Abstract
Summary
Despite effective weight reduction, the impact of bariatric surgery on bone is a major concern. Mechanisms include decreased mechanical loading, calcium and vitamin D malabsorption, deficiency in other nutrients, and alterations in fat- and gut-derived hormones. The evidence to support clinical care pathways to prevent bone loss and fractures is at this point weak.
Introduction
There is a growing concern regarding the potential deleterious impact of bariatric surgery on bone metabolism. This comprehensive review addresses this controversial topic.
Methods
We reviewed and analyzed articles evaluating bone metabolism and mechanisms for the ensuing putative bone loss in adult patients exclusively undergoing Roux-en-Y gastric bypass (RYGB) surgery, for the period spanning 1942 till September 2012.
Results
Mechanisms identified to contribute to alterations in bone metabolism after bypass surgery include: decreased mechanical loading, calcium and vitamin D malabsorption with secondary hyperparathyroidism, deficiency in other nutrients, in addition to alterations in adipokines, gonadal steroids, and gut-derived hormones favoring bone loss, with the exception of serotonin and glucagon-like peptide-1. The relative contribution of each of these hormones to changes in bone homeostasis after bypass surgery remains undefined. Bone loss reflected by a decline in bone mineral density (BMD) and an increase in bone turnover markers have been reported in many studies, limited for the most part by the exclusive use of dual energy X-ray absorptiometry. Well-designed long-term prospective trials with fractures as an outcome, and studies investigating the magnitude, reversibility, and impact of the observed metabolic changes on fracture outcomes are lacking.
Conclusion
Robust conclusions regarding bone loss and fracture outcome after RYGB surgery cannot be drawn at this time. Although not evidence based, baseline evaluation and sequential monitoring with measurement of BMD and calciotropic hormones seem appropriate, with adequate calcium and vitamin D replacement. Beneficial interventions remain unclear.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of obesity is dramatically rising; 35.7 % of US adults from the NHANES 2009–2010 population were found to be obese [1]. Estimates from the World Health Organization (WHO) project that by 2015, around 2.3 billion adults will be overweight and more than 700 million will be obese [2]. Unfortunately, diet therapy and medical management have limited success in the treatment of morbid obesity. Bariatric surgery has proven to be the only effective long-term treatment option for weight reduction, resulting, in addition, to improvements or complete remission of associated co-morbidities. In a meta-analysis including 22,904 patients, bariatric surgery resulted in a mean weight loss of 61 %, with substantial improvement in several co-morbidities including diabetes, hyperlipidemia, hypertension, and obstructive sleep apnea [3]. Many other conditions including infertility, menstrual irregularities, nonalcoholic liver disease, pseudo tumor cerebri, degenerative joint disease, and cardiovascular disease, can also be ameliorated or even resolve after bariatric surgery [4].
Although obesity has long been considered a protective factor for bone disease, concomitant vitamin D deficiency and elevated parathyroid hormone (PTH) levels, mediators of bone loss, are common findings in obese individuals. However, unlike other obesity-related co-morbid conditions, vitamin D deficiency and secondary hyperparathyroidism are not corrected after bariatric surgery, and may even be exacerbated by the malabsorptive state that often ensues. In addition, a negative impact of bariatric surgery on bone metabolism could also be explained by a decrease in the mechanical loading and subsequent reduction in osteoblast differentiation, and by the resulting hormonal changes produced by changes in the adipose tissue mass and in the normal anatomy and physiology of the gastrointestinal tract.
RYGB is currently one of the most commonly performed, and is considered by many surgeons as the “gold standard” procedure [5]. Studies investigating the impact of RYGB surgery on bone metabolism have demonstrated a decrease in calcium absorption, secondary hyperparathyroidism, accelerated bone loss, and enhanced risk for skeletal fragility [6]. However, the mechanisms by which RYGB surgery affect bone integrity has not been fully elucidated. In this paper, we will present a comprehensive review of the potential factors that impact bone metabolism at baseline in obese subjects and post-RYGB procedure.
Methodology for literature search
A PubMed search was conducted from the period of 1946 until September 2012 using the search terms: “adipokines”, “adiponectin”, “amylin”, “bariatric surgery”, “BMD”, “bone loss”, “bone markers”, “calciotropic hormones”, “estradiol”, “fractures”, “ghrelin”, GLP-1”, “glucose-dependent insulinotropic polypeptide (GIP)”, “gut hormones”, “insulin”, “leptin”, “neuropeptides”, “obesity”, “peptide YY (PYY)”, “RYGB”, “secondary hyperparathyroidism”, “serotonin”, “testosterone”, and “vitamin D.” The above terms were used in mixed combinations. Boolean operators and truncations were used to expand our search results, and only English articles were selected. Our search yielded 526 articles that were screened by abstract and title and the most relevant studies were selected for inclusion in the review. Studies reporting on changes in calciotropic hormones only, studies in adolescents, or studies including restrictive procedures or other malabsorptive procedures were excluded. Thirty-one cross-sectional and prospective studies published until September 2012 assessing bone markers, and/or BMD in adult patients undergoing RYGB were identified; of which 16 studies exclusively reporting on RYGB in adults, were retained. The results of these 16 studies, including five cross-sectional and 11 prospective studies, were reviewed in detail and summarized in Table 2.
References from the retrieved articles, and publications available in the authors’ libraries and three suggested by journal reviewers were also used.
For a review regarding the mechanisms of actions for the main relevant hormones and their changes post-RYGB, the most comprehensive and/or recent reference was used in view of the limit on the number of references allowed.
RYGB surgery and gut hormones
RYGB surgery is a combined malabsorptive and restrictive procedure that diverts food from a large portion of the stomach and the proximal small intestine into the distal small intestine. It consists of creating a small gastric pouch connected to the small intestine via a Roux-en-Y configuration as shown in Fig. 1. The Roux limb is anastomosed to the gastric pouch and connected downstream to the biliopancreatic limb; the latter conduct biliary and pancreatic secretions. The lengths of the Roux limb and the biliopancreatic limb can be adjusted to determine the degree of malabsorption [7]. With these changes in the anatomy of the gastrointestinal tract, a substantial alteration in the secretion of several gut hormones ensues. These hormones are involved in appetite regulation, energy balance, and glucose homeostasis as well. Alterations in these hormones contribute to the resulting metabolic benefits seen after RYGB surgery. In addition, an effect of these changes in gut peptides on bone metabolism have been demonstrated as well (Fig. 2). The next section follows a detailed review of individual gut hormones, their known impact on bone metabolism, changes in levels after RYGB surgery, and the anticipated or known effect of such a change on bone as summarized in Table 1.
Gut hormones and impact on bone. Changes in gut hormones post-RYGB (blue arrows) and impact on bone (red signs). GIP glucose-dependent insulinotropic polypeptide secreted by K cells in proximal small bowel, GLP-1 glucagon-like peptide-1 secreted by L-cells of the distal ileum and the colon, PYY peptide YY secreted by L cells of the distal ileum and colon. Ghrelin secreted by X-A like cells of the stomach, serotonin secreted by entero-chromaffin cells in the duodenum, amylin and insulin secreted by pancreatic β cells. RYGB: Roux-en-Y gastric bypass. References describing above are provided in the text
Neuroendocrine/gut hormones and bone
Peptide YY
Peptide YY (PYY) is a 36-amino acid peptide produced by the enteroendocrine L-cells of the terminal ileum and colon, and reduces appetite and food intake [8]. PYY has also been shown to influence bone metabolism as well. It circulates in two forms PYY1–36 and PYY3–36, both of which bind to the hypothalamic NPY Y2 receptor with high affinity [9, 10].
It has been reported to circulate in lower levels in obese subjects [11], and obese subjects with lower levels of PYY [10] had a higher BMD [12]. High levels of PYY were found in anorexic female adolescents and were associated with low levels of bone turnover markers [13]. Amenorrheic anorexic athletes had higher PYY levels and lower bone density compared to eumenorrheic control athletes and furthermore, PYY was also found to be a negative predictor of PINP, a bone formation marker, and of lumbar bone mineral apparent density Z-scores in adolescent athletes [14]. The above data suggest a negative correlation between PYY and bone formation. In animal models, conflicting data has been reported on PYY knockout mice. Baldock et al. showed that Y2 receptor knockout mice exhibited a twofold increase in cancellous bone volume [15], suggesting a central hypothalamic inhibitory influence on bone. Similarly, Wong et al. reported that PYY knockout mice displayed an increased bone mass phenotype [16]. In contrast, Wortley demonstrated a decrease in BMD and bone mineral content (BMC) and a reduction in bone strength in PYY-deficient mice [17]. The conflicting findings in animal models warrant further investigation into the effect of PYY on bone metabolism.
RYGB surgery has been associated with an increase in PYY levels [18] and since human data support a negative relationship between PYY and bone; a potential negative impact on bone mass would be anticipated. However, to our knowledge, no studies have yet assessed the changes in PYY levels after RYGB surgery, and their relationship to bone remodeling and density.
Glucose-dependent insulinotropic polypeptide
Another gut hormone affecting bone homeostasis is GIP. GIP is a 42-amino acid gastrointestinal peptide secreted by the K cells in the proximal small bowel. Elevated levels of GIP have been found in obese subjects [19].
