Abstract
Background
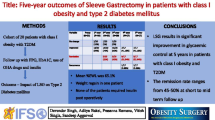
Laparoscopic sleeve gastrectomy (LSG) is an effective stand-alone bariatric procedure with favorable short-term results on weight reduction and comorbidity resolution. This study aims to evaluate the long-term results of LSG to see if weight reduction and diabetic improvement are sustainable.
Methods
We conducted a prospective observational study on patients receiving LSG as an index stand-alone bariatric operation in our unit.
Results
Between 2006 and 2014, there were 140 patients (91 females) aged 37.9 ± 10.5 years with a body mass index of 41.0 ± 7.0 kg/m2. At 1-year (n = 123), 2-year (n = 99), 3-year (n = 77), 4-year (n = 52), and 5-year (n = 44) follow-ups, the mean percentages of excess weight loss (%EWL) were 70.5, 65.2, 60.2, 53.2, and 57.2 %, respectively, while the corresponding proportions with failed weight loss (%EWL <30 %) were 7.3, 9.1, 13.0, 25.0, and 22.7 %. Weight regain (>25 % rebound in %EWL) was evident with time as 0, 1.0, 11.6, 19.2, and 29.5 % in the first 5-year follow-ups. In 65 patients with type 2 diabetes mellitus, remission (complete and partial) was achieved in 34.5 % at 1-year, 52.7 % at 3-year, and 70.6 % at 5-year follow-ups. Proportions of patients having optimal glycemic control (HbA1c <7 %) increased significantly from 26.2 % preoperatively to 80.9 % at the first year and maintained at 78.6 % at the fifth year (P < 0.001).
Conclusions
LSG was effective in achieving substantial weight reduction and improved diabetic control for morbidly obese patients. Although weight regain was possible with time, majority of patients could maintain sustainable weight loss, diabetes remission, and glycemic improvement in the long run.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic sleeve gastrectomy (LSG) is a restrictive bariatric procedure that works by reducing the gastric reservoir volume to limit food intake and induce satiety. The effect of surgical weight loss can also be attributed to the reduction of ghrelin production after the resection of ghrelin-producing cells in the gastric fundus and the upregulation of incretin hormone secretion by LSG [1–3]. With these combined restrictive and hormone modulation effects, LSG has been shown to be an effective stand-alone bariatric operation with favorable short-term results on weight reduction and comorbidity resolution [4]. To date, there was only a limited number of studies reporting the long-term results of LSG in the literature [4–10]. It remains unclear if LSG can produce sustainable weight loss and comorbidity improvement in long-term follow-up.
Type 2 diabetes mellitus (T2DM) is a global epidemic that is closely related to obesity. Bariatric surgery has been proven to be more effective than nonsurgical therapies for weight loss and glycemic control in diabetic patients [11–14]. Systematic reviews on short-term follow-up data suggested that diabetic patients experienced a high T2DM resolution rate of over 60 % after LSG [15]. However, the impact of LSG on long-term diabetic control still remains undefined. It is unclear if this high remission rate can be sustained and if recurrent T2DM may occur in longer-term follow-up.
The objective of this study was to evaluate the long-term results of LSG on weight control and T2DM improvement to see if these effects were sustainable in the long run.
Materials and Methods
Patients
This was a prospective observational study on consecutive patients who received LSG as a stand-alone bariatric operation in the Prince of Wales Hospital. We performed LSG since 2006 to treat obese patients who met the eligibility criteria for bariatric surgery according to the Asia-Pacific Bariatric Surgery Group consensus guidelines 2005 [16]. After 2012, we changed the eligibility criteria by following the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO)—Asian Pacific Chapter consensus statement 2011 [17]. Patients with a body mass index (BMI) greater than 35 kg/m2 regardless of the existence of comorbidities or BMI greater than 30 kg/m2 and having inadequately controlled T2DM or metabolic syndrome were included for LSG. We excluded patients who received LSG as a revisional procedure from other types of bariatric surgery. The study protocol was approved by our institutional research ethics committee. Informed consent was obtained from all patients included in this study.
