Abstract
Background
The available evidence indicates a progressive increase in the incidence and severity of the deficiency of certain vitamins and related clinical conditions (i.e., metabolic bone disease). Because of the potential role of fat-soluble vitamins and carotenoids in bone metabolism, our aim was to assess the time-course changes of fat-soluble vitamins and serum markers of bone metabolism in candidates for obesity surgery and following two bariatric procedures.
Methods
Sixty-five candidates for bariatric surgery and 150 serum samples after obesity surgery (i.e., Roux-en-Y gastric bypass, n = 85; biliopancreatic diversion, n = 65) were consecutively analyzed over a period of more than 2 years. Retinol, α- and γ-tocopherol, 25-OH-vitamin D3, β-cryptoxanthin, and β-carotene were analyzed by high-performance liquid chromatography. Calcium, phosphorus, alkaline phosphatase, intact parathyroid hormone (iPTH), osteocalcin, beta-crosslaps, and N-terminal peptide of procollagen I (P1NP) were determined using commercial kits.
Results
Retinol, β-cryptoxanthin, β-carotene, and α- and γ-tocopherol levels were significantly lower in post-surgery samples while osteocalcin, b-crosslaps, and P1NP were significantly increased. Along the time and regardless of the surgical procedure, P1NP, b-crosslaps, and osteocalcin increased during the first 12–24 months but declined afterward. 25-OH-vitamin D increased during the first 12 months and tended to decrease afterward while iPTH remained constant or decreased but increased after 1 year in both groups. Vitamin A remained constant but α- and γ-tocopherol, β-cryptoxanthin, and β-carotene decreased in both groups.
Conclusions
In addition to the nutritional assessment, regular monitoring of bone markers seems necessary in these patients and the early introduction of preventive strategies (i.e., the use of antiresorptive agents) should be evaluated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Overweight and obesity is a growing health problem, with the number of interventions performed increasing significantly in recent years. Nutrient deficiencies are common following bariatric surgery and may depend on the surgical approach, as they are proportional to the length of the absorptive area and the percent weight loss [1–3]. The available evidence indicates a high prevalence of micronutrient deficiencies in morbidly obese patients [4] and a progressive increase in the incidence and severity of the deficiency of certain vitamins (i.e., A, E, D) and related clinical conditions (i.e., metabolic bone disease) [1–3].
Obesity is associated with a reduced risk of osteoporosis while, overall, bariatric surgery procedures are complicated by gastrointestinal complaints, bone resorption, and bone loss [5, 6]. Longitudinal studies of obese patients after gastric bypass operations demonstrate a greater than expected drop in bone mineral density (BMD) [7], and low body weight and recent weight loss are confirmed risk factors for osteoporotic fractures [8, 9]. Also, biliopancreatic diversion is followed by bone mass loss, mainly attributed to calcium and vitamin D malabsorption leading to secondary hyperparathyroidism [10].
More recently, several dietary factors and antioxidants (i.e., vitamin A, vitamin E, carotenoids) have attracted much attention due to their potential relevance in bone health. Evidence includes the negative association between osteocalcin (a bone formation marker) and retinol [11], the association between carotenoid intake and loss of bone mineral density [12], and the in vitro, animal, and human evidence suggesting a unique anabolic effect on bone calcification and osteoporosis prevention of β-cryptoxanthin [13]. Additionally, high oxidative stress is associated with reduced BMD and bone metabolism markers in hypercholesterolemic subjects [14] and elderly men [15], and serum α-tocopherol levels seem to modify the association between urinary 8-iso-PGF2α and BMD in the elderly [15]. Thus, because of the potential role of fat-soluble vitamins and carotenoids in bone metabolism, our aim was to assess the time-course changes of fat-soluble vitamins and serum markers of bone metabolism in candidates for obesity surgery and following two commonly used bariatric procedures: biliopancreatic diversion (BPD) and Roux-en-Y gastric bypass (RYGBP).
