Abstract
Aim
Hepatic resections for hepatocellular carcinoma (HCC) in cirrhotic liver are characterized by early recurrence and poor survival. In this study, we analyzed several factors affecting both survival and recurrence after hepatic resection.
Patients and methods
From October 1995 to April 2007, 550 patients underwent hepatic resections, of which, 175 patients had HCC in cirrhotic liver in Gastroenterology Surgical Center, Mansoura University, Egypt. There were 131 males (74.9%) and 44 females (25.1%) with a mean age of 54.8 ± 9.2 years (ranges from 26 to 75 years).
Results
Most of our patients were in Child's Pugh class A (86.9%). Major hepatic resection was done for 65 patients (37.1%), segmentectomy was done for 62 patients (35.4%), and localized resection was done for 48 patients (27.4%). Hospital mortality occurred in 16 (9.1%) patients, while hospital morbidity occurred in 40% of patients. The 1, 3, and 5 years survival were 68.6%, 29.6%, and 10.7%, respectively. The prognostic factors affecting recurrence were multifactorial, and the univariate analysis showed that multifocality of the tumor (p = 0.006), capsule (p = 0.001), staging (p = 0.001), blood transfusion (p = 0.02), infiltration of the cut margin (p = 0.001), vascular invasion (p = 0.006), and lymph nodes infiltration (p = 0.014) affect the recurrence rate, while with multivariate analysis, only cut margin was significantly affecting the recurrence (p = 0.026). Also, factors that significantly predicted survival were preoperative serum albumin (p = 0.005), tumor differentiation (p = 0.008), staging (p = 0.001), tumor's capsule (p = 0.001), cut margin (p = 0.031), vascular invasion (p = 0.049), and operative blood transfusion (p = 0.001). However, tumor differentiation (p = 0.048) was the only independent factor on multivariate analysis affecting long-term survival.
Conclusion
In our experience, the prognostic factors after resection for recurrence and survival are different and multifactorial. However, resection of HCC in cirrhotic liver with preserved liver function is the treatment of choice in the present time and can be done with favorable results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is one of the most common malignancies worldwide. There are at least one million new cases diagnosed yearly, and about equal number of deaths occurs yearly from this disease [1, 2]. It is common in areas with endemic viral hepatitis B or C, which is the usual scenario in many African countries [3]. Hepatic resection and liver transplantation are the main stay of treatment with curative intent [4–6]. For patients with early HCC and decompensated cirrhosis, liver transplantation is the treatment of choice since the procedure potentially cures both the cirrhosis and the HCC, and the outcome after liver transplantation is universally accepted to be better than hepatic resection [6, 7]. Liver transplantation was done in Egypt; however, the practice is still very limited to a few centers due to shortage of living donors and legal handles with cadaveric transplantation. So, hepatic resection is the main line of treatment presently for patients with HCC in most centers in our country. As reported previously, most of our patients developed HCC on the background of cirrhosis, and this poses a lot of challenges in their management [8, 9]. Hence, only few of these patients could benefit from liver resection because of the stage of the tumors and their clinical status at presentation.
Despite improved resection techniques and subsequent decreased operative morbidity and mortality in hepatic surgery, there are frequent intrahepatic recurrences of HCC after radical hepatic resections [9, 10]. Several factors have been suggested to be responsible for the recurrence and possible reduced survival after liver resection for HCC [11–13]. Liver cirrhosis has been documented to be an independent risk factor for reduced survival and tumor-free period in patients with HCC [14]. However, there are few reports about independent factors affecting the overall survival and recurrence after hepatic resection for this group of patients with liver cirrhosis. Hence, the aim of this study is to determine factors affecting overall survival and recurrence following hepatic resection for patients with HCC in cirrhotic liver.
Patients and methods
From October 1995 to April 2007, 550 patients underwent hepatic resections for different malignant and benign lesions, of which, 175 patients had HCC in cirrhotic liver in Gastroenterology Surgical Center, Mansoura University, Egypt.
