Abstract
The role of lymph node dissection (LND) in the treatment of patients with hepatocellular carcinoma (HCC) or intrahepatic cholangiocarcinoma (ICC) remains controversial. We sought to systematically review all available evidence to determine the role of LND in patients with HCC and ICC. Studies that reported on LND, lymph node metastasis (LNM), and short- and long-term outcomes for patients with HCC or ICC survival were identified from PubMed, Cochrane, Embase, Scopus, and Web of Science databases. Data were extracted, synthesized, and analyzed using standard techniques. A total of 603 and 434 references were identified for HCC and ICC, respectively. Among HCC patients, the overall prevalence of LND was 51.6 % (95 % confidence interval (CI) 19.7-83.5) with an associated LNM incidence of 44.5 % (95 % CI 27.4–61.7). LNM was associated with a 3- and 5-year survival of 27.5 and 20.8 %, respectively. Among ICC patients, most patients 78.5 % (95 % CI 76.2–80.7) underwent LND; 45.2 % (95 % CI 39.2–51.2) had LNM. Three and 5-year survival among ICC patients with LNM was 0.2 % (95 % CI 0–0.7) and 0 %, respectively. While there are insufficient data to recommend a routine LND in all patients with HCC or ICC, the potential prognostic value of LND suggests that LND should at least be considered at the time of surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liver cancer is the fifth most common neoplasm worldwide with nearly 750,000 new cases and nearly 700,000 deaths estimated in 2008 alone.1 Among primary liver cancer cases, the two most common forms are hepatocellular carcinoma (HCC), accounting for 70–85 % of primary liver cancer cases,2 and intrahepatic cholangiocarcinoma (ICC) representing 10–15 % of all primary liver cases.3,4 Nearly one half of all HCC cases in the USA are attributable to viral hepatic infection (HBV or HCV).5–10 Rising rates of obesity have also caused a surge in nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH), which have been found to be independent risk factors for the development of HCC.8,11–16 Risk factors for ICC, on the other hand, are less well understood but include the presence of intrahepatic stones and primary sclerosing cholangitis.17,18
Prognosis in patients with primary liver cancer is poor. Median survival after diagnosis with HCC is estimated between 1 to 60 months depending on the stage of disease at presentation with an estimated overall 5-year survival of 12–28 %.19–22 Similarly, patients with ICC have an estimated median survival of only 18–39 months and an estimated 5-year survival between 25–40 %.23–25 Though complete surgical resection provides the best option for long-term survival,26,27 only 22–30 % of patients with HCC and 30–54 % of patients with ICC are eligible for curative-intent resection at the time of presentation.19,28–30 Prognosis after surgical resection is heavily influenced by several tumor-specific characteristics in patients with HCC including tumor size, the presence of minor or major vascular invasion, and lymph node metastasis (LNM).26,31,32 Similarly, factors with prognostic significance after ICC resection are the presence of vascular invasion, multiple tumors, and LNM.17,33,34 In fact, LNM has been found to be one of the most important adverse prognostic factors in patients with HCC and ICC.35–37 Despite this, the utility of a formal evaluation of lymph node involvement at the time of surgery has been debated.
The importance of performing a lymph node dissection (LND) in an oncological resection has been established for several other hepato-pancreato-biliary tumors including extrahepatic cholangiocarcinoma,38 gallbladder cancer,39 and fibrolamellar HCC.40 However, the benefit of performing an LND during surgical resection for primary liver cancer remains controversial. Several authors have advocated for routine LND in order to comprehensively evaluate the extent of disease and accurately stage patients.25,41 Others have reported an association with LND and increased survival,42 possibly through improved locoregional tumor control.43 Conversely, several authors have found that an LND provides no survival benefit,44,45 and that the dissection only adds to the complexity and morbidity of the operation.35
In this context, we sought to systematically review all available evidence to determine the utility of performing an LND in patients with HCC and ICC. Furthermore, we aimed to identify all studies evaluating the prognostic importance of LNM in patients undergoing curative-intent resection for HCC and ICC.
Materials and Methods
Search Strategy
A systematic search of the literature was performed for studies published until December 31, 2013 using the following databases: PubMed, Cochrane, Embase, Scopus, and Web of Science. The following search terms were used to identify all articles relevant to our study: (“carcinoma, hepatocellular”46) OR (hepatocellular [tiab] AND (cancer* [tiab] OR neoplasm* [tiab] OR carcinoma* [tiab] OR tumor* [tiab] OR tumour* [tw]) OR (“intrahepatic cholangiocarcinoma”) OR (“carcinoma, intrahepatic bile duct”) OR (“intrahepatic biliary duct carcinoma”) AND (“lymph node excision”46 OR “lymph node excisions” OR “lymphadenectomy” OR “lymphadenectomies” OR “lymph node dissection”). Equivalent search strategies were used in the Embase and Web of Science databases.
Inclusion and Exclusion Criteria
All randomized controlled trials and cohort studies that evaluated the impact of LND on clinical outcomes in patients undergoing curative intent surgery for HCC and ICC were included in the study. Studies including patients with fibrolamellar HCC were excluded from the analysis. Articles were also excluded if they did not contain sufficient information regarding the incidence of LND within the cohort. Furthermore, studies with low sample size (<10 patients), limited follow-up time (<1 year), or insufficient operative data (type and extent of hepatic resection and LND) were also excluded.
