Abstract
Purpose
Bariatric surgery has been associated with bone remodeling changes. The action of adipokines on the expression of receptor activator of nuclear factor kappa β ligand (RANKL) and osteoprotegerin (OPG) and on an increase in sclerostin could be related to these changes.
Materials and Methods
This study aimed to assess the repercussions of weight loss, fat mass (FM), and fat-free mass (FFM) loss and biochemical and hormonal changes on bone remodeling markers after Roux-en-Y gastric bypass (RYGB). Anthropometric data, parathyroid hormone (PTH), bone-specific alkaline phosphatase (BSAP), collagen type 1 C-telopeptide (CTX), 25-hydroxy vitamin D (25-OH-VitD), leptin, adiponectin, RANKL, OPG, and sclerostin of 30 menstruating women were measured preoperatively (Pre), and 3, 12, and 24 months (m) after RYGB.
Results
Leptin (34.4 (14.7; 51.9) vs. 22.5 (1.9; 52.7) ng/mL) and OPG (3.6 (1.1; 11.5) vs. 3.4 (1.5; 6) pmol/L) decreased, and adiponectin (7.4 (1.7; 18.4) vs. 13.8 (3.0; 34.6) μg/mL), CTX (0.2 (0.1; 2.2) vs. 0.6 (0.4; 6.0) ng/mL), RANKL (0.1 (0.0; 0.5) vs. 0.3 (0.0; 2.0) pmol/L), and sclerostin (21.7 (3.2; 75.1) vs. 34.8 (6.4; 80.5) pmol/L) increased after 3 m. BSAP increased after 12 m (10.1 (5.4; 18.9) vs. 13.9 (6.9; 30.2) μg/mL) (p < 0.005). CTX correlated positively with adiponectin at 24 m and inversely with leptin Pre; OPG at 3 m; weight, FM, FFM, and leptin at 24 m. RANKL correlated directly with weight at 3 m. Sclerostin correlated inversely with weight Pre and FM at 3 m. BSAP correlated negatively with 25-OH-VitD at 12 m, and positively with PTH at 24 m.
Conclusions
RYGB induced weight loss, and biochemical, hormonal, and body composition changes are associated with higher bone remodeling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity has increased in the last decades, assuming an epidemic character as it affects approximately 600 million people globally and about one-third of the North American population [1]. In this context, bariatric surgery has been increasingly used as a therapeutic option for obese individuals who do not obtain satisfactory results from conventional treatments. Currently, it is considered the most effective and long-lasting treatment for obesity [2, 3]. Among the available surgical techniques, Roux-en-Y gastric bypass (RYGB) has been one of the most used, because of its lower rates of morbidity and mortality and high excess weight loss percentage [4].
Despite the benefits related to weight loss, this procedure has negative repercussions on bone metabolism [5–8], which could be particularly concerning in women [6]. Although the pathophysiological mechanisms responsible for these changes are still not totally elucidated, a possibility would be that weight and body composition changes induced by surgery would promote changes in hormone metabolism and adipose tissue, leading to variations in the levels of important adipokines [9–12], which could modulate the expression of the receptor activator of nuclear factor kappa β ligand (RANKL) and osteoprotegerin (OPG) [13–17].
Moreover, the lower mechanical load stemming from rapid and intense weight loss after surgery may increase the expression of sclerostin [6, 18–20]. This protein, coded by the SOST gene and produced exclusively by osteocytes, inhibits bone formation by inhibiting the terminal differentiation of osteoblasts and promotes their apoptosis [21, 22]. Sclerostin also reduces bone formation by Wnt, binding to the receptor LRP5/6 in osteoblast cell membrane, blocking the signaling pathway Wnt/β-catenin, and inhibiting the transcription of osteogenic genes [23–26].