Methods
Sixty-five candidates for bariatric surgery (12 men, 53 women; age 42 ± 10 years) and a total of 150 serum samples after obesity surgery (i.e., RYGBP (n = 85) and BPD (n = 65)) were consecutively collected and assessed. Average time of sample collection after surgery was 15 months (11, 18 months, 95% confidence interval (CI)) for patients with BPD and 17 months (11, 22 months, 95% CI) for those with RYGBP. For 19 subjects, both pre-operative and post-operative samples were obtained. Since the consecutive visits of the patients after surgery are individually scheduled according to clinical criteria, to assess the effect of time after surgery, samples were combined to get time intervals as follows: 0–3, >3–12, >12–24, and >24 months. According to these intervals, a total of 52 samples corresponded to 0–3 months (18 for BPD and 34 for RYGBP), 39 to >3–12 months (17 for BPD and 22 for RYGBP), 28 to >12–24 months (17 for BPD and 11 for RYGBP), and 31 to >24 months (13 for BPD and 18 for RYGBP).
Fasting blood samples were drawn for the routine assessment of fat-soluble vitamins (retinol, α-tocopherol, and 25-OH-D3). Additionally, we analyzed provitamin A carotenoids (β-cryptoxanthin and β-carotene), γ-tocopherol, and bone metabolism markers including calcium, phosphorus, alkaline phosphatase, intact parathyroid hormone (iPTH), osteocalcin, beta-crosslaps (b-CTx), and N-terminal peptide of procollagen I (P1NP). Serum samples were stored at −20°C until analysis (<2 weeks for vitamin and carotenoid analysis and <3 months for bone markers).
Samples were analyzed by a quality-controlled high-performance liquid chromatography (HPLC) method used for the simultaneous determination of vitamins A (retinol), E (α- and γ-tocopherol), and 25-OH-vitamin D3, which also allows the separation and quantification of β-cryptoxanthin and β-carotene [16]. The validity of the HPLC method is contrasted periodically through our participation in the Fat-Soluble Quality Assurance Programme (National Institute of Standards and Technology, Gaithersburg, MD, USA) and the Vitamin D External Quality Assurance Survey (Charing Cross Hospital, London, UK).
Osteocalcin, iPTH, CTx, and P1NP were determined using commercially available electrochemiluminescence immunoassays (Elecsys 2010, Roche Diagnostics), with variation coefficients <6.5% for all the analytes (Manufacturer information sheets). Other serum biochemical determinations (i.e., alkaline phosphatase, calcium, phosphorus) were carried out at the General Biochemistry Laboratory of the hospital according to routine quality-controlled standard methods.
Statistical Analysis
All data are expressed as mean and 95% confidence intervals. Baseline versus post-operative values, surgery-induced changes between the two groups (BPD versus RYGBP), and changes along the time within and between groups of surgical procedures were assessed using one-factor ANOVA and Dunnett’s post hoc test (pre-surgery levels were used as the reference). Relationships between fat-soluble vitamins, carotenoids, and bone markers were assessed using Pearson correlation coefficients. The statistical software package SPSS release 12.0.1 (SPSS, Inc., Chicago, IL, USA) was used. P values less than 0.05 were considered statistically significant.
Results
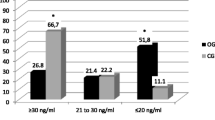
On a group level, post-surgery values were significantly lower than pre-surgery concentrations for retinol, provitamin A carotenoids, and vitamin E (both α- and γ-tocopherol) while bone remodeling markers (osteocalcin, b-crosslaps, and P1NP) were significantly increased after obesity surgery (Table 1). Comparing both surgical procedures, levels of PTH were significantly higher and alkaline phosphatase lower in DPB than in RYGBP samples while calcium, 25-OH-vitamin D, α- and γ-tocopherol, and provitamin A carotenoids were significantly lower in BPD samples. beta-Crosslaps, P1NP, osteocalcin, phosphorus, and vitamin A did not differ according to the type of surgical procedure (Table 1).