Data Extraction, Synthesis, and Analysis
Using a custom-designed data extraction form, the following data from each study were extracted: study period, country of origin, and design as well as standard demographic and clinical characteristics of the cohort (number of patients and age), treatment characteristics (use of perioperative therapy, type, and extent of hepatic resection and LND), pathologic information (total number of lymph nodes harvested, number of positive lymph nodes, and lymph node ratio), and clinical outcomes (post-operative complications, overall survival, intrahepatic recurrence, LN recurrence, and total recurrence rate). The overall incidence of LNM was calculated by dividing the number of patients with metastatic lymph nodes by the number of patients who underwent LND. A second reviewer independently reviewed all articles and checked all extracted data for accuracy.
Statistical Analysis
The aggregated proportional variables (LND, LNM, recurrence, morbidity, and survival) were computed by “metan” or “meta” command which is an average of proportions weighted by the inverse of their variances. The fix/random model described by DerSimonian and Laird47 was used to calculate pool estimation based on the Q 2 and I 2 heterogeneity test results. For Q statistics, due to the low power of this test, a minimum P value cutoff of 0.1 was established as a threshold of heterogeneity. For I 2 results, values of approximately 25, 50, and 75 % were interpreted as low, medium, and high heterogeneity, respectively.48 The standard error (Se i) for each proportional variable (pi) was computed using the binominal distribution
The Z value for comparing two weighted pooled proportions was computed according to the following formula:
The total number of lymph nodes examined (TNLE) was reported as mean and standard deviation. When studies reported this variable as median and range, the mean and variance were estimated by taking into account the sample size as proposed by Hozo et al.49 Pooled estimations were made if at least three articles were available.50 All statistical analyses were performed using STATA version 10.0 (Stata Corp LP, College Station, TX, USA).
Results
Hepatocellular Carcinoma
Search Results and Article Review
We identified 603 studies through searches of PubMed (104), Embase (209), Cochrane (0), Scopus (140), and Web of Sciences (150) databases. Case reports (20), review articles (14), duplicate references (279), and non-English texts (38) were excluded. After abstract reviewing, 242 of the 252 original articles found were eliminated for failure to meet inclusion criteria. In addition, three additional studies were omitted after full-text review due to incomplete data and failure to meet inclusion criteria (Fig. 1a).51–53 Ultimately, seven studies (four prospective cohort studies41,54–56 and three retrospective studies42,45,57) were considered for final analysis (Table 1). No randomized controlled trials comparing liver resection alone and liver resection with LND were identified.
Description of New Historical Cohort
In our new historical cohort a total of 5,844 patients underwent surgical resection for HCC between 1982 and 2012. Mean age was 59.4 years (SD ± 5.60). In aggregate, 51.6 % of patients (95 % confidence interval (CI) 19.7–83.5) underwent LND at the time of resection. Among those who underwent LND, the most common site for LND was along the common hepatic artery (91.9 %) followed by dissection of the hepatic pedicle (50.0 %) and retro-pancreatic space (39.4 %). Among patients with at least one lymph node evaluated, 44.5 % (95 % CI 27.4–61.7) had evidence of LNM on pathologic examination. The aggregate mean TNLE was 6.4 (95 % CI 1.8–11.1). The lymph node ratio (LNR), or the proportion of LNM to TNLE, was reported as 0.39 (77/195) in one study57 and 0.12 (439/3,433) in another.56
Effect of LNM and LND on Survival, Recurrence, and Mortality
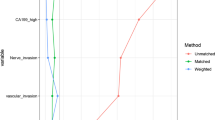
Three studies,45,56,57 involving 3,520 (60.2 %) patients, compared survival among patients with and without LNM (Table 2). Patients with LNM had worse 3- (27.5 %, 95 % CI 13.1–41.8 %) and 5-year survival (20.8 %, 95 % CI 13.2–28.4 %) compared with patients without LNM (3-year survival 60.2 %, 95 % CI 52.8–67.5 %; 5-year survival 42.6 %, 95 % CI 36.6–48.6 %) (P < 0.001) (Fig. 2a)
Two studies42,57 reported the effect of LND on survival among patients with radiographic or biopsy-proven LNM and found a higher median survival among patients who underwent a LND (P value <0.05). No comparisons, however, were made between patients who underwent LND and those who did not undergo LND. Among those who underwent LND, aggregate morbidity was 21.4 % (95 % CI 18.2–24.6), whereas mortality was 20.8 % (95 % CI 0–43.8). There were insufficient data among the articles reviewed to calculate aggregate morbidity and mortality among patients who did not undergo LND.
Intrahepatic Cholangiocarcinoma
Search Results and Study Selection
We identified 434 articles from searches of PubMed (151), Embase (151), Scopus (43), and Web of Science (89) databases. In a preliminary literature review, duplicate references (162), case reports (16), review articles (7), and non-English articles (24) were excluded. After abstract screening, 181 articles did not fulfill the inclusion criteria and were omitted. Additionally, after full-text review, eight articles58–65 were omitted because they did not report on the incidence of LND, and five articles35,66–69 were excluded because they did not differentiate between hepatic lymph node sampling and LND (Fig. 1b). Ultimately, 21 studies (6 prospective43,44,70–73 and 15 retrospective17,25,34,72,74–84) were included in the final analysis; no randomized controlled trials comparing ICC resection with and without LND were found (Table 3).
Ten articles 25,71,74–77,79,80,82,84 consisting of 1,033 (43.8 %) patients reported on preoperative TNM stage. The majority of patients had either advanced stage III (22.4 %, 95 % CI 9.1–35.8 %) or stage IV (36.2 %, 95 % CI 28.0–44.4 %) disease; the remaining patients had early stage I (18.7 %, 95 % CI 11.2–.26.1 %) or stage II (24.2 %, 95 % CI 19.2–29.2 %) disease. The use of neoadjuvant chemotherapy was reported in only one study83 among which 11 % of patients (n = 5) received preoperative treatment.