Thus, changes in the levels of adipokines, RANKL, OPG, and sclerostin could be involved in the bone remodeling changes that occur after bariatric surgery, with bone repercussions proportional to weight loss [19, 20, 27–29]. However, studies on the subject are still scarce, and the relationships that exist between these proteins and bone remodeling after surgery have not been totally clarified. Thus, the objective of this study was to assess the repercussions of RYGB-related weight loss and body composition, biochemical, and hormonal changes on serum bone remodeling markers.
Materials and Methods
This prospective and observational study assessed the biochemical, hormonal, and bone remodeling parameters of obese women before and after RYGB, and it was approved by the local Research Ethics Committee (protocol number 3710-2010) and the studies were conducted according to the principles of the 1964 Helsinki Declaration. Informed consent was obtained from all individual participants included in the study.
Patients
The sample consisted of menstruating women aged 18 to 50 years, with obesity grades II (gII; BMI 35–39.99) or III (gIII; BMI ≥40.0). The women underwent RYGB according the institution’s protocol between May 2009 and December 2011. After the women were informed about the objectives of the study and the data collection procedures, they read and signed an informed consent form.
The exclusion criteria were the presence of the following conditions diagnosed by protocol tests established by the American Consensus for Bariatric Surgery [2]: severe renal or hepatic diseases, collagen diseases, hypogonadism, hyperparathyroidism, hyperthyroidism, type 2 diabetes mellitus (DM) decompensated or hypercortisolism, or use of drugs that knowingly affect bone metabolism (corticosteroids, thiazides diuretics, anticonvulsant, and furosemide); discontinuation of nutritional or medical follow-up; and gestation.
Preoperatively, the patients were followed at an outpatient clinic for 12 months by dietitians, psychologists, and endocrinologists to better prepare them for surgery and minimize perioperative risks. During this time, the patients underwent tests to exclude endocrine causes of obesity and assess surgical risk. Of the 35 initial candidates, one patient died 1 week after surgery, and another, 6 months after surgery, both from obesity-related complications. Three patients were lost to follow-up. Thus, 30 patients were effectively studied.
Study Design
The patients eligible for surgery were called 3 days before the procedure for data collection (age, self-reported ethnicity) and baseline anthropometric and biochemical assessments (T0). These assessments were repeated 3 (T3), 12 (T12), and 24 months (T24) after surgery. In each visit, the patients received medical and nutritional advice and were prescribed a multivitamin/multimineral supplement (Materna®), protein supplement (30 g/day, Isofort®, for the first 30 days after surgery), calcium citrate (1200 to 1500 mg/day), cholecalciferol (3000 IU/day), and intramuscular vitamin B12 (5000 IU every 3 months, Citoneurin®) [30].
Anthropometric measurements (weight (in kilograms (kg)) and height (in meters (m)), body mass index (BMI), weight loss (%), and body composition (fat mass (FM, in kilograms and percentage) and the fat-free mass (FFM, in kilograms and percentage) determined by bioelectrical impedance analysis (Maltron BF model 906; Rayleigh, Essex, England))) were collected on all study occasions by the same researcher (MFGB).
Laboratory Analysis
The studied bone remodeling markers were collagen type 1 C-telopeptide (CTX) and bone-specific alkaline phosphatase (BSAP). The other biochemical and hormonal variables were serum calcium (Ca), parathyroid hormone (PTH), 25-hydroxy vitamin D (25-OH-VitD), leptin, adiponectin, RANKL, OPG, and sclerostin.
Blood was collected in tubes containing separator gel components, using a needle coupled with the Vacutainer® system, and the tubes were centrifuged at 3000 rpm by a cooled centrifuge for 10 min. The serum was frozen to −80 °C until determination of the Ca and PTH levels by the dry chemistry method and chemiluminescence, respectively. BSAP and CTX were determined by chemiluminescence (Beckman Coulter, Fullerton, CA); 25-OH-VitD was measured by high-performance liquid chromatography (HPLC) (DiaSorin kit, Stillwater, MN, USA). The serum was also used for the measurements of adiponectin, leptin, RANKL, OPG, and sclerostin, which were measured by enzyme-linked immunosorbent assay-ELISA (Biomedica Medizinprodukte GmbH & Co. KG, Vienna, Austria).