Operative Technique
Our operative technique was previously described [18]. The entire greater curve was first taken down starting from 6 cm proximal to the pylorus up to the angle of His until the left diaphragmatic crus was exposed. With an orogastric bougie inserted for size calibration, a gastric sleeve was created from the antrum to the angle of His using sequential firings of laparoscopic linear staplers. All LSG procedures were performed by one of the three bariatric surgeons in our unit. The decision on bougie size and staple line reinforcement was chosen upon surgeons’ discretion.
Follow-up
All LSG patients were prospectively followed up at 1-month, half-year, 1-year, 1.5-year, 2-year, and then annually in an outpatient basis. Measurements of body weight, BMI, percentage of body fat (%fat), and waist circumference (WC) were conducted, and these results were collected in our prospective bariatric surgery database. For patients who did not turn up for follow-up assessments, telephone contacts were conducted individually to locate them. After getting the patients’ consent, medical records of these patients from their own healthcare providers or other hospitals were retrieved to review their body weight, body composition parameters, and other obesity-related comorbidity status at different follow-up time points. The relevant data were then entered into our bariatric surgery database. For patients with T2DM, the fasting blood glucose (FBG) and glycosylated hemoglobin (HbA1c) levels were measured at each follow-up. Since January 2010, fasting insulin and fasting C-peptide levels were also measured in T2DM patients at 6 weeks, 6 months, and 1 year after LSG.
Outcome Measures
The percentage of excess weight loss (%EWL) was used to represent the extent of weight reduction, and it was estimated using a BMI value of 25 kg/m2 as the ideal body weight. Successful weight loss was defined as having %EWL greater than 50 %, and failed weight loss was defined as having %EWL less than 30 %. Alternatively, the proportions of patients successfully reverting to the nonobese category after LSG (BMI <30 kg/m2) were evaluated. During follow-up assessment, rebound in body weight was also estimated. The percentage of rebound in excess weight loss (%REWL) was calculated as the percentage difference between the %EWL measured and the best %EWL achieved during postoperative follow-up. %REWL was zero if the best %EWL was not yet reached. Weight regain (WR) was defined as positive if %REWL was greater than 25 %. In addition, the proportions of patients having BMI rebound to 35 kg/m2 or above were also estimated.
For patients with T2DM, the changes in HbA1c levels and the T2DM remission rates during follow-up were used as outcome measures. Type 2 diabetes mellitus was defined using the World Health Organization 1999 diagnostic criteria (FBG ≥7.0 mmol/L or 2-h postprandial plasma glucose ≥11.1 mmol/L) [19]. The glycemic control was defined as optimal if the HbA1c level was less than 7 %. Remission of T2DM was defined using the American Diabetes Association 2009 criteria [20]. Complete remission was defined as a FBG of <5.6 mmol/L and HbA1c of <6.5 % for at least 1 year without using active pharmacologic therapy. Partial remission was defined as FBG of 5.6–6.9 mmol/L and HbA1c of <6.5 % for at least 1 year without using active pharmacologic therapy.
Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics® version 22 (IBM, New York, USA). Continuous variables were presented as mean and standard deviation while nominal and categorical data were reported as count and percentage. Parametric data was compared using t test while data changes over the follow-up period were compared using ANOVA test. Differences between nonparametric outcomes were analyzed using chi-square test and Mann-Whitney U test where appropriate. A P value of <0.05 was regarded as significant.