In vitro, exogenous GIP showed an anti-apoptotic effect on mouse and human osteoblasts [20]. Bollag et al. reported an increase in intracellular cAMP and calcium and stimulation of alkaline phosphatase activity and collagen type 1 synthesis in osteoblast-like cell lines treated with GIP, reflecting an increase in bone formation [21]. Furthermore, GIP was found to have an inhibitory effect on osteoclast-resorptive activity [22]. Daily administration of GIP in ovariectomized Sprague–Dawley rats reduced the rate of estrogen-deficiency-induced bone loss [23]. In addition, mice lacking GIP receptors had decreased osteoblastic bone formation and increased osteoclastic bone resorption [20, 24]. These data suggest that GIP, a gut-released peptide, plays a direct role in the modulation of bone formation. One clinical study evaluated GIP levels in young women with anorexia nervosa and found no correlation between GIP and BMD in those women [25].
Bypassing the duodenum and part of the jejunum in the RYGB surgery is expected to result in a decrease in GIP secretion. Studies investigating changes in GIP post-RYGB surgery reported a decrease for the most part, a change that would be expected to negatively affect bone, but inconsistencies have been noted [26]. However, studies evaluating changes in GIP after RYGB surgery in correlation with changes in bone mass are lacking.
Ghrelin
Ghrelin is a 28-amino acid orexigenic gut peptide secreted by X/A like cells of the gastric mucosa. Its levels are increased pre-prandially and suppressed after meals [27]. Lehto-Axtelius et al. initially proposed that loss of oxyntic mucosa is mainly responsible for gastrectomy-induced osteopenia [28]. Ghrelin stimulates the release of growth hormone (GH) via binding to growth hormone secretagogue receptor (GHS-R). Since GH is well known to enhance bone formation, therefore ghrelin may play a role in bone metabolism via the GH/IGF-1 axis [29]. Indeed, ghrelin’s direct action on bone was further confirmed by Fukushima et al. who reported an increase in BMD in GH-deficient rats treated with a 4-week intraperitoneal ghrelin infusion [30]. In vivo, ghrelin has been also shown to enhance osteogenesis of intramembranous bone and stimulate new bone formation in calvarial bone defects in rats [31]. Furthermore, many in vitro studies have demonstrated the effects of ghrelin on bone cells. Ghrelin enhanced proliferation and differentiation of osteoblast cell lines in both rats and humans and repressed apoptosis of osteoblastic cells in rats [30, 32]. In humans, studies on the association of ghrelin with BMD and bone markers have led to conflicting results, both in adults and children. Biver et al. found no convincing data to support an association between ghrelin and BMD. Differences in study population, gender, body mass index (BMI), bony sites assessed, and ghrelin sampling assay could partially explain the discrepancies between the studies. In addition, an age-dependent effect of ghrelin on bone has been more recently evoked that could also explain the inconsistencies [33].
Since RYGB surgery consists of reducing the stomach to a small gastric pouch, ghrelin produced by the gastric fundus, is expected to be reduced after surgery. This has been confirmed by Cummings et al. who demonstrated a profound suppression of ghrelin after RYGB [34], findings confirmed by several other studies. Conversely, increased or unchanged ghrelin levels following RYGB were also observed [35]. This inconsistency in the obtained results have been explained by different surgical techniques including variable pouch configuration [36], and possible iatrogenic vagal nerve dysfunction as has been demonstrated in the study by le Roux et al. [37]. Heterogeneity in the populations studied, differences in postoperative improvements [38], as well as variability in plasma ghrelin assays could also explain this inconsistency. If RYGB results in decrease in ghrelin level, a negative effect on bone metabolism would be anticipated, based on animal studies.
Glucagon-like peptide-1
Glucagon-like peptide-1 (GLP-1), a 30-amino acid peptide secreted by the L-cells of the distal ileum and the colon, stimulates insulin secretion and ameliorates beta cell function [39, 40]. It has been shown to affect bone metabolism as well. Initially, Yamada published that GLP-1 lacked any direct effect on osteoblasts and osteoclasts but resulted in increased bone resorption via a calcitonin-dependent pathway [41]. However, more recently, Nuche-Berenguer et al. demonstrated that GLP-1 can directly influence osteoblastic cells through a GPI/IPG-coupled receptor different than the pancreatic cAMP-linked GLP-1 receptor [42]. Furthermore, an insulin and PTH-independent bone osteogenic effect of GLP-1 has been demonstrated in insulin-resistant and type 2 diabetic rat models, after a continuous 3-day infusion [43]. In humans, a 44-week treatment of exenetide did not affect BMD and markers of bone metabolism despite a significant weight reduction [44].
Many investigators observed increased GLP-1 levels after RYGB [18]. The resulting increase in GLP-1 is expected to positively influence bone metabolism. Data correlating the increase in GLP-1 after RYGB with changes in bone metabolism is lacking.
Amylin
Amylin, a 37-amino acid hormone co-secreted with insulin by the pancreatic beta cells, circulates at higher levels in obese people, suggesting a state of amylin resistance [45]. Amylin has been shown to affect both bone resorption and bone formation through its action both on osteoblasts and osteoclasts, as demonstrated in animal models and cell cultures. Amylin was shown to stimulate both human [46] and rodent [47] osteoblast proliferation and activity, to inhibit osteoclast development in mouse bone marrow cultures, and to reduce the activity of mature osteoclasts via increases in intracellular cyclic AMP concentration [48, 49]. In addition, a reduction in both basal and PTH hormone-stimulated bone resorption was demonstrated in neonatal mouse calvariae treated with amylin [50]. Systemic administration of amylin improved bone mass by inhibiting resorption and stimulating formation in adult male mice [51]. Amylin-deficient mice displayed a low bone mass phenotype secondary to an increase in bone resorption [52]. In human studies, Wojcik recently reported a positive association between fasting amylin and BMD at the PA spine, total hip, and femoral neck in 15 women with anorexia nervosa. This association persisted for femoral neck and total hip after controlling for percent body fat [25]. Furthermore, amylin deficiency may contribute to the impaired bone formation seen in type 1 diabetics [53]. Interestingly, amylin analogues are currently under development as potential anti-osteoporotic agents [54].
Few data has been reported on the changes in amylin levels after RYGB surgery. Male Sprague–Dawley obese rats showed significant reduction in plasma amylin levels after RYGB surgery [55]. While short-duration studies up to 4 weeks post-RYGB reported no change in amylin levels [56, 57], a decrease was reported by Bose el al. in a study of eleven morbidly obese diabetic women, at 1 month that remained unchanged at 12 months after RYGB [58]. Weight loss post-RYGB surgery, would be expected to result in a decrease in amylin, and to thus negatively influence bone metabolism.
Insulin
Insulin is a 53-amino acid hormone secreted by the beta cells of the pancreas. Both anabolic and catabolic effects of insulin on bone have been described. The exact mechanisms underlying the anabolic effect remain unclear [59]. Insulin has been shown to promote osteoblast proliferation and differentiation via MAPK and PI3K pathway in MG-63 cells [59]. In addition, the anabolic action of insulin on bone could be mediated indirectly through IGF-1 receptors [60]. Hyperinsulinemia also results in an increase in free androgen levels that have been shown to positively impact bone in women [61]. Furthermore, Thomas et al. demonstrated the presence of insulin receptors on osteoclasts that could mediate the inhibitory effect of insulin on bone resorption in vitro [62]. Conversely, insulin signaling in human osteoblasts favored bone resorption by reducing the ability of osteoblasts to produce osteoprotegerin and resulted in an increase in undecarboxylated osteocalcin [63]. Insulin resistance and hyperinsulinemia are associated with an enhanced free fatty acid levels which are known to modulate osteoclastogenesis [64]. A positive correlation between circulating insulin levels and bone density has been shown in several clinical studies independent of BMI and fat mass [65].
After RYGB surgery, a reduction in insulin levels have been observed [18], and the expected consequence would therefore be a negative effect on bone mass. However, further studies are needed to better define the potential role of insulin in regulation of bone metabolism in humans.
Serotonin
Over 90 % of the body’s serotonin is synthesized by the enterochromaffin cells within the gastrointestinal tract. Circulating peripheral serotonin acts as a hormone to inhibit bone formation, while brain derived serotonin acts as a neurotransmitter favoring bone mass accrual [66]. Yadav et al. have demonstrated that the expression of the rate-limiting enzyme in the biosynthesis of serotonin, tryptophan hydroxylase 1 (Tph1), is inhibited by LDL-receptor-related protein 5 (LRP5) [67]. Loss of function mutations in LRP5 were identified to play a central role in the pathophysiology of osteoporosis in pseudoglioma syndrome [68], while gain of function mutations result in a high bone mass phenotype [69]. Paracrine signaling through the Wnt pathway has been suggested as the implicated mechanism; however, this is not widely accepted. Reducing serotonin blood levels by a low tryptophan diet normalized bone formation and bone mass in Lrp5 knockout mice [67]. A study in postmenopausal women, not on hormonal therapy, revealed a negative correlation between serum serotonin levels and bone density [70]. In addition, patients treated with SSRI displayed enhanced bone loss, decreased bone mass, and an increased risk for fractures [71].
We were unable to identify any studies investigating alterations in serotonin levels after RYGB surgery. However, by excluding the duodenum in RYGB, serotonin levels are expected to decrease, and thus would eliminate the negative effect of gut-derived serotonin on bone. Indeed, of all concerned hormones with RYGB (Fig. 2), serotonin and GLP-1 are the only known hormones so far whose altered secretion and levels post-RYGB would be anticipated to positively affect bone homeostasis.
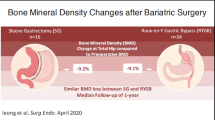
Effect of RYGB on bone markers, BMD, and fractures
Among the different bariatric surgeries, malabsorptive surgeries including RYGB surgery have shown the most substantial adverse effects on bone metabolism compared to purely restrictive surgeries [72–75].