Statistical Analyses
Statistical analyses of the anthropometric and laboratory data were performed by the software SPSS® version 21.0 for Windows (Statistical Package for the Social Sciences) and Microsoft Office Excel version 2010. The study occasions were compared by the non-parametric Friedman test, followed by Dunn’s multiple comparison test. Spearman’s correlation coefficient verified the correlation between the various study variables. All analyses used a statistical significance level of 5%.
Results
Clinical Characteristics
The median age of the patients at baseline was 41.5 years, and 70% (n = 21) reported being white. The calculated 24-month excess weight lost (%EWL) for these patients was 71.9 ± 18.1% using the calculation method [62]. The median (min-max) BMI decreased from 48.3 (37.8; 62.2) kg/m2 before surgery to 39 (30.8; 50.9) kg/m2, 33.1 (23.1; 41.2) kg, and 31.8 (23; 40.4) kg/m2 at 3, 12 (p < 0.001), and 24 months of procedure, respectively. Before surgery, 90% of the patients had obesity gIII; at the end of the follow-up, 57% (17) of the patients continued to be obese, and only 10% (3) had a BMI compatible with their ideal weight (p < 0.01; Table 1). Surgery promoted progressive and significant loss of weight and its compartments, which were more expressive in the first year after surgery (p < 0.05; Table 1). Total weight decreased by a median (min-max) of 40.95 (21.0; 75.0) kg, of which 33.45 (16.3; 63.5) kg were FM and 7.9 (1.4; 17.1) kg were FFM. In percentages, fat mass decreased by 12 (5.1; 30.8) %, and FFM increased by 12.03 (5.1; 30.9) % (p < 0.05).
Laboratory Data
The baseline serum levels of 25-OH-VitD were compatible with vitamin D insufficiency or deficiency in 90% of the patients. This percentage had decreased to 70% by T3 and T12 and to 66% by T24. Ca and PTH levels did not change between T0 and T24 (p > 0.05) (Table 2).
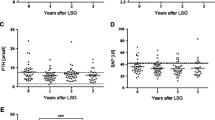
Adiponectin increased significantly while leptin decreased between T0 and the other occasions. Unlike adiponectin, whose level changed between T3 and T12, leptin level did not change between the postoperative follow-ups (Table 2; Fig. 1).
Changes in serum adipokine, bone remodeling markers, and other bone markers in 30 patients submitted to Roux-en-Y gastric bypass (RYGB) before (T0) and 3 (T3), 12 (T12), and 24 (T24) months after surgery. a Adiponectin (T0 < T3, T12, T24; T3 < T24; p < 0.05). b Leptin (T0 > T3, T12, T24; p < 0.05). c Collagen type 1 C-telopeptide (CTX) (T0 < T3, T12; T3 > T24; p < 0.05). d Bone-specific alkaline phosphatase (BSAP) (T0 < T12, T24; T3 < T12, T24; p < 0.05). e Receptor activator of nuclear factor kappa β ligand (RANKL) (T0 < T3; T3 > T24; p < 0.05). f Osteoprotegerin (OPG) (T0 > T3, T12, T24; p < 0.05). g Serum sclerostin changes in 30 patients submitted to Roux-en-Y gastric bypass (RYGB) before and 3, 12, and 24 months after surgery (T0 < T3 ; T3 > T12, T24; p < 0.05)
RANKL and sclerostin were higher at T3, but OPG was lower. Postoperatively, RANKL changed between T3 and T12, sclerostin changed between all three postoperative follow-ups, and OPG did not vary (Table 2; Fig. 1).
Serum CTX increased significantly between T0 and T3, remained high at T12, and decreased by T24 (p < 0.001) (Table 2; Fig. 1). BSAP was higher at T12 (p < 0.001) and remained high at T24 (Table 2; Fig. 1).