Preoperative assessments
All the patients underwent clinical evaluation, laboratory investigation, and imaging studies. The imaging studies include ultrasonography (US), enhanced computed tomography scan (CT scan), Doppler examination, magnetic resonance imaging, and occasional angiography using iodized oil (Lipiodol) as contrast medium followed by computed tomography. The aim of the imaging studies were to confirm diagnosis of HCC and for its initial staging as regard its size, number of lesions, the affected segments, and vascular invasion. Laparoscopic assessment was done if the radiological assessments were inconclusive. Chest X-ray was done to rule out metastasis to the chest. Upper gastrointestinal endoscopies were done routinely for all the patients, and obliteration of esophageal varices was done using injection sclerotherapy or band ligation. Patients were candidates for surgery if serum total bilirubin level is below 2 mg/dL, serum albumin above 3 g/dL, prothrombin level above 60%, absence of ascites, portal vein thrombosis, and extra hepatic metastasis. Those patients considered to have potentially resectable tumors had cardiorespiratory evaluation and were also reviewed by the anesthesiologist.
Surgical technique and procedures
The surgery was performed through bilateral subcostal incision with upward midline extension when necessary. The operative field was kept open using special retractors. Thorough exploration of the liver with intraoperative US was performed after its partial mobilization, sectioning the falciform and triangular ligaments and pulling the liver caudally to better expose its diaphragmatic surface. Definition of the area to be resected and marking the dissection line were performed under intraoperative US guidance. The types of hepatic resection were defined lately according to a recent consensus classification [15]. Right hepatectomy, left hepatectomy, extended right hepatectomy, and extended left hepatectomy were considered major hepatic resection (three segments or more), whereas segmentectomy of one or two segments and nonanatomic wedge resection were classified as minor hepatic resection (two segments or fewer). For each patient, the extent of surgery was decided preoperatively based on radiologic characteristic of the tumor. This was however subjected to modification by the surgeon based on intraoperative finding, such as gross severity of cirrhosis, and the size of the liver remnant. In general, minor hepatic resection was the preferred procedure if macroscopic tumor clearance could be achieved, but major hepatic resections were performed quite liberally for patients with more centrally located tumors close to a major portal vein or hepatic vein, provided their liver function reserve was considered adequate. Blood losses during the procedures were minimized by performing liver transection under warm ischemia, using Pringle maneuver with clamping for 15 min at 5-min intervals and hemihepatic selective vascular occlusion. Liver dissection was done using harmonic scalpel and ultrasonic device in the majority of cases while artery forceps fracture in some cases. Bleeding from the liver cut surfaces were controlled using under running stitches, electrocautery, and argon plasma coagulator. Intraoperative cholangiography was performed to detect any intraoperative bile leakage and asses the integrity of the biliary system.
Follow up
All patients were followed up at the outpatient clinic monthly for the first 3 months and then thrice monthly as long as the patients survived. At each follow-up, clinical, biochemical, and ultrasonographic assessments of patients were done. Tumor marker, α-fetoprotein, level was also measured. On suspicion of recurrence, abdominal CT scan was performed.
Data and statistical analysis
The sociodemographic, clinical, preoperative, intraoperative, and postoperative data were recorded. The collected data was organized, tabulated, and statistically analyzed using SPSS software statistical computer package version 13.0. For quantitative variables, the range, mean, and standard deviation were calculated. The difference in mean age was tested using analysis of variance. Most of the studied variables were not found to follow the normal distribution. Wilcoxon's singled-rank test was performed to test mean values before and after operation. Mann–Whitney test was performed to test mean values between two different groups. Kruskal–Wallis test was used to compare variables between more than two groups. For qualitative variables, the number and percent distribution was calculated. Binary logistic regression was used for multivariate analysis of factors affecting survival. Chi square was used as a test of significance, and when found inappropriate, Fisher's exact test was used. Significance was adopted at p < 0.05 for interpretation of results of tests of significance.
