Abstract
Although the incidence of some malignancy has decreased over the recent years, this is not the case of papillary thyroid microcarcinoma (PTMC), whose incidence has increased worldwide. Most PTMC are found incidentally after histological examination of specimens from surgery for benign thyroid disease. Hashimoto’s thyroiditis, whose incidence has also increased, coexists in about one in three PTMC patients. Three different mechanisms have been proposed to clarify the association between chronic lymphocytic thyroiditis and PTMC, namely tumor development/growth by: (i) TSH stimulation, (ii) expression of certain proto-oncogenes, (iii) chemokines and other molecules produced by the lymphocytic infiltrate. Whether Hashimoto’s thyroiditis protects against lymph node metastasis is debated. Overall, autommune thyroiditis seems to contribute to the favorable prognosis of PTMC. Major limitations of the studies so far performed include: (i) retrospective design, (ii) limited statistical power, (iii) high risk of selection bias, (iv) and predominant Asian ethnicity of patients. Full genetic profiling of both diseases and identification of environmental factors capable to trigger them, as well as well-powered prospective studies on different ethnical groups, may help understand their causal association and why their frequencies are continuing raising.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 General aspects
Papillary thyroid carcinoma (PTC) accounts for at least 70% of thyroid malignancies. According to the largest diameter, microcarcinomas (i.e. ≤1 cm, PTMC) are distinguished from macrocarcinomas (>1 cm) [1]. Although the incidence of certain malignancies has decreased over the recent years, this is not the case of PTC, whose incidence has increased worldwide [2,3,4,5]. Indeed, most of this upward trend results from PTMC, which account for up to 43% of the newly diagnosed PTC [6]. The reason for this trend is multifactorial. Three causes have been pinpointed: widespread use of ultrasonography and consequent detection of thyroid micronodules, widespread use of ultrasonography-guided fine-needle aspiration cytology (FNAC), and detailed histopathological examination of specimens after thyroidectomy [7]. PTMC is often found incidentally after histological examination of specimens from surgery for benign thyroid disease or from autopsy, and therefore is also called “occult” carcinoma [8, 9].
In an American study based on data of a national program from nine registries, PTMC accounted for 49% (95%CI = 47–51%) of the increase in PTC incidence from 1988 to 2002 [10]. Londero et al. demonstrated that the crude incidence of PTMC in Denmark doubled over 12 years (from 0.35 per 100,000 per year in 1996 to 0.74 per 100,000 per year in 2008), and about two-thirds (62%) of PTMC were diagnosed incidentally [11]. Compared with the nonincidental PTMC (i.e. diagnosis based on FNAC), the incidental ones were diagnosed in older patients, were less frequently found in male patients, were smaller, less frequently multifocal and extended outside the thyroid [11]. In a Chinese retrospective study from eight cancer registries, the reported proportion of PTMC was zero in the timespan 1972–1985, but 32% in the timespan 2000–2014 [12].
Hashimoto’s thyroiditis (also known as chronic lymphocytic thyroiditis or autoimmune thyroiditis) is the most common thyroid disorder, and its prevalence has raised by 8-fold over the last decades [4, 13, 14]. The increasing incidence of Hashimoto’s thyroiditis and PTC/PTMC led several authors to ascertain whether or not the first disease predisposes to the second [15,16,17,18,19]. Following the first report by Dailey in 1955 [20], accompanying chronic lymphocytic thyroiditis (consisting of lymphocytic cell infiltration, oxyphilic cells, lymphoid follicles, and reactive germinal centers) in histological specimens of PTC, was shown to range from 10% to 58% of cases [7, 21, 22].
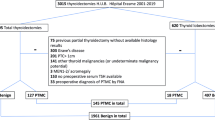
Table 1 summarizes original studies addressing the frequency of Hashimoto’s thyroiditis in PTMC patients or the frequency of PTMC in Hashimoto’s thyroiditis patients.
In a Serbian retrospective study on 2466 patients who underwent thyroid surgery for presumed benign thyroid disease from 2008 to 2013, the overall incidence of PTMC was 16.3%, but was significantly greater (22.7%, χ2 = 10.80, P < 0.001) among patients with histological findings of Hashimoto’s thyroiditis [2]. Accordingly, Hashimoto’s thyroiditis was an independent predictor of PTMC (OR = 1.54, 95%CI = 1.15–2.05, P < 0.003) at the multivariate logistic regression model [2]. In other two series, the rate of PTMC was even greater (39%) [1, 34]. In a Chinese retrospective, case-control study on 927 PTMC patients and 927 sex- and age-matched controls selected from participants of a cross-sectional study performed in the same population, the rate of thyroglobulin antibody (TgAb) or thyroperoxidase antibody (TPOAb) positivity was 23.4% or 18.4% in patients, as compared with the corresponding rates of 12.0% (P = 0.001) or 12.7% (P < 0.001) in controls [15]. Positivity of either antibody resulted in a two-fold increased risk of PTMC (OR = 1.9), this risk being even greater in patients aged 18–30 years (OR = 11.5). The major limitation of this study was that duration of Hashimoto’s thyroiditis was not assessed [15].
Very recently, we reported histological evidence of Hashimoto’s thyroiditis in 168/505 (33.3%) PTC specimens [23]. This rate was very similar to that reported in a Turkish study on 919 PTC cases (34.5%) [7], and in a Chinese study on 1250 PTC cases (29.1%) [26], but it was higher compared to that reported by a recent Danish study on 11,155 PTC cases (18.9%) [19]. In our series, when Hashimoto’s thyroiditis coexisted, the average size of PTC was <1 cm, and was about 3 mm smaller compared with specimens in which Hashimoto’s thyroiditis was absent (9.39 ± 6.10 vs. 321 12 ± 9.71 mm, P = 0.002) [23]. In the Turkish study mentioned above, about two-thirds (874/1321) of the papillary lesions were ≤ 1 cm, and among them, those with coexistent autoimmune thyroiditis were significantly smaller compared to those without it (3.84 ± 2.33 mm vs. 4.24 ± 2.52 mm, P = 0.026) [7].