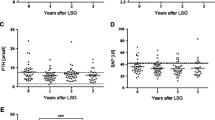
Along the time and regardless of the surgical procedure, P1NP and beta-crosslaps increased during the first 12 months and osteocalcin up to 12–24 months, but all of them declined afterward (Fig. 1a–c). As shown, although maximum values were reached at different time points according to the type of surgery, no significant differences between the two procedures were observed at any of the time intervals evaluated. Calcium, phosphorus, and alkaline phosphatase showed fluctuations but remained within reference values. In both groups, 25-OH-vitamin D increased during the first 12 months with a trend to decrease afterward while PTH remained constant or decreased during the first 0–12 months (RYGBP group) but tended to increase after 1 year in both groups. Vitamin A showed small variations in both groups but tended to remain constant over the time, while α-tocopherol, γ-tocopherol, β-cryptoxanthin, and β-carotene decreased in both groups, being more pronounced in the BPD patients (Table 1). For subjects with pre- and post-surgery samples (n = 19), time-course changes could be assessed only during the first year. Similarly, in this group, significant increments were observed in bone remodeling markers (P1NP, p = 0.004 at 0–3 months; b-crosslaps, p < 0.001 at 0–3 and 3–12 months; osteocalcin, p = 0.029 at 3–12 months) and 25-OH-vitamin D (p = 0.009 at 3–12 months) while a significant decrease was evident for γ-tocopherol (p = 0.003 at 0–3 months and p = 0.005 at 3–12 months), β-cryptoxanthin (p = 0.003 and 0.001 at 0–3 and 3–12 months, respectively), and β-carotene (p = 0.046 at 0–3 months). Vitamin A, vitamin E, and PTH decreased but did not reach statistical significance.
Time course of serum concentrations of bone turnover markers in candidates and after obesity surgery. a beta-Crosslaps (dashed line; upper reference level for pre-menopausal women), b P1NP (dashed line; upper reference level for pre-menopausal women), c osteocalcin (dashed line; upper reference level for pre-menopausal women >20 years). Dark circles BPD group, light circles RYGBP group. *p < 0.05; **p < 0.005 (one-way ANOVA and Dunnett’s post hoc test (pre-surgery levels as the reference))
In pre-surgery samples, bone remodeling markers (except alkaline phosphatase) were significantly correlated (r > 0.61, p < 0.001) while parathyroid hormone was inversely correlated with 25-OH-vitamin D (r = −0.29, p = 0.035) and calcium (r = −0.28, p = 0.05) but unrelated to bone markers. Only serum vitamin A was positively associated with serum osteocalcin (r = 0.31, p = 0.25). Post-surgery, bone markers, including alkaline phosphatase, remained positively correlated but other associations changed. PTH was positively associated with P1NP (r = 0.22, p = 0.011) and negatively with calcium (r = −0.31, p < 0.001), 25-OH-vitamin D (r = −0.53, p < 0.001), α-tocopherol (r = −0.18, p = 0.034), and β-carotene (r = −0.19, p = 0.034). Both α-tocopherol and vitamin A showed positive relations with serum calcium (r = 0.22, p < 0.010) while only γ-tocopherol showed inverse significant correlations with P1NP (r = −0.26, p = 0.002) and osteocalcin (r = −0.25, p = 0.003). Serum 25-OH-vitamin D correlated with beta-crosslaps (r = 0.22, p = 0.008).
Discussion
Overall, the present results are consistent with previous findings regarding the effect of obesity surgery on nutritional markers of fat-soluble vitamin status in these patients [4, 17–19]. Also, our findings support that while nutrient insufficiencies are common following bariatric surgery, for some nutrients, the degree is related to the surgical approach (i.e., γ-tocopherol, β-cryptoxanthin, β-carotene) and probably proportional to the length of the absorptive area [1, 2]. Similarly, our observations regarding the increases in bone turnover markers during the first year after obesity surgery are consistent with previous studies [18–20]. In addition, this increment in bone turnover markers was present regardless of the type of surgical procedure (i.e., BPD or RYGBP) as previously observed [21], the changes in 25-OH-vitamin D status, or the presence of secondary hyperparathyroidism [6, 20, 22].
It has been suggested that bone mass reduction is a normal adaptation to the decreased loading of the bone following weight loss [22] and that bone markers remain increased in the long term [18, 23]. Consistently, we found these increments during the first year both on a group level and also in the subgroup of patients with pre- and post-surgery samples. Nevertheless, we observed that these increments reached a maximum during the first year post-surgery, showing a clear trend to decrease during the second year and over, even when the values may not reach pre-surgical concentrations. In this sense, the decline observed in bone markers after 1 year could be an artifact due to the combination of samples to establish the time intervals. However, this decreasing trend was consistently observed regardless of the type of surgical procedure, suggesting true time-dependent changes unrelated to the degree of surgery-induced malabsorption. In this sense, the trend to “normalize” bone markers is possibly related to the stabilization of weight loss after 1 to 2 years in these patients and is consistent with previous observations [10, 20].