Description of New Historical Cohort
A total of 2,358 patients underwent resection for ICC from 1973 to 2012 and were included in the analysis. The mean age was 62.4 (SD ± 3.2) years. Among the entire cohort, 78.5 % (95 % CI 76.2–80.7) of patients underwent LND, and 45.2 % (95 % CI 39.2–51.2) of these had LNM. The mean TNLE was 13.8 (95 % CI 9.2–18.41). The most common site of LND was the hepatoduodenal ligament (44.5 %, 95 % CI 37.9–51.1) followed by the common hepatic artery (95 % CI 6.5–12.5).25,70,73,75,80–83
LN Involvement and LND Effects on ICC Patients’ Prognosis
Long-term survival of node-positive and node-negative patients was reported in eight studies43,72,73,76,78,79,82,85 (Table 4). The 3- and 5-year survival of patients with LNM were 0.2 % (95 % CI 0–0.7) and 0 %, respectively, compared with 55.6 % (95 % CI 50.4–60.9) and 45.1 % (95 % CI 37.3–52.9) among patients without LNM (P < 0.001) (Fig. 2b).
Four articles72,75,76,78 reported the effect of LND on survival of patients with known LNM. Among these, three studies found no difference in survival between patients who underwent LND and those who did not undergo LND.72,75,78 In contrast, one study76 found an improved survival among patients who underwent LND versus those who did not (13 vs. 4 months; P < 0.001). There were insufficient data to calculate pooled morbidity and mortality for ICC patients based on whether or not an LND was performed.
Discussion
The importance of LN sampling at the time of curative-intent surgical resection has been established for several gastrointestinal malignancies such as gastric,86 pancreatic,87 and gallbladder cancer.88 Despite the strong negative prognostic effect of LNM in patients with HCC and ICC, the exact role of performing an LND has not been clearly established. Some authors suggest that an LND should be performed in all patients with primary liver cancer in order to appropriately stage individuals and guide perioperative management.70,89 Conversely, other investigators studying the effects of LND have failed to find a prognostic effect of LN status on survival and thus have recommended against routine regional lymphadenectomy.68 Unlike in patients with gallbladder cancer, a formal LND is not a part of the National Comprehensive Cancer Network (NCCN) guidelines for the treatment of HCC.90 Furthermore, in patients with ICC, NCCN guidelines only suggest that an LND should be considered at the time of surgical resection. In this study, we pooled together individual patient data from previous reports of patients with HCC (n = 5,844) and ICC (n = 2,358) to generate one of the largest historical cohorts, in order to identify overall utilization of LND and the impact of LNM among these patients. We found that 51.6 % of patients with HCC and 78.5 % of patients with ICC underwent an LND in our cohort. Among these patients, we found that the presence of LNM with HCC or ICC conferred a worse overall survival compared with patients who did not have LNM.
After pooling individual patient data among studies analyzing the effects of LND and LNM in patients undergoing surgical resection for HCC, we found that despite the known negative prognostic significance of LNM, a formal LND was performed in only approximately one half (51.6 %) of patients. Among the patients who underwent a formal LND, 44.5 % of LND patients were found to have LNM. This incidence of LNM among patients with HCC is higher than those quoted in previous studies.91,92 Previous reports of LNM among patients with HCC are quoted between 1 and 2 % among patients deemed to be candidates for surgical resection at the time of presentation.93 Our meta-analysis, however, reveals a significantly higher incidence of LNM likely due, in part, to publication/selection bias as our new historical cohort included only studies in which LND was performed. Thus, the incidence of LND and LNM in the studies included in our historical cohort likely overestimates the “true” incidence of LNM generally found in patients with HCC. Specifically, selection bias is likely to have resulted in an overestimation in the rates of LND and LNM, as patients with suspected nodal involvement were more likely to undergo an LND. Our data do suggest, however, that among patients with HCC, those who do undergo LND—for whatever clinical indication—have a high incidence of LNM. Our data are similar to the findings by Sun et al.,45 who reported that while only 5.1 % of all operable HCC patients had LNM, the incidence of LNM among patients undergoing LND was 81.2 %. Unfortunately, no randomized prospective trial has evaluated the incidence of LNM in patients undergoing LND for HCC. As such, current evidenced-based NCCN guidelines do not support a routine nodal dissection in patients with HCC.90 However, several authors and institutions still support an LND at the time of HCC resection in order to adequately determine the extent of disease. Furthermore, previous authors have suggested a possible locoregional control benefit as support for performing an LND.43 Despite this, as evidenced by our data, the exact method of LND is not standardized. In fact, though dissection along the common hepatic artery was performed in the majority of patients, only half of the patients received dissection of the hepatic pedicle. Regardless, the presence of LNM (3-year survival 27.5 %) conferred a worse prognosis compared with patients who did not have LNM (3-year survival 60.2 %). Supporting this, Lee et al.57 found LNM to be an independent predictor for worse survival after controlling for various patient and disease-specific factors.