Results
Between May 2006 and June 2014, 140 patients (49 males and 91 females) underwent laparoscopic sleeve gastrectomy as a stand-alone operation in our unit. The mean preoperative body weight and BMI were 112.3 ± 20.0 kg and 41.0 ± 7.0 kg/m2, respectively. The mean waist circumference was 124.4 ± 14.1 cm. Majority of them (131 patients, 93.6 %) had obesity-related comorbidities including dyslipidemia (n = 48), hypertension (n = 75), obstructive sleep apnea (n = 75), osteoarthritis (n = 70), and gastroesophageal reflux disease (n = 20). Sixty-five patients (46.4 %) were suffering from T2DM at presentation while metabolic syndrome was present in 94 patients (67.1 %).
Perioperative Data
All sleeve gastrectomy procedures were performed by the laparoscopic approach. There was no conversion to open procedure. The mean operating time was 134.8 ± 45.9 min. Orogastric bougie was used in all patients, with 82 patients (58.6 %) having a bougie size below 40Fr and 58 patients (41.4 %) having a bougie size of 40Fr or above. The median hospital stay was five (2–39) days. There was no operative mortality. Early major morbidities occurred in five patients (3.6 %). There were two early staple line leakages (1.4 %) at postoperative days 5 and 14. One of them was treated with endoscopic clipping while the other was managed successfully with the insertion of self-expandable metal stent. There were three patients (2.1 %) suffering from postoperative bleeding and were all treated with conservative measures. For late morbidities, sleeve stricture was evident in five patients (3.6 %). All were managed with endoscopic balloon dilatation, but two patients required operative revision to laparoscopic Roux-en-Y gastric bypass. One patient (0.7 %) developed proximal pouch dilatation and was treated with laparoscopic pouch resection.
Weight Control
The mean follow-up duration was 37.8 ± 26.3 months. At 1, 2, 3, 4, and 5 years, a total of 123, 99, 77, 52, and 44 patients completed follow-up, and the respective lost-to-follow-up rates were 6.1, 8.3, 13.4, 20.0, and 15.3 %. The mean %EWL was 70.5 % at 1 year, 65.2 % at 2 years, 60.2 % at 3 years, 53.2 % at 4 years, and 57.2 % at 5 years (Table 1). The proportions of patients having successful weight loss (%EWL >50 %) were 79.7, 71.7, 58.4, 55.8, and 54.5 % from 1 to 5 years respectively while the corresponding proportions of patients having failed weight loss (%EWL <30 %) were 7.3, 9.1, 13.0, 25.0, and 22.7 % (Fig. 1). At 1, 2, 3, 4, and 5 years, the proportions of patients successfully reverting to the nonobese category (BMI <30 kg/m2) were 51.2, 47.5, 40.2, 28.8, and 34.1 %, respectively (Table 1).
Weight Regain
During the postoperative period, the best %EWL was estimated and rebound in %EWL was assessed. Similar to the trend of drop in %EWL over time, rebound in %EWL also increased progressively during follow-up (Fig. 2). The overall mean %REWL were 0.7 % at 1-year, 4.9 % at 2-year, 11.0 % at 3-year, 17.4 % at 4-year, and 18.9 % at 5-year follow-ups (Table 1). Weight regain (defined as %REWL >25 %) was not evident in the first year but was present in 1.0 % at 2 years, 11.6 % at 3 years, 19.2 % at 4 years, and 29.5 % at 5 years (Fig. 1). The proportions of patients having BMI rebound to ≥35 kg/m2 were 0.8 % at 1 year, 8.1 % at 2 years, 10.4 % at 3 years, 13.4 % at 4 years, and 9.1 % at 5 years (Table 1).
Revisional Surgery
During postoperative follow-up, eight patients (5.7 %) received revisional laparoscopic Roux-en-Y gastric bypass from LSG, one for intractable gastroesophageal reflux symptoms, two for sleeve stricture, and five for poor weight control. In the latter five patients, four had failed weight loss with their mean %EWL of only 24.6 % prior to revision. One patient received revision because of weight regain from %EWL >50 % to %EWL <30 %, and his %REWL prior to revision was 25.4 %. There was no revision to other types of bariatric surgery in this cohort.
