Abstract
Background
The primary purpose of this study was to assess weight loss and occurrence of weight regain among patients who underwent Roux-en-Y gastric bypass (RYGB) using categorical analysis.
Methods
Study participants were selected from patients who underwent RYGB from a single institution. Participants (n = 300, mean procedure age = 45.6 ± 9.9) completed surveys for self-reported preoperative weight, current weight, and subsequent weights over postoperative years. Measured weights and confirmed procedure dates were acquired from patient medical records. Mean preoperative weight and BMI were 140.8 kg ± 32.1 and 49.7 ± 9.9, respectively, and mean years since surgery was 6.9 ± 4.9. Study subjects were mostly Caucasian (56.7 %) and female (80.3 %). Participants were stratified a priori into four cohorts based on percent of weight loss at 1 year, <25 % (n = 39), 25–30 % (n = 51), 30–35 % (n = 73), and >35 % (n = 113). General linear model analyses were conducted to assess the effect of year one weight loss on percent weight regain.
Results
The mean weight regain for all patients was 23.4 % of maximum weight loss. Using categorical analysis, mean weight regain in the <25, 25–30, 30–35, and >35 % weight loss cohorts was 29.1, 21.9, 20.9, and 23.8 %, respectively. Excessive weight regain, defined as ≥25 % of total lost weight, occurred in 37 % of patients.
Conclusion
Weight gain is a common complication following RYGB surgery. Despite the percentage of weight loss over the first year, all cohort patient groups regained on average between 21 and 29 % of lost weight. Excessive weight gain was experienced by over one third of patients. Greater initial absolute weight loss leads to more successful long-term weight outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction/Purpose
Bariatric surgery is the most effective treatment for patients with severe obesity for weight loss and reduction in comorbidities, although mean weight loss varies among the different procedure types [1, 2]. Recent data from the Longitudinal Assessment of Bariatric Surgery (LABS-2) study demonstrated that median percent weight loss for Roux-en-Y gastric bypass (RYGB) participants was 31.5 % of baseline weight at 3 years after surgery compared to 15.9 % for laparoscopic adjustable gastric banding (LAGB) patients [3]. However, other longer-term studies have demonstrated that weight regain occurs overtime depending upon the procedure performed and duration of time following surgery [4, 5]. For example, the Swedish Obese Subjects (SOS) study, the largest nonrandomized intervention trial comparing weight loss outcomes in a group of over 4000 surgical and nonsurgical subjects, has previously reported 10-year data [6]. Total body weight change was maximal after 1 year in the three surgical subgroups (RYGB, −38 ± 7 %; VBG, −26 ± 10 %; and banding, −21 ± 10 %). For the RYGB and banding subgroups, 10-year weight change was −25 ± 11 and −13.2 ± 13 %, respectively. Thus, at 10 years, subjects who underwent RYGB experienced a mean weight regain of 12 % total body weight and those who underwent fixed or variable banding regained 8 % total body weight. This translates into regaining 34 % (for RYGB) and 38 % (for banding) of the maximal lost weight at 1 year. Despite the occurrence of weight gain, there is no consensus as to what constitutes significant regain post-bariatric surgery [7].
Though the impact of weight regain following bariatric surgery is becoming apparent as a significant postoperative complication, most studies in the surgical literature have only reported mean weight values in their data analyses [8, 9]. This is in contrast to the nonsurgical literature where reporting categorical outcome data has become common practice. For example, lifestyle interventions [10, 11] and pharmacological treatment studies [12, 13] routinely report mean percent weight loss in addition to predefined 5 and 10 % categorical groups. The latter calculation provides additional information for the patient regarding the odds or likelihood of achieving a beneficial response. Additional outcome reporting may include cohort analysis, i.e., examining the trajectory patterns of weight loss and regain among predetermined groups of patients. This analysis allows determination of the effect of early weight loss on longer-term success. The use of predetermined weight trajectories and percentile charts has recently been employed in analyzing surgical weight loss outcomes as well [3, 14].
The primary purpose of this study was to assess weight loss and occurrence of weight regain among patients who underwent RYGB using categorical analysis and to determine whether initial weight loss predicts longer-term success among stratified cohorts of patients based on weight loss in the first postoperative year.