Significant increments in serum and urinary N-telopeptide, C-telopeptide, and serum osteocalcin have been consistently reported in patients after RYGB surgery, and are summarized in Table 2 [76–80]. These increments vary widely between studies, ranging between 29 and 319 %, and have been observed as early as 3 months after surgery [76] and persisted at 18 months post-surgery [78], regardless of calcium and vitamin D supplementation.
In all retrospective studies reported herein, no significant difference in femoral neck BMD was observed in patients up to 10 years after RYGB surgery compared to overweight controls [81], and to body mass index matched controls [82, 83]. However, as shown by Beck et al., patients with a greater BMI have more robust femur geometry and thus a higher hip BMD [84]. Similarly, cross-sectional and retrospective studies reported similar or greater bone density at the lumbar spine, total body, and radius in subjects post-bariatric surgery compared to controls [76, 81–83, 85]. However, in view of the cross-sectional design of the studies, the small number of patients, and the heterogeneity of the population included, no robust conclusions could be drawn.
Prospective studies assessing changes in BMD up to 3 years [86] after RYGB surgery in men, and women in various menopausal stages, are detailed in Table 2. The greatest reduction in BMD was noted in the hip region including the trochanter [76], femoral neck [79, 87, 88], and total hip [86, 89], with losses ranging from 9 to 11 %. While two studies showed no significant change in lumbar spine BMD after RYGB surgery [79, 82], the remaining three studies reported a decline, that varied from 3 to 7 % at 9–12 months [76, 87, 88], and an additional 3 % decrement in one of the studies at 3 years [86] (Table 2). Bone density changes at the distal radius after RYGB surgery were evaluated in two studies with conflicting results [79, 82]. While Fleischer et al. reported no significant BMD change at the radius 12 months after RYGB surgery, Goode et al. reported a decrease in ultradistal radius BMD despite a 6 months supplementation of calcium and vitamin D. Similarly, total body BMD either showed no change [87] or decreased [89, 90] by less than 3.2 % up to 1 year following RYGB. Therefore, prospective studies show that bone density continues to decline after the first postoperative year, even after maximal weight loss has been achieved, as observed in one study [86]. However, the greater decline in bone density at the hip, a weight-bearing site, may be in part due to the decreased loading of the skeleton after weight reduction. More importantly, the reported decrements in bone mass by dual energy X-ray absorptiometry (DXA) should be interpreted with caution in view of issues of reproducibility [91], as well as possible confounding from artifacts due to loss of fat and soft tissue. Extreme obesity and excess fat reduce the accuracy of DXA measurements, resulting in an erroneous estimation of the actual decreases in bone density following substantial weight reduction [20]. Indeed, this was reflected by a reduction in total bone area in addition to the decrease in BMD and BMC after RYGB surgery which is highly suggestive of technical artifact such as fat loss [90]. Measurement of skeletal sites with less fat overlay, such as the forearm, is less likely to be prone to measurement errors as compared to others with more surrounding fat, such as the spine [91, 92]. Studies evaluating the effects of fat simulation on BMD measurements by DXA have reported under- or overestimation in BMD values, depending on the DXA scanner model and software used [93, 94]. Another limitation is the difficulty faced by technicians in positioning obese subjects within the scan area [95], and variability in positioning of the fat panniculus affecting accuracy of BMD measurements at the hip. Limitations of the prospective studies are their limited number, the small number and heterogeneity of study subjects, and the fact that all but one [82] lacked a control group.
Studies evaluating fracture as an outcome post-bypass surgery are scarce. One retrospective uncontrolled study evaluated the incidence of falls and fractures after RYGB in 167 individuals via a telephone survey who underwent RYGB for morbid obesity. The mean age of the participants was 47 years; the majority were women who experienced a mean weight loss of 127 lbs. Of the participants, 5 % reported postoperative fractures involving wrists, arms, ankles, thumbs, and toes, and 8 % reported a new diagnosis of osteoporosis or osteopenia during a mean postoperative interval of 2.4 years. One third reported a history of one or more falls postoperatively [96]. Another recent retrospective controlled cohort study, taking advantage of the General Practice Research database, included all bariatric surgery techniques and among which RYGB accounted for 29 % of the surgeries performed. While there was no increased risk of fracture at a mean follow-up of 2.2 years in patients after bariatric surgery compared with controls, the authors report a trend towards an increased fracture risk after 5 years, and in patients who had the greatest reduction in body weight [97]. The numbers were 1.19 % fractures/person-years in the surgical group and 0.91 % fractures/person-years in the control group, P value was not significant. Similarly, the adjusted relative risk for any fractures in those who experienced an excess weight loss greater than 50 % was 1.46 [0.55–3.85], P value was not significant. In rats that underwent gastro-jejunal bypass, a reduction in cortical as well as trabecular BMD, and a deterioration in bone quality, as assessed by X-ray microtomography, were observed, thus suggesting true bone loss [26]. Such CT-based studies that would help elucidate the relative contribution of artifactual changes of bone density by DXA on true bone loss, if any, are lacking in humans. In addition, evidence of fragility through fracture occurrence is also missing.
Other factors implicated in changes in bone metabolism after RYGB surgery
Several factors, besides changes in gut hormones, have been implicated in bone loss after RYGB surgery including decreased mechanical loading, malabsorption, and changes in adipose tissue and its hormones (Fig. 3). The impact of each on the regulation of bone turnover before and after bariatric surgery, and their effect on bone, are reviewed in detail.
Pathways for bone loss after RYGB surgery. Details for the effect of each hormone provided in Table 1 and in the text. GIP glucose-dependent insulinotropic polypeptide, GLP-1 glucagon-like peptide-1, PTH parathyroid hormone, RYGB Roux-en-Y gastric bypass
Decreased mechanical loading
Mechanical loading of bone has recently been shown to decrease sclerostin gene (SOST) expression in osteocytes leading to a significant reduction in sclerostin levels [98]. Sclerostin antagonizes the Wnt/β catenin signaling pathway implicated in osteoblast differentiation and function, and thus negatively regulates bone formation [99]. Weight loss decreases mechanical loading, and would be anticipated to increase SOST, and thus to cause bone loss. Such pathway could at least partially explain the bone loss associated with the dramatic weight reduction after bariatric surgery. Studies evaluating changes in sclerostin with surgically induced weight loss are lacking. However, diet-induced weight loss of 9.6 ± 1.2 % in obese older adults was associated with a significant increase of sclerostin levels of 6.6 ± 1.7 % and 10.5 ± 1.9 % at 6 and 12 months, respectively, increments that were prevented by exercise training [100]. Sclerostin antibody drug molecules are currently being tested in phase II and III trials in postmenopausal osteoporosis and such drugs may provide an attractive strategy for the prevention and treatment of bone loss after weight reduction surgeries.
Calciotropic hormones
Changes in calciotropic hormones after RYGB surgery
Circulating serum 25 hydroxy-vitamin D, 25(OH)D, is the most appropriate marker of vitamin D nutritional status. A large number of studies report a low level of circulating 25(OH)D in obese individuals with a prevalence ranging from 21 to 90 %. This large proportion could in part also be due to a decreased bioavailability of vitamin D as a result of its sequestration in excess adipose tissue and from lower sun exposure related to a more sedentary lifestyle and a tendency to be overdressed [101, 102]. As opposed to other obesity-related complications, vitamin D deficiency, and secondary hyperparathyroidism if present preoperatively, are not corrected, and may even be exacerbated, after bariatric surgery. However, the impact of bariatric surgery on vitamin D levels remains controversial. Vitamin D deficiency states were not significantly altered after RYGB surgery in some studies [80, 103, 104] while others demonstrate a fall in 25(OH)D levels that progressed over time [86, 105]. At 3 years after RYGB surgery, mean 25(OH)D levels in 59 morbidly obese women decreased from a baseline of 55.3 to 37.9 nmol/l despite calcium and vitamin D supplementation [86].Though the skin remains the predominant source of vitamin D accounting for more than 80 % of circulating vitamin D, dietary intake may also play a role [106]. A few studies reported an increase in postoperative vitamin D levels after 6 months in subjects supplemented with calcium and vitamin D [78, 82]. After 18 months of RYGB surgery, 25(OH)D levels increased significantly from a mean of 17.7 to 25.6 ng/ml however remained in the insufficient range, if one considered the norms defined by the International Osteoporosis Foundation and by the Endocrine Society [78, 107, 108]. The prevalence of vitamin D deficiency varied from 7–51 % in different studies depending on the vitamin D supplementation, the type of surgery, and duration of follow-up [109]. It is noteworthy to mention that the high prevalence of hypovitaminosis D reported at baseline or post-RYGB surgery, in part reflects the variable definitions and cut-offs used to define vitamin D deficiency (for e.g., 25(OH) < 20 ng or < 30 ng/ml), type of assay used, diet, and lifestyle of study subjects, in addition to the geographic latitude of the countries where the studies were conducted. Several studies have shown a positive association of obesity with increased levels of serum PTH [101, 110–113]. Post-bariatric surgery, further increments in PTH levels have been reported in up to 53 % of patients [105, 114, 115]. This could be explained by a postoperative depletion in vitamin D and calcium secondary to reduced intake and malabsorption. When the true fractional excretion of calcium absorption (TFCA) was measured following a calcium load, a significant decrease in TFCA of 34 % was noted in 21 women 6 months after RYGB as compared to baseline [77]. Patients may also develop magnesium depletion postoperatively with resulting skeletal resistance to PTH effect [116]. However, decrements in serum Mg levels after bypass surgery have not been consistently reported across studies [82, 114, 117]. The fact that serum magnesium level is a poor predictor of intracellular and total body magnesium stores may underestimate magnesium deficits, and thus explain those discrepancies. Nevertheless, secondary hyperparathyroidism due to calcium and vitamin D malabsorption cannot by itself explain the bone loss observed after RYGB surgery. Weight loss per se, and the resulting decrease in fat mass, seem to play an important role in the pathophysiology of bone loss after bariatric surgery.