Type 2 Diabetes Mellitus and Glycemic Control
Sixty-five patients (24 males and 41 females) with a mean age of 40.9 ± 10.0 years had T2DM for a median duration of 4.5 years (range 1–32 years) before LSG. The mean body weight and BMI were 110.2 ± 20.8 kg and 40.6 ± 6.2 kg/m2, respectively. Their mean preoperative HbA1c was 8.2 ± 1.8 %, and only 17 (26.2 %) of them were under optimal glycemic control (HbA1c <7 %). A total of 21 patients (32.3 %) were using insulin therapy while 44.6 % (n = 29), 23.1 % (n = 15), and 16.9 % (n = 11) of the patients were using one, two, and three or more oral anti-diabetes agents (OADs), respectively. Preoperative fasting C-peptide was measured in 42 patients (64.6 %). Their mean fasting C-peptide level was 3.4 ± 2.0 ng/ml, and 57.1 % of them had a fasting C-peptide level <3 ng/ml.
The mean follow-up duration was 31.2 ± 24.4 months. During 1-year, 2-year, 3-year, 4-year, and 5-year follow-ups, there were 55 patients (98.2 %), 45 patients (93.8 %), 36 patients (92.3 %), 23 patients (92.0 %), and 17 patients (89.5 %) completed follow-up, respectively. The mean HbA1c levels dropped significantly from 8.2 ± 1.8 % preoperatively to 6.3 ± 0.8 % (P < 0.001) over the 5 years (Table 2). The proportions of patients with optimal glycemic control (HbA1c <7 %) increased significantly from 26.2 % preoperatively to 80.9, 76.7, 74.2, 68.8, and 78.6 % at each successive follow-up year (P < 0.001). At 1 year, the overall T2DM remission (complete and partial) was achieved in 34.5 % of patients. This figure rose to 53.3 % at 2 years and maintained at 52.7 % at 3 years, 60.9 % at 4 years, and 70.6 % at 5 years. At the last follow-up (mean duration 31.2 ± 24.4 months), the proportion of patients with optimal glycemic control increased from 26.2 to 78.9 % (P < 0.001). The overall T2DM remission rate was 55.4 % (50.8 % complete remission and 4.6 % partial remission), and 14 patients (66.7 %) stopped using supplemental insulin therapy.
In patients who had previously achieved T2DM remission, two patients (3.1 %) developed recurrent T2DM during follow-up. There was no recurrent T2DM at 2 and 4 years, but one respective patient (one male and one female) developed recurrent T2DM at 3 and 5 years. Both of them did not require insulin therapy. One was treated by an OAD while the other was managed with diet control. Weight regain was not evident in both patients throughout the follow-up period.
Other Comorbidity Improvements
In a mean follow-up of 37.8 ± 26.3 months, 60 (63.8 %) out of 94 patients had metabolic syndromes resolved. Improvement in disease control was observed for dyslipidemia in 45.8 %, hypertension in 49.3 %, obstructive sleep apnea in 70.0 %, and osteoarthritis in 40.0 % of patients.
Discussion
LSG was initially developed as a bridging procedure to the duodenal switch for super obese high-risk patients. Short-term results from various studies demonstrated that LSG was a technically less complex stand-alone bariatric operation with a safer complication profile and lower mortality [21]. We had previously reported the early results of our first 29 LSG patients as combined data with another collaborative hospital and showed that the early %EWL achieved was up to 63.5 % at 1 year [18]. In the current study, we had conducted a long-term observational analysis on our own patients. Results from the present study suggested that LSG was effective in achieving substantial weight reduction over short-term, medium-term, and long-term follow-ups. Although weight rebound was evident with time, the mean %REWL remained acceptably low at medium- and long-term assessment. Majority of patients did not have remarkable weight regain in medium follow-up, but weight regain was observed in about 30 % of patients in long-term follow-up. Apart from weight control, our results also showed that T2DM remission was sustainable in medium- and long-term assessment. The proportions of patients with optimal glycemic control (HbA1c < 7 %) maintained almost well above 70 % throughout the postoperative period after LSG.