Finally, a number of studies have also reported an increased prevalence of Hashimoto’s thyroiditis and PTC in patients with nonthyroid autoimmune diseases, such as systemic lupus erythematosus [37], systemic sclerosis [38, 39], and hepatitis C virus-associated mixed cryoglobulinemia syndrome [40, 41], suggesting that the sustained activation of the immune system in these patients may lead to autoimmune thyroiditis, and in turn, to PTC. Indeed, in both chronic lymphocytic thyroiditis and PTC unbalance of T-lymphocytes populations, namely overactivation of the T-helper 1 lymphocytes, was demonstrated [41]. These cells secrete interferon-γ, which in turn induces the secretion of interferon-γ chemokines (CXCL9, CXCL10, CXCL11) by thyrocytes, hence perpetuating the autoimmne process [41].
2 Pathogenesis of the association
Three different mechanisms have been proposed to clarify the association between chronic lymphocytic thyroiditis and PTMC, namely tumor development/growth by: (i) TSH stimulation, (ii) expression of certain proto-oncogenes, (iii) chemokines and other molecules produced by the lymphocytic infiltrate.
TSH plays a pivotal role in regulating growth and differentiation of thyrocytes by its binding with TSH receptor, and via other growth factors expression, such as the epidermal growth factor, the insulin-like growth factor, and insulin [42, 43]. Concerning thyroid cancer, TSH may play a causal role in cancer growth rather than in its initiation [44, 45]. Indeed, lowering serum TSH levels (i.e. TSH suppression) by levothyroxine is part of differentiated thyroid cancer treatment in intermediate to high risk patients [46].
Two recent meta-analyses have shown that preoperative serum TSH is a risk factor for thyroid cancer, and that the higher TSH the higher the risk of malignancy [47, 48]. In particular, in the meta-analysis by Zheng et al., which is the largest one performed so far (56 studies and over 20,000 thyroid cancer cases included), the positive association between TSH levels and likelihood of thyroid cancer was maintained regardless of the tumor size [48]. Concerning PTMC, 6 out of 28 studies meta-analyzed by McLeod [49] focused on serum TSH levels. Three studies found at least one positive correlation between TSH levels and adverse prognostic indicators. Unfortunately, because of the small number of cases, results were inconsistent [49]. Another three studies did not find any significant difference in preoperative TSH between patients with PTMC and those with benign nodular goiter [50,51,52].
Fiore et al. demonstrated that serum TSH levels are significantly higher in patients with PTC compared with those with benign nodular disease, and in thyroid antibody-positive patients compared with antibody-negative patients [53]. More recently, it was found that TSH levels ≥2.26 mU/L are associated with a three-fold higher risk of malignancy [54]. Conversely, subnormal TSH levels (< 0.4 mU/L) protect against the risk of PTC [53].
A South Korean study demonstrated that malignancy rate of thyroid micronodules was higher in euthyroid patients (n = 315, 10.8%) with serum TSH above the population mean (≥1.37 mU/L) compared to those with serum TSH below the population mean (n = 168, 4.8%, P = 0.025). Both univariate and multivariate logistic regression revealed that TSH levels were a risk factor for thyroid malignancy [55]. A very recent Turkish retrospective study, investigated the association between preoperative TSH levels and clinicopathological features of PTC >1 cm (n = 279), PTMC (n = 384), and benign nodular disease (n = 969) [45]. The authors found that median serum TSH was the highest in patients with PTC >1 cm (1.57 mU/L), higher in patients with PTMC (1.30 mU/L), and the lowest in benign patients (0.98 mU/L, P < 0.001 for all comparisons). Also, TPOAb and TgAb positivity rate, and lymphocytic thyroiditis was greater in patients having malignant thyroid disease (PTC >1 cm and PTMC) compared with patients having benign thyroid disease [45]. Upon excluding TPOAb and/or TgAb positive patients and those with autoimmune thyroiditis from the analysis, patients with either PTMC or PTC >1 cm had significantly greater TSH levels compared with those with benign histopathology, with a 1.3-fold increase of malignancy risk for each 1 mU/L increase in serum TSH. Finally, there was no difference in serum TSH according to the size of the malignant lesion. The authors concluded that serum TSH increases the malignancy risk regardless of autoimmunity [45]. Qu demonstrated that preoperative serum TSH in PTMC patients is significantly higher in presence of autoimmune thyroiditis than in absence of it (2.39 ± 1.92 vs. 2.0 ± 1.45 mU/L, P = 0.001) [26]. However, TSH level does not correlate with pathologic features of the tumor such as size, bilaterality, multifocality, and extrathyroidal extension [26].
Whether thyroid autoimmunity is the cause or the consequence of thyroid cancer is still debated. On one hand, neoplastic cells trigger chronic inflammatory response aimed at destroying cancer cells [26]. For instance, Fas pathway activation together with IL-1 and cytotoxic T cells, either directly or indirectly, suppress cancer cells growth and promote their apoptosis [56, 57]. On the other hand, the inflammation-induced mileu consisting of growth factors, chemokines, cytokines, and metalloproteinases fuels cancer cell proliferation [58]. In addition, environmental triggers may promote cancer cell growth [59,60,61,62].