Other nutritional and micronutrients deficiencies
In addition to the above described alterations, multiple macronutrients and micronutrients deficiencies have been reported after RYGB surgery. Protein malabsorption is the major macronutrient deficiency described that would negatively impact bone. Indeed, a reduced dietary protein intake implies a negative effect on bone as noted by increased bone turnover markers and a rise in PTH with a low protein diet [118]. Additional micronutrient deficiencies include deficiencies in trace elements (chromium, copper, manganese, selenium, and zinc); essential minerals (iodide and iron); and water-soluble vitamins including thiamine, riboflavin, niacin, folic acid, pyridoxine, biotin, pantothenic acid, cobalamin, and vitamin C. In addition to vitamin D deficiency, deficiencies in other fat-soluble vitamins (A, E, and K) are also observed. Many of these micronutrients have been shown to support bone health although their exact contribution remains to be elucidated [119].
Adipokines and bone
Fat is an important organ that has been increasingly recognized to harbor hormones with a substantial impact on bone metabolism [120] (Fig. 4). One particular research group has systematically investigated the cross-talk between fat and bone over the last decade, and unraveled novel pathways between mineral and fuel metabolism [121, 122]. A number of adipokines including leptin, adiponectin, tumor necrosis factor-α (TNF-α), and interleukin-6 (IL-6), among others, appear to be involved in bone physiology. Conversely, bone-derived factors such as osteocalcin and osteopontin seem to also regulate glucose homeostasis. The two most studied adipokines to-date are leptin and adiponectin, and the impact of bariatric surgery on this bone–adipose axis remains to be delineated [65].
Leptin
Leptin, a 167-amino acid peptide primarily secreted by adipocytes, circulates at levels proportional to fat stores and regulates appetite and energy expenditure [123]. However, increased levels of leptin seen in obese individuals do not effectively suppress appetite because of an underlying resistance to the hormone [124]. In addition to its role in appetite, reproduction, and energy expenditure, leptin plays a role in bone physiology. Leptin receptors have been identified throughout the body including bone marrow stem cells, osteoblasts, and osteoclasts, and several in vitro studies have reported an anabolic effect of leptin on osteoblasts. Leptin was shown to promote proliferation of isolated fetal rat calvarial osteoblasts [125] and differentiation of human osteoblast precursor cells. It was also shown to stimulate matrix mineralization, and increase the production of osteoblast specific proteins such as osteocalcin, alkaline phosphatase, and of collagen type 1 [126–128]. An inhibitory effect of leptin on bone resorption has also been demonstrated, through inhibition of osteoclast generation from human peripheral blood mononuclear cells and osteoclast differentiation from mouse spleen cells [129]. This is consistent with findings of an inhibition of osteoclastogenesis in mouse bone marrow cultures [125]. This effect of leptin could be mediated by an increase in osteoprotegerin, and/or a decrease in RANK ligand levels [130]. Thus, findings from in vitro studies indicate that leptin could positively influence bone density by increasing bone formation and reducing bone resorption. However, in vivo studies have yielded contradictory results. Steppan et al. showed an increase in femoral length, total body bone area, bone mineral content, and bone density in ob/ob mice after administration of leptin intraperitonially [131]. Similarly, Cornish et al. showed an increase in bone strength of greater than 20 % in adult mice treated with subcutaneous leptin for 4 weeks [125]. Ovariectomized rats showed a decrease in trabecular bone loss when treated with continuous subcutaneous leptin [130]. Conversely, Ducy et al. showed that intra-cerebro-ventricular administration of leptin resulted in decreased bone formation and increased bone loss in ob/ob (deficient in leptin) and wt mice [132]. Takeda et al. reported that the central anti-osteogenic effect of leptin on bone may be mediated by the sympathetic nervous system through β2 receptors on osteoblasts since it was effectively blocked by propranolol [133]. In addition to its binding to hypothalamic receptors, leptin enhances sympathetic signaling by inhibiting serotonin release from the brainstem. Serotonin promotes bone formation and bone mass accrual by stimulating HTR2C receptors on neurons in the ventromedial hypothalamus [134]. Another mediator identified in leptin regulation of bone metabolism is the cocaine amphetamine regulated transcript (CART). Leptin increases CART that in turn decreases bone resorption by inhibiting RANK-ligand expression on osteoblasts in contrast to the antiosteogenic central effect on bone [135]. Therefore, leptin seems to regulate bone metabolism differentially, negatively through central pathways via the sympathetic nervous system and CART, and positively via a direct local peripheral effect on bone cells. Human studies assessing leptin’s effects on bone homeostasis have yielded controversial results. Some studies found a positive association between leptin and BMD including that from the large Rancho Bernardo Study [136–138], while others found no association between leptin and BMD [139] or bone turnover markers [140, 141]. The discrepancies in the reported results could be attributed to differences in the study populations, BMI, bone sites assessed, and lack of adjustments for bone-related factors. Furthermore, all of these were exclusively association studies.
Leptin circulates in proportion to body fat mass [142] and as expected, a decrease in leptin levels has been reported after RYGB surgery [18]. A decrease in peripheral leptin levels would be anticipated to result in a decrease in bone mass, if one considered its peripheral effects exclusively. Indeed, the reduction in leptin levels reported were highly correlated with the increase in serum N-telopeptide of type I collagen (NTX) at 6 and 12 months after RYGB surgery [78]. However, the ultimate effect of leptin on bone post-RYGB remains to be elucidated.
Adiponectin
Adiponectin, a 244-amino acid also produced by adipocytes that tends to circulate at lower levels in obese individuals [143]. Interestingly, in addition to its production by adipocytes, adiponectin is also secreted at low levels by bone-forming cells [144]. Besides its anti-inflammatory properties and its role in regulation of insulin sensitivity and fatty acid oxidation, adiponectin may also be involved in bone homeostasis [145]. Most but not all the association studies reported an inverse relationship between adiponectin and BMD. The reduced levels of adiponectin associated with obesity, and the inverse relationship between adiponectin and BMD could partially explain the protective effects of fat on bone. In a recent meta-analysis of 59 studies, most of which were cross-sectional, a total of 10,451 healthy men and women of variable menopausal status were sampled. Among the various adipokines assessed, including leptin, adiponectin, resistin, and ghrelin, adiponectin showed the highest negative association with BMD (pooled r from −0.14 to −0.4), a relationship that was independent of BMI, gender, and menopausal status [146]. However, in contrast to most clinical studies, adiponectin was shown to decrease osteoclastogenesis and activate osteoblastogenesis both in vivo and in vitro [147]. Adiponectin increased human osteoblast proliferation, enhanced matrix mineralization [148], and inhibited osteoclastogenesis in murine macrophage cell lines [149]. Conversely, and in line with clinical studies, adiponectin knockout mice displayed an increase in bone mass [145] and osteoprogenitor cell cultures treated with recombinant mouse adiponectin showed a decrease in osteogenesis [150]. Therefore, the effect of adiponectin on bone remains unclear. Post-RYGB surgery, an increase in adiponectin levels has been described and the impact of such an increment on bone remains to be clarified [18]. One study reported a significant association between the rise in adiponectin and the reduction in BMD at 12 months after RYGB [89] while another found no correlation between adiponectin and bone turnover markers [78] after surgery.
Gonadal steroids and bone
Gonadal steroids play a critical role in bone modeling, the attainment of peak bone mass [151], and bone remodeling afterwards. A reduction in estradiol and an increase in sex hormone binding globulin (SHBG), in free and total testosterone, are observed both after nonsurgical and surgical weight loss [152]. The impact of the changes in those hormones after bariatric surgery on the skeletal integrity of bone is however not well studied. Interestingly, besides the favorable action of bone on glucose metabolism and energy expenditure via osteocalcin, a similarly novel role in the regulation of reproductive function, mainly testosterone synthesis, has been described by the same group [153].
Estradiol
Estrogen is a major sex steroid for bone health, modulating bone growth and remodeling. An enhancing effect of estrogen on intestinal calcium reabsorption has been described in both experimental animals and humans [151]. In addition, estrogen reduces osteoclast formation and activity by enhancing the production of tumor growth factor-β (TGF-β) and osteoprotegerin (OPG), and decreasing the expression of RANK-ligand (RANK-L). Estrogen also enhances osteoclast apoptosis, by reducing the synthesis of cytokines such as interleukin 1 (IL-1), IL-6, TNF-α, and macrophage colony stimulating factor (M-CSF). The effect of estrogen on osteoblasts is less clear, with conflicting results [153] and is summarized in Fig. 5. Adipocytes are an important source of estrogens derived from aromatization. Whereas one study showed significant decrements in serum estradiol levels from112.27 ± 9.23 to 87.64 ± 7.92 pg/ml in 14 premenopausal women post-vertical banded gastroplasty [154]. We are unaware of any such study being conducted post-RYGB. Conversely, a reduction in estradiol levels was demonstrated in 64 severely obese men 2 years after such surgery [155]. In view of the established protective effect of estrogen on bone, the anticipated lower estrogen levels post-RYGB would increase bone remodeling.