Our data supported the role of LSG in achieving substantial weight reduction as a stand-alone bariatric operation for morbid obesity. In this study, a high mean %EWL was achieved as early as 1 year and then maintained well above 50 % throughout the postoperative period. The vast majority of published data on LSG concluded its merits in achieving promising weight reduction in terms of %EWL at short-term follow-up. As for long-term follow-up data, a recent systematic review on 492 patients by Diamantis et al. found a 5-year mean %EWL of 62.3 % [22]. Earlier studies from the western population by Bohjiadian et al. [5], Sarela et al. [6], and Rawlins et al. [7] revealed that the %EWL was 57–73 % at early- (1 year), 60–77 % at medium- (3 years), and 55–81 % at long-term (≥4 years) follow-ups. In this study representing the Chinese population, the %EWL was 70.5 % at early- (1 year), 60.2 % at medium- (3 years), and 57.2 % at long-term (5 years) follow-up. Despite the difference in ethnic origin, the %EWL achieved by Chinese patients after LSG were largely similar to that of the western population.
With regard to the trend of postoperative %EWL change, our data suggested a slow progressive drop in %EWL and a similar trend of increasing %REWL over time. Results from literature publications about the change in %EWL were heterogeneous. While Bohjiadian and Sarela reported a peak %EWL at 3 years [5, 6], Rawlins demonstrated an unusual rising trend of %EWL with time that reached a peak at 4 years [7]. As for the present study analyzing 140 patients, the best %EWL was achieved at early follow-up at 1 year as 70.5 %. It dropped gradually to 60.2 % at 3 years but maintained at 57.2 % at 5 years. These findings were similar to a recent Chinese study by Zachariah et al. who reported the dropping trend of %EWL of 72.3 % at 1 year, 71.9 % at 3 years, and 63.7 % at 5 years [9]. In the survey on LSG at the Fourth International Consensus Summit on Sleeve Gastrectomy 2012, the %EWL at 1, 3, and 5 years were lower at 59.3, 54.7, and 52.4 %, respectively [23]. Our results on %EWL similarly demonstrated a progressively falling trend over time. Such declining results of %EWL implied the tendency of weight regain with time after LSG.
Bariatric surgery was traditionally believed to be effective in achieving sustainable weight reduction. Our results showed that weight rebound after LSG was evident with time but the mean %REWL was well below 20 % throughout the five postoperative years. Looking at the %REWL, our patients were regaining only 11.0 % at 3 years and 18.9 % at 5 years. Only 9.1 % of patients were having BMI rebound to ≥35 kg/m2 by 5 years after LSG. The proportions of patients achieving successful weight loss (%EWL >50 %) were 79.7 % at short-term, 58.4 % at medium-term, and still 54.5 % at long-term follow-ups. The proportions of patients with failed weight loss (%EWL <30 %) were low at 13.0 and 22.7 % at respective medium- and long-term follow-ups. By 5 years after LSG, 29.5 % of patients developed weight regain (%REWL >25 %). These results reflected that regain in body weight and fall in %EWL were possible after LSG in long-term follow-up. Although majority of patients could achieve sustainable weight loss, remarkable rebound in %EWL (%REWL >25 %) was present in about 30 % of patients.
There were several postulations for weight regain. First, weight regain might be attributed to anatomical factors. As the size of the gastric sleeve was directly related to the extent of weight loss, sleeve dilatation after LSG might potentially account for gradual weight regain. Secondly, a previous study by Bohdjalian et al. suggested the importance of hormonal factors in weight regain and showed that the plasma ghrelin levels were higher in weight regain patients as compared to those who experienced appropriate weight loss or maintenance after LSG [5]. Besides, a recent systematic review by Karmali et al. also reported the factors of dietary noncompliance, physical inactivity, and mental health disorders as potential causes of weight regain [24].