Results
From October 1995 to April 2007, 175 patients with HCC in cirrhotic livers had various forms of hepatic resection at Gastroenterology Surgical Center, Mansoura University, Egypt. Table 1 showed the clinical data of our patients. There were 131 males (74.9%) and 44 females (25.1%) with a mean age of 54.8 ± 9.2 years (ranges from 26 to 75 years). The most common symptom is right hypochondrial dull aching pain in 130 (74.3%) patients and accidentally discovered in 24 patients (13.7%), and jaundice in three patients (1.7%) due to infiltration of the biliary system, weight loss, and internal hemorrhage, which account for 1.1% each.
One hundred and thirty-eight (78.9%) patients were positive for hepatitis C virus (HCV) markers, five (2.9%) patients were positive for hepatitis B virus surface antigen (HBsAg), while seven (4.0%) patients were positive for both virus markers. Most of the patients were in Child's Pugh class A (152 (86.9%)), and the other 28 (13.1%) patients were in Child's Pugh class B. The mean serum albumin, total bilirubin, prothrombin time, and serum α-fetoprotein at presentation were 3.9 ± 0.5 g/dL, 1 ± 0.9 g/dL, 85.8 ± 12.3 s, and 572.3 ± 80.9 ng/mL. Table 2 showed the various surgical procedures performed. Major hepatic resection was done for 65 patients (37.1%), segmentectomy was done for 62 patients (35.4%), and localized resection was done for 48 patients (27.4%). The mean operative time was 3.1 ± 0.9 h. Blood transfusion was required in 102 (58.3%) patients (mean 3 ± 1 unit). As shown in Table 3, the sizes of the tumor vary from less than 5 cm in 35 (20%) patients to more than 10 cm in 50 (28.6%) patients.
Postoperative pathological examination revealed well-differentiated tumors in 34 (19.5%) patients, moderately differentiated tumor in 76 (43.4%) patients, and poorly differentiated tumor in 65 (37.1%) patients. All other pathological findings are shown in Table 3. The mean hospital stay was 9.6 ± 4.7 days. Hospital morbidity includes acute liver cell failure in 19 patients (10.9%), bile leak in ten patients (5.7%), and upper gastrointestinal bleeding in one patient (0.6%) due to rupture esophageal varices and treated by emergency injection sclerotherapy. Pleural effusion on the right side occurred in 13 patients (7.4%) which were treated by insertion of chest tube for 1 week. Wound infection occurred only in six patients (3.4%). Hospital mortality occurred in 16 patients (9.1%) from liver cell failure (LCF); ten of them were Child B, and six of them were Child A (Table 4).
Recurrence
Late complications included recurrence of HCC in 78 patients (49.1%). Most of the recurrences occurred within the first year (62.8%) compared to 29 (37.2%) after the first year. The most common site for recurrence was the liver in 61 patients (78.2%), while distant metastasis occurred in seven patients (9%). The factors affecting the recurrence rate were shown in Table 5. The most significant factors were tumor capsule, cut margin infiltration, vascular invasion, lymph nodes infiltration, multifocality, tumor–node–metastasis (TNM) staging, and operative blood transfusion. The treatment for recurrence was conservative in 58 of cases (74.3%), chemoembolization (CHE) in 12 cases (15.4%), radiofrequency (RF) in five cases (6.4%), and re-exploration and resection in three (3.8%) cases.
Table 6 showed univariate and multivariate analysis for variables as predictors of recurrence after surgical resection where infiltrated cut margin was the only predictor on multivariate analysis.
Survival and prognostic factors
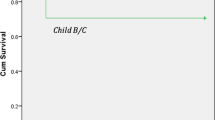
The median survival after surgical resection was 24 months. One-year survival was 72%, 3-year survival was 42%, while 5-year survival was 21% (Fig. 1).
-
Univariate analysis: The result of a univariate analysis using the Kaplan–Meier product limits method for the relations between clinical, pathological, and interventional variables for survival after resectional surgery shown in Table 7. Based on the results mentioned above, factors that significantly predicted survival were preoperative serum albumin, tumor differentiation, staging, tumor's capsule, cut margin, vascular invasion, and operative blood transfusion.