A number of molecular markers have been investigated in PTMC in the past years. BRAF(V600E)/TPO-Cre mice, in which the oncogene BRAFV600E was knocked-in, develop severe hypothyroidism together with a short-latence, invasive PTC [63]. Upon crossing these mice with TSH receptor knockout mice, resulting mice [BRAF(V600E)/TPO-Cre/Gnas-E1(fl/fl)] have PTC with attenuated phenotype, namely smaller and less invasive tumors, which resemble the indolent PTMC that are commonly encountered in humans [63]. Finally, suppression of TSH in mice with wild-type TSH receptor [BRAF(V600E)/TPO-Cre] does not revert cancer phenotype. These pioneering experiments demonstrate that the higher TSH the higher the risk of larger, aggressive malignancies [63].
BRAF mutations are found in up to half of PTMC cases, with the highest frequency in the tall cell variant and in the sclerosing variant [64, 65], and associate with tumor aggressiveness (large tumor size, extrathyroidal extension, multifocality, lymph nodal metastasis, and advanced stage) [64, 66]. Jung reported that the frequency of BRAF-mutated PTMC did not change over the timespan 1974–2009, confirming that the growing incidence of PTMC is not only derived from detection of incidental, nonprogressing tumors, given that BRAF mutations occur mainly in aggressive, progressing tumors [67]. Interestingly, BRAF mutations rate is significantly lower in PTMC compared with PTC [68]. The presence of concomitant autoimmune thyroiditis is associated with a lower prevalence of BRAF mutations in PTC [25]. Moreover, Marotta showed that concurrent lymphocytic infiltration of Hashimoto’s thyroiditis is a protective factor against PTC progression, regardless of BRAF status [69]. Finally, a meta-analysis that evaluated clinico-pathological features of PTMC in relation to BRAF V600E status, found that the latter did not correlate with accompanying Hashimoto’s thyroiditis [70].
RET/PTC rearrangements (−1, −2 and − 3), resulting in aberrant activity of RET protein tyrosine kinase receptor, transform thyrocytes in culture, and give rise to thyroid carcinoma in transgenic mice, recapitulating microscopic features of human PTC [71]. Tallini reported that RET activation, which was found in 81/201 (40.3%) PTC, correlated with tumors exhibiting features of the classic variant PTC or with PTMC (P = 0.017) [72]. About 40% of PTMC harbor RET/PTC rearrangements, but it is not clear whether their prevalence in PTMC is higher compared with PTC [73, 74]. Similarly to BRAF mutations, RET/PTC rearrangements are more frequent in PTC with aggressive phenotype and in aggressive variants of PTC [75, 76]. Furthermore, both BRAF mutations and RET/PTC rearrangements are capable to trigger proinflammatory programmes in thyrocytes [17], and in turn, BRAF and RET expression is enhanced in oxyphil cell metaplasia in Hashimoto’s thyroiditis specimens [77].
Other molecular markers of PTC/PTMC aggressiveness, such as cyclin D1 and galectin-3, have been also studied in Hashimoto’s thyroiditis, but their impact on prognosis of cancer patients in whom PTC/PTMC and Hashimoto’s thyroiditis coexist is still unknown [78,79,80].
3 Histopathological aspects
In general, PTMC is associated with a favorable prognosis, and its course is indolent, the reported mortality being <0.5% [81]. Indeed, in autopsy series the frequency of PTMC is up to 36% [82]. Accompanying Hashimoto’s thyroiditis may also contribute to the favorable prognosis, as it may protect against cancer progression [36, 83, 84] and aggressiveness [7] (see 2. Pathogenetical aspects).
Nevertheless, at the time of thyroidectomy, 15–40% of PTMC patients have extrathyroidal involvement, mainly lymph node metastasis [9, 85], and very rarely (0.3%) distant metastases [5]. Lymph node metastases, most frequently involving the central compartment (VI level), are frequently occult, namely found at histological examination in absence of clinical evidence at physical examination and ultrasonography [27]. According to the “nodes beget nodes” concept, nodal involvement is considered a predictor of cancer recurrence and is associated with a poor prognosis [5], as demonstrated in a Danish registry study [11]. In this study, lymph node metastasis was the only risk factor affecting significantly the recurrence-free survival of PTMC patients [11].
Baser et al. reported a higher number of lymph node metastases in PTC patients without histopathological signs of autoimmune thyroiditis compared to those with them (581 metastases in 879 patients vs. 312 in 442, P = 0.012) [7]. This difference was confirmed when considering only PTMC (329 in 594 vs. 162 in 280, P = 0.015) [7]. In a large retrospective study on over 5000 PTMC the authors found that male gender, conventional variant, tumor size >5 mm, bilaterality and extrathyroidal extension predicted central lymph node involvement, but per 10-years age increment and histologically proven chronic lymphoctytic thyroiditis protected against VI level metastasis [35]. Zhang et al. evaluated 178 patients with PTMC who had undergone prophylactic VI level dissection [27]. Occult metastases were found less frequently in Hashimoto’s thyroiditis patients compared with patients without signs of thyroiditis (17.8% vs. 27.6%), this difference being nonsignificant [27]. Recently, Yu et al. found a trendwise significant negative association between TPOAb positivity and VI level metastasis (OR = 0.998, P = 0.08) in 917 PTMC [86]. A large meta-analysis by Qu on 21 retrospective studies and 4 prospective studies including over 7000 patients found that age > 45 years and lymphocytic thyroiditis protected against central nodes metastasis (OR = 0.65 and OR = 0.70, respectively), whereas male gender, tumor size >5 mm, multifocality, capsular invasion, extrathyroidal extension, lymphovascular invasion, and lateral lymph node metastasis, were associated to VI level involvement [87].