Estrogen effect on mediators of bone metabolism. IL-1 interleukin 1, IL-6 interleukin 6, TNF-α tumor necrosis factor-α, M-CSF macrophage colony stimulating factor, TGF-β tumor growth factor-β, OPG osteoprotegerin, RANK-L receptor activator of nuclear factor kappa-B ligand. References describing above are detailed in text
Testosterone
Androgens also play a major role in maintaining skeletal homeostasis through several mechanisms. Intestinal calcium absorption is enhanced either directly or indirectly through a vitamin-D-mediated effect as demonstrated in prepubertal boys [156] and sexually maturing male rats [157]. A positive effect of androgens on calcium reabsorption by the kidney has also been suggested by some studies [158]. Furthermore, androgens stimulate osteoblast proliferation and differentiation and regulate various autocrine and paracrine cytokines involved in bone homeostasis, such as transforming growth factor-β, insulin-like growth factors, interleukin-6, and fibroblast growth factor. Furthermore, through the regulation of OPG production, androgens decrease osteoclast activity and hence bone resorption [153, 159] (Fig. 6). In addition, androgens protect against oxidative-stress-induced bone loss and promote bone strength by increasing muscle mass [159]. Obesity has been associated with altered sexual male function including erectile dysfunction, abnormalities in sperm parameters, and infertility that can be explained by obesity-associated hormonal changes [160, 161]. Obese men are described to be in a state of hypogonadotropic hyperestrogenic hypoandrogenemia, with decreased total and free testosterone, gonadotropin, and SHBG levels, and increased circulating estrogen levels [160]. Diet-induced weight loss and surgical weight loss have been associated with an increase in testosterone levels and an improvement in sexual function. An increase in total testosterone up to 101 % has been reported after RYGB compared to an increase of 37–57 % after nonsurgical weight loss [152]. Hammoud et al. reported a significant increase in total testosterone in 22 severely obese subjects 2 years after gastric bypass surgery by 310.8 ± 47.6 ng/dl vs. 14.2 ± 15.3 ng/dl in 42 obese controls, and an increase in free testosterone by 45.2 ± 5.2 pg/ml in subjects vs. 0.4 ± 3.0 pg/ml in controls [155]. Hence, the increase in androgen levels after bariatric surgery would be expected to positively influence bone metabolism. Indeed, a variation in serum-free testosterone levels within the normal range was an independent positive predictor of BMD and of prior osteoporosis-related fractures in older men [162].
Conclusion
RYGB surgery has been shown to have a major impact on bone metabolism secondary to the resulting malabsorption and the ensuing hormonal changes (Table 1). The mechanisms by which bariatric surgery affects bone metabolism and the contribution of the gut and fat hormones to bone integrity are not well elucidated. Decreased mechanical loading, by antagonizing Wnt-signaling pathway, and calcium and vitamin D malabsorption with secondary hyperparathyroidism, would contribute to bone loss. In addition, changes in fat- and gut-derived hormones tend to favor bone loss, with the exception of serotonin and GLP-1. Indeed, among the various described hormones, the effects of the adipokines leptin and adiponectin on bone are well described, while data on the impact of serotonin, GLP-1, ghrelin, PYY, and GIP is less abundant but emerging. Scarce are the studies investigating relationships between changes in such hormones, bone remodeling, and bone density. Furthermore, the extent to which the anticipated increased bone turnover would last, and whether such changes would result in an increased risk for fractures, remains to be demonstrated. Conversely, the role of bone as an endocrine organ that modulates energy metabolism and stimulates insulin and adiponectin secretion through osteocalcin is increasingly being recognized. Increases in osteocalcin after RYGB could contribute to the metabolic benefits seen with this surgery. Finally, well-designed prospective studies on bariatric surgery patients are needed and a better understanding of the role of gut and neuropeptide hormones in bone metabolism is warranted. In the interim, in view of the current evidence, we would recommend that patients submitted to RYGB surgery have an evaluation with measurement of BMD and calciotropic hormones, receive adequate replacement with calcium and vitamin D, with close monitoring for alterations in their bone metabolism. The evidence is not sufficient to recommend specific clinical care pathways and management guidelines to prevent bone loss.
References
Flegal KM, Carroll MD, Kit BK, Ogden CL (2012) Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA 307:491–497
(2008) Obesity and Overweight. World Health Organization. http://www.who.int/mediacentre/factsheets/fs311/en
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292:1724–1737
Kleinman NL, Melkonian A, St B, Rohrbacker N, Lynch WD, Gardner HH (2009) The impact of morbid obesity and bariatric surgery on comorbid conditions: a comprehensive examination of comorbidities in an employed population. J Occup Environ Med 51:170–179
Carlos do Rego Furtado L (2010) Procedure and outcomes of Roux-en-Y gastric bypass. Br J Nurs 19:307–313
Folli F, Sabowitz BN, Schwesinger W, Fanti P, Guardado-Mendoza R, Muscogiuri G (2012) Bariatric surgery and bone disease: from clinical perspective to molecular insights. Int J Obes (Lond) 36:1373–1379
Buchwald H, Buchwald JN (2002) Evolution of operative procedures for the management of morbid obesity 1950–2000. Obes Surg 12:705–717
Adrian TE, Ferri GL, Bacarese-Hamilton AJ, Fuessl HS, Polak JM, Bloom SR (1985) Human distribution and release of a putative new gut hormone, peptide YY. Gastroenterology 89:1070–1077
Batterham RL, Bloom SR (2003) The gut hormone peptide YY regulates appetite. Ann N Y Acad Sci 994:162–168
Batterham RL, Cohen MA, Ellis SM, Le Roux CW, Withers DJ, Frost GS, Ghatei MA, Bloom SR (2003) Inhibition of food intake in obese subjects by peptide YY3-36. N Engl J Med 349:941–948
le Roux CW, Batterham RL, Aylwin SJ et al (2006) Attenuated peptide YY release in obese subjects is associated with reduced satiety. Endocrinology 147:3–8
Reid IR (2002) Relationships among body mass, its components, and bone. Bone 31:547–555
Misra M, Miller KK, Tsai P, Gallagher K, Lin A, Lee N, Herzog DB, Klibanski A (2006) Elevated peptide YY levels in adolescent girls with anorexia nervosa. J Clin Endocrinol Metab 91:1027–1033
Russell M, Stark J, Nayak S, Miller KK, Herzog DB, Klibanski A, Misra M (2009) Peptide YY in adolescent athletes with amenorrhea, eumenorrheic athletes and non-athletic controls. Bone 45:104–109
Baldock PA, Sainsbury A, Couzens M, Enriquez RF, Thomas GP, Gardiner EM, Herzog H (2002) Hypothalamic Y2 receptors regulate bone formation. J Clin Invest 109:915–921
Wong IP, Driessler F, Khor EC et al (2012) Peptide YY regulates bone remodeling in mice: a link between gut and skeletal biology. PLoS One 7:e40038
Wortley KE, Garcia K, Okamoto H et al (2007) Peptide YY regulates bone turnover in rodents. Gastroenterology 133:1534–1543
Dirksen C, Jorgensen NB, Bojsen-Moller KN, Jacobsen SH, Hansen DL, Worm D, Holst JJ, Madsbad S (2012) Mechanisms of improved glycaemic control after Roux-en-Y gastric bypass. Diabetologia 55:1890–1901
Vilsboll T, Krarup T, Sonne J, Madsbad S, Volund A, Juul AG, Holst JJ (2003) Incretin secretion in relation to meal size and body weight in healthy subjects and people with type 1 and type 2 diabetes mellitus. J Clin Endocrinol Metab 88:2706–2713
Tsukiyama K, Yamada Y, Yamada C et al (2006) Gastric inhibitory polypeptide as an endogenous factor promoting new bone formation after food ingestion. Mol Endocrinol 20:1644–1651
Bollag RJ, Zhong Q, Phillips P et al (2000) Osteoblast-derived cells express functional glucose-dependent insulinotropic peptide receptors. Endocrinology 141:1228–1235
Zhong Q, Itokawa T, Sridhar S et al (2007) Effects of glucose-dependent insulinotropic peptide on osteoclast function. Am J Physiol Endocrinol Metab 292:E543–E548
Bollag RJ, Zhong Q, Ding KH, Phillips P, Zhong L, Qin F, Cranford J, Mulloy AL, Cameron R, Isales CM (2001) Glucose-dependent insulinotropic peptide is an integrative hormone with osteotropic effects. Mol Cell Endocrinol 177:35–41