As opposed to patients with HCC, NCCN guidelines suggest that surgeons should consider a formal regional LND for patients with ICC in order to provide relevant staging information.90 Our data noted that the majority of patients with ICC did undergo an LND. In fact, over three quarters of the patients included in our analytic cohort (78.5 %) underwent an LND. Among these patients, 45.2 % were found to have LNM. Our data, however, consisted of pooled individual patient data largely derived from studies originating from Asian countries (66 %) where LND is more commonly performed in patients with ICC. In a multi-institutional analysis,34 de Jong et al. found an LND rate of only 55 % in Western centers treating ICC. In contrast, studies by Nakagawa et al.,85 Choi et al.,25 and Murakami et al.77 reported that an LND is routinely performed at these East Asian institutions. Given the high rate of LNM found among patients undergoing LND in our cohort, the data strongly suggest the adoption of a routine LND for all patients with ICC. Again, however, the rates of LND and LNM are likely to be overestimated in these studies due to a combination of selection and publication bias. Despite this, our data shows that the presence of LNM confers a significantly worse prognosis among patients with ICC (3-year survival: LNM 0.2 % vs. no LNM 55.6 %). As such, a formal LND provides significant prognostic information that may help guide future perioperative management and surveillance. In addition to adequate staging, Guglielmi et al.75 reported that overall survival was better among node-negative patients who underwent an LND versus those patients who did not. Taken together, a routine regional LND should be strongly considered in all patients undergoing surgical resection for ICC.
There are several limitations that should be considered when interpreting the data. The majority of studies included for analysis were retrospective in nature. Particularly in the case of LND rates, these studies may therefore suffer from selection bias. Furthermore, due to the paucity and heterogeneity of patient-level data, we were unable to control for other factors that may impact prognosis in addition to LNM such as extent of tumor invasion or presence of vascular invasion. Furthermore, most studies did not provide data on the extent of LND, thereby precluding any analysis of the anatomic area covered in any given “lymphadenectomy.” The goal of this study, however, was to provide a comprehensive review of synthesized data on the utilization and impact of LND among patients with HCC or ICC. Finally, despite efforts to use the best statistical methods available to estimate aggregate means,49 the TNLE reported may in fact be lower than estimated.
In conclusion, the performance of a regional LND in patients undergoing surgical resection for HCC and ICC was variable. Only approximately one half of patients with HCC and three quarters of patients with ICC underwent an LND at the time of surgical resection. Among those patients who did undergo LND, LNM was found in nearly one half of patients with HCC and ICC and conferred a significantly worse overall prognosis. While there are insufficient data to recommend a routine LND in all patients with HCC or ICC, given the potential valuable prognostic data that may help guide perioperative management, an LND should at least be considered. While the overall very low incidence of LND among patients with HCC makes routine LND perhaps unwarranted, the relative higher incidence of nodal metastasis among patients with ICC makes LND a stronger consideration for this disease. Further prospective studies are needed to determine the appropriate extent of LND and the impact of LND on perioperative morbidity among patients with primary liver cancer.
References
Jemal A, Bray F, Center M M, Ferlay J, Ward E, and Forman D. Global cancer statistics. CA: A Cancer Journal for Clinicians 2011; 61:69–90.
Venook A P, Papandreou C, Furuse J, and de Guevara L L. The incidence and epidemiology of hepatocellular carcinoma: a global and regional perspective. The Oncologist 2010; 15:5–13.
Aljiffry M, Abdulelah A, Walsh M, Peltekian K, Alwayn I, and Molinari M. Evidence-Based Approach to Cholangiocarcinoma: A Systematic Review of the Current Literature. J Am Coll Surg 2009; 208:134–147.
Bektas H, Schrem H, Kleine M, Tamac A, Vondran F, Uzunyayla S, and Klempnauer J. Primary Liver Tumours–Presentation, Diagnosis and Surgical Treatment. Liver Tumors-Epidemiology, Diagnosis, Prevention and Treatment. In Tech 2013:91–116.
Feliu J, Sastre J, Maurel J, and Isla D. Hepatocellular and biliary tract carcinomas: SEOM clinical guidelines. Clinical and Translational Oncology 2011; 13:536–544.
Al-Bahrani R, Abuetabh Y, Zeitouni N, and Sergi C. Cholangiocarcinoma: risk factors, environmental influences and oncogenesis. Ann Clin Lab Sci 2013; 43:195–210.
Ly K N, Xing J, Klevens R M, Jiles R B, Ward J W, and Holmberg S D. The increasing burden of mortality from viral hepatitis in the United States between 1999 and 2007. Ann Intern Med 2012; 156:271–8.
Venook A P, Papandreou C, Furuse J, and de Guevara L L. The incidence and epidemiology of hepatocellular carcinoma: a global and regional perspective. Oncologist 2010; 15 Suppl 4:5–13.
El-Serag H B and Rudolph K L. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology 2007;132:2557–76.
Prevention C f D C a. Viral Hepatitis Surveillance-United States, 2011. 2011;
Llovet J M. Updated treatment approach to hepatocellular carcinoma. J Gastroenterol 2005; 40:225–35.
Ascha M S, Hanouneh I A, Lopez R, Tamimi T A, Feldstein A F, and Zein N N. The incidence and risk factors of hepatocellular carcinoma in patients with nonalcoholic steatohepatitis. Hepatology 2010; 51:1972–8.
Sun B and Karin M. Obesity, inflammation, and liver cancer. J Hepatol 2012; 56:704–13.
Calle E E, Rodriguez C, Walker-Thurmond K, and Thun M J. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med 2003; 348:1625–38.
Polesel J, Zucchetto A, Montella M, Dal Maso L, Crispo A, La Vecchia C, Serraino D, Franceschi S, and Talamini R. The impact of obesity and diabetes mellitus on the risk of hepatocellular carcinoma. Ann Oncol 2009; 20:353–7.
Wong J B, McQuillan G M, McHutchison J G, and Poynard T. Estimating future hepatitis C morbidity, mortality, and costs in the United States. Am J Public Health 2000; 90:1562–9.
Cho S Y, Park S J, Kim S H, Han S S, Kim Y K, Lee K W, Lee S A, Hong E K, Lee W J, and Woo S M. Survival analysis of intrahepatic cholangiocarcinoma after resection. Annals of Surgical Oncology 2010; 17:1823–1830.