Materials and Methods
Participants and Procedures
Through a search of bariatric surgery medical records at Northwestern Memorial Hospital, the Northwestern Enterprise Data Warehouse (EDW) identified 705 patients who underwent RYGB between the dates of January 1, 1999, and June 30, 2009, and had postoperative follow-up of at least 2 years. A self-report questionnaire was created that asked potential participants to report demographic data along with current weight (i.e., weight at time of survey completion), preoperative weight, and subsequent weights over postoperative years 1 to 7. Participants were contacted by mail and asked to complete the survey online, by telephone or on paper. Participants who did not respond to the survey were sent two follow-up letters. One patient was initially excluded due to death since surgery. In total, 300 patients responded to the survey (43 %), and 404 subjects were lost to follow-up, including 132 return-to-senders and 272 nonresponders (Fig. 1). Informed consent was obtained from all individual participants included in the study through the Northwestern University Institutional Review Board (IRB).
Outcome Measures
Recorded (preoperative and yearly postoperative) weights and confirmed procedure dates were acquired from patient medical records via the Northwestern EDW, the electronic medical record (EMR), and paper chart review. Recorded weight was used as the primary measurement, but in cases where a measured weight was not available, participant self-reported weight was utilized. Significant correlations, from between 0.83 at 1 year postsurgery to 0.99 at 7 years postsurgery, were seen between recorded and self-report weights (p < 0.0001).
Data analysis of percent weight regain was first conducted on the total study population followed by specific analysis of predetermined cohorts. Percent weight regain was defined as the percentage of weight regained from the nadir weight, i.e., [100 (current weight − nadir weight)] / (preoperative weight − nadir weight). Of the 300 study participants, 295 were included in statistical analysis for overall percent weight regain based on having the following criteria available for analysis: recorded preoperative weight, lowest postoperative weight, and current weight.
Of the 295 participants included in the statistical analysis, 276 were further selected and stratified a priori into four predetermined cohorts based on weight loss during the first postoperative year: <25 % weight loss (n = 39, 14.1 %), 25–30 % weight loss (n = 51, 18.5 %), 30–35 % weight loss (n = 73, 26.4 %), and >35 % weight loss (n = 113, 40.9 %). Nineteen participants were excluded from stratification since they did not have a year 1 weight. We chose the lowest value of <25 % weight loss since successful weight loss is commonly defined in terms of achieving ≥50 % excess weight loss (EWL) [2], a value that is equivalent to 25 % total body weight loss for patients with a BMI of 45 to 50 kg/m2 [15]. Patients were further stratified into 5 % increments to capture cohorts who were losing less than mean weight losses as seen from the literature. We also noted whether subjects had “excessive weight regain” after surgery, defined as a percent weight regain ≥25 % from year 1 weight. As a secondary outcome, we preliminarily explored psychosocial items to assess the patients’ behavioral and mental health changes since surgery. Responses to these selected items were either collected as dichotomous (yes/no) variables or recorded using a Likert-type scale ranging from 1 to 5. Items of interest are listed in Table 1.
Statistical Analyses
Chi-squares and independent samples t tests were utilized to compare responders versus nonresponders by demographic characteristics. To assess the association of year one weight loss with percent weight regain, one-way ANOVA was initially conducted using Welch’s statistic to assess equality of means. Then, to assess the effect of other potential explanatory variables, estimates were obtained from general linear models which each included first-year weight loss cohort and one additional measure. These variables included demographic (gender, age, race/ethnicity, and marital status), physical activity (first year change in activity, days per week for routine exercise, and exercise session duration), dietary (postoperative change in diet, binge eating, control of portion size and food urges, emotional eating, and dumping syndrome), as well as preoperative and current smoking and drinking behaviors, preoperative BMI, time since surgery, and postoperative weight loss medication. For each potential explanatory variable, estimates were obtained from both a main effects model and from one in which the potential explanatory variable interacts with first-year weight loss cohort. Next, all potentially important explanatory variables (p < 0.20 from previous models) and significant interactions were included together with the first-year weight loss cohort in a single multivariable model and backward selection sequentially eliminated nonsignificant measures.