Table 7 Factors affecting survival -
Multivariate analysis: The variables that were significant by univariate analysis were subsequently analyzed using the Cox proportional hazard model. The only factor that was significantly related to patient's survival was tumor differentiation (Table 8).
Table 8 Univariate and multivariate analysis for variables as predictors of survival after surgical resection
Discussion
Two issues had long challenge the rational for hepatic resection in patients with HCC in cirrhotic liver. These include the high incidence of recurrence which may be more than 50% within 5 years of resection [16, 17] and low survival rate with perioperative mortality up to 20% [18]. Recurrence can be classified as early (within 12 months to 3 years) or late [19]. The two different timings of recurrence are thought to represent disease of differing biologies that have very different prognoses. Early recurrence usually represents residual tumor spread from the primary main tumor and left in the remnant liver, and is a poor prognostic sign. Significant risk factors for early recurrence include preoperative tumor rupture, venous invasion, and nonanatomic resection [20, 21]. Late recurrence usually results from metachronous multicentric hepatocarcinogenesis. Possible risk factors for late recurrence include cirrhosis, a higher grade of hepatitis activity, a high preoperative aspartate aminotransferase level (especially in an HCV-positive patient), and multiple tumors [21–23]. As previously reported, most of the recurrence in our patients and in other series are multicentric in location and distant from the resection margin [8, 16, 17]. This will imply that wide resection margin had been found not to convey much additional benefit in preventing recurrence [23]. Most surgeons will advocate limited resection of the tumor especially in patients with liver cirrhosis. However, some study had challenged this opinion. It is believed that HCC has a high propensity to metastasis through the portal veins even when diagnosed at early stage [20, 21, 24]. This finding had empowered the aggressive surgeons to carry out major resection in this group of patients so that proper clearance of the portal channels can be performed. In our previous report, however, we found that there was no significant difference in the recurrence rate that occurred between major resection and minor or localized resection of the liver [8]. Recurrence in our series was about 49%. This was essentially similar to finding in previous reports. Most of the recurrences are found in the liver [16, 17, 25]. About 10% of the recurrence occurred at a site away from the liver. This implies that there was possible systemic involvement before surgical interference. This was beautifully described by Jeng et al. that patients with high circulating HCC cells had high risk of early recurrence [26].
In the present study, the prognostic factors affecting the time to recurrence was multifactorial, and the univariate analysis showed that multifocality of the tumor, capsule, staging, blood transfusion, infiltration of the cut margin, vascular invasion, and lymph nodes infiltration affects the recurrence rate, while with multivariate analysis, only cut margin was significantly affecting the recurrence. In contrast to the study of Portolani et al. [27] on 213 patients, of them, only 113 patients have cirrhosis, the positivity of HCV and the presence of cirrhosis showed a prognostic value at the univariate and multivariate analysis, but other features in our study did not have a prognostic impact, while in the study of Kaibori et al. [13], the tumor stage and intraoperative blood transfusion had prognostic impact on the recurrence. Although, these results were similar to ours, the other reported factors mentioned by the author were not, such as patient age and tumor size [13].
The role of perioperative blood transfusion on intrahepatic recurrence of HCC was first suggested by Yamamoto et al. [28], whereas Matsumata et al. [29] reported that the association between blood transfusion and recurrence-free survival was recognized, but only in patients without intrahepatic metastasis. Furthermore, Makino et al. found that the association between perioperative blood transfusion and the cancer-free survival could only be detected in HCC patients with portal vein invasion [30]. In general, the detrimental effect of blood transfusion could be attributed to the induction of nonspecific immunosuppression, such as increased activity and number of suppresser T lymphocyte, decreased natural killer cell function, depressed macrophage and monocyte phagocytic activity, and increased levels of immunosuppressant prostaglandin E2 [30, 31]. The indications of blood transfusion are obviously determined by a number of factors, such as amount of blood loss during surgery, the extent of the surgical procedure, and the skill of the surgeon. To improve the prognosis of patients with resectable HCC, it is worthwhile to reduce intraoperative blood loss and avoid blood transfusion when possible.