Charbel H and Al-Kawas F. Cholangiocarcinoma: Epidemiology, Risk Factors, Pathogenesis, and Diagnosis. Current Gastroenterology Reports 2011; 13:182–187.
Altekruse S F, McGlynn K A, Dickie L A, and Kleiner D E. Hepatocellular Carcinoma Confirmation, Treatment, and Survival in Surveillance, Epidemiology, and End Results Registries, 1992–2008. Hepatology 2012; 55:476–482.
Llovet J M, Bustamante J, Castells A, Vilana R, Ayuso M D C, Sala M, Brú C, Rodés J, and Bruix J. Natural history of untreated nonsurgical hepatocellular carcinoma: Rationale for the design and evaluation of therapeutic trials. Hepatology 1999; 29:62–67.
Weinmann A, Koch S, Niederle I M, Schulze-Bergkamen H, König J, Hoppe-Lotichius M, Hansen T, Pitton M B, Düber C, Otto G, Schuchmann M, Galle P R, and Wörns M A. Trends in Epidemiology, Treatment, and Survival of Hepatocellular Carcinoma Patients Between 1998 and 2009: An Analysis of 1066 Cases of a German HCC Registry. Journal of clinical gastroenterology 2013;
Uzzau A, Pertoldeo M L, Cherchi V, Bertozzi S, Avellini C, and Soardo G. Surgical Treatment Strategies and Prognosis of Hepatocellular Carcinoma. 2013
Morimoto Y, Tanaka Y, Ito T, Nakahara M, Nakaba H, Nishida T, Fujikawa M, Ito T, Yamamoto S, and Kitagawa T. Long-term survival and prognostic factors in the surgical treatment for intrahepatic cholangiocarcinoma. J Hepatobiliary Pancreat Surg 2003; 10:432–440.
Konstadoulakis M M, Roayaie S, Gomatos I P, Labow D, Fiel M-I, Miller C M, and Schwartz M E. Fifteen-year, single-center experience with the surgical management of intrahepatic cholangiocarcinoma: operative results and long-term outcome. Surgery 2008; 143:366–374.
Choi S-B, Kim K-S, Choi J-Y, Park S-W, Choi J-S, Lee W-J, and Chung J-B. The prognosis and survival outcome of intrahepatic cholangiocarcinoma following surgical resection: association of lymph node metastasis and lymph node dissection with survival. Ann Surg Oncol 2009; 16:3048–3056.
Herman J M and Pawlik T M, Hepatocellular Carcinoma, Gallbladder Cancer, and Cholangiocarcinoma, in Radiation Oncology: An Evidence-Based Approach, J.J. Lu and L.W. Brady, Editors. 2008. p. 221–243.
Tan J C, Coburn N G, Baxter N N, and Law C H. Surgical Management of Intrahepatic Cholangiocarcinoma-A Population-Based Study. Ann Surg Oncol 2008; 15:600–608.
Nathan H, Segev D L, Mayo S C, Choti M A, Cameron A M, Wolfgang C L, Hirose K, Edil B H, Schulick R D, and Pawlik T M. National trends in surgical procedures for hepatocellular carcinoma: 1998–2008. Cancer 2012; 118:1838–1844.
Cance W G, Stewart A K, and Menck H R. The National Cancer Data Base Report on treatment patterns for hepatocellular carcinomas: improved survival of surgically resected patients, 1985–1996. Cancer 2000; 88:912–20.
Dodson R M, Weiss M J, Cosgrove D, Herman J M, Kamel I, Anders R, Geschwind J F, and Pawlik T M. Intrahepatic cholangiocarcinoma: management options and emerging therapies. J Am Coll Surg 2013; 217:736–750 e4.
Pawlik T M, Delman K A, Vauthey J-N, Nagorney D M, Ng I O-L, Ikai I, Yamaoka Y, Belghiti J, Lauwers G Y, Poon R T, and Abdalla E K. Tumor size predicts vascular invasion and histologic grade: Implications for selection of surgical treatment for hepatocellular carcinoma. Liver Transplantation 2005; 11:1086–1092.
Ishii T, Hatano E, Yasuchika K, Taura K, Seo S, and Uemoto S. High risk of lung metastasis after resection of hepatocellular carcinoma more than 7 cm in diameter. Surg Today 2013:1–6.
Hyder O, Marques H, Pulitano C, Marsh J W, Alexandrescu S, Bauer T W, Gamblin T C, Sotiropoulos G C, Paul A, Barroso E, Clary B M, Aldrighetti L, Ferrone C R, Zhu A X, Popescu I, Gigot J F, Mentha G, Feng S, and Pawlik T M. A Nomogram to Predict Long-term Survival After Resection for Intrahepatic Cholangiocarcinoma: An Eastern and Western Experience. JAMA Surg 2014;
de Jong M C, Nathan H, Sotiropoulos G C, Paul A, Alexandrescu S, Marques H, Pulitano C, Barroso E, Clary B M, Aldrighetti L, Ferrone C R, Zhu A X, Bauer T W, Walters D M, Gamblin T C, Nguyen K T, Turley R, Popescu I, Hubert C, Meyer S, Schulick R D, Choti M A, Gigot J F, Mentha G, and Pawlik T M. Intrahepatic cholangiocarcinoma: an international multi-institutional analysis of prognostic factors and lymph node assessment. J Clin Oncol 2011; 29:3140–5.