Results
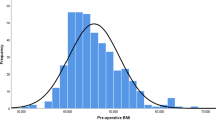
Of the 704 potential subjects, 300 individuals (43 %) responded to the request to complete the questionnaire (hereto referred to as “participants”). Participants were more likely to be female (p = 0.042) and were significantly fewer years postsurgery (p = 0.001) than nonresponders. There was no significant difference in race or procedure age between groups (Table 2). Participants ranged in age from 21 to 67 years old at the time of the surgery (mean 45.6 years ±9.9). The majority of the sample was female (80 %) and Caucasian (57 %). Participants also identified as Black/African-American (21 %), Latino/a (5 %), and other/multiracial (7 %). Race data was missing for 11 % of the participants. Mean preoperative body weight and BMI were 140.8 kg ± 32.1 and 49.7 kg/m2 ± 9.9, respectively, and mean years since surgery was 6.9 ± 2.3. Mean weight loss in the first postoperative year was 47.0 kg (22.4) or 33.1 % (9.6) of preoperative weight. Mean percent weight regain from nadir weight was 23.4 % ± 20.4 (Table 3, Fig. 2).
Percent weight regain over time between the four predefined cohorts is shown in Fig. 3. No significant differences were seen between the four groups (p = 0.371). However, on post hoc analysis, the largest difference was seen between patients who lost <25 % of their weight and patients who lost 30–35 % of their weight in the first postoperative year (p = 0.041) (Table 4). When we analyzed the total population of patients (n = 276), we found no overall difference between the four groups (p = 0.371), with mean percent regain of 23.4 %. If only self-reported weights are considered, no difference is evident between groups (p = 0.971), with mean percent regain of 21.6 % among 171 patients. And if only measured weights are considered, no difference is evident between groups (p = 0.281), with mean percent regain of 17.2 % among 154 patients. Thus, there appears to be a slight nonsignificant bias toward greater weight regain when self-reported weights are utilized.
Frequency distribution of percent weight regain by categorical analysis based on weight loss at 1 year. The four cohorts are <25, 25–30, 30–35, and >35 % total weight loss. Excessive weight regain, defined as >25 % of total weight loss, was seen in 38.5, 35.3, 32.9 and 38.1 % of participants in the four cohorts, respectively
Of the 295 patients included in the total population analysis, 109 (36.9 %) were found to have excessive weight regain, defined as ≥25 % gain from postoperative year 1. In cohort analysis, 38.5, 35.3, 32.9, and 38.1 % of participants regained excessive weight in the <25 % weight loss group, 25–30 % weight loss group, 30–35 % weight loss group, and >35 % weight loss group, respectively.
Of the potential explanatory variables (Table 5), age at surgery, preoperative BMI, time since surgery, first-year change in physical activity, days per week of routine exercise, exercise session duration, postoperative medication use causing weight gain, change in diet, binge eating, portion size control, control of food urges, emotional eating, and inability to stop or control intake met the α = 0.20 criteria as candidate variables. Only an interaction between food urge control and first-year weight loss cohort was evident (p = 0.042). After backward selection, variables remaining with weight loss cohort (p = 0.241) in the model for percent weight regain included preoperative BMI (p < 0.001), time since surgery (p < 0.001), first-year change in physical activity (p = 0.013), portion size control (p < 0.001), control of food urges (p = 0.001), and emotional eating (p = 0.003). Additional univariate ANOVAs were conducted to examine the differences in percent of weight regain between participants based on their responses to the following exploratory psychosocial items: supportiveness of their support system (p < 0.0001), depression (p = 0.040), and stress (p = 0.08).
Discussion
There are two primary findings of our study that have important patient care implications. The first is that weight regain is a common occurrence following RYGB. Our study population experienced a mean weight loss of 39.3 % of preoperative body weight and a mean percent weight regain of 23.4 % over an average of 6.9 postoperative years, with 36.9 % of participants experiencing excessive weight regain (≥25 % weight gain from nadir). Our results are comparable with those found in the literature for average percent weight regain over time, though the range of weight regain in these studies varies widely [4–6, 16]. The second major finding is that percentage of weight lost in the first postoperative year was not significantly associated with percent weight regain postoperatively. All four weight loss cohorts regained between 21 and 29 % of lost weight. However, losing more weight in the first postoperative year is predictive of better long-term absolute weight loss outcomes. That is, participants who lost more weight in the first year postsurgery had a greater absolute weight loss over time. This observation has important implications regarding early postoperative management to maximize patient weight loss outcomes and addressing patient expectations. Ritz et al. came to a similar conclusion after identifying patients who lost <30 % excess weight over the first six postoperative months [17]. Better long-term retention of weight loss following greater initial weight loss has been observed in nonsurgical treatments [18–21].
Presentation of outcome data using categorical analysis is often more meaningful for patient care than mean weight loss, allowing assessment of long-term response rates, improvement in comorbidities, and associated predictive variables. In the Look AHEAD study, categorical weight loss at year one was found to be predictive of weight loss and metabolic health outcomes at 4 and 8 years [20–22]. Categorical weight loss has also been used to explore behavioral associated contributors of success, e.g., treatment attendance, self-reported physical activity, and caloric intake predict greater success [23]. Analysis of clinical data and responses to our set of psychosocial and behavioral questions yielded significant correlations between percentage of weight regain after year 1 and self-rated level of change in physical activity, portion size control, control of food urges, and emotional eating. Two predictive clinical variables were preoperative BMI and time since surgery. Furthermore, there was a statistically significant difference in weight regain among patients who experienced depression. Although deemed exploratory, these secondary outcomes reaffirm the significance of psychosocial and behavioral factors in weight regain among bariatric surgery patients. Other studies have confirmed the importance of these factors in predicting weight regain [24–27].
Limitations
There are several limitations of our study that warrant comment. We used self-reported weights for our data analysis when a measured weight was not available. Although the difference between the two weights was highly correlated, it may represent an underreporting bias. We did not see a statistical difference between groups when we analyzed subcohorts with measured versus self-reported body weights which add validity to our study. Recent data from the LABS-2 study found that average degree of underreporting by self-report versus recorded clinical weight was only 0.7 kg for women and 1.0 kg for men [3]. Our response rate was 43 %. Although participants did not differ from nonresponders by age or race, average postoperative years were statistically shorter in participants (6.9 years) compared to nonresponders (9.2 years) and they were more likely to be female. We were unable to compare groups based on preoperative BMI. Over the period of this observational study, the Roux limb increased in length from 75–100 to 125–150 cm. It is possible that a difference in technique could account for some of the weight regain outcomes; however, this was not a variable that was directly analyzed. Lastly, we did not use validated questionnaires for assessing the effect of behavioral and psychosocial factors on percent weight regain. Thus, the results from these questions should only be viewed as exploratory data.
In conclusion, weight gain is a common complication of RYGB surgery, with over 1/3 of patients regaining excessive weight, defined as ≥25 % of total lost weight. Despite the percentage of weight loss over the first year, all cohort groups of patients regained a mean of 21 to 29 % of lost weight (average 23.4 %). However, greater initial absolute weight loss leads to more successful long-term weight outcomes. Weight regain was associated with specific psychosocial and behaviorals factors that need further exploration. Analyzing outcome data using categorical weight loss and stratified groups may allow greater targeting of patients who may benefit from earlier recognition and treatment.
References
Puzziferri N, Nakonezny PA, Livingston EH, et al. Variation of weight loss following gastric bypass and gastric band. Ann Surg. 2008;248(2):233–42.
Benoit SC, Hunter TD, Francis DM, et al. Use of bariatric outcomes longitudinal database (BOLD) to study variability in patient success after bariatric surgery. Obes Surg. 2014;24:936–43.
Courcoulas AP, Christian NJ, Belle SH, Longitudinal Assessment of Bariatric Surgery (LABS) Consortium, et al. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA. 2013;310(22):2416–25.
Christou NV, Look D, MacLean LD. Weight gain after short- and long-limb gastric bypass in patients followed for longer than 10 years. Ann Surg. 2006;244(5):734–40.
Shah M, Simha V, Garg A. Review: long-term impact of bariatric surgery on body weight, comorbidities, and nutritional status. J Clin Endocrinol Metab. 2006;91(11):4223–31.
Sjöström L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–93.
Karmali S, Brar R, Shi X, et al. Weight recidivism post-bariatric surgery: a systematic review. Obes Surg. 2013;23:1922–33.
Puzziferri N, Rosheck TB, Gallegher R, et al. Long-term follow up after bariatric surgery. A systematic review. JAMA. 2014;312:934–42.
Chang SH, Stoll CRT, Song J, et al. The effectiveness and risks of bariatric surgery. An updated systematic review and meta-analysis, 2003-2012. JAMA Surg. 2014;149:275–87.
Jebb SA, Ahern AL, Olson AD, et al. Caterson ID. Primary care referral to a commercial provider for weight loss treatment versus standard care: a randomized controlled trial. Lancet. 2011;378:1485–92.
Wadden TA, Volger S, Sarwer DB, et al. A two-year randomized trial of obesity treatment in primary care practice. N Engl J Med. 2011;365:1969–79.
Smith SR, Weissman NJ, Anderson CM, et al. Multicenter, placebo-controlled trial of lorcaserin for weight management. N Engl J Med. 2010;363:245–56.
Gadde KM, Ryan DH, Peterson CA, et al. Effects of low-dose, controlled-release, phentermine plus topiramate combination on weight and associated comorbidities in overweight and obese adults (CONQUER): a randomized, placebo-controlled, phase 3 trial. Lancet. 2011;377:1341–52.
Van de Laar AWJM, Acherman YIZ. Weight loss percentile charts of large representative series: a benchmark defining sufficient weight loss challenging current criteria for success of bariatric surgery. Obes Surg. 2014;24:727–34.
Bray GA, Bouchard C, Church TS, et al. Is it time to change the way we report and discuss weight loss? Obesity. 2009;17(4):619–21.
Magro DO, Geloneze B, Delfini R, et al. Long-term weight regain after gastric bypass: a 5-year prospective study. Obes Surg. 2008;18:648–51.
Ritz P, Caiazzo R, Becouarn G, et al. Early prediction of failure to lose weight after obesity surgery. Surg Obes Relat Dis. 2013;9:118–22.
Astrup A, Rossner S. Lessons from obesity management programmes: greater initial weight loss improves long-term maintenance. Obes Rev. 2000;1:17–9.
Barte JCM, ter Bogt NCW, Bogers RP, et al. Maintenance of weight loss after lifestyle interventions for overweight and obesity, a systematic review. Obes Rev. 2010;11:899–906.
Neiberg RH, Wing RR, Bray GA, et al. Patterns of weight change associated with long-term weight change and cardiovascular disease risk factors in the Look AHEAD study. Obesity. 2012;20(10):2048–56.
Unick JL, Hogan PE, Neiberg RH, et al. Evaluation of early weight loss thresholds for identifying nonresponders to an intensive lifestyle intervention. Obesity. 2014;22(7):1608–16.
Wadden TA, Neiberg RH, Wing RR, et al. Four-year weight losses in the Look AHEAD study: factors associated with long-term success. Obesity. 2011;19(10):1987–98.
The Look AHEAD Research Group. Eight-year losses with an intensive lifestyle intervention: the look AHEAD study. Obesity. 2014;22(1):5–13.
Kofman MD, Lent MR, Swencionis C. Maladpative eating patterns, quality of life, and weight outcomes following gastric bypass: results of an internet survey. Obesity. 2010;18(10):1938–43.
Odom J, Zalesin KC, Washington TL, et al. Behavioral predictors of weight regain after bariatric surgery. Obes Surg. 2010;20:349–56.
Livhits M, Mercado C, Yermilov I, et al. Behavioral factors associated with successful weight loss after gastric bypass. Am Surg. 2010;76(10):1139–42.
Colles SL, Dixon JB, O’Brien PE. Grazing and loss of control related to eating: two high risk factors following bariatric surgery. Obesity. 2008;16(3):615–22.
Acknowledgments
Northwestern Medicine
Enterprise Data Warehouse (EDW)
Center for Lifestyle Medicine
Department of Surgery
Department of Medical Social Sciences
Chris Mitchell, EDW
Conflict of Interest
The authors declare that they have no conflict of interest.
Disclosure Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cooper, T.C., Simmons, E.B., Webb, K. et al. Trends in Weight Regain Following Roux-en-Y Gastric Bypass (RYGB) Bariatric Surgery. OBES SURG 25, 1474–1481 (2015). https://doi.org/10.1007/s11695-014-1560-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1560-z