Xie D, Cheng H, Hamrick M et al (2005) Glucose-dependent insulinotropic polypeptide receptor knockout mice have altered bone turnover. Bone 37:759–769
Wojcik MH, Meenaghan E, Lawson EA, Misra M, Klibanski A, Miller KK (2010) Reduced amylin levels are associated with low bone mineral density in women with anorexia nervosa. Bone 46:796–800
Rao RS, Kini S (2011) GIP and bariatric surgery. Obes Surg 21:244–252
Date Y, Kojima M, Hosoda H, Sawaguchi A, Mondal MS, Suganuma T, Matsukura S, Kangawa K, Nakazato M (2000) Ghrelin, a novel growth hormone-releasing acylated peptide, is synthesized in a distinct endocrine cell type in the gastrointestinal tracts of rats and humans. Endocrinology 141:4255–4261
Lehto-Axtelius D, Stenstrom M, Johnell O (1998) Osteopenia after gastrectomy, fundectomy or antrectomy: an experimental study in the rat. Regul Pept 78:41–50
Ohlsson C, Bengtsson BA, Isaksson OG, Andreassen TT, Slootweg MC (1998) Growth hormone and bone. Endocr Rev 19:55–79
Fukushima N, Hanada R, Teranishi H et al (2005) Ghrelin directly regulates bone formation. J Bone Miner Res 20:790–798
Deng F, Ling J, Ma J, Liu C, Zhang W (2008) Stimulation of intramembranous bone repair in rats by ghrelin. Exp Physiol 93:872–879
Maccarinelli G, Sibilia V, Torsello A, Raimondo F, Pitto M, Giustina A, Netti C, Cocchi D (2005) Ghrelin regulates proliferation and differentiation of osteoblastic cells. J Endocrinol 184:249–256
van der Velde M, van der Eerden BC, Sun Y, Almering JM, van der Lely AJ, Delhanty PJ, Smith RG, van Leeuwen JP (2012) An age-dependent interaction with leptin unmasks ghrelin's bone-protective effects. Endocrinology 153:3593–3602
Cummings DE, Weigle DS, Frayo RS, Breen PA, Ma MK, Dellinger EP, Purnell JQ (2002) Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med 346:1623–1630
Pournaras DJ, le Roux CW (2010) Ghrelin and metabolic surgery. Int J Pept 2010:217267. doi:10.1155/2010/217267
Pories WJ (2008) Ghrelin? Yes, it is spelled correctly. Ann Surg 247:408–410
le Roux CW, Neary NM, Halsey TJ, Small CJ, Martinez-Isla AM, Ghatei MA, Theodorou NA, Bloom SR (2005) Ghrelin does not stimulate food intake in patients with surgical procedures involving vagotomy. J Clin Endocrinol Metab 90:4521–4524
McLaughlin T, Abbasi F, Lamendola C, Frayo RS, Cummings DE (2004) Plasma ghrelin concentrations are decreased in insulin-resistant obese adults relative to equally obese insulin-sensitive controls. J Clin Endocrinol Metab 89:1630–1635
Gutniak M, Orskov C, Holst JJ, Ahren B, Efendic S (1992) Antidiabetogenic effect of glucagon-like peptide-1 (7–36)amide in normal subjects and patients with diabetes mellitus. N Engl J Med 326:1316–1322
Farilla L, Bulotta A, Hirshberg B, Li Calzi S, Khoury N, Noushmehr H, Bertolotto C, Di Mario U, Harlan DM, Perfetti R (2003) Glucagon-like peptide 1 inhibits cell apoptosis and improves glucose responsiveness of freshly isolated human islets. Endocrinology 144:5149–5158
Yamada C, Yamada Y, Tsukiyama K, Yamada K, Udagawa N, Takahashi N, Tanaka K, Drucker DJ, Seino Y, Inagaki N (2008) The murine glucagon-like peptide-1 receptor is essential for control of bone resorption. Endocrinology 149:574–579
Nuche-Berenguer B, Portal-Nunez S, Moreno P, Gonzalez N, Acitores A, Lopez-Herradon A, Esbrit P, Valverde I, Villanueva-Penacarrillo ML (2010) Presence of a functional receptor for GLP-1 in osteoblastic cells, independent of the cAMP-linked GLP-1 receptor. J Cell Physiol 225:585–592
Nuche-Berenguer B, Moreno P, Esbrit P, Dapia S, Caeiro JR, Cancelas J, Haro-Mora JJ, Villanueva-Penacarrillo ML (2009) Effect of GLP-1 treatment on bone turnover in normal, type 2 diabetic, and insulin-resistant states. Calcif Tissue Int 84:453–461
Bunck MC, Eliasson B, Corner A, Heine RJ, Shaginian RM, Taskinen MR, Yki-Jarvinen H, Smith U, Diamant M (2011) Exenatide treatment did not affect bone mineral density despite body weight reduction in patients with type 2 diabetes. Diabetes Obes Metab 13:374–377
Pieber TR, Roitelman J, Lee Y, Luskey KL, Stein DT (1994) Direct plasma radioimmunoassay for rat amylin-(1–37): concentrations with acquired and genetic obesity. Am J Physiol 267:E156–E164
Villa I, Rubinacci A, Ravasi F, Ferrara AF, Guidobono F (1997) Effects of amylin on human osteoblast-like cells. Peptides 18:537–540
Cornish J, Callon KE, Cooper GJ, Reid IR (1995) Amylin stimulates osteoblast proliferation and increases mineralized bone volume in adult mice. Biochem Biophys Res Commun 207:133–139
Alam AS, Moonga BS, Bevis PJ, Huang CL, Zaidi M (1993) Amylin inhibits bone resorption by a direct effect on the motility of rat osteoclasts. Exp Physiol 78:183–196
Cornish J, Callon KE, Bava U, Kamona SA, Cooper GJ, Reid IR (2001) Effects of calcitonin, amylin, and calcitonin gene-related peptide on osteoclast development. Bone 29:162–168
Pietschmann P, Farsoudi KH, Hoffmann O, Klaushofer K, Horandner H, Peterlik M (1993) Inhibitory effect of amylin on basal and parathyroid hormone-stimulated bone resorption in cultured neonatal mouse calvaria. Bone 14:167–172
Cornish J, Callon KE, King AR, Cooper GJ, Reid IR (1998) Systemic administration of amylin increases bone mass, linear growth, and adiposity in adult male mice. Am J Physiol 275:E694–E699
Dacquin R, Davey RA, Laplace C, Levasseur R, Morris HA, Goldring SR, Gebre-Medhin S, Galson DL, Zajac JD, Karsenty G (2004) Amylin inhibits bone resorption while the calcitonin receptor controls bone formation in vivo. J Cell Biol 164:509–514
Zaidi M, Shankar VS, Huang CL, Pazianas M, Bloom SR (1993) Amylin in bone conservation current evidence and hypothetical considerations. Trends Endocrinol Metab 4:255–259
Kowalczyk R, Harris PW, Brimble MA, Callon KE, Watson M, Cornish J (2012) Synthesis and evaluation of disulfide bond mimetics of amylin-(1–8) as agents to treat osteoporosis. Bioorg Med Chem 20:2661–2668
Shin AC, Zheng H, Townsend RL, Sigalet DL, Berthoud HR (2010) Meal-induced hormone responses in a rat model of Roux-en-Y gastric bypass surgery. Endocrinology 151:1588–1597
Kashyap SR, Daud S, Kelly KR, Gastaldelli A, Win H, Brethauer S, Kirwan JP, Schauer PR (2010) Acute effects of gastric bypass versus gastric restrictive surgery on beta-cell function and insulinotropic hormones in severely obese patients with type 2 diabetes. Int J Obes (Lond) 34:462–471
Jacobsen SH, Olesen SC, Dirksen C et al (2012) Changes in gastrointestinal hormone responses, insulin sensitivity, and beta-cell function within 2 weeks after gastric bypass in non-diabetic subjects. Obes Surg 22:1084–1096
Bose M, Teixeira J, Olivan B, Bawa B, Arias S, Machineni S, Pi-Sunyer FX, Scherer PE, Laferrere B (2010) Weight loss and incretin responsiveness improve glucose control independently after gastric bypass surgery. J Diabetes 2:47–55
Yang J, Zhang X, Wang W, Liu J (2010) Insulin stimulates osteoblast proliferation and differentiation through ERK and PI3K in MG-63 cells. Cell Biochem Funct 28:334–341
Niu T, Rosen CJ (2005) The insulin-like growth factor-I gene and osteoporosis: a critical appraisal. Gene 361:38–56
Dagogo-Jack S, al-Ali N, Qurttom M (1997) Augmentation of bone mineral density in hirsute women. J Clin Endocrinol Metab 82:2821–2825
Thomas DM, Udagawa N, Hards DK, Quinn JM, Moseley JM, Findlay DM, Best JD (1998) Insulin receptor expression in primary and cultured osteoclast-like cells. Bone 23:181–186
Ferron M, Wei J, Yoshizawa T, Del Fattore A, DePinho RA, Teti A, Ducy P, Karsenty G (2010) Insulin signaling in osteoblasts integrates bone remodeling and energy metabolism. Cell 142:296–308
Cornish J, MacGibbon A, Lin JM et al (2008) Modulation of osteoclastogenesis by fatty acids. Endocrinology 149:5688–5695
Reid IR (2008) Relationships between fat and bone. Osteoporos Int 19:595–606
Yadav VK, Oury F, Suda N et al (2009) A serotonin-dependent mechanism explains the leptin regulation of bone mass, appetite, and energy expenditure. Cell 138:976–989
Yadav VK, Ryu JH, Suda N et al (2008) Lrp5 controls bone formation by inhibiting serotonin synthesis in the duodenum. Cell 135:825–837
Gong Y, Slee RB, Fukai N et al (2001) LDL receptor-related protein 5 (LRP5) affects bone accrual and eye development. Cell 107:513–523
Boyden LM, Mao J, Belsky J, Mitzner L, Farhi A, Mitnick MA, Wu D, Insogna K, Lifton RP (2002) High bone density due to a mutation in LDL-receptor-related protein 5. N Engl J Med 346:1513–1521
Modder UI, Achenbach SJ, Amin S, Riggs BL, Melton LJ 3rd, Khosla S (2010) Relation of serum serotonin levels to bone density and structural parameters in women. J Bone Miner Res 25:415–422