Morine Y, Shimada M, Utsunomiya T, Imura S, Ikemoto T, Mori H, Hanaoka J, Kanamoto M, and Miyake H. Clinical impact of lymph node dissection in surgery for peripheral-type intrahepatic cholangiocarcinoma. Surg Today 2012; 42:147–51.
Kokudo N, Sato T, Seki M, Ohta H, Azekura K, Ueno M, Matsubara T, Yanagisawa A, Kato Y, and Takahashi T. Hepatic lymph node involvement in resected cases of liver metastases from colorectal cancer. Dis Colon Rectum 1999; 42:1285–90; discussion 1290–1.
Abdel-Wahab M, El-Husseiny T, Hanafy E, Shobary M, and Hamdy E. Prognostic factors affecting survival and recurrence after hepatic resection for hepatocellular carcinoma in cirrhotic liver. Langenbeck’s Archives of Surgery 2010; 395:625–632.
Kitagawa Y, Nagino M, Kamiya J, Uesaka K, Sano T, Yamamoto H, Hayakawa N, and Nimura Y. Lymph node metastasis from hilar cholangiocarcinoma: audit of 110 patients who underwent regional and paraaortic node dissection. Ann Surg 2001; 233:385–92.
Shimada H, Endo I, Togo S, Nakano A, Izumi T, and Nakagawara G. The role of lymph node dissection in the treatment of gallbladder carcinoma. Cancer 1997; 79:892–899.
Mavros M N, Mayo S C, Hyder O, and Pawlik T M. A systematic review: treatment and prognosis of patients with fibrolamellar hepatocellular carcinoma. J Am Coll Surg 2012; 215:820–30.
Ercolani G, Grazi G L, Ravaioli M, Grigioni W F, Cescon M, Gardini A, Del Gaudio M, and Cavallari A. The role of lymphadenectomy for liver tumors: further considerations on the appropriateness of treatment strategy. Ann Surg 2004; 239:202–9.
Kobayashi S, Takahashi S, Kato Y, Gotohda N, Nakagohri T, Konishi M, and Kinoshita T. Surgical treatment of lymph node metastases from hepatocellular carcinoma. J Hepatobiliary Pancreat Sci 2011; 18:559–66.
Miwa S, Miyagawa S, Kobayashi A, Akahane Y, Nakata T, Mihara M, Kusama K, Soeda J, and Ogawa S. Predictive factors for intrahepatic cholangiocarcinoma recurrence in the liver following surgery. Journal of Gastroenterology 2006; 41:893–900.
Shimada M, Yamashita Y, Aishima S, Shirabe K, Takenaka K, and Sugimachi K. Value of lymph node dissection during resection of intrahepatic cholangiocarcinoma. Br J Surg 2001; 88:1463–6.
Sun H C, Zhuang P Y, Qin L X, Ye Q H, Wang L, Ren N, Zhang J B, Qian Y B, Lu L, Fan J, and Tang Z Y. Incidence and prognostic values of lymph node metastasis in operable hepatocellular carcinoma and evaluation of routine complete lymphadenectomy. J Surg Oncol 2007; 96:37–45.
Attias J, Karawani H, Shemesh R, and Nageris B. Predicting hearing thresholds in occupational noise-induced hearing loss by auditory steady state responses. Ear Hear 2014; 35:330–8.
DerSimonian R and Laird N. Meta-analysis in clinical trials. Controlled Clinical Trials 1986; 7:177–188.
Higgins J P T and Thompson S G. Quantifying heterogeneity in a meta-analysis. Statistics in Medicine 2002; 21:1539–1558.
Hozo S P, Djulbegovic B, and Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC medical research methodology 2005; 5:13.
Aalaei-Andabili S H and Alavian S M. Important steps for a reliable meta-analysis. The Lancet Infectious Diseases 2012; 12:663.
Grobmyer S R, Wang L, Gonen M, Fong Y, Klimstra D, D’Angelica M, DeMatteo R P, Schwartz L, Blumgart L H, and Jarnagin W R. Perihepatic lymph node assessment in patients undergoing partial hepatectomy for malignancy. Ann Surg 2006; 244:260–4.
Hashimoto M, Matsuda M, and Watanabe G. Metachronous resection of metastatic lymph nodes in patients with hepatocellular carcinoma. Hepato-Gastroenterology 2009; 56:788–792.
Abe T, Furuse J, Yoshino M, Kinoshita T, Konishi M, Inoue K, and Hasebe T. Clinical characteristics of hepatocellular carcinoma with an extensive lymph node metastasis at diagnosis. American journal of clinical oncology 2002; 25:318–323.
Awazu M, Fukumoto T, Takebe A, Ajiki T, Matsumoto I, Kido M, Tanaka M, Kuramitsu K, and Ku Y. Lymphadenectomy combined with locoregional treatment for multiple advanced hepatocellular carcinoma with lymph node metastases. Kobe Journal of Medical Sciences 2013; 59:E17-E27.
Ravaioli M, Ercolani G, Grazi G L, Cescon M, Dazzi A, Zanfi C, and Pinna A D. Safety and prognostic role of regional lymphadenectomy for primary and metastatic liver tumors. Updates Surg 2010; 62:27–34.
Xiaohong S, Huikai L, Feng W, Ti Z, Yunlong C, and Qiang L. Clinical significance of lymph node metastasis in patients undergoing partial hepatectomy for hepatocellular carcinoma. World J Surg 2010; 34:1028–33.
Lee C W, Chan K M, Lee C F, Yu M C, Lee W C, Wu T J, and Chen M F. Hepatic resection for hepatocellular carcinoma with lymph node metastasis: clinicopathological analysis and survival outcome. Asian J Surg 2011; 34:53–62.