In the literature, results on T2DM remission after LSG were variable. In a systematic review of 673 patients receiving LSG, the short-term T2DM remission rate was 66.2 % at 13 months [15]. However, the long-term diabetic control after LSG was yet to be elucidated because of the lack of long-term follow-up data. Zachariah et al. reported a T2DM resolution rate of 86 % at 1 year, 71 % at 3 years, and 66 % at 5 years while Sieber et al. and Rawlins et al. both stated a considerably higher T2DM remission rate at 5 years (85 and 100 %, respectively) [7–9]. However, the definitions of T2DM remission were not well stated in these reports and were believed to be heterogeneous and arbitrary. In this study, we adopted the stringent American Diabetic Association criteria to define T2DM remission using FBG values, HbA1c levels, and medication profiles. We believed our results were a good reflection of T2DM remission rates in Chinese population. In addition, the postoperative T2DM remission rate was largely affected by the duration and severity of preoperative T2DM status. It was presumable that patient cohorts from different studies were different and so a direct comparison of the T2DM remission rates among different studies was deemed impossible.
Compared to the literature results on T2DM remission, our data revealed more stable T2DM remission rates throughout the postoperative follow-up period. Despite the progressive drop in mean %EWL and the increase in %REWL, the overall T2DM remission (complete and partial) rates were maintained at 52.7–70.6 % from medium- to long-term follow-ups. Regardless of the remission status, the respective mean HbA1c levels at both medium- and long-term follow-ups improved significantly from 8.2 to 6.7 and 6.3 %. There was excellent improvement in glycemic control with almost over 70 % of patients being able to achieve HbA1c <7 % from early- to long-term follow-ups. Recurrent T2DM was possible but only developed in a small minority of patients at long-term evaluation. Even with recurrence, such patients did not require insulin therapy for disease control. All these results supported that LSG was able to produce sustainable glycemic improvement in the long run.
To overcome the common limitation of high lost-to-follow-up [5–7, 10], we had conducted a robust strategy to retrieve the missing follow-up data. For patients who did not turn up for follow-up assessments, we performed repeated individual telephone contacts to locate the patients. Once these patients were reached, we obtained their consents to retrieve their medical records from other healthcare providers or hospitals for data related to weight control and co-morbidity change. Relevant data at different follow-up time points were then re-entered into our bariatric surgery database. This effectively helped to minimize our lost-to-follow-up rates to only 6.1 % at short-term, 13.4 % at medium-term, and 15.3 % at long-term follow-ups. We believe that the available data in this study could make a representative contribution to the understanding of the long-term effects of LSG on weight loss, weight regain, and diabetic remission in Chinese patients.
In conclusion, laparoscopic sleeve gastrectomy is effective in achieving substantial weight loss and glycemic improvement of type 2 diabetes mellitus in morbidly obese Chinese patients. While weight regain was evident with time, the extent of rebound in %EWL was not remarkably high. T2DM remission and significant glycemic improvement are sustainable in long-term follow-up.
References
Langer FB, Reza Hoda MA, Bohdjalian A, et al. Sleeve gastrectomy and gastric banding: effects on plasma ghrelin levels. Obes Surg. 2005;15(7):1024–9.
Cohen R, Uzzan B, Bihan H, et al. Ghrelin levels and sleeve gastrectomy in super-super-obesity. Obes Surg. 2005;15(10):1501–2.
Karamanakos SN, Vagenas K, Kalfarentzos F, et al. Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy: a prospective, double blind study. Ann Surg. 2008;247(3):401–7.
Shi X, Karmali S, Sharma AM, et al. A review of laparoscopic sleeve gastrectomy for morbid obesity. Obes Surg. 2010;20(8):1171–7.
Himpens J, Dobbeleir J, Peeters G. Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann Surg. 2010;252(2):319–24.
