Abstract
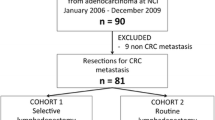
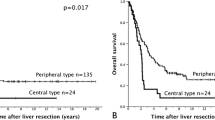
PURPOSE: Lymph node metastasis in the hepatoduodenal ligament is known as one of the most significant prognostic factors after liver resection for colorectal metastasis. However, there have been very few articles on the clinical features of node-positive patients and on detailed distribution of positive nodes. Further, there has been no established strategy on how to handle hepatic lymph nodes during liver resection. To address these subjects, a retrospective study was conducted. METHODS: During the period of 1980 through April 1998, 182 hepatic resections were performed for metastatic colorectal carcinoma. Of these, 78 cases had hepatic lymph node sampling during the operation. Distribution of positive nodes, location of liver metastasis, stage of the primary lesion, and outcome after liver resection were analyzed. RESULTS: Nine cases (12 percent) had secondary lymph node metastases in the hepatoduodenal ligament. The incidence was slightly higher (13.5 percent) in the most recent 44 consecutive cases. There was a tendency for liver metastases in the right lobe to metastasize to No. 12b (or node of the foramen of Winslow, lymph nodes along the common bile duct) and liver metastases in the left lobe to metastasize to No. 8a (anterosuperior group of the lymph nodes along the common hepatic artery). Outcome of node-positive patients (n=9) was extremely poor (P<0.001) compared with that of node-negative patients (n=66), and the most common site of recurrence in the node-positive patients was remnant liver and hepatic lymph nodes. Preoperatively, there were no significant predicting factors for positive hepatic lymph nodes. CONCLUSIONS: No. 8a and No. 12b nodes are principal nodes that should be palpated and sampled during liver resection to check the secondary lymphatic spread from liver metastases. Hepatic nodal involvement indicates the progression of disease beyond simple liver metastases and may not be the indication for simple surgical removal. Further study, including hepatoduodenal dissection and systemic adjuvant chemotherapy, may elucidate the survival benefit, if any, of liver resection in node-positive patients.
Similar content being viewed by others
References
Hughes KS, Simon R, Songhorabodi S. resection of the liver for colorectal carcinoma metastases: a multi-institutional study of patterns of recurrence. Surgery 1986;100:27884.
Cady B, Stone MD, McDermott WV,et al. Technical and biological factors in disease-free survival after hepatic resection for colorectal cancer metastasis. Arch Surg 1992;127:561–569.
Ekberg H, Tranberg K-G, Andersson R,et al. Pattern of recurrence in liver resection for colorectal secondaries. World J Surg 1987;11:541–7.
Rosen CB, Nagorney DM, Taswell HF,et al. Perioperative blood transfusion and determinants of survival after liver resection for metastatic colorectal carcinoma. Ann Surg 1992;216:493–505.
Scheele J, Stang R, Altendorf-Hofmann A, Paul M. Resection of colorectal liver metastases. World J Surg 1995;19:59–71.
Wang JY, Chiang J-M, Jeng L-B, Changchien CR, Chen JS, Hsu KC. Resection of liver metastases from colorectal cancer: are there any truly significant clinical prognosticators? Dis Colon Rectum 1996;39:847–51.
Beckurts KT, Holscher AH, Thorban ST, Bollschweiler E, Siewert JR. Significance of lymph node involvement at the hepatic hilum in the resection of colorectal liver metastases. Br J Surg 1997;84:1081–4.
Nakamura S, Yokoi Y, Suzuki S, Baba S, Muro H. Results of extensive surgery for liver metastasis in colorectal carcinoma. Br J Surg 1992;79:35–8.
Nishi M, Omori Y, Miwa K, eds. Japanese Research Society for Gastric Cancer. Japanese classification of gastric carcinoma. 1st English ed. Tokyo: Kanehara, 1995.
Miyazaki I, ed. Japanese Society of Biliary Surgery. General rules for surgical and pathological studies on cancer of biliary tract [in Japanese]. 3rd ed. Tokyo: Kanehara, 1993.
Sobin LH, Wittekind Ch (International Union Against Cancer), eds. TNM classification of malignant tumours. 5th ed. New York: John Wiley & Sons, 1997,
Trutmann M, Sasse D. The lymphatics of the liver. Anat Embryol 1994;190:201–9.
August DA, Sugarbaker PH, Schneider PD. Lymphatic dissemination of hepatic metastasis. Implications for the follow-up and treatment of patients with colorectal cancer. Cancer 1984;55:1490–4.
Wolodjko WP. Das Lymphsystem der menschlichen Leber in Beziehung zu ihrer Segmentgliederung. Z Anat Entwicklungsg 1967;126:154–71.
Clermont D. Lymphatiques des voies biliaires: cancer de la vesicule (anatomie pathologique et traitement chirurgical). Toulouse: 1909.
Fahin RB, McDonald JR, Richards JC, Ferris DO. Carcinoma of the gallbladder: a study of its mode of spread. Ann Surg 1962;156:114–24.
Ito M, Mishima Y, Sato T. An anatomical study of the lymphatic drainage of the gallbladder. Surg Radiol Anat 1991;13:89–104.
Watanabe J, Nakashima O, Kojiro M. Clinicopathologic study on lymph node metastasis of hepatocellular carcinoma: a retrospective study of 660 consecutive autopsy cases. Jpn J Clin Oncol 1994;24:37–41.
Une Y, Misawa K, Shimamura T,et al. Treatment of lymph node recurrence in patients with hepatocellular carcinoma. Surg Today 1994;24:606–9.
Elias D, Saric J, Jaeck D. Prospective study of microscopic lymph node involvement of the hepatic pedicle during curative hepatectomy for colorectal metastases. Br J Surg 1996;83:942–5.
Chang A, Schneider PD, Sugarbaker PH, Simpson C, Culnane M, Steinberg SM. A prospective randomized trial of regional versus systemic continuous 5-fluorode-oxyuridine chemotherapy in the treatment of colorectal liver metastases. Ann Surg 1987;206:685–93.
Adson MA. Resection of liver metastases—when is it worthwhile? World J Surg 1987;11:511–20.
Author information
Authors and Affiliations
About this article
Cite this article
Kokudo, N., Sato, T., Seki, M. et al. Hepatic lymph node involvement in resected cases of liver metastases from colorectal cancer. Dis Colon Rectum 42, 1285–1290 (1999). https://doi.org/10.1007/BF02234215
Issue Date:
DOI: https://doi.org/10.1007/BF02234215