Hyder O, Hatzaras I, Sotiropoulos G C, Paul A, Alexandrescu S, Marques H, Pulitano C, Barroso E, Clary B M, Aldrighetti L, Ferrone C R, Zhu A X, Bauer T W, Walters D M, Groeschl R, Gamblin T C, Marsh J W, Nguyen K T, Turley R, Popescu I, Hubert C, Meyer S, Choti M A, Gigot J F, Mentha G, and Pawlik T M. Recurrence after operative management of intrahepatic cholangiocarcinoma. Surgery (United States) 2013; 153:811–818.
Sulpice L, Rayar M, Boucher E, Pele F, Pracht M, Meunier B, and Boudjema K. Intrahepatic cholangiocarcinoma: impact of genetic hemochromatosis on outcome and overall survival after surgical resection. Journal of Surgical Research 2013; 180:56–61.
Nanashima A, Shibata K, Nakayama T, Tobinaga S, Araki M, Kunizaki M, Takeshita H, Hidaka S, Sawai T, Nagayasu T, and Tagawa T. Relationship Between Microvessel Count and Postoperative Survival in Patients with Intrahepatic Cholangiocarcinoma. Ann Surg Oncol 2009; 16:2123–2129.
Zhou X-D, Tang Z-Y, Fan J, Zhou J, Wu Z-Q, Qin L-X, Ma Z-C, Sun H-C, Qiu S-J, Yu Y, Ren N, Ye Q-H, Wang L, and Ye S-L. Intrahepatic cholangiocarcinoma: report of 272 patients compared with 5,829 patients with hepatocellular carcinoma. Journal of Cancer Research and Clinical Oncology 2009; 135:1073–1080.
Guglielmi A, Ruzzenente A, Campagnaro T, Pachera S, Valdegamberi A, Nicoli P, Cappellani A, Malfermoni G, and Iacono C. Intrahepatic Cholangiocarcinoma: Prognostic Factors After Surgical Resection. World J Surg 2009; 33:1247–1254.
Shimada K, Sano T, Sakamoto Y, Esaki M, Kosuge T, and Ojima H. Clinical impact of the surgical margin status in hepatectomy for solitary mass-forming type intrahepatic cholangiocarcinoma without lymph node metastases. J Surg Oncol 2007; 96:160–165.
Tajima Y, Kuroki T, Fukuda K, Tsuneoka N, Furui J, and Kanematsu T. An intraductal papillary component is associated with prolonged survival after hepatic resection for intrahepatic cholangiocarcinoma. Br J Surg 2004; 91:99–104.
Morimoto Y, Tanaka Y, Ito T, Nakahara M, Nakaba H, Nishida T, Fujikawa M, Ito T, Yamamoto S, and Kitagawa T. Long-term survival and prognostic factors in the surgical treatment for intrahepatic cholangiocarcinoma. Journal of Hepato-Biliary-Pancreatic Surgery 2003; 10:432–440.
Igami T, Ebata T, Yokoyama Y, Sugawara G, Takahashi Y, and Nagino M. Staging of Peripheral-Type Intrahepatic Cholangiocarcinoma: Appraisal of the New TNM Classification and its Modifications. World J Surg 2011; 35:2501–2509.
Saxena A, Chua T, Sarkar A, Chu F, and Morris D. Clinicopathologic and Treatment-Related Factors Influencing Recurrence and Survival after Hepatic Resection of Intrahepatic Cholangiocarcinoma: A 19-Year Experience from an Established Australian Hepatobiliary Unit. Journal of Gastrointestinal Surgery 2010; 14:1128–1138.
Shirabe K, Mano Y, Taketomi A, Soejima Y, Uchiyama H, Aishima S, Kayashima H, Ninomiya M, and Maehara Y. Clinicopathological prognostic factors after hepatectomy for patients with mass-forming type intrahepatic cholangiocarcinoma: Relevance of the lymphatic invasion index. Annals of Surgical Oncology 2010; 17:1816–1822.
Portolani N, Baiocchi G L, Coniglio A, Piardi T, Grazioli L, Benetti A, Ferrari Bravo A, and Giulini S M. Intrahepatic cholangiocarcinoma and combined hepatocellular-cholangiocarcinoma: a Western experience. Ann Surg Oncol 2008; 15:1880–90.
Ercolani G, Grazi G L, Ravaioli M, Grigioni W F, Cescon M, Gardini A, Del Gaudio M, and Cavallari A. The role of lymphadenectomy for liver tumors - Further considerations on the appropriateness of treatment strategy. Annals of Surgery 2004; 239:202–209.
Ribero D, Pinna A D, Guglielmi A, Ponti A, Nuzzo G, Giulini S M, Aldrighetti L, Calise F, Gerunda G E, Tomatis M, Amisano M, Berloco P, Torzilli G, Capussotti L, and Italian Intrahepatic C. Surgical Approach for Long-term Survival of Patients With Intrahepatic Cholangiocarcinoma A Multi-institutional Analysis of 434 Patients. Archives of Surgery 2012; 147:1107–1113.
Uchiyama K, Yamamoto M, Yamaue H, Ariizumi S I, Aoki T, Kokudo N, Ebata T, Nagino M, Ohtsuka M, Miyazaki M, Tanaka E, Kondo S, Uenishi T, Kubo S, Yoshida H, Unno M, Imura S, Shimada M, Ueno M, and Takada T. Impact of nodal involvement on surgical outcomes of intrahepatic cholangiocarcinoma: A multicenter analysis by the Study Group for Hepatic Surgery of the Japanese Society of Hepato-Biliary-Pancreatic Surgery. Journal of Hepato-Biliary-Pancreatic Sciences 2011; 18:443–452.