Oxidative stress may increase bone resorption through activation of nuclear factor-kappa β, and it has been pointed out that oxidative stress can activate bone resorption and deactivate bone formation [15]. Also, increased serum 8-iso-PGF2α levels (a marker of in vivo oxidative stress) has been associated with a lower bone mass and reduced serum bone alkaline phosphatase and osteocalcin concentrations, supporting a possible role for oxidative stress in the development of lower bone mass [14]. Thus, as previously observed [24], the chronic low levels of tocopherols and provitamin A carotenoids (which may display antioxidant activities) observed in these patients (especially after BPD) compromise their availability to tissues and reduce the fat-soluble antioxidant capacity, constituting an additional risk factor for other clinical conditions (i.e., osteoporosis). In this context, gamma-tocopherol displays several biological activities (including antioxidant and anti-inflammatory) [25], and in the present study, it showed significant inverse correlations with bone formation markers (P1NP and osteocalcin). Nevertheless, correlations should be cautiously interpreted as they may only reflect parallel but independent effects rather than related phenomena. Similarly, in the present study, the lack of associations between carotenoids (i.e., β-cryptoxanthin) and bone turnover markers does not necessarily indicate the absence of an effect on bone metabolism since such an effect may be present above certain threshold in serum [12] or upon supplementation with that carotenoid [13]. In addition, the low diagnostic specificity and sensitivity of some parameters as bone remodeling indicators (i.e., total alkaline phosphatase) may also contribute to the lack of correlation with other bone turnover markers.
Finally, bariatric surgery leads to significant changes (i.e., reduction in body weight, total and LDL cholesterol) sufficient to modify comorbidities [21], but a higher incidence of osteoporosis and higher risk of pathological fracture after malabsorptive surgery is well-known [1, 2]. Regardless of the surgical procedure used, after obesity surgery, there is a significant decrease in serum levels of retinol, α- and γ-tocopherol, β-carotene, and β-cryptoxanthin with a consistent increase in bone turnover markers over the first year, with a trend to decrease afterward. Thus, in addition to the nutritional assessment, regular monitoring of bone turnover markers seems to be necessary in these patients, and the early introduction of preventive strategies (i.e., the use of antiresorptive agents) should be evaluated.
References
Elder K, Wolfe BM. Bariatric surgery: a review of procedures and outcomes. Gastroenterology. 2007;132:2253–71.
Ledoux S, Msika S, Moussa F, et al. Comparison of nutritional consequences of conventional therapy of obesity, adjustable gastric banding and gastric bypass. Obes Surg. 2006;16(8):1041–9.
Aasheim ET, Bjorkman S, Sovik TT, et al. Vitamin status after bariatric surgery: a randomized study of gastric bypass and duodenal switch. Am J Clin Nutr. 2009;90:15–22.
Ernst B, Thurnheer M, Schmid S, et al. Evidence for the necessity to systematically assess micronutrient status prior to bariatric surgery. Obes Surg. 2009;19:66–73.
Coates PS, Fernstrom JD, Fernstrom MH, et al. Gastric bypass surgery for morbid obesity leads to an increase in bone turnover and a decrease in bone mass. J Clin Endocrinol Metab. 2004;89:1061–5.
Giusti V, Gasteyger C, Suter M, et al. Gastric banding induces negative bone remodelling in the absence of secondary hyperparathyroidism: potential role of serum C telopeptides for follow-up. Int J Obes (Lond). 2005;29:1429–35.
von Mach NA, Stoeckli R, Bilz S, et al. Changes in bone mineral content after surgical treatment of morbid obesity. Metabolism. 2004;53:918–21.
Cummings SR, Nevitt MC, Browner WS, et al. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995;332:767–73.
Nguyen ND, Pongchaiyakul Ch, Center JR, et al. Abdominal fat and hip fracture risk in the elderly: the Dubbo Osteoporosis Epidemiology Study. BMC Musculoskelet Disord. 2005;6:11. doi:10.1186/1471-2474-6-11.