We found that the resection margin is an independent factor affecting both survival and recurrence after hepatic resection. One important issue that remains very controversial in liver resection for patients with HCC on top of cirrhosis is the oncologic resection margin. A few studies have shown that a resection margin smaller than 1 cm was an adverse prognostic factor for long-term survival [32, 33]. However, others have found no correlation between the width of the resection margin and long-term outcome. These seemingly conflicting results have resulted in a discrepancy among hepatic surgeons on the definition of curative resection for HCC. In general, it is thought that both surgical curability and postoperative hepatic functional preservation are crucial for the successful treatment of patients with HCCs [16, 17, 19, 20]. Especially in patients with cirrhosis, smaller surgical margins would better prevent postoperative complications, including liver failure, though there is a concern of recurrence in the remnant liver, including the cut stump (the cut surface of the remnant liver). For patients with cirrhosis, the balance between surgical curability and preservation of function of the remnant liver is of great importance. In patients with centrally located tumors that are close to the major intrahepatic vessels, resections are difficult to perform with adequate surgical margins. To avoid postoperative liver failure for patients with cirrhosis, hepatic surgeons often have no choice but to carefully dissect and resect the tumor away from vascular structures (exposing the tumor surface) to remove tumor tissue adhering to or compressing the large vascular structures.
Well-encapsulated HCC was found to be less prone to recurrence compared to diffused tumor. Encapsulated tumors generally displace normal vasculature rather than invade major vessels. Hence, the possibility of having oncologic clearance is high with encapsulated tumors than diffused. Univariate analysis of many factors suggested to influence survival showed that about seven factors affected the survival significantly. Tumor stage has bearing with the size of the tumor. The Liver Cancer Study Group of Japan has reported that HCC tumor size and survival rate after liver resection are inversely correlated [34]. Additionally, some investigators have noted that outcome after resection for a large HCC is extremely poor [35]. However, it had been documented that in well-selected patients with large tumor, hepatic resection could offer good long-term survival. Tumor grade was an independent factor that clearly affects long-term survival. The grade of histological differentiation (grading) of the tumor represents much more biological aggressiveness of HCC and, therefore, may better predict the risk of tumor recurrence in particular patients [36]. However, Kaibori et al., [13] reported that the degree of differentiation has a negative prognostic impact as regard the recurrence rate for patients conforming to or outside the Milan criteria. In our present series, the histopathological grade of differentiation was grade I–II in 110 patients (62.9%) and grade III (poorly differentiated) in 65 patients (37.1%). Moreover, it was found that tumor grading is a negative prognostic index as regard the recurrence, while it is a positive prognostic index for overall survival in univariate and multivariate analysis.
In our experience, the prognostic factors after resection for recurrence and survival are different and multifactorial. However, resection of HCC in cirrhotic liver with preserved liver function is the treatment of choice and can be done with favorable results and long-term survival. As regard recurrence, multifocality of the tumor, capsule, staging, blood transfusion, infiltration of the cut margin, vascular invasion, and lymph nodes infiltration affect the recurrence rate, while cut margin was significantly on multivariate analysis. Also, factors that significantly predicted survival were preoperative serum albumin, tumor differentiation, staging, tumor's capsule, cut margin, vascular invasion, and operative blood transfusion, while tumor differentiation was the only independent factor on multivariate analysis.