Yet, other studies found neither difference in the rate of central lymph node metastasis in patients with and without autoimmune thyroiditis nor any influence of autoimmune thyroiditis in the risk of central lymph node involvement [1, 28]. In a Turkish retrospective study on 141 PTMC and 82 PTC >1 cm, sex, age, tumor size, multifocality, bilaterality, extrathyroidal extension, clinical suspicion, and chronic lymphocytic thyroiditis did not predict VI level metastasis at multivariate logistic regression analysis [24]. Similarly, Li et al. showed that Hashimoto’s thyroiditis was neither a positive nor a negative predictor of central lymph node involvement in a series of 273 PTMC cases [29]. These findings were consistent with those by Kim et al. [31], although in metastatic patients, multifocality and bilaterality were more frequent in those with autoimmune thyroiditis compared to those without it (44.4% vs. 29.2%, and 29.6% vs. 14.6%) [31].
The lack of association between Hashimoto’s thyroiditis and central lymph node metastasis was confirmed by a meta-analysis on six studies including 1668 Asian PTMC patients without clinically cervical lymph node metastasis [88]. Importantly, significant heterogeneity between studies was found (I2 = 62.4%, P = 0.021) [88]. These findings were consistent with those of a larger meta-analysis on 14 studies, six of which evaluated the incidence of central node metastasis in PTMC with and without autoimmune thyroiditis [89]. Furthermore, a recent Chinese study reported no association between Hashimoto’s thyroiditis and both central and lateral lymph node metastasis [26].
Another factor influencing thyroid cancer prognosis is size. A number of studies have shown that larger PTMC are more aggressive compared to smaller PTMC, suggesting tailored therapeutic approach according to the tumor size. Indeed, different largest diameters (5 mm [32, 90], 6 mm [32], or 7 mm [91]) have been proposed as cut-off thresholds to distinguish larger, aggressive PTMC from smaller, indolent PTMC. In this regard, Hashimoto’s thyroiditis does not influence PTMC size [32, 90].
4 Discussion
PTMC is considered a well-differentiated, slow-growing, indolent tumor. It is still debated whether the concomitant increase in PTMC and Hashimoto’s thyroiditis incidence over the last years is true or stems from increased interest in these diseases, access to improved diagnostic tools (such as FNAC, ultrasonography and thyroid antibodies assays), and/or increased environmental factors capable to trigger these diseases [4, 13, 74, 92, 93]. Major limitations of the studies so far performed include: (i) retrospective design, (ii) limited statistical power, (iii) high risk of selection bias, (iv) and predominant Asian ethnicity of patients.
Detection and characterization of small nodules by ultrasonography in the context of inhomogeneous echotexture such as in autoimmune thyroiditis is challenging [94]. For this purpose, elastosonography has been proposed to help discriminate low-suspicion nodules from high-suspicion nodules. Li et al. evaluated the stiffness of 558 micronodules by measuring their strain ratio by elastosonography, namely reference tissue strain divided by lesion strain [95]. The higher the strain ratio the harder the nodule compared to surrounding thyroid parenchyma, with harder nodules having greater chances of being malignant. Strain ratio measurements were lower in the 181 malignant nodules coexisting with Hashimoto’s thyroiditis compared with the 377 such nodules without Hashimoto’s thyroiditis. Also, strain ratio correlated inversely with TPOAb titer [95].
Even though PTMC is considered the initial stage of macrocarcinoma, as both share a number of biological, molecular and histological features, there is mounting evidence that some tumors grow slowly and remain quiescent for many years, while others show aggressive behavior [96]. Therefore, certain tumor features at diagnosis have been proposed to guide the subsequent therapeutic approach.
About one in three PTMC patients have lymph node metastasis, either central or lateral, irrespective of coexisting chronic lymphocytic thyroiditis [88]. However, ultrasonography has a relatively low sensitivity in detecting lymph node metastasis, which has been estimated at around 40% for VI level lymph nodes ≥5 mm [86, 97]. Therefore, at least two-thirds of such patients may not be diagnosed preoperatively. Also, the risk of node involvement and multifocality is higher in larger papillary microcarcinomas (>5 mm) [34, 98]. In light of these findings, although the recent American Thyroid Association guidelines recommend central lymph node dissection only in case of either clinically evidence of lymph node metastasis (cN1) or uninvolved lymph nodes (cN0) with advanced primary tumor (T3 or T4 stage) [46], prophylactic VI level dissection has been proposed for high-risk patients, namely those with large, bilateral, multifocal tumors, those with nonclassic variants, and for young patients [24, 29, 75, 86, 87, 89]. Whether autoimmune thyroiditis is associated with a less frequent nodal involvement in PTMC patients is debated. While some papers found an apparent association [7, 80], others showed no difference in VI level involvement [1, 24, 28, 29].
At diagnosis, advanced stage and aggressive tumors are associated also to higher levels of serum TSH [45]. It is unclear whether high TSH levels per se or underlying autoimmunity, are capable to predispose to PTC. Indeed, Kim and Park have shown that TSH levels, even in the normal range, correlate positively with an advanced TNM stage regardless of autoimmune thyroiditis [99].
In conclusion, PTMC and Hashimoto’s incidence has risen obviously over the last decades. The contribution of Hashimoto’s thyroiditis on biological behavior of PTMC is still controversial, given that accompanying Hashimoto’s thyroiditis might be not powerful enough to improve PTMC outcome significantly. Full genetic profiling of both diseases and identification of environmental factors capable to trigger them, as well as well-powered prospective studies on different ethnical groups, may help understand their causal association and why their frequencies are continuing raising.
References
Bircan HY, Koc B, Akarsu C, Demiralay E, Demirag A, Adas M, et al. Is Hashimoto's thyroiditis a prognostic factor for thyroid papillary microcarcinoma? Eur Rev Med Pharmacol Sci. 2014;18(13):1910–5.