At T24, CTX correlated inversely with body weight (r = −0.451; p = 0.024), FM (r = −0.418; p = 0.038), and FFM (r = −0.417; p = 0.038) in kilograms. CTX also correlated negatively with serum leptin preoperatively (r = −0.40; p = 0.031), at T24 (r = −0.554; p = 0.004), and with OPG at T3 (r = −0.37; p = 0.048); finally, it correlated positively with adiponectin at T24 (r = 0.453; p = 0.023). RANKL was directly correlated with body weight at T3 (r = 0.366; p = 0.046). Sclerostin correlated inversely with body weight at T0 (r = −0.379; p = 0.039) and with FM at T3 (r = −0.391; p = 0.03). BSAP correlated negatively with 25-OH-VitD at T12 (r = −0.412; p = 0.033) and positively with PTH at T24 (r = 0.49; p = 0.024).
Discussion
The negative influence of weight loss and the hormonal and biochemical changes induced by bariatric surgery on bone health has been reported [7, 11, 20, 31–35], in addition to the association between excess body weight loss and bone mineral density (BMD) 1 to 2 years after RYGB [20, 34, 36].
Bone turnover increased in the study sample, evidence by higher CTX and BSAP after RYGB. Interestingly, CTX increased 3 months after the procedure, remained high at the 1-year follow-up, and decreased by the 2-year follow-up. These findings corroborate Yu et al. (2015) who found that this marker increased significantly and was associated with BMD 2 years after RYGB [7]. Elias et al. (2014) compared RYGB with vertical-banded gastroplasty, found that these changes did not occur in women submitted to gastroplasty, and suggested that bone loss may be more strongly associated with techniques that promote malabsorption [37]. The BSAP levels in the study sample had increased by T12 and remained high at T24, confirming Bruno et al. (2010), who observed this same behavior in this enzyme after the same follow-up period [38]. These findings suggest that bone formation occurs after bone resorption. Indeed, another study did not find changes in this marker shortly after RYGB [39].
The mechanisms involved in the relationship between bariatric surgery and bone changes are complex and not fully understood. A possibility would be the effect of adipokines on bone remodeling and markers. However, data on this effect are controversial. Some studies find an association with bone formation markers and report positive [13, 19, 40] or negative action, regardless of gender, age, and BMI [41, 42]. The adiponectin of the present sample was directly correlated with CTX at T24. Its levels increased progressively from T3 to T12, but had stabilized by T24. As a matter of fact, this adipokine is inversely related to the amount of adipose tissue and can be associated with postoperative bone changes [43]. Although scarce, studies have reported an increase in adiponectin and its association with higher bone resorption, evidenced by higher collagen type 1 cross-linked N-telopeptide (NTX), or lower total, spinal, and pelvic BMD in patients submitted to RYGB [29, 44, 45].
Leptin was inversely correlated with CTX at T0 and T24. Its level decreased significantly between T0 and T3, but stabilized after T3. Weight loss reduces leptin secretion, suggesting that this protein may have a paracrine or endocrine effect on bone remodeling [42, 46]. Leptin seems to behave contrary to adiponectin as it correlates directly with weight [29, 47, 48] and inversely with bone resorption markers, such as NTX [38, 42, 49].
In addition to adipokines, other proteins seem to be involved in the pathophysiological mechanism associated with bariatric surgery-induced bone changes. In bone remodeling, the balance between bone formation and resorption is sustained by the RANK/RANKL/OPG axis [50], which regulates osteoclastogenesis and is responsible for bone resorption or osteoclast apoptosis, stimulating bone formation [51]. The adipose tissue may unbalance the RANKL/RANK/OPG axis and consequently, change bone mass. The significant increase in RANKL in the study sample associated with OPG decrease after surgery, as well as the inverse relationship between CTX and OPG at T3 suggest higher osteoclastic activity and early bone resorption after RYGB. These findings confirm other studies that suggest a strong correlation between weight loss and body composition changes as bone resorption increases and BMD decreases [13, 52, 53]. Studies on RANKL and OPG behavior after RYGB in humans were not found.