References
Parkin DM, Bray F, Ferlay J, Pisani P (2001) Estimating the world cancer burden Globocan 2000. Int J Cancer 94:153–156
Bosch FX, Ribes J, Díaz M et al (2004) Primary liver cancer: worldwide incidence and trends. Gastroenterology 127:S5–S16
Sherman M (2005) Hepatocellular carcinoma: Epidemiology, risk factors, and screening. Semin Liver Dis 24:143–154
Siegel AB, McBride RB, El-Serag HB et al (2008) Racial disparities in utilization of liver transplantation for hepatocellular carcinoma in the United States, 1998–2002. Am J Gastroenterol 103:120–127
Chang C, Chau G, Lui W, Tsay S, King K, Wu C (2004) Long-term results of hepatic resection for hepatocellular carcinoma originating from the noncirrhotic liver. Arch Surg 139:320–325
Llovet JM, Burroughs A, Bruix J (2003) Hepatocellular carcinoma. Lancet 362:1907–1917
Hemming AW, Cattral MS, Reed AI, Van der Werf WJ, Greig PD, Howard RJ (2001) Liver transplantation for hepatocellular carcinoma. Ann Surg 233:652–659
Abdel Wahab M, Sultan A, El-Ghawalby N, Fathy O et al (2004) Hepatic resection in cirrhotic liver for treatment of hepatocellular carcinoma in Egyptian patients: experience with 140 cases in a single center. Hepato-Gastroenterol 51:559–563
Yeh CN, Chen MF, Lee WC, Jeng LB (2002) Prognostic factors of hepatic resection for hepatocellular carcinoma with cirrhosis univariate and multivariate analysis. J Surg Oncol 81:195–202
Nagasue N, Uchida M, Makino Y et al (1993) Incidence and factors associated with intrahepatic recurrence following resection of hepatocellular carcinoma. Gastroenterology 105:488–494
Song T, Edmund Ip W, Fong Y (2004) Hepatocellular carcinoma: current surgical management. Gastroenterology 127:S248–S260
Ibrahim S, Roychowdhury A, Khoon Hean T (2007) Risk factors for intrahepatic recurrence after hepatectomy for hepatocellular carcinoma. Am J Surg 194:17–22
Kaibori M, Saito T, Matsui Y, Uchida Y, Ishizaki M, Kamiyaa Y (2007) A review of the prognostic factors in patients with recurrence after liver resection for hepatocellular carcinoma. Am J Surg 193:431–437
Taura K, Ikai I, Hatamo E, Yasuchika K, Nakajima A et al (2007) Influence of coexisting cirrhosis on outcomes after hepatic resection for hepatocellular carcinoma fulfilling the Milan criteria: an analysis of 293 patients. Surgery 142:685–694
Terminology Committee of the International Hepato-Pancreato-Biliary Association (2000) The Brisbane 2000 terminology of liver anatomy and resections. HPB 2:333–339
Adachi E, Maeda T, Matsumata T et al (1995) Risk factors for intrahepatic recurrence inhuman small hepatocellular carcinoma. Gastroenterology 108:768–775
Kumada T, Nakano S, Takeda I et al (1997) Patterns of recurrence after initial treatment in patients with small hepatocellular carcinoma. Hepatology 25:87–92
Nadig DE, Wade TP, Fairchild RB, Virgo KS, Johnson FE (1997) Major hepatic resection: indications and results in a national hospital system from 1988 to 1992. Arch Surg 132:115–119
Sun HC, Tang ZY (2003) Preventive treatments for recurrence after curative resection of hepatocellular carcinoma—a literature review of randomized control trials. World J Gastroenterol 9:635–640
Imamura H, Matsuyama Y, Tanaka E, Ohkubo T, Hasegawa K, Miyagawa S, Sugawara Y, Minagawa M, Takayama T, Kawasaki S, Makuuchi M (2003) Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol 38:200–207
Poon RT, Fan ST, Ng IO, Lo CM, Liu CL, Wong J (2000) Different risk factors and prognosis for early and late intrahepatic recurrence after resection of hepatocellular carcinoma. Cancer 89:500–507