Slijepcevic N, Zivaljevic V, Marinkovic J, Sipetic S, Diklic A, Paunovic I. Retrospective evaluation of the incidental finding of 403 papillary thyroid microcarcinomas in 2466 patients undergoing thyroid surgery for presumed benign thyroid disease. BMC Cancer. 2015;15:330. https://doi.org/10.1186/s12885-015-1352-4.
Rizzo M, Sindoni A, Talamo Rossi R, Bonaffini O, Panetta S, Scisca C, et al. Annual increase in the frequency of papillary thyroid carcinoma as diagnosed by fine-needle aspiration at a cytology unit in Sicily. Hormones. 2013;12(1):46–57.
Latina A, Gullo D, Trimarchi F, Benvenga S. Hashimoto's thyroiditis: similar and dissimilar characteristics in neighboring areas. Possible implications for the epidemiology of thyroid cancer. PloS One. 2013;8(3):e55450. https://doi.org/10.1371/journal.pone.0055450.
Hay ID, Hutchinson ME, Gonzalez-Losada T, McIver B, Reinalda ME, Grant CS, et al. Papillary thyroid microcarcinoma: a study of 900 cases observed in a 60-year period. Surgery. 2008;144(6):980–7; discussion 7–8. https://doi.org/10.1016/j.surg.2008.08.035.
Lin JD, Kuo SF, Chao TC, Hsueh C. Incidental and nonincidental papillary thyroid microcarcinoma. Ann Surg Oncol. 2008;15(8):2287–92. https://doi.org/10.1245/s10434-008-9958-2.
Baser H, Ozdemir D, Cuhaci N, Aydin C, Ersoy R, Kilicarslan A, et al. Hashimoto's thyroiditis does not affect ultrasonographical, cytological, and histopathological features in patients with papillary thyroid carcinoma. Endocr Pathol. 2015;26(4):356–64. https://doi.org/10.1007/s12022-015-9401-8.
Yu XM, Wan Y, Sippel RS, Chen H. Should all papillary thyroid microcarcinomas be aggressively treated? An analysis of 18,445 cases. Ann Surg. 2011;254(4):653–60. https://doi.org/10.1097/SLA.0b013e318230036d.
Lin JD. Increased incidence of papillary thyroid microcarcinoma with decreased tumor size of thyroid cancer. Med Oncol. 2010;27(2):510–8. https://doi.org/10.1007/s12032-009-9242-8.
Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA. 2006;295(18):2164–7. https://doi.org/10.1001/jama.295.18.2164.
Londero SC, Krogdahl A, Bastholt L, Overgaard J, Trolle W, Pedersen HB, et al. Papillary thyroid microcarcinoma in Denmark 1996–2008: a national study of epidemiology and clinical significance. Thyroid : official journal of the American Thyroid Association. 2013;23(9):1159–64. https://doi.org/10.1089/thy.2012.0595.
Du L, Wang Y, Sun X, Li H, Geng X, Ge M, et al. Thyroid cancer: trends in incidence, mortality and clinical-pathological patterns in Zhejiang Province, Southeast China. BMC Cancer. 2018;18(1):291. https://doi.org/10.1186/s12885-018-4081-7.
Benvenga S, Trimarchi F. Changed presentation of Hashimoto's thyroiditis in North-Eastern Sicily and Calabria (Southern Italy) based on a 31-year experience. Thyroid : official journal of the American Thyroid Association. 2008;18(4):429–41. https://doi.org/10.1089/thy.2007.0234.
Rizzo M, Rossi RT, Bonaffini O, Scisca C, Altavilla G, Calbo L, et al. Increased annual frequency of Hashimoto's thyroiditis between years 1988 and 2007 at a cytological unit of Sicily. Ann Endocrinol. 2010;71(6):525–34. https://doi.org/10.1016/j.ando.2010.06.006.
Liu Y, Li C, Zhao W, Wang Y. Hashimoto's thyroiditis is an important risk factor of papillary thyroid microcarcinoma in younger adults. Horm Metab Res = Hormon- und Stoffwechselforschung = Hormones et metabolisme. 2017;49(10):732–8. https://doi.org/10.1055/s-0043-117892.
Chen YK, Lin CL, Cheng FT, Sung FC, Kao CH. Cancer risk in patients with Hashimoto's thyroiditis: a nationwide cohort study. Br J Cancer. 2013;109(9):2496–501. https://doi.org/10.1038/bjc.2013.597.
Guarino V, Castellone MD, Avilla E, Melillo RM. Thyroid cancer and inflammation. Mol Cell Endocrinol. 2010;321(1):94–102. https://doi.org/10.1016/j.mce.2009.10.003.
Singh B, Shaha AR, Trivedi H, Carew JF, Poluri A, Shah JP. Coexistent Hashimoto's thyroiditis with papillary thyroid carcinoma: impact on presentation, management, and outcome. Surgery. 1999;126(6):1070–6 discussion 6–7.
Resende de Paiva C, Gronhoj C, Feldt-Rasmussen U, von Buchwald C. Association between Hashimoto's thyroiditis and thyroid cancer in 64,628 patients. Front Oncol. 2017;7:53. https://doi.org/10.3389/fonc.2017.00053.
Dailey ME, Lindsay S, Skahen R. Relation of thyroid neoplasms to Hashimoto disease of the thyroid gland. AMA Arch Surg. 1955;70(2):291–7.
Tamimi DM. The association between chronic lymphocytic thyroiditis and thyroid tumors. Int J Surg Pathol. 2002;10(2):141–6. https://doi.org/10.1177/106689690201000207.
Melcescu E, Horton WB, Pitman KT, Vijayakumar V, Koch CA. Euthyroid Graves' orbitopathy and incidental papillary thyroid microcarcinoma. Hormones. 2013;12(2):298–304.