Schwan S, Hallberg P (2009) SSRIs, bone mineral density, and risk of fractures—a review. Eur Neuropsychopharmacol 19:683–692
Strauss BJ, Marks SJ, Growcott JP, Stroud DB, Lo CS, Dixon JB, O'Brien PE (2003) Body composition changes following laparoscopic gastric banding for morbid obesity. Acta Diabetol 40(Suppl 1):S266–S269
DiGiorgi M, Daud A, Inabnet WB, Schrope B, Urban-Skuro M, Restuccia N, Bessler M (2008) Markers of bone and calcium metabolism following gastric bypass and laparoscopic adjustable gastric banding. Obes Surg 18:1144–1148
Dixon JB, Strauss BJ, Laurie C, O'Brien PE (2007) Changes in body composition with weight loss: obese subjects randomized to surgical and medical programs. Obesity (Silver Spring) 15:1187–1198
von Mach MA, Stoeckli R, Bilz S, Kraenzlin M, Langer I, Keller U (2004) Changes in bone mineral content after surgical treatment of morbid obesity. Metabolism 53:918–921
Coates PS, Fernstrom JD, Fernstrom MH, Schauer PR, Greenspan SL (2004) Gastric bypass surgery for morbid obesity leads to an increase in bone turnover and a decrease in bone mass. J Clin Endocrinol Metab 89:1061–1065
Riedt CS, Brolin RE, Sherrell RM, Field MP, Shapses SA (2006) True fractional calcium absorption is decreased after Roux-en-Y gastric bypass surgery. Obesity (Silver Spring) 14:1940–1948
Bruno C, Fulford AD, Potts JR, McClintock R, Jones R, Cacucci BM, Gupta CE, Peacock M, Considine RV (2010) Serum markers of bone turnover are increased at six and 18 months after Roux-en-Y bariatric surgery: correlation with the reduction in leptin. J Clin Endocrinol Metab 95:159–166
Fleischer J, Stein EM, Bessler M, Della Badia M, Restuccia N, Olivero-Rivera L, McMahon DJ, Silverberg SJ (2008) The decline in hip bone density after gastric bypass surgery is associated with extent of weight loss. J Clin Endocrinol Metab 93:3735–3740
El-Kadre LJ, Rocha PR, de Almeida Tinoco AC, Tinoco RC (2004) Calcium metabolism in pre- and postmenopausal morbidly obese women at baseline and after laparoscopic Roux-en-Y gastric bypass. Obes Surg 14:1062–1066
Ott MT, Fanti P, Malluche HH, Ryo UY, Whaley FS, Strodel WE, Colacchi TA (1992) Biochemical evidence of metabolic bone disease in women following Roux-Y gastric bypass for morbid obesity. Obes Surg 2:341–348
Goode LR, Brolin RE, Chowdhury HA, Shapses SA (2004) Bone and gastric bypass surgery: effects of dietary calcium and vitamin D. Obes Res 12:40–47
Valderas JP, Velasco S, Solari S, Liberona Y, Viviani P, Maiz A, Escalona A, Gonzalez G (2009) Increase of bone resorption and the parathyroid hormone in postmenopausal women in the long-term after Roux-en-Y gastric bypass. Obes Surg 19:1132–1138
Beck TJ, Petit MA, Wu G, LeBoff MS, Cauley JA, Chen Z (2009) Does obesity really make the femur stronger? BMD, geometry, and fracture incidence in the women's health initiative-observational study. J Bone Miner Res 24:1369–1379
Gomez JM, Vilarrasa N, Masdevall C, Pujol J, Solano E, Soler J, Elio I, Gallart L, Vendrell J (2009) Regulation of bone mineral density in morbidly obese women: a cross-sectional study in two cohorts before and after bypass surgery. Obes Surg 19:345–350
Vilarrasa N, San Jose P, Garcia I, Gomez-Vaquero C, Miras PM, de Gordejuela AG, Masdevall C, Pujol J, Soler J, Gomez JM (2011) Evaluation of bone mineral density loss in morbidly obese women after gastric bypass: 3-year follow-up. Obes Surg 21:465–472
Vilarrasa N, Gomez JM, Elio I et al (2009) Evaluation of bone disease in morbidly obese women after gastric bypass and risk factors implicated in bone loss. Obes Surg 19:860–866
Casagrande DS, Repetto G, Mottin CC, Shah J, Pietrobon R, Worni M, Schaan BD (2012) Changes in bone mineral density in women following 1-year gastric bypass surgery. Obes Surg 22:1287–1292
Carrasco F, Ruz M, Rojas P et al (2009) Changes in bone mineral density, body composition and adiponectin levels in morbidly obese patients after bariatric surgery. Obes Surg 19:41–46
Mahdy T, Atia S, Farid M, Adulatif A (2008) Effect of Roux-en Y gastric bypass on bone metabolism in patients with morbid obesity: Mansoura experiences. Obes Surg 18:1526–1531
Yu EW, Thomas BJ, Brown JK, Finkelstein JS (2012) Simulated increases in body fat and errors in bone mineral density measurements by DXA and QCT. J Bone Miner Res 27:119–124
Hangartner TN, Johnston CC (1990) Influence of fat on bone measurements with dual-energy absorptiometry. Bone Miner 9:71–81
Tothill P, Laskey MA, Orphanidou CI, van Wijk M (1999) Anomalies in dual energy X-ray absorptiometry measurements of total-body bone mineral during weight change using Lunar, Hologic and Norland instruments. Br J Radiol 72:661–669
Madsen OR, Jensen JE, Sorensen OH (1997) Validation of a dual energy X-ray absorptiometer: measurement of bone mass and soft tissue composition. Eur J Appl Physiol Occup Physiol 75:554–558
Bolotin HH (2007) DXA in vivo BMD methodology: an erroneous and misleading research and clinical gauge of bone mineral status, bone fragility, and bone remodelling. Bone 41:138–154
Berarducci A, Haines K, Murr MM (2009) Incidence of bone loss, falls, and fractures after Roux-en-Y gastric bypass for morbid obesity. Appl Nurs Res 22:35–41
Lalmohamed A, de Vries F, Bazelier MT, Cooper A, van Staa TP, Cooper C, Harvey NC (2012) Risk of fracture after bariatric surgery in the United Kingdom: population based, retrospective cohort study. BMJ 345:e5085
Robling AG, Bellido T, Turner CH (2006) Mechanical stimulation in vivo reduces osteocyte expression of sclerostin. J Musculoskelet Neuronal Interact 6:354
Bonewald LF, Johnson ML (2008) Osteocytes, mechanosensing and Wnt signaling. Bone 42:606–615
Armamento-Villareal R, Sadler C, Napoli N, Shah K, Chode S, Sinacore DR, Qualls C, Villareal DT (2012) Weight loss in obese older adults increases serum sclerostin and impairs hip geometry but both are prevented by exercise training. J Bone Miner Res 27:1215–1221
Bell NH, Epstein S, Greene A, Shary J, Oexmann MJ, Shaw S (1985) Evidence for alteration of the vitamin D-endocrine system in obese subjects. J Clin Invest 76:370–373
Compston JE, Vedi S, Ledger JE, Webb A, Gazet JC, Pilkington TR (1981) Vitamin D status and bone histomorphometry in gross obesity. Am J Clin Nutr 34:2359–2363
Ybarra J, Sanchez-Hernandez J, Gich I, De Leiva A, Rius X, Rodriguez-Espinosa J, Perez A (2005) Unchanged hypovitaminosis D and secondary hyperparathyroidism in morbid obesity after bariatric surgery. Obes Surg 15:330–335
Sanchez-Hernandez J, Ybarra J, Gich I, De Leiva A, Rius X, Rodriguez-Espinosa J, Perez A (2005) Effects of bariatric surgery on vitamin D status and secondary hyperparathyroidism: a prospective study. Obes Surg 15:1389–1395
Johnson JM, Maher JW, DeMaria EJ, Downs RW, Wolfe LG, Kellum JM (2006) The long-term effects of gastric bypass on vitamin D metabolism. Ann Surg 243:701–704, discussion 704–705
Holick MF (2003) Vitamin D: A millenium perspective. J Cell Biochem 88:296–307
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96:1911–1930
Dawson-Hughes B, Mithal A, Bonjour JP, Boonen S, Burckhardt P, Fuleihan GE, Josse RG, Lips P, Morales-Torres J, Yoshimura N (2010) IOF position statement: vitamin D recommendations for older adults. Osteoporos Int 21:1151–1154
Bloomberg RD, Fleishman A, Nalle JE, Herron DM, Kini S (2005) Nutritional deficiencies following bariatric surgery: what have we learned? Obes Surg 15:145–154
Bolland MJ, Grey AB, Ames RW, Horne AM, Gamble GD, Reid IR (2006) Fat mass is an important predictor of parathyroid hormone levels in postmenopausal women. Bone 38:317–321
Snijder MB, van Dam RM, Visser M, Deeg DJ, Dekker JM, Bouter LM, Seidell JC, Lips P (2005) Adiposity in relation to vitamin D status and parathyroid hormone levels: a population-based study in older men and women. J Clin Endocrinol Metab 90:4119–4123
Ostrowska Z, Zwirska-Korczala K, Buntner B, Pardela M, Drozdz M (1998) Assessment of bone metabolism in obese women. Endocr Regul 32:177–181
Kamycheva E, Sundsfjord J, Jorde R (2004) Serum parathyroid hormone level is associated with body mass index. The 5th Tromso study. Eur J Endocrinol 151:167–172
Diniz Mde F, Diniz MT, Sanches SR, Salgado PP, Valadao MM, Araujo FC, Martins DS, Rocha AL (2004) Elevated serum parathormone after Roux-en-Y gastric bypass. Obes Surg 14:1222–1226
Youssef Y, Richards WO, Sekhar N, Kaiser J, Spagnoli A, Abumrad N, Torquati A (2007) Risk of secondary hyperparathyroidism after laparoscopic gastric bypass surgery in obese women. Surg Endosc 21:1393–1396