Yamamoto M, Takasaki K, and Yoshikawa T. Lymph node metastasis in intrahepatic cholangiocarcinoma. Jpn J Clin Oncol 1999; 29:147–50.
Ali S M, Clark C J, Zaydfudim V M, Que F G, and Nagorney D M. Role of major vascular resection in patients with intrahepatic cholangiocarcinoma. Annals of Surgical Oncology 2013; 20:2023–2028.
Guglielmi A, Ruzzenente A, Campagnaro T, Valdegamberi A, Bagante F, Bertuzzo F, Conci S, and Iacono C. Patterns and Prognostic Significance of Lymph Node Dissection for Surgical Treatment of Perihilar and Intrahepatic Cholangiocarcinoma. Journal of Gastrointestinal Surgery 2013; 17:1917–1928.
Li S Q, Liang L J, Hua Y P, Peng B G, He Q, Lu M D, and Chen D. Long-term outcome and prognostic factors of intrahepatic cholangiocarcinoma. Chin Med J (Engl) 2009; 122:2286–91.
Murakami Y, Uemura K, Sudo T, Hashimoto Y, Nakashima A, and Sueda T. Intrahepatic Cholangiocarcinoma: Clinicopathological Differences Between Peripheral Type and Hilar Type. Journal of Gastrointestinal Surgery 2012; 16:540–548.
Shimada K, Sano T, Nara S, Esaki M, Sakamoto Y, Kosuge T, and Ojima H. Therapeutic value of lymph node dissection during hepatectomy in patients with intrahepatic cholangiocellular carcinoma with negative lymph node involvement. Surgery 2009; 145:411–6.
Suzuki S, Sakaguchi T, Yokoi Y, Okamoto K, Kurachi K, Tsuchiya Y, Okumura T, Konno H, Baba S, and Nakamura S. Clinicopathological prognostic factors and impact of surgical treatment of mass-forming intrahepatic cholangiocarcinoma. World J Surg 2002; 26:687–93.
Tamandl D, Kaczirek K, Gruenberger B, Koelblinger C, Maresch J, Jakesz R, and Gruenberger T. Lymph node ratio after curative surgery for intrahepatic cholangiocarcinoma. Br J Surg 2009; 96:919–25.
Tsuji T, Hiraoka T, Kanemitsu K, Takamori H, Tanabe D, and Tashiro S. Lymphatic spreading pattern of intrahepatic cholangiocarcinoma. Surgery 2001; 129:401–7.
Uenishi T, Kubo S, Yamazaki O, Yamada T, Sasaki Y, Nagano H, and Monden M. Indications for surgical treatment of intrahepatic cholangiocarcinoma with lymph node metastases. Journal of Hepato-Biliary-Pancreatic Surgery 2008; 15:417–22.
Yedibela S, Demir R, Zhang W, Meyer T, Hohenberger W, and Schonleben F. Surgical treatment of mass-forming intrahepatic cholangiocarcinoma: An 11-year western single-center experience in 107 patients. Annals of Surgical Oncology 2009; 16:404–412.
Yonemori A, Kondo S, Matsuno Y, Ito T, Nakanishi Y, Miyamoto M, Tanaka E, and Hirano S. Prognostic Impact of Regional Lymph Node Micrometastasis in Patients With Node-Negative Biliary Cancer. Annals of Surgery 2010; 252:99–106.
Nakagawa T, Kamiyama T, Kurauchi N, Matsushita M, Nakanishi K, Kamachi H, Kudo T, and Todo S. Number of lymph node metastases is a significant prognostic factor in intrahepatic cholangiocarcinoma. World J Surg 2005; 29:728–33.
Jiang L, Yang K-H, Guan Q-L, Zhao P, Chen Y, and Tian J-H. Survival and recurrence free benefits with different lymphadenectomy for resectable gastric cancer: A meta-analysis. J Surg Oncol 2013; 107:807–814.
Pavlidis T E, Pavlidis E T, and Sakantamis A K. Current opinion on lymphadenectomy in pancreatic cancer surgery. Hepatobiliary Pancreat Dis Int 2011; 10:21–5.
Hueman M T, Vollmer C M, Jr., and Pawlik T M. Evolving treatment strategies for gallbladder cancer. Ann Surg Oncol 2009; 16:2101–15.
Isa T, Kusano T, Shimoji H, Takeshima Y, Muto Y, and Furukawa M. Predictive factors for long-term survival in patients with intrahepatic cholangiocarcinoma. The American journal of surgery 2001; 181:507–511.
NCCN Guidelines(R) Updates. J Natl Compr Canc Netw 2013; 11:xxxii-xxxiii.
Klintmalm G B. Liver transplantation for hepatocellular carcinoma: a registry report of the impact of tumor characteristics on outcome. Ann Surg 1998; 228:479.
Marsh J W, Dvorchik I, Bonham C A, and Iwatsuki S. Is the pathologic TNM staging system for patients with hepatoma predictive of outcome? Cancer 2000; 88:538–543.
Japan L C S G o. Primary liver cancer of Japan: clinicopathological features and results of surgical treatment. Ann Surg Oncol 1990; 211:277–287.
Acknowledgments
Dr. Aslam Ejaz was supported, in part, by the Eleanor B. Pillsbury Foundation for surgical research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Amini, N., Ejaz, A., Spolverato, G. et al. Management of Lymph Nodes During Resection of Hepatocellular Carcinoma and Intrahepatic Cholangiocarcinoma: A Systematic Review. J Gastrointest Surg 18, 2136–2148 (2014). https://doi.org/10.1007/s11605-014-2667-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2667-1