Ercolani G, Grazi GL, Ravaioli M, Del Gaudio M, Gardini A, Cescon M, Varotti G, Cetta F, Cavallari A (2003) Liver resection for hepatocellular carcinoma on cirrhosis univariate and multivariate analysis of risk factors for intrahepatic recurrence. Ann Surg 237:536–543
Poon RT, Fan ST, Lo CM, Liu CL, Wong J (2002) Long-term survival and pattern of recurrence after resection of small hepatocellular carcinoma in patients with preserved liver function implications for a strategy of salvage transplantation. Ann Surg 235:373–382
Shirabe K, Kanematsu T, Matsumata T, Adachi E, Akazawa K, Sugimachi K (1991) Factors linked to early recurrence of small hepatocellular carcinoma after hepatectomy:univariate and multivariate analyses. Hepatology 14:802–805
Sim GH, Lucien L, Ooi PJ (2003) Results of resections for hepatocellular carcinoma in a new hepatobiliary unit. ANZ J Surg 73:8–13
Jeng K, Sheen I, Tsai Y (2004) Does the presence of circulating hepatocellular carcinoma cells indicate a risk of recurrence after resection? Am J Gastroenterol 99:1503–1509
Portolani N, Coniglio A, Ghidoni S, Giovanelli M, Benetti A, Tiberio G, Giulini S (2006) Early and late recurrence after liver resection for hepatocellular carcinoma: prognostic and theraputic implications. Ann Surg 243:229–235
Yamamoto J, Kosuge T, Takayama T et al (1994) Perioperative blood transfusion promotes recurrence of hepatocellular carcinoma after hepatectomy. Surgery 115:303–309
Matsumata T, Ikeda Y, Hayashi H et al (1993) The association between transfusion and cancer free survival after curative resection for hepatocellular carcinoma. Cancer 72:1866–1871
Makino Y, Yamanoi A, Kimoto T, El-Assal ON, Kohno H, Nagasue N (2000) The influence of perioperative blood transfusion on intrahepatic recurrence after curative resection of hepatocellular carcinoma. Am J Gastroenterol 95:1294–1300
Okuno K, Ozaki M, Shigeoka H et al (1994) Effect of packed red cell and whole blood transfusion on liver-associated immune function. Am J Surg 168:340–344
Yamamoto M, Takasaki K, Ohtsubo T, Katsuragawa H, Fukuda C, Katagiri S (2001) Effectiveness of systematized hepatectomy with Glisson's pedicle transection at the hepatic hilus for small nodular hepatocellular carcinoma: retrospective analysis. Surgery 130(3):443–448
Regimbeau JM, Kianmanesh R, Farges O, Dondero F, Sauvanet A, Belghiti J (2002) Extent of liver resection influences the outcome in patients with cirrhosis and small hepatocellular carcinoma. Surgery 131(3):311–317
The Liver Cancer Study Group of Japan (1990) Primary liver cancer in Japan. Ann Surg 211:277
Ko S, Kanehiro H, Hisanaga M, Nagao M, Ikeda N, Nakajima Y (2002) Liver fibrosis increases the risk of intrahepatic recurrence after hepatectomy for hepatocellularcarcinoma. Br J Surg 89(1):57–62
Jonas S, Bechstein W, Steinmuller T, Hermann M, Radke C, Berg T (2001) Vascular invasion and histopathologic grading determine outcome after liver transplantation for hepatocellular carcinoma in cirrhosis. Hepatology 33:1080–1086
Author information
Authors and Affiliations
Corresponding author
Additional information
Mohamed Abdel-Wahab made substantial contributions to study conception and design and critical revision of the manuscript. Mohamed Shobray and Emad Hamdy are responsible for the acquisition of data. Ehab Elhanafy is responsible for the analysis and interpretation of data. Drafting of manuscript was done by Tarek Salah El-Husseiny.
Rights and permissions
About this article
Cite this article
Abdel-Wahab, M., El-Husseiny, T.S., El Hanafy, E. et al. Prognostic factors affecting survival and recurrence after hepatic resection for hepatocellular carcinoma in cirrhotic liver. Langenbecks Arch Surg 395, 625–632 (2010). https://doi.org/10.1007/s00423-010-0643-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-010-0643-0