Ieni A, Vita R, Magliolo E, Santarpia M, Di Bari F, Benvenga S, et al. One-third of an archivial series of papillary thyroid cancer (years 2007–2015) has coexistent chronic lymphocytic thyroiditis, which is associated with a more favorable tumor-node-metastasis staging. Front Endocrinol. 2017;8:337. https://doi.org/10.3389/fendo.2017.00337.
Akin S, Yazgan Aksoy D, Akin S, Kilic M, Yetisir F, Bayraktar M. Prediction of central lymph node metastasis in patientswith thyroid papillary microcarcinoma. Turk J Med Sci. 2017;47(6):1723–7. https://doi.org/10.3906/sag-1702-99.
Lim JY, Hong SW, Lee YS, Kim BW, Park CS, Chang HS, et al. Clinicopathologic implications of the BRAF(V600E) mutation in papillary thyroid cancer: a subgroup analysis of 3130 cases in a single center. Thyroid : official journal of the American Thyroid Association. 2013;23(11):1423–30. https://doi.org/10.1089/thy.2013.0036.
Qu N, Zhang L, Lin DZ, Ji QH, Zhu YX, Wang Y. The impact of coexistent Hashimoto's thyroiditis on lymph node metastasis and prognosis in papillary thyroid microcarcinoma. Tumour Biol : the journal of the International Society for Oncodevelopmental Biology and Medicine. 2016;37(6):7685–92. https://doi.org/10.1007/s13277-015-4534-4.
Zhang LY, Liu ZW, Liu YW, Gao WS, Zheng CJ. Risk factors for nodal metastasis in cN0 papillary thyroid microcarcinoma. Asian Pac J Cancer Prev : APJCP. 2015;16(8):3361–3.
Yang Y, Chen C, Chen Z, Jiang J, Chen Y, Jin L, et al. Prediction of central compartment lymph node metastasis in papillary thyroid microcarcinoma. Clin Endocrinol. 2014;81(2):282–8. https://doi.org/10.1111/cen.12417.
Li M, Zhu XY, Lv J, Lu K, Shen MP, Xu ZL, et al. Risk factors for predicting central lymph node metastasis in papillary thyroid microcarcinoma (CN0): a study of 273 resections. Eur Rev Med Pharmacol Sci. 2017;21(17):3801–7.
Choi SY, Park H, Kang MK, Lee DK, Lee KD, Lee HS, et al. The relationship between the BRAF(V600E) mutation in papillary thyroid microcarcinoma and clinicopathologic factors. World J Surg Oncol. 2013;11:291. https://doi.org/10.1186/1477-7819-11-291.
Kim HS, Choi YJ, Yun JS. Features of papillary thyroid microcarcinoma in the presence and absence of lymphocytic thyroiditis. Endocr Pathol. 2010;21(3):149–53. https://doi.org/10.1007/s12022-010-9124-9.
Lai X, Zhang B, Jiang Y, Li J, Zhao R, Yang X, et al. Sonographic and clinical features of papillary thyroid microcarcinoma less than or equal to five millimeters: a retrospective study. PloS One. 2016;11(2):e0148567. https://doi.org/10.1371/journal.pone.0148567.
Giordano D, Gradoni P, Oretti G, Molina E, Ferri T. Treatment and prognostic factors of papillary thyroid microcarcinoma. Clin Otolaryngol : official journal of ENT-UK ; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery. 2010;35(2):118–24. https://doi.org/10.1111/j.1749-4486.2010.02085.x.
Fu X, Lou S, Shi H, Liu Q, Chen Z, Zhou Y. Clinicopathologic analysis of 254 cases of papillary thyroid microcarcinoma. Zhonghua bing li xue za zhi = Chin J Pathol. 2015;44(4):258–61.
Kim SK, Park I, Woo JW, Lee JH, Choe JH, Kim JH, et al. Predictive Factors for Lymph Node Metastasis in Papillary Thyroid Microcarcinoma. Ann Surg Oncol. 2016;23(9):2866–73. https://doi.org/10.1245/s10434-016-5225-0.
Noguchi S, Yamashita H, Uchino S, Watanabe S. Papillary microcarcinoma. World J Surg. 2008;32(5):747–53. https://doi.org/10.1007/s00268-007-9453-0.
Ferrari SM, Elia G, Virili C, Centanni M, Antonelli A, Fallahi P. Systemic lupus erythematosus and thyroid autoimmunity. Front Endocrinol. 2017;8:138. https://doi.org/10.3389/fendo.2017.00138.
Antonelli A, Ferri C, Ferrari SM, Di Domenicantonio A, Giuggioli D, Galleri D, et al. Increased risk of papillary thyroid cancer in systemic sclerosis associated with autoimmune thyroiditis. Rheumatology. 2016;55(3):480–4. https://doi.org/10.1093/rheumatology/kev358.
Fallahi P, Ruffilli I, Giuggioli D, Colaci M, Ferrari SM, Antonelli A, et al. Associations between systemic sclerosis and thyroid diseases. Front Endocrinol. 2017;8:266. https://doi.org/10.3389/fendo.2017.00266.
Ferri C, Colaci M, Fallahi P, Ferrari SM, Antonelli A, Giuggioli D. Thyroid involvement in hepatitis C virus-infected patients with/without mixed cryoglobulinemia. Front Endocrinol. 2017;8:159. https://doi.org/10.3389/fendo.2017.00159.
Antonelli A, Ferrari SM, Corrado A, Di Domenicantonio A, Fallahi P. Autoimmune thyroid disorders. Autoimmun Rev. 2015;14(2):174–80. https://doi.org/10.1016/j.autrev.2014.10.016.