Finally, complementing the hypothesis of the relationship between adipose tissue loss and higher bone resorption, researchers have proposed that skeletal load may be an efficient means of avoiding bone loss and increasing the formation of new bone [54]. Thus, load changes may induce a compensatory increase in bone remodeling [55] mediated by osteocytes and sclerostin and inhibit the Wnt/β-catenin pathway [23–25, 56]. When the body is not properly exercised or the skeletal load decreases very quickly due to the intense and rapid weight loss promoted by bariatric surgery, bone turnover increases, as indicated by bone resorption markers, which are sometimes associated with lower BMD and higher risk of fractures [6, 57]. The endogenous inhibitor of the Wnt pathway, sclerostin, is considered a key regulator of bone homeostasis, and it can be used as a new marker for bone resorption assessment [20, 58]. This protein increases in individuals who join a weight loss program after they lose at least 10% of their body weight [38, 59–61]. Nevertheless, its role after bariatric surgery is controversial. The increase in serum sclerostin provides important information about the continuous loss of BMD after surgery [19, 20]. Nonetheless, Grethen et al. (2012) did not find serum sclerostin changes in obese women submitted to RYGB and normal-weight women [19]. Sclerostin increased significantly in the study sample between T0 and T3, but had decreased by T12. This protein was negatively correlated with total body weight before surgery and with FM 3 months after RYGB, which could be partly explained by the mechanostat theory. Therefore, while preoperative excess weight would be associated with low sclerostin, protecting against bone resorption, the rapid initial weight loss, especially the loss of body fat induced by bariatric surgery, could increase the protein level in the first months after RYGB. Thus, lower sclerostin in the long-term follow-ups could be related, among others, to weight loss deceleration during this phase.
Some of the study limitations include its observational character and sample size. Despite these limitations, this study is clinically important because it established that FM and FFM loss after RYGB can be associated with changes in proteins intrinsically related to bone tissue metabolism, namely adiponectin, leptin, RANKL, OPG, and sclerostin, which can be involved in the mechanisms associated with higher bone remodeling after surgery.
Conclusion
Bariatric surgery remains the most effective treatment for severely obese patients, although the potential effects on bone health are only partially understood. There is a complex relationship between weight loss and biochemical, hormonal, and body composition changes induced by RYGB, with many peripheral and central mediators potentially involved in the regulation of bone homeostasis.
Changes of sclerostin, CTX, and adiponectin in this study provide further important information on bone metabolism in patients after bariatric surgery. Apparently, the weight reduction and the body compartments and changes of adipokines interfere on bone remodeling. The clinical implications for osteoporosis and fracture risk are still unclear and additional data are clearly needed to characterize the clinical impact of the observed bone loss, but, in order to prevent bone loss and fractures, the health care team should start monitoring the aspects of the daily life of patients who undergo RYGB early and thoroughly.
References
World Health Organization. Global status report on non communicable diseases 2014. Disponível em:< http://www.who.int/nmh/publications/ncd-status-report-2014/en/>. Access in: mar. 2016.
Mechanick JI, Kushner RF, Sugerman HJ, et al. American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery medical guidelines for clinical practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient. Endocr Pract. 2008;14(Suppl 1):1–83.
Ricci C, Gaeta M, Rausa E, et al. Early impact f bariatric surgery on type II diabetes, hipertension, and hyperlipidemia: a systematic review, meta-analysis and meta-regression on 6.587 patients. Obes Surg. 2014;24:522–8.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23(4):427–36.
Stemmer K, Bielohuby M, Grayson BE, et al. Roux-en-Y gastric bypass surgery but not vertical sleeve gastrectomy decreases bone mass in male rats. Endocrinology. 2013;154:2015–24.
Stein EM, Silverberg SJ. Bone loss after bariatric surgery: causes. Consequences and Management Lancet Diabetes Endocrinol. 2014;2(2):165–74.
Yu EW, Bouxsein ML, Putman MS, et al. Two-year changes in bone density after Roux-en-Y gastric bypass surgery. J Clin Endocrinol Metab. 2015;100(4):1452–9.
Liu C, Wu D, Zhang J, et al. Changes in bone metabolism in morbidly obese patients after bariatric surgery: a meta-analysis. Obes Surg. 2016;26(1):91–7.
Yu EW. Bone metabolism after bariatric surgery. J Bone Miner Res. 2014;29(7):1507–18.
Karefylakis C, Näslund I, Edholm D, et al. Vitamin D status 10 years after primary gastric bypass: gravely high prevalence of hypovitaminosis D and raised PTH levels. Obes Surg. 2014;24(3):343–8.
Hage MP, El-Hajj FG. Bone and mineral metabolism in patients undergoing Roux-en-Y gastric bypass. Osteoporosis Int. 2014;25:423–39.
Butte NF, Brandt ML, Wong WW, et al. Energetic adaptations persist after bariatric surgery in severely obese adolescents. Obesity (Silver Spring). 2015;23(3):591–601.
Luo XH, Guo LJ, Xie H, et al. Adiponectin stimulates RANKL and inhibits OPG expression in human osteoblastos through the MAPK signalling pathway. J Bone Miner Res. 2006;21:1648–56.
Nakamichi Y, Udagawa N, Kobayashi Y, et al. Osteoprotegerin reduces the serum level of receptor activator of NF-ΚB ligand derived from osteoblasts. J Immunol. 2007;178:192–200.
Elissondo N, Rosso LG, Maidana P, et al. Adiponectina: una adipocitoquina con múltiples funciones protectoras. Acta Bioquím Clín Latinoam. 2008;42(1):17–33.
Cao JJ. Effects of obesity on bone metabolism. J Orthop Surg Res. 2011;6:30.
Kanazawa I. Adiponectin in metabolic bone disease. Curr Med Chem. 2012;19(32):5481–92.
Hogan SL. The effects of weight loss on calcium and bone. Crit Care Nurs Q. 2005;28(3):269–75.
Grethen E, Hill KM, Jones R, et al. Serum leptin, parathyroid hormone, 1,25-dihydroxyvitamin D, fibroblast growth factor 23, bone alkaline phosphatase, and sclerostin relationships in obesity. J Clin Endocrinol Metab. 2012;97(5):1655–62.
Muschitz C, Kocijan R, Marterer C, et al. Sclerostin levels and changes in bone metabolism after bariatric surgery. J Clin Endocrinol Metab. 2015;100(3):891–901.
Wijenayaka AR, Kogawa M, Lim HP, et al. Sclerostin stimulates osteocyte support of osteoclast activity by a RANKL-dependent pathway. PLoS One. 2011;6:e25900.
Atkins GJ, Rowe PS, Lim HP, et al. Sclerostin is a locally acting regulator of late-osteoblast/preosteocyte differentiation and regulates mineralization through a MEPE-ASARM-dependent mechanism. J Bone Miner Res. 2011;26:1425–36.
Moester MJC, Papapoulos SE, Löwik CWGM, et al. Sclerostin: current knowledge and future perspectives. Calcif Tissue Int. 2010;87(2):99–107.
Lewiecki EM. Sclerostin: a novel target for intervention in the treatment of osteoporosis. Discov Med. 2011;12(65):263–73.
Dovjak P, Dorfer S, Föger-Samwald U, et al. Serum levels of sclerostin and dickkopf-1: effects of age, gender and fracture status. Gerontology. 2014;60:493–501.
Eriksen EF. Commentary on sclerostin deficiency is linked to altered bone composition. J Bone Miner Res. 2014;29(10):2141–3.
Fleischer J, Stein EM, Bessler M, et al. The decline in hip bone density after gastric bypass surgery is associated with extent of weight loss. J Clin Endocrinol Metab. 2008;93(10):3735–40.
Gannagé-Yared MH, Yaghi C, Habre B, et al. Osteoprotegerin in relation to body weight, lipid parameters insulin sensitivity, adipocytokines, and C-reactive protein in obese and non-obese young individuals: results from both cross-sectional and interventional study. Eur J Endocrinol. 2008;158(3):353–9.
Wroblewski E, Swidnicka-Siergiejko A, Hady HR, et al. Variation in blood levels of hormones in obese patients following weight reduction induced by endoscopic and surgical bariatric therapies. Cytokine. 2016;77:56–62.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Endocr Pract. 2013;19(2):337–72.
Viégas M, Vasconcelos RS, Neves AP, et al. Bariatric surgery and bone metabolism: a systematic review. Arq Bras Endocrinol Metabol. 2010;54(2):158–63.
Vasconcelos RS, Viégas M, Marques TF, et al. Factors associated with secondary hyperparathyroidism in premenopausal women undergoing Roux-en-Y gastric bypass for the treatment of obesity. Arq Bras Endocrinol Metabol. 2010;54(2):233–8.
Williams SE. Metabolic bone disease in the bariatric surgery patient. J Obes. 2011;2011:634614.
Carrasco F, Basfi-fer K, Rpjas P, et al. Changes in bone mineral density after sleeve gastrectomy or gastric bypass: relationships with variations in vitamin D, ghrelin, and adiponectin levels. Obes Surg. 2014;24:877–84.
Register TC, Divers J, Bowden DW, et al. Relationships between serum adiponectin and bone density, adiposity and calcified atherosclerotic plaque in the African American-Diabetes Heart Study. J Clin Endocrinol Metab. 2013 May;98(5):1916–22.
Balsa JA, Lafuente C, Gómez-Martín JM, et al. The role of serum osteoprotegerin and receptor–activator of nuclear factor-κB ligand in metabolic bone disease of women after obesity surgery. J Bone Miner Metab. 2015;1-7
Elias E, Casselbrant A, Werling M, et al. Bone mineral density and expression of vitamin D receptor-dependent calcium uptake mechanisms in the proximal small intestine after bariatric surgery. Br J Surg. 2014;101(12):1566–75. doi:10.1002/bjs.9626.
Bruno C, Fulford AD, Potts JR, et al. Serum markers of bone turnover are increased at six and 18 months after Roux-en-Y bariatric surgery: correlation with the reduction in leptin. J Clin Endocrinol Metab. 2010;95(1):159–66. doi:10.1210/jc.2009-0265.
Biagioni MFG, Mendes AL, Nogueira CR, et al. Weight-reducing gastroplasty with Roux-en-Y gastric bypass: impact on vitamin D status and bone remodeling markers. Metab Syndr Relat Disord. 2014;12(1):11–5.
Oshima K, Nampei A, Matsuda M, et al. Adiponectin increases bone mass by suppressing osteoclast and activating osteoblast. Biochem Biophys Res Commun. 2005;331(2):520–6.
Lenchik L, Register TC, Hsu FC, et al. Adiponectin as a novel determinant of bone mineral density and visceral fat. Bone. 2003;33(4):646–51.
Aguirre L, Napoli N, Waters D, et al. Increasing adiposity is associated with higher adipokine levels and lower bone mineral density in obese older adults. J Clin Endocrinol Metab. 2014;99(9):3290–7.
Naot D, Cornish J. Cytokines and hormones that contribute to the positive association between fat and bone. Front Endocrinol. 2014;5:70.
Carrasco F, Ruz M, Rojas P, et al. Changes in bone mineral density, body composition and adiponectin levels in morbidly obese patients after bariatric surgery. Obes Surg. 2009;19(1):41–6.
Bruno C, Fulford AD, Potts JR, et al. Serum markers of bone turnover are increased at six and 18 months after Roux-en-Y bariatric surgery: correlation with the reduction in leptin. J Clin Endocrinol Metab. 2010;95:159–66.
Prado WL, Piano A, Lazaretti-Castro M, et al. Relationship between bone mineral density, leptin and insulin concentration in Brazilian obese adolescents. J Bone Miner Metab. 2009;27:613–9.
Thomas T, Burguera B. Is leptin the link between fat and bone mass? J Bone Miner Res. 2002;17:1563–9.
Walicka M, Czerwińska E, Tałałaj M, et al. Influence of weight reduction on leptin concentration and bone mineral density in patients with morbid obesity before and 6 months after bariatric surgery. Endokrynologia Polska. 2009;60(2):97–102.
Mohiti-Ardekani J, Soleymani-Salehabadi H, et al. Relationships between serum adipocyte hormones (adiponectin, leptin, resistin), bone mineral density and bone metabolic markers in osteoporosis patients. J Bone Miner Metab. 2014;32(4):400–4.
Bonewald LF, Johnson ML. Osteocytes, mechanosensing and Wnt signaling. Bone. 2008;42(4):606–15.
Zhang R, Oyajobi BO, Harris SE, et al. Wnt/β-catenin signaling activates bone morphogenetic protein 2 expression in osteoblasts. Bone. 2013;52(1):145–56.
Yamauchi T, Kamon J, Waki H, et al. The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat Med. 2001;7:941–6.
Wang Y, Lam KS, Xu JY, et al. Adiponectin inhibits cell proliferation by interacting with several growth factors in an oligomerization-dependent manner. J Biol Chem. 2005;280:18341–7.
Schoenau E. Bone mass increase in puberty: what makes it happen? Horm Res Paediatr. 2006;65(2):2–10.
Frost HM. Bone “mass” and the “mechanostat”. A proposal Anat Rec. 1987;219:1–9.
Van Bezooijen RL, Svensson JP, Eefting D, et al. Wnt but not BMP signaling is involved in the inhibitory action of sclerostin on BMP-stimulated bone formation. J Bone Miner Res. 2007;22(1):19–28.
Schwartz AV, Johnson KC, Kahn SE, et al. Effect of 1 year of an intentional weight loss intervention on bone mineral density in type 2 diabetes: results from the look AHEAD randomized trial. J Bone Miner Res. 2012;27(3):619–27.
Bellido T. Summary—osteocyte control of bone formation via Sost/sclerostin. J Musculoskelet Neuronal Interact. 2006;6(4):360–3.
Granado-Lorencio F, Simal-Antón A, Salazar-Mosteiro J, et al. Time-course changes in bone turnover markers and fat-soluble vitamins after obesity surgery. Obes Surg. 2010;20:1524–9.
Villareal RA, Sadler C, Napoli N, et al. Weight loss in obese older adults increases serum sclerostin and impairs hip geometry but both are prevented by exercise training. Bone Miner Res. 2012;27(5):1215–21.
Muschitz C, Kocijan R, Haschka J, et al. The impact of vitamin D, calcium, protein supplementation, and physical exercise on bone metabolism after bariatric surgery: the BABS study. J Bone Miner Res. 2016;31(3):672–82.
Deitel M, Greenstein R. Editorial: recommendations for reporting weight loss. Obes Surg. 2003;13:159–60.
Acknowledgments
This project was supported by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), process number 2009/50169-6. The authors gratefully acknowledge the statistical support of Dr HRC Nunes and are grateful to the surgeons and nursing staff of the Surgery Department, Clinical Hospital, FMB, Unesp.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the local Research Ethics Committee (protocol number 3710-2010) and was conducted according to the principles of the 1964 Helsinki Declaration. Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Biagioni, M.F.G., Mendes, A.L., Nogueira, C.R. et al. Bariatric Roux-En-Y Gastric Bypass Surgery: Adipocyte Proteins Involved in Increased Bone Remodeling in Humans. OBES SURG 27, 1789–1796 (2017). https://doi.org/10.1007/s11695-017-2546-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2546-4