Bohdjalian A, Langer FB, Shakeri-Leidenmühler S, et al. Sleeve gastrectomy as sole and definitive bariatric procedure: 5-year results for weight loss and ghrelin. Obes Surg. 2010;20(5):535–40.
Sarela AI, Dexter SP, O’Kane M, et al. Long-term follow-up after laparoscopic sleeve gastrectomy: 8–9-year results. Surg Obes Relat Dis. 2012;8(6):679–84.
Rawlins L, Rawlins MP, Brown CC, et al. Sleeve gastrectomy: 5-year outcomes of a single institution. Surg Obes Relat Dis. 2013;9(1):21–5.
Sieber P, Gass M, Kern B, et al. Five-year results of laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2014;10(2):243–9.
Zachariah SK, Chang PC, Ooi AS, et al. Laparoscopic sleeve gastrectomy for morbid obesity: 5 years experience from an Asian center of excellence. Obes Surg. 2013;23(7):939–46.
Gloy VL, Briel M, Bhatt DL, et al. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJ. 2013;347:f5934.
Maggard-Gibbons M, Maglione M, Livhits M, et al. Bariatric surgery for weight loss and glycemic control in nonmorbidly obese adults with diabetes: a systematic review. JAMA. 2013;309(21):2250–61.
Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366(17):1567–76.
Mingrone G, Panunzi S, De Gaetano A, et al. N Engl J Med. 2012;366(17):1577–85.
Gill RS, Birch DW, Shi X, et al. Sleeve gastrectomy and type 2 diabetes mellitus: a systematic review. Surg Obes Relat Dis. 2010;6(6):707–13.
Lee WJ, Wang W. Bariatric surgery: Asia-Pacific perspective. Obes Surg. 2005;15(6):751–7.
Kasama K, Mui W, Lee WJ, et al. IFSO-APC consensus statements 2011. Obes Surg. 2012;22(5):677–84.
Mui WL, Ng EK, Tsung BY, et al. Laparoscopic sleeve gastrectomy in ethnic obese Chinese. Obes Surg. 2008;18(12):1571–4.
Definition, diagnosis and classification of diabetes mellitus and its complication. World Health Organization 1999.
Buse JB, Caprio S, Cefalu WT, et al. How do we define cure of diabetes? Diabetes Care. 2009;32(11):2133–5.
Trastulli S, Desiderio J, Guarino S, et al. Laparoscopic sleeve gastrectomy compared with other bariatric surgical procedures: a systematic review of randomized trials. Surg Obes Relat Dis. 2013;9(5):816–29.
Diamantis T, Apostolou KG, Alexandrou A, et al. Review of long-term weight loss results after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2014;10(1):177–83.
Gagner M, Deitel M, Erickson AL, et al. Survey on laparoscopic sleeve gastrectomy (LSG) at the Fourth International Consensus Summit on Sleeve Gastrectomy. Obes Surg. 2013;23(12):2013–7.
Karmali S, Brar B, Shi X, et al. Weight recidivism post-bariatric surgery: a systematic review. Obes Surg. 2013;23(11):1922–33.
Conflict of Interest
Dr. Shirley Yuk-Wah Liu, Dr. Simon Kin-Hung Wong, Ms. Candice Chuen-Hing Lam, Ms. Man Yee Yung, Prof. Alice Pik-Shan Kong, and Prof. Enders Kwok-Wai Ng declare that they have no conflict of interest to disclose in this work.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in this study.
Statement of Human Rights
All procedures performed in this study were in accordance with the ethical standards of our institutional research ethics committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, S.YW., Wong, S.KH., Lam, C.CH. et al. Long-term Results on Weight Loss and Diabetes Remission after Laparoscopic Sleeve Gastrectomy for A Morbidly Obese Chinese Population. OBES SURG 25, 1901–1908 (2015). https://doi.org/10.1007/s11695-015-1628-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-1628-4