Burikhanov R, Coulonval K, Pirson I, Lamy F, Dumont JE, Roger PP. Thyrotropin via cyclic AMP induces insulin receptor expression and insulin Co-stimulation of growth and amplifies insulin and insulin-like growth factor signaling pathways in dog thyroid epithelial cells. J Biol Chem. 1996;271(46):29400–6.
Westermark K, Karlsson FA, Westermark B. Thyrotropin modulates EGF receptor function in porcine thyroid follicle cells. Mol Cell Endocrinol. 1985;40(1):17–23.
Boelaert K. The association between serum TSH concentration and thyroid cancer. Endocr Relat Cancer. 2009;16(4):1065–72. https://doi.org/10.1677/ERC-09-0150.
Tam AA, Ozdemir D, Aydin C, Bestepe N, Ulusoy S, Sungu N, et al. Association between preoperative thyrotrophin and clinicopathological and aggressive features of papillary thyroid cancer. Endocrine. 2018;59(3):565–72. https://doi.org/10.1007/s12020-018-1523-6.
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association Guidelines Task Force on thyroid nodules and differentiated thyroid cancer. Thyroid : official journal of the American Thyroid Association. 2016;26(1):1–133. https://doi.org/10.1089/thy.2015.0020.
Shi RL, Liao T, Qu N, Liang F, Chen JY, Ji QH. The usefulness of preoperative thyroid-stimulating hormone for predicting differentiated thyroid microcarcinoma. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2016;154(2):256–62. https://doi.org/10.1177/0194599815618388.
Zheng J, Li C, Lu W, Wang C, Ai Z. Quantitative assessment of preoperative serum thyrotropin level and thyroid cancer. Oncotarget. 2016;7(23):34918–29. https://doi.org/10.18632/oncotarget.9201.
McLeod DS, Watters KF, Carpenter AD, Ladenson PW, Cooper DS, Ding EL. Thyrotropin and thyroid cancer diagnosis: a systematic review and dose-response meta-analysis. J Clin Endocrinol Metab. 2012;97(8):2682–92. https://doi.org/10.1210/jc.2012-1083.
Negro R, Valcavi R, Riganti F, Toulis KA, Colosimo E, Bongiovanni M, et al. Thyrotropin values in patients with micropapillary thyroid cancer versus benign nodular disease. Endocr Pract : official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 2013;19(4):651–5. https://doi.org/10.4158/EP12385.OR.
Shi L, Li Y, Guan H, Li C, Shi L, Shan Z, et al. Usefulness of serum thyrotropin for risk prediction of differentiated thyroid cancers does not apply to microcarcinomas: results of 1,870 Chinese patients with thyroid nodules. Endocr J. 2012;59(11):973–80.
Choi JS, Nam CM, Kim EK, Moon HJ, Han KH, Kwak JY. Evaluation of serum thyroid-stimulating hormone as indicator for fine-needle aspiration in patients with thyroid nodules. Head Neck. 2015;37(4):498–504. https://doi.org/10.1002/hed.23616.
Fiore E, Rago T, Provenzale MA, Scutari M, Ugolini C, Basolo F, et al. Lower levels of TSH are associated with a lower risk of papillary thyroid cancer in patients with thyroid nodular disease: thyroid autonomy may play a protective role. Endocr Relat Cancer. 2009;16(4):1251–60. https://doi.org/10.1677/ERC-09-0036.
Golbert L, de Cristo AP, Faccin CS, Farenzena M, Folgierini H, Graudenz MS, et al. Serum TSH levels as a predictor of malignancy in thyroid nodules: A prospective study. PloS One. 2017;12(11):e0188123. https://doi.org/10.1371/journal.pone.0188123.
Moon SS, Lee YS, Lee IK, Kim JG. Serum thyrotropin as a risk factor for thyroid malignancy in euthyroid subjects with thyroid micronodule. Head Neck. 2012;34(7):949–52. https://doi.org/10.1002/hed.21828.
Arscott PL, Stokes T, Myc A, Giordano TJ, Thompson NW, Baker JR Jr. Fas (CD95) expression is up-regulated on papillary thyroid carcinoma. J Clin Endocrinol Metab. 1999;84(11):4246–52. https://doi.org/10.1210/jcem.84.11.6139.
Kimura H, Yamashita S, Namba H, Tominaga T, Tsuruta M, Yokoyama N, et al. Interleukin-1 inhibits human thyroid carcinoma cell growth. J Clin Endocrinol Metab. 1992;75(2):596–602. https://doi.org/10.1210/jcem.75.2.1322431.
Boi F, Minerba L, Lai ML, Marziani B, Figus B, Spanu F, et al. Both thyroid autoimmunity and increased serum TSH are independent risk factors for malignancy in patients with thyroid nodules. J Endocrinol Investig. 2013;36(5):313–20. https://doi.org/10.3275/8579.
Koch CA. How can environmental factors contribute to the incidence of thyroid cancer? Horm Metab Res = Hormon- und Stoffwechselforschung = Hormones et metabolisme. 2017;49(3):229–31. https://doi.org/10.1055/s-0043-103572.
Koch CA, Diamanti-Kandarakis E. Introduction to endocrine disrupting chemicals--is it time to act? Rev Endocr Metab Disord. 2015;16(4):269–70. https://doi.org/10.1007/s11154-016-9338-3.
Lewis J, Hoover J, MacKenzie D. Mining and environmental health disparities in native american communities. Curr Environ Health Rep. 2017;4(2):130–41. https://doi.org/10.1007/s40572-017-0140-5.
Duntas LH, Stathatos N. Toxic chemicals and thyroid function: hard facts and lateral thinking. Rev Endocr Metab Disord. 2015;16(4):311–8. https://doi.org/10.1007/s11154-016-9331-x.
Franco AT, Malaguarnera R, Refetoff S, Liao XH, Lundsmith E, Kimura S, et al. Thyrotrophin receptor signaling dependence of Braf-induced thyroid tumor initiation in mice. Proc Natl Acad Sci U S A. 2011;108(4):1615–20. https://doi.org/10.1073/pnas.1015557108.
Virk RK, Van Dyke AL, Finkelstein A, Prasad A, Gibson J, Hui P, et al. BRAFV600E mutation in papillary thyroid microcarcinoma: a genotype-phenotype correlation. Mod Pathol : an official journal of the United States and Canadian Academy of Pathology, Inc. 2013;26(1):62–70. https://doi.org/10.1038/modpathol.2012.152.
Sheu SY, Schwertheim S, Worm K, Grabellus F, Schmid KW. Diffuse sclerosing variant of papillary thyroid carcinoma: lack of BRAF mutation but occurrence of RET/PTC rearrangements. Mod Pathol : an official journal of the United States and Canadian Academy of Pathology, Inc. 2007;20(7):779–87. https://doi.org/10.1038/modpathol.3800797.
Lin KL, Wang OC, Zhang XH, Dai XX, Hu XQ, Qu JM. The BRAF mutation is predictive of aggressive clinicopathological characteristics in papillary thyroid microcarcinoma. Ann Surg Oncol. 2010;17(12):3294–300. https://doi.org/10.1245/s10434-010-1129-6.
Jung CK, Little MP, Lubin JH, Brenner AV, Wells SA Jr, Sigurdson AJ, et al. The increase in thyroid cancer incidence during the last four decades is accompanied by a high frequency of BRAF mutations and a sharp increase in RAS mutations. J Clin Endocrinol Metab. 2014;99(2):E276–85. https://doi.org/10.1210/jc.2013-2503.
Shi CL, Guo Y, Lyu YC, Nanding Z, Gao WC, Shi TF, et al. Clinical pathological characteristics of resectable papillary thyroid microcarcinoma. Zhonghua zhong liu za zhi [Chin J Oncol]. 2017;39(5):361–6. https://doi.org/10.3760/cma.j.issn.0253-3766.2017.05.008.
Marotta V, Guerra A, Zatelli MC, Uberti ED, Di Stasi V, Faggiano A, et al. BRAF mutation positive papillary thyroid carcinoma is less advanced when Hashimoto's thyroiditis lymphocytic infiltration is present. Clin Endocrinol. 2013;79(5):733–8. https://doi.org/10.1111/cen.12194.
Ma YJ, Deng XL, Li HQ. BRAF(V(6)(0)(0)E) mutation and its association with clinicopathological features of papillary thyroid microcarcinoma: A meta-analysis. J Huazhong Univ Sci Technolog Med Sci = Hua zhong ke ji da xue xue bao Yi xue Ying De wen ban = Huazhong keji daxue xuebao Yixue Yingdewen ban. 2015;35(4):591–9. https://doi.org/10.1007/s11596-015-1476-4.
Ciampi R, Nikiforov YE. RET/PTC rearrangements and BRAF mutations in thyroid tumorigenesis. Endocrinology. 2007;148(3):936–41. https://doi.org/10.1210/en.2006-0921.
Tallini G, Santoro M, Helie M, Carlomagno F, Salvatore G, Chiappetta G, et al. RET/PTC oncogene activation defines a subset of papillary thyroid carcinomas lacking evidence of progression to poorly differentiated or undifferentiated tumor phenotypes. Clin Cancer Res : an official journal of the American Association for Cancer Research. 1998;4(2):287–94.
Su X, He C, Ma J, Tang T, Zhang X, Ye Z, et al. RET/PTC rearrangements are associated with elevated postoperative TSH levels and multifocal lesions in papillary thyroid cancer without concomitant thyroid benign disease. PloS One. 2016;11(11):e0165596. https://doi.org/10.1371/journal.pone.0165596.
Rodrigues AC, Penna G, Rodrigues E, Castro P, Sobrinho-Simoes M, Soares P. The genetics of papillary microcarcinomas of the thyroid: diagnostic and prognostic implications. Curr Genomics. 2017;18(3):244–54. https://doi.org/10.2174/1389202918666170105094459.
Kuo EJ, Goffredo P, Sosa JA, Roman SA. Aggressive variants of papillary thyroid microcarcinoma are associated with extrathyroidal spread and lymph-node metastases: a population-level analysis. Thyroid : official journal of the American Thyroid Association. 2013;23(10):1305–11. https://doi.org/10.1089/thy.2012.0563.
Benvenga S, Koch CA. Molecular pathways associated with aggressiveness of papillary thyroid cancer. Curr Genomics. 2014;15(3):162–70. https://doi.org/10.2174/1389202915999140404100958.
Kang DY, Kim KH, Kim JM, Kim SH, Kim JY, Baik HW, et al. High prevalence of RET, RAS, and ERK expression in Hashimoto's thyroiditis and in papillary thyroid carcinoma in the Korean population. Thyroid : official journal of the American Thyroid Association. 2007;17(11):1031–8. https://doi.org/10.1089/thy.2007.0035.
Khoo ML, Ezzat S, Freeman JL, Asa SL. Cyclin D1 protein expression predicts metastatic behavior in thyroid papillary microcarcinomas but is not associated with gene amplification. J Clin Endocrinol Metab. 2002;87(4):1810–3. https://doi.org/10.1210/jcem.87.4.8352.
Ma H, Yan J, Zhang C, Qin S, Qin L, Liu L, et al. Expression of papillary thyroid carcinoma-associated molecular markers and their significance in follicular epithelial dysplasia with papillary thyroid carcinoma-like nuclear alterations in Hashimoto's thyroiditis. Int J Clin Exp Pathol. