125 cm and alimentary limb from 70 to 150 cm. When it came to OAGB, surgeons used a bougie size of 32–38 Fr for pouch construction and a biliopancreatic limb ranging from 150 to 210 cm.
Participating centres recommended 3–4 times follow-up in the first year, 1–2 times in the second year, and annually thereafter. Dietary advice was given at each follow-up either by a nutritionist or by the bariatric surgeon themselves. There was also a variation in nutritional supplementation recommendation amongst the centres. All OAGB and RYGB patients were recommended lifelong supplementation. Some (11/25) centres used specific bariatric multivitamins with or without additional iron and calcium supplements as needed. Others (14/25) used over the counter multivitamins along with iron and calcium supplements. Most (23/25) centres recommended lifelong multivitamin/mineral supplementation to sleeve patients. The recommendations varied from centre to centre in terms of the preparation.
Calculations
WR was calculated from the minimum recorded weight.
Percent WR was defined as (5 years recorded weight − minimum recorded weight) × 100/(preoperative weight − minimum recorded weight)
We have used three different definitions of significant WR to be able to compare our outcomes with the literature.
-
Definition 1:Regain of more than 25% of lost weight from the nadir weight [12, 15]
-
Definition 2:Regain of more than 10 kg from the nadir weight [16,17,18,19,20,21]
-
Definition 3:Regain of more than 5 BMI points from the nadir weight [12, 22]
Exclusions
Patients with less than 3-year data were excluded as the purpose of this study was to understand medium and long-term outcomes. We also excluded data on procedures other than SG, RYGB, and OAGB as this paper only focusses on outcomes with these three procedures commonly performed in India. Patients with missing data points were kept for the descriptive statistics and comparison of means but were excluded from the correlation/regression analysis.
Statistical Methods
Categorical variables are expressed as number of patients and percentage of patients and compared across the groups using Pearson’s chi-square test for independence of attributes/Fisher’s exact test as appropriate. Continuous variables are expressed as descriptive statistics and compared across groups using paired t test for parametric data and Mann-Whitney U test/Kruskal Wallis test for non-parametric data. Over time comparison has been done using Wilcoxon sign rank test. Association between continuous variables is captured using Spearman’s rank correlation coefficient. The statistical software SPSS version 20 has been used for the analysis. A p value of < 0.05 was considered significant.
Results
Basic Demographics
Twenty-six high-volume bariatric surgery centres with 32 bariatric surgeons (Table 1) shared their data for this exercise. A total of 9617 patients with minimum 3 years of follow-up (5458 (56.8%) SG, 2965 (30.8 %) RYGB, and 1194 (12.4 %) OAGB patients) were included in the final analysis. Follow-up data was available for 7937 (82.5%), 5282 (54.9%), 5781 (60.1%), and 3231 (33.5%) patients at 1, 2, 3, and 5 years respectively. Procedure wise breakdown and follow-up are given in Table 2.
Descriptive Statistics
Out of 9617 patients, 57.6% were females. The median age, preoperative weight, and BMI were 41 years (range, 6–92 years), 115 kg (64–320 kg), and 43 kg/m2 (27.5–131.5 kg/m2) respectively. Median preoperative haemoglobin and albumin levels were 12.7 g/dL (6.10–18.8 g/dL) and 3.98 mg/dL (1.3–7.3 mg/dL). Table 3 lists the basic demographics of patients broken down by procedures.
Weight Loss Outcomes
Table 4 provides and compares weight loss outcomes at different time intervals. Median %TWL at 3 years was 28.71, 29.99, and 33.33 respectively after SG, RYGB, and OAGB (p < 0.001). Median %EWL at 3 years was 68.78, 68.54, and 79.01 respectively (p < 0.001).
At 5 years, median %TWL after SG, RYGB, and OAGB was 24.05, 27.82, and 32.62 respectively (p < 0.001). Percentage EWL was 57.28, 60.85, and 70.37 respectively after SG, RYGB, and OAGB (p < 0.001).
Weight Regain
According to definitions 1, 2, and 3, the proportion of those with significant WR was 26.2% (847/3238), 20.6% (668/3240), and 11.3% (365/3231) in the whole cohort. Median WR at 5 years was 14.1% of lost weight, 1.92 kg/m2 BMI points, and 5 kg.
Table 5 presents WR data in the three groups and compares them. Median percent WR from the nadir weight after SG, RYGB, and OAGB was 18.6%, 10.67%, and 1.98% respectively (p < 0.001). Median absolute WR in kilogram was 6.0 kg, 4.0 kg, and 1.0 kg from the nadir weight respectively in SG, RYGB, and OAGB groups (p < 0.001). Median BMI regain from the nadir BMI was 2.34, 1.46, and 0.35 kg/m2 respectively. SG had significantly higher WR compare to RYGB and OAGB.
Percent of those with significant WR using definition 1 was 35.1%, 14.6%, and 3.0% after SG, RYGB, and OAGB respectively (p < 0.001). Using definition 2, the numbers were 27.3%, 11.8%, and 3% respectively (p < 0.001). Applying definition 3, percentage of those with significant WR in SG, RYGB, and OAGB patients was 15.9%, 5.0%, and 1.0% respectively (p < 0.001) (Table 5). Significantly, more patients regained a significant amount of weight in the SG group compared to the RYGB and OAGB group (p < 0.001).
Effect of Preoperative BMI on Weight Patterns
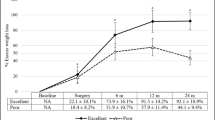
In the superobese group, OAGB had higher %TWL and %EWL than SG and RYGB at 3 and 5 years (Fig. 1).
The superobese group had significantly higher weight regain compared to those with BMI ≤ 50 kg/m2 according to definitions 2 (p ≤ 0.001) and 3 (p ≤ 0.001) but lower regain when definition 1 was applied (p ≤ 0.001) (Fig. 2).
Relationship of Haemoglobin and Albumin with BMI trends
Figures 3 and 4 show haemoglobin and albumin levels with different procedures at different time periods. Severe albumin deficiency (defined as < 3.0 g/dL) was highest in OAGB (5.9%) patients followed by SG (2.9%) and RYGB (2.2%) at 5 years (p = 0.023). Haemoglobin levels < 10 g/dL were seen in 8.2%, 9.0%, and 13.9% of SG, RYGB, and OAGB patients respectively (p = 0.043).
Discussion
This first multicentre data collaboration on bariatric surgery from India demonstrates weight loss outcomes up to 5 years after SG, RYGB, and OAGB.
SG accounted for the largest number of procedures in keeping with its global popularity [8]. Interestingly, OAGB accounted for 12.4% of the three most commonly performed procedures in this study compared to 1.8% worldwide [8]. This reflects the popularity of this procedure in India [23].
The age distribution of our cohort seems to follow the worldwide pattern with the 30–60-year age group being the commonest. The proportion of males in our study is a little higher (42.6%) than most series reported worldwide [24]. This may be attributed to the males being more economically productive and thus having an easier access to health care in the Indian population.
There seems to be a growing acceptance for adolescent bariatric and metabolic surgery in the country as reflected by the numbers in the cohort (136 patients under 18 years of age).
This study shows (Table 4) significant superior weight loss outcomes and less WR with OAGB compared to RYGB and SG, and with RYGB compared to SG. This is similar to findings of a randomised study by Zhang et al [25] where authors found 76.2% EWL with RYGB compared to 63.2% (p = 0.02) with SG. Another study by Salminent et al. [26, 27] found 57.0% EWL at 5 years with RYGB compared to 49.0% with SG even though the difference did not reach statistical significance in that study with much fewer numbers than ours.
Superior weight loss outcomes with gastric bypass may, at least in part, be explained by greater alteration in the neurohormonal milieu in diversionary procedure and may explain the durability of the results. In a paper by Peterli and others, a higher trend towards postprandial GLP-1 and PYY was seen although the difference did not reach statistical significance [28].
Our results for weight regain are similar to those reported in the literature who have applied definitions used by us [15,16,17,18, 21, 29,30,31]. Seven of these studies are on sleeve gastrectomy [15,16,17,18, 21, 29, 30], one on RYGB [31], and none on OAGB.
Although a small percentage of patients did not experience any WR, most patients exhibited some WR at 5 years. When analysed for procedure groups, the median regain was statistically significant for all three procedures examined in this study.
With each of the three definitions applied, SG has the highest WR followed by RYGB and OAGB. The apparent lower WR with OAGB may be due to comparatively fewer patients at the 5-year mark as reflected in the fact that 17.0% OAGB patients had the data for 5-year follow-up as opposed to 36.8% RYGB patients and 35.6% of SG patients. Our finding that SG patients had lowest TWL at 5 years and the higher tendency to WR has also been observed by others [25] though there is no study up to date in the scientific literature specifically examining and comparing WR with different procedures.
There was a higher variability in WR with SG patients compared to RYGB and OAGB. This means that despite higher WR than other procedures, there is a subset of SG patients who are doing remarkably well. We propose further studies to identify and define this subgroup. This will help us do a better procedure selection.
We further found that though Hb levels stabilised after some time in SG patients, levels continued to drop in those undergoing either type of bypasses. Anaemia is a recognised problem after bariatric surgery, and gastric bypass patients are known to be more likely to develop anaemia than those undergoing SG [13]. That is why standard recommendations for nutritional supplementation after bariatric surgery recognise a higher need for many micronutrients in gastric bypass patients [32]. These findings should, however, lead to evaluation of micronutrient supplementation recommendation guidelines for different procedures in India and the compliance with them.
Similarly, though albumin levels eventually stabilised in both SG and RYGB patients, they continued to drop in OAGB patients. Even more worryingly, severe albumin deficiency was seen in a large number of patients, and the number was highest with OAGB (5.9% in comparison with SG (2.9%) and RYGB (2.2%)). This must lead to the evaluation of nutritional support practises following surgery as well as a discussion on the most appropriate limb length for patients undergoing OAGB in India. Surprisingly, SG had more rates of severe albumin deficiency than RYGB. Although statistically significant, this may not be clinically significant. We are unable to explain the same. Prospective studies may be needed to study this properly.
Although we have used hypoalbuminemia as a surrogate for protein deficiency, this study does not evaluate the incidence of significant protein-calorie malnutrition, a recognised problem with OAGB [33] or the true burden of micronutrient deficiency, likely to be higher with a gastric bypass.
Because of variability in reporting WR, comparison and true estimation of the problem become difficult. A recently published paper by King and others [34] has tried to see the correlation of different definitions of WR with clinical outcomes. They found that percent of lost weight and applying the definition of significant regain as > 20% of maximum weight loss could be best associated with clinical outcomes except for hyperlipidaemia. In a paper published in 2017, Lauti and other selected 6 definitions for review [12]. They found comparable and consistent results with three of these definitions. We have selected those three definitions based on these findings and found strikingly different results.
Applying BMI > 5 kg/m2 points definition gives a lower number of significant regainers followed by definition 2 and definition 1 in our series. This may be because the median BMI in our cohort is lower than the other study [30].
Also, in the superobese group, patients are regaining more absolute weight but a lesser proportion of the lost weight compared to those with BMI ≤ 50 kg/m2. Therefore, in higher BMI group, WR is highest with definition 3 and lowest with definition 1. This brings up the question about which definition should be applied to measure weight regain. We propose that we should define weight regain differently for different BMI groups. We propose that we define significant weight regain in patients as a gain of BMI > 5 points (definition 3) for patients with preoperative BMI ≤ 50 kg/m2 and more than 25% of lost weight (definition 1) in patients with preoperative BMI > 50 kg/m2.
However, weight regain is an outcome where the cutoffs may not be entirely applicable. Patient’s perception and comorbidity resolution are important considerations that should be incorporated in the definition/scoring system for WR to be more meaningful.
There are several weaknesses of this study that need to be acknowledged. One of the biggest drawbacks of this study is that it is a retrospective comparison of a non-randomised cohort. Indeed, our data show significant baseline differences amongst the three groups. At the same time, this is a real-world data showing what patients can expect with different procedures in India in terms of weight loss and basic nutritional outcomes. Our follow-up of 60.1% and 33.5% at 3 and 5 years is poor, but follow-up is a recognised problem within bariatric literature and there are only a handful of studies in the literature with adequate follow-up of 80.0% or more [35]. Variation in techniques with different procedures also makes any comparison difficult, but in recent times, even randomised multicentre studies allow different centres to use their own techniques for different procedures [36]. Despite all these obvious limitations, this study does report on 5-year data on 3231/9617 patients. Given there is so little data on 5-year outcomes with bariatric surgery in general and from India in particular means the data in this study is clinically important for patients and practitioners of bariatric surgery in India and elsewhere.
Conclusion
This is the first report on medium and long-term outcomes with SG, RYGB, and OAGB in Indian patients. This is also the first scientific comparison of WR with these three procedures in medium to long term. SG patients have lower weight loss at 3 and 5 years in comparison to RYGB and OAGB, but at the same time, SG seems to have the least impact on Hb and albumin levels in the long term.
OAGB seems to result in the least weight regain but has the highest incidence of anaemia and severe hypoalbuminaemia. OAGB also seemed to deliver better weight loss outcomes in comparison to SG and RYGB in the superobese patients. Definition selection for reporting WR had a significant impact on the numbers obtained, and there is a need for standardising the reporting of WR in bariatric literature.
References
Juodeikis Ž, Brimas G. Long-term results after sleeve gastrectomy: a systematic review. Surg Obes Relat Dis. 2017;13:693–9.
Shoar S, Saber AA. Long-term and midterm outcomes of laparoscopic sleeve gastrectomy versus Roux-en-Y gastric bypass: a systematic review and meta-analysis of comparative studies. Surg Obes Relat Dis. 2017;13:170–80.
Rutledge R, Walsh TR. Continued excellent results with the mini-gastric bypass: six-year study in 2,410 patients. Obes Surg. 2005;15:1304–8.
Bruzzi M, Rau C, Voron T, et al. Single anastomosis or mini-gastric bypass: long-term results and quality of life after a 5-year follow-up. Surg Obes Relat Dis. 2015;11:321–6.
Alkhalifah N, Lee W-J, Hai TC, et al. 15-year experience of laparoscopic single anastomosis (mini-)gastric bypass: comparison with other bariatric procedures. Surg Endosc. 2018;32:3024–31.
Kular KS, Manchanda N, Rutledge R. A 6-year experience with 1,054 mini-gastric bypasses—first study from Indian subcontinent. Obes Surg. 2014;24:1430–5.
Jammu GS, Sharma R. A 7-year clinical audit of 1107 cases comparing sleeve gastrectomy, Roux-en-Y gastric bypass, and mini-gastric bypass, to determine an effective and safe bariatric and metabolic procedure. Obes Surg. 2016;26(5):926–32
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery and endoluminal procedures: IFSO Worldwide Survey 2014. Obes Surg. 2017;27:2279–89.
Parikh M, Eisenberg D, Johnson J, et al. American Society for Metabolic and Bariatric Surgery Clinical Issues Committee. American Society for Metabolic and Bariatric Surgery review of the literature on one-anastomosis gastric bypass. Surg Obes Relat Dis. 2018;14:1088–92.
Courcoulas AP, Christian NJ, Belle SH, et al. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA. 2013;310:2416–25.
Mahawar KK, Graham Y, Carr WRJ, et al. Revisional Roux-en-Y gastric bypass and sleeve gastrectomy: a systematic review of comparative outcomes with respective primary procedures. Obes Surg. 2015;25:1271–80.
Lauti M, Lemanu D, Zeng ISL, et al. Definition determines weight regain outcomes after sleeve gastrectomy. Surg Obes Relat Dis. 2017;13:1123–9.
Bailly L, Schiavo L, Sebastianelli L, Fabre R, Pradier C, Iannelli A. Anemia and bariatric surgery: results of a national French survey on administrative data of 306,298 consecutive patients between 2008 and 2016. Obes Surg. 2018;28(8):2313–20
Karimi M, Kabir A, Nejatifar M, et al. Trend of changes in serum albumin and its relation with sex, age, and BMI following laparoscopic mini-gastric bypass surgery in morbid obese cases. Obes Surg. 2018;28:671–80.
Liu SY-W, Wong SK-H, Lam CC-H, et al. Long-term results on weight loss and diabetes remission after laparoscopic sleeve gastrectomy for a morbidly obese Chinese population. Obes Surg. 2015;25:1901–8.
Abdallah E, El Nakeeb A, Yousef T, et al. Impact of extent of antral resection on surgical outcomes of sleeve gastrectomy for morbid obesity (a prospective randomized study). Obes Surg. 2014;24:1587–94.
Braghetto I, Csendes A, Lanzarini E, et al. Is laparoscopic sleeve gastrectomy an acceptable primary bariatric procedure in obese patients? early and 5-year postoperative results. Surg Laparosc Endosc Percutan Tech. 2012;22:479–86.
Casella G, Soricelli E, Giannotti D, et al. Long-term results after laparoscopic sleeve gastrectomy in a large monocentric series. Surg Obes Relat Dis. 2016;12:757–62.
Ritz P, Becouarn G, Douay O, et al. Gastric bypass is not associated with protein malnutrition in morbidly obese patients. Obes Surg. 2009;19:840–4.
Obeidat F, Shanti H, Mismar A, et al. The magnitude of antral resection in laparoscopic sleeve gastrectomy and its relationship to excess weight loss. Obes Surg. 2015;25:1928–32.
Bohdjalian A, Langer FB, Shakeri-Leidenmühler S, et al. Sleeve gastrectomy as sole and definitive bariatric procedure: 5-year results for weight loss and ghrelin. Obes Surg. 2010;20:535–40.
Brethauer SA, Aminian A, Romero-Talamás H, et al. Can diabetes be surgically cured? long-term metabolic effects of bariatric surgery in obese patients with type 2 diabetes mellitus. Ann Surg. 2013;258:1.
Mahawar KK, Kular KS, Parmar C, et al. Perioperative practices concerning one anastomosis (mini) gastric bypass: a survey of 210 surgeons. Obes Surg. 2018;28:204–11.
Young MT, Phelan MJ, Nguyen NT. A decade analysis of trends and outcomes of male vs female patients who underwent bariatric surgery. J Am Coll Surg. 2016;222:226–31.
Zhang Y, Zhao H, Cao Z, et al. A randomized clinical trial of laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy for the treatment of morbid obesity in China: a 5-year outcome. Obes Surg. 2014;24:1617–24.
Salminen P, Helmiö M, Ovaska J, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity. JAMA. 2018;319:241.
Alkhalifah N, Lee W-J, Hai TC, Ser K-H, Chen J-C, Wu C-C. 15-year experience of laparoscopic single anastomosis (mini-)gastric bypass: comparison with other bariatric procedures. Surg Endosc. 2018;32(7):3024–31
Peterli R, Steinert RE, Woelnerhanssen B, et al. Metabolic and hormonal changes after laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy: a randomized, Prospective Trial. Obes Surg. 2012;22:740–8.
Braghetto I, Cortes C, Herquiñigo D, et al. Evaluation of the radiological gastric capacity and evolution of the BMI 2-3 years after sleeve gastrectomy. Obes Surg. 2009;19:1262–9.
Lauti M, Kularatna M, Hill AG, et al. Weight regain following sleeve gastrectomy—a systematic review. Obes Surg. 2016;26:1326–34.
Cooper TC, Simmons EB, Webb K, et al. Trends in weight regain following Roux-en-Y gastric bypass (RYGB) bariatric surgery. Obes Surg. 2015;25:1474–81.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient-2013 update: cosponsored by American Association Of Clinical Endocrinologists, The Obesity Society, And American Society Fo. Obesity. 2013;21:S1–27.
Mahawar K, Parmar C, Carr WJ, et al. Impact of biliopancreatic limb length on severe protein–calorie malnutrition requiring revisional surgery after one anastomosis (mini) gastric bypass. J Minim Access Surg. 2018;14:37.
King WC, Hinerman AS, Belle SH, et al. Comparison of the performance of common measures of weight regain after bariatric surgery for association with clinical outcomes. JAMA. 2018;320:1560.
Puzziferri N, Roshek TB, Mayo HG, et al. Long-term follow-up after bariatric surgery. JAMA. 2014;312:934.
Blencowe NS, Brown JM, Cook JA, et al. Interventions in randomised controlled trials in surgery: issues to consider during trial design. Trials. 2015;16:392.
Acknowledgments
We are thankful to Dr. Aparna Govil Bhasker for the help in organising the study as well as guidance in writing the manuscript, Kankona Dey for the help in data compilation, Dr. Laila Baig for organising the consensus meeting, Manjari Agarwal for data compilation, and Mr. Souvik Dutta for statistical analysis.
Author information
Authors and Affiliations
Consortia
Contributions
SJB, KM, and SS conceived the idea for the topic. SJB initiated the research and wrote the manuscript. PP collected most of the data and wrote the manuscript. SJB and PP contributed equally to the manuscript. KM and SS wrote and edited parts of the manuscript. All authors participated in the discussions on the topic. All authors have seen the final version and approve of it.
Corresponding author
Ethics declarations
Conflict of Interest Statement
The authors declare that they have no conflict of interest.
Statement of Human and Animal Rights
Not applicable.
Statement of Informed Consent
For this type of study, formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
IBSOR Collaborators
Dr. Abhay Agarwal - Apollo Hospitals, Mumbai, India; Hinduja Hospitals, Mumbai, India; Sevenhills Hospitals, Mumbai, India
Dr. Arun Prasad - Manipal Hospitals, Dwarka, New Delhi, India
Dr. Atul Peters - Apollo Institute of Metabolic and Bariatric Surgery, New Delhi, India
Dr. Deep Goel - BLK Superspeciality Hospital, New Delhi, India
Dr. Digvijaysingh Bedi - Hope Obesity Centre, Ahmedabad, India
Dr. Jaydeep H. Palep - Nanavati Superspeciality Hospital, Mumbai, India
Dr. Lakshmi Kona Kumari - Gleneagles Global Hospital, Hyderabad
Dr. Mahendra Narwaria - Asian Bariatrics Pvt ltd, Ahmedabad, India
Dr. Manish Baijal - Max Superspeciality Hospital Saket, New Delhi, India
Dr. Manish Khaitan - Columbia Asia Hospital, Ahmedabad, India
Dr. Mathias Fobi - Mohak Bariatrics and Robotics, Indore, India
Dr. Mohit Bhandari - Mohak Bariatrics and Robotics, Indore, India
Dr. Nandkishore Dukipatti - Livlife Hospitals, Hyderabad, India
Dr. Nidhi Khandelwal - Nanavati Superspeciality Hospital, Mumbai, India
Dr. Om Tantia - ILS Hospitals, Kolkata
Dr. P. Pravin Raj - Gem Hospital and Research Centre, Coimbatore, India
Dr. Pallawi Priya - Belle Vue Clinic, Kolkata, India
Dr. Parveen Bhatia - Bhatia Global Hospital, Sir Ganga Ram Hospital, New Delhi, India
Dr. Pradeep Chowbey - Max Superspeciality Hospital Saket, New Delhi, India
Dr. Rajkumar Palaniappan - Apollo Hospitals, Chennai, India
Dr. Rajkumar JS - Lifeline Hospitals, Chennai, India
Dr. Rajesh Khullar - Max Superspeciality Hospital Saket, New Delhi, India
Dr. Ramen Goel - Wockhardt Hospital, Mumbai, India
Dr. Randeep Wadhawan - Fortis Hospitals, Vasan Kunj, New Delhi, India
Dr. Sarfaraz J. Baig - Belle Vue Clinic, Kolkata, India
Dr. Shivaram HV - Aster CMI Hospital, Bengaluru, India
Dr. Sreejoy Pattnaik - Shanti Memorial Hospital, Cuttack, India
Dr. Sudheer Kalhan - Sir Ganga Ram Hospital, New Delhi, India
Dr. Sumeet Shah - Max Smart Superspeciality Hospital, New Delhi, India
Dr. Surendra Ugale - Kirloskar Hospitals, Hyderabad, India
Dr. Vandana Soni - Max Superspeciality Hospital Saket, New Delhi, India
Dr. Vivek Bindal - Sir Ganga Ram Hospital, New Delhi, India
Rights and permissions
About this article
Cite this article
Baig, S.J., Priya, P., Mahawar, K.K. et al. Weight Regain After Bariatric Surgery—A Multicentre Study of 9617 Patients from Indian Bariatric Surgery Outcome Reporting Group. OBES SURG 29, 1583–1592 (2019). https://doi.org/10.1007/s11695-019-03734-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03734-6