Balsa JA, Botella.Carretero JI, Peromingo R, et al. Chronic increase of bone turnover markers after biliopancreatic diversion is related to secondary hyperparathyroidism and weight loss. Relation with bone mineral density. Obes Surg. 2010;20(4):468–73.
Högström M, Nordström A, Nordström P. Retinol, retinol-binding protein 4, abdominal fat mass, peak bone mineral density, and markers of bone metabolism in men: the Northern Osteoporosis and Obesity (NO2) Study. Eur J Endocrinol. 2008;158:765–70.
Sahni S, Hannan MT, Blumberg J, et al. Inverse association of carotenoid intakes with 4-y change in bone mineral density in elderly men and women; The Framingham Osteoporosis Study. Am J Clin Nutr. 2009;89:416–24.
Yamaguchi M, Igarashi A, Morita S, et al. Relationship between serum β-cryptoxanthin and circulating bone metabolic markers in healthy individuals with the intake of juice (Citrus unshiu) containing β-cryptoxanthin. J Health Sci. 2005;51(6):738–43.
Mangiafico RA, Malaponte G, Pennisi P, et al. Increased formation of 8-iso-prostaglandin F2α is associated with altered bone metabolism and lower bone mass in hypercholesterolaemic subjects. J Int Med. 2007;261(6):587–96.
Östman B, Michaëlsson K, Helmersson J, et al. Oxidative stress and bone mineral density in elderly men: antioxidant activity of alpha-tocopherol. Free Rad Biol & Med. 2009;47:668–73.
Granado-Lorencio F, Olmedilla-Alonso B, Herrero-Barbudo C, et al. Simultaneous determination of vitamins A, E and 25-OH-vitamin D application in clinical assessment. Clin Biochem. 2006;39(2):180–2.
Mahdy T, Atia S, Farid M, et al. Effect of Roux-en Y gastric bypass on bone metabolism in patients with morbid obesity: Mansoura experiences. Obes Surg. 2008;18(12):1526–31.
Bruno C, Fulford AD, Potts JR, et al. Serum markers of bone turnover are increased at six and 18 months after Roux-en-Y baroatric surgery: correlation with the reduction of leptin. J Clin Endocrinol Metab. 2010;95(1):159–66.
DiGiorgi M, Daud A, Inbnet WB, et al. Markers of bone and calcium metabolism following gastric bypass and laparoscopic adjustable gastric banding. Obes Surg. 2008;18(9):1144–8.
Fleischer J, Stein EM, Bessler M, et al. The decline in hip bone density after gastric bypass surgery is associated with extent of weight loss. J Clin Endocinol Metab. 2008;93(10):3725–40.
Riedl M, Vila G, Maier C, et al. Plasma osteopontin increases after bariatric surgery and correlates with markers of bone turnover but not with insulin resistance. J Clin Endocrinol Metab. 2008;93:2307–12.
Tsiftsis DD, Mylonas P, Mead N, et al. Bone mass decreases in morbidly obese women after long-limb biliopancreatic diversion and marked weight loss without secondary hyperparathyroidism. A physiological adaptation to weight loss? Obes Surg. 2009;19(11):1497–503.
Valderas JP, Velasco S, Solari S, et al. Increase of bone resorption and the parathyroid hormone in postmenopausal women in the long-term after Roux-en-Y gastric bypass. Obes Surg. 2009;19(8):1132–8.
Granado-Lorencio F, Herrero-Barbudo C, Olmedilla-Alonso B, et al. Hypocarotenemia in bariatric surgery: a preliminary approach on this potential risk factor. Obes Surg. 2009;19(7):879–83.
Jiang Q, Christen S, Shigenaga MK, et al. gamma-Tocopherol, the major form of vitamin E in the US diet, deserves more attention. Am J Clin Nutr. 2001;74:714–22.
Acknowledgments
This work has been partially funded by Ministerio de Ciencia e Innovación (AGL-2008-02591-C02-02-ALI), Spain.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Granado-Lorencio, F., Simal-Antón, A., Salazar-Mosteiro, J. et al. Time-Course Changes in Bone Turnover Markers and Fat-Soluble Vitamins After Obesity Surgery. OBES SURG 20, 1524–1529 (2010). https://doi.org/10.1007/s11695-010-0257-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-010-0257-1