Sahota O, Mundey MK, San P, Godber IM, Hosking DJ (2006) Vitamin D insufficiency and the blunted PTH response in established osteoporosis: the role of magnesium deficiency. Osteoporos Int 17:1013–1021
Johansson HE, Zethelius B, Ohrvall M, Sundbom M, Haenni A (2009) Serum magnesium status after gastric bypass surgery in obesity. Obes Surg 19:1250–1255
Rizzoli R, Bonjour JP (2004) Dietary protein and bone health. J Bone Miner Res 19:527–531
Aaseth J, Boivin G, Andersen O (2012) Osteoporosis and trace elements—an overview. J Trace Elem Med Biol 26:149–152
Zhao LJ, Jiang H, Papasian CJ, Maulik D, Drees B, Hamilton J, Deng HW (2008) Correlation of obesity and osteoporosis: effect of fat mass on the determination of osteoporosis. J Bone Miner Res 23:17–29
Confavreux CB, Levine RL, Karsenty G (2009) A paradigm of integrative physiology, the crosstalk between bone and energy metabolisms. Mol Cell Endocrinol 310:21–29
Lee NK, Karsenty G (2008) Reciprocal regulation of bone and energy metabolism. Trends Endocrinol Metab 19:161–166
Himms-Hagen J (1999) Physiological roles of the leptin endocrine system: differences between mice and humans. Crit Rev Clin Lab Sci 36:575–655
Considine RV, Sinha MK, Heiman ML et al (1996) Serum immunoreactive-leptin concentrations in normal-weight and obese humans. N Engl J Med 334:292–295
Cornish J, Callon KE, Bava U et al (2002) Leptin directly regulates bone cell function in vitro and reduces bone fragility in vivo. J Endocrinol 175:405–415
Gordeladze JO, Drevon CA, Syversen U, Reseland JE (2002) Leptin stimulates human osteoblastic cell proliferation, de novo collagen synthesis, and mineralization: impact on differentiation markers, apoptosis, and osteoclastic signaling. J Cell Biochem 85:825–836
Thomas T (2004) The complex effects of leptin on bone metabolism through multiple pathways. Curr Opin Pharmacol 4:295–300
Reseland JE, Syversen U, Bakke I, Qvigstad G, Eide LG, Hjertner O, Gordeladze JO, Drevon CA (2001) Leptin is expressed in and secreted from primary cultures of human osteoblasts and promotes bone mineralization. J Bone Miner Res 16:1426–1433
Holloway WR, Collier FM, Aitken CJ, Myers DE, Hodge JM, Malakellis M, Gough TJ, Collier GR, Nicholson GC (2002) Leptin inhibits osteoclast generation. J Bone Miner Res 17:200–209
Burguera B, Hofbauer LC, Thomas T, Gori F, Evans GL, Khosla S, Riggs BL, Turner RT (2001) Leptin reduces ovariectomy-induced bone loss in rats. Endocrinology 142:3546–3553
Steppan CM, Crawford DT, Chidsey-Frink KL, Ke H, Swick AG (2000) Leptin is a potent stimulator of bone growth in ob/ob mice. Regul Pept 92:73–78
Ducy P, Amling M, Takeda S, Priemel M, Schilling AF, Beil FT, Shen J, Vinson C, Rueger JM, Karsenty G (2000) Leptin inhibits bone formation through a hypothalamic relay: a central control of bone mass. Cell 100:197–207
Takeda S, Elefteriou F, Levasseur R, Liu X, Zhao L, Parker KL, Armstrong D, Ducy P, Karsenty G (2002) Leptin regulates bone formation via the sympathetic nervous system. Cell 111:305–317
Yadav VK, Karsenty G (2009) Leptin-dependent co-regulation of bone and energy metabolism. Aging (Albany NY) 1:954–956
Karsenty G (2006) Convergence between bone and energy homeostases: leptin regulation of bone mass. Cell Metab 4:341–348
Weiss LA, Barrett-Connor E, von Muhlen D, Clark P (2006) Leptin predicts BMD and bone resorption in older women but not older men: the Rancho Bernardo study. J Bone Miner Res 21:758–764
Pasco JA, Henry MJ, Kotowicz MA, Collier GR, Ball MJ, Ugoni AM, Nicholson GC (2001) Serum leptin levels are associated with bone mass in nonobese women. J Clin Endocrinol Metab 86:1884–1887
Blain H, Vuillemin A, Guillemin F, Durant R, Hanesse B, de Talance N, Doucet B, Jeandel C (2002) Serum leptin level is a predictor of bone mineral density in postmenopausal women. J Clin Endocrinol Metab 87:1030–1035
Zoico E, Zamboni M, Adami S, Vettor R, Mazzali G, Tosoni P, Bissoli L, Bosello O (2003) Relationship between leptin levels and bone mineral density in the elderly. Clin Endocrinol (Oxf) 59:97–103
Martini G, Valenti R, Giovani S, Franci B, Campagna S, Nuti R (2001) Influence of insulin-like growth factor-1 and leptin on bone mass in healthy postmenopausal women. Bone 28:113–117
Goulding A, Taylor RW (1998) Plasma leptin values in relation to bone mass and density and to dynamic biochemical markers of bone resorption and formation in postmenopausal women. Calcif Tissue Int 63:456–458
Maffei M, Halaas J, Ravussin E et al (1995) Leptin levels in human and rodent: measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nat Med 1:1155–1161
Peake PW, Kriketos AD, Campbell LV, Shen Y, Charlesworth JA (2005) The metabolism of isoforms of human adiponectin: studies in human subjects and in experimental animals. Eur J Endocrinol 153:409–417
Berner HS, Lyngstadaas SP, Spahr A, Monjo M, Thommesen L, Drevon CA, Syversen U, Reseland JE (2004) Adiponectin and its receptors are expressed in bone-forming cells. Bone 35:842–849
Williams GA, Wang Y, Callon KE et al (2009) In vitro and in vivo effects of adiponectin on bone. Endocrinology 150:3603–3610
Biver E, Salliot C, Combescure C, Gossec L, Hardouin P, Legroux-Gerot I, Cortet B (2011) Influence of adipokines and ghrelin on bone mineral density and fracture risk: a systematic review and meta-analysis. J Clin Endocrinol Metab 96:2703–2713
Oshima K, Nampei A, Matsuda M, Iwaki M, Fukuhara A, Hashimoto J, Yoshikawa H, Shimomura I (2005) Adiponectin increases bone mass by suppressing osteoclast and activating osteoblast. Biochem Biophys Res Commun 331:520–526
Luo XH, Guo LJ, Yuan LQ, Xie H, Zhou HD, Wu XP, Liao EY (2005) Adiponectin stimulates human osteoblasts proliferation and differentiation via the MAPK signaling pathway. Exp Cell Res 309:99–109
Yamaguchi N, Kukita T, Li YJ, Martinez Argueta JG, Saito T, Hanazawa S, Yamashita Y (2007) Adiponectin inhibits osteoclast formation stimulated by lipopolysaccharide from Actinobacillus actinomycetemcomitans. FEMS Immunol Med Microbiol 49:28–34
Shinoda Y, Yamaguchi M, Ogata N et al (2006) Regulation of bone formation by adiponectin through autocrine/paracrine and endocrine pathways. J Cell Biochem 99:196–208
Riggs BL, Khosla S, Melton LJ 3rd (2002) Sex steroids and the construction and conservation of the adult skeleton. Endocr Rev 23:279–302
Rao SR, Kini S, Tamler R (2011) Sex hormones and bariatric surgery in men. Gend Med 8:300–311
Karsenty G (2012) The mutual dependence between bone and gonads. J Endocrinol 213:107–114
Guney E, Kisakol G, Ozgen G, Yilmaz C, Yilmaz R, Kabalak T (2003) Effect of weight loss on bone metabolism: comparison of vertical banded gastroplasty and medical intervention. Obes Surg 13:383–388
Hammoud A, Gibson M, Hunt SC, Adams TD, Carrell DT, Kolotkin RL, Meikle AW (2009) Effect of Roux-en-Y gastric bypass surgery on the sex steroids and quality of life in obese men. J Clin Endocrinol Metab 94:1329–1332
Mauras N, Haymond MW, Darmaun D, Vieira NE, Abrams SA, Yergey AL (1994) Calcium and protein kinetics in prepubertal boys. Positive effects of testosterone. J Clin Invest 93:1014–1019
Hope WG, Ibarra MJ, Thomas ML (1992) Testosterone alters duodenal calcium transport and longitudinal bone growth rate in parallel in the male rat. Proc Soc Exp Biol Med 200:536–541
Couchourel D, Leclerc M, Filep J, Brunette MG (2004) Testosterone enhances calcium reabsorption by the kidney. Mol Cell Endocrinol 222:71–81
Carnevale V, Romagnoli E, Cipriani C, Del Fiacco R, Piemonte S, Pepe J, Scillitani A, Minisola S (2010) Sex hormones and bone health in males. Arch Biochem Biophys 503:110–117
Hammoud AO, Gibson M, Peterson CM, Meikle AW, Carrell DT (2008) Impact of male obesity on infertility: a critical review of the current literature. Fertil Steril 90:897–904
Hammoud AO, Wilde N, Gibson M, Parks A, Carrell DT, Meikle AW (2008) Male obesity and alteration in sperm parameters. Fertil Steril 90:2222–2225
Mellstrom D, Johnell O, Ljunggren O, Eriksson AL, Lorentzon M, Mallmin H, Holmberg A, Redlund-Johnell I, Orwoll E, Ohlsson C (2006) Free testosterone is an independent predictor of BMD and prevalent fractures in elderly men: MrOS Sweden. J Bone Miner Res 21:529–535
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hage, M.P., El-Hajj Fuleihan, G. Bone and mineral metabolism in patients undergoing Roux-en-Y gastric bypass. Osteoporos Int 25, 423–439 (2014). https://doi.org/10.1007/s00198-013-2480-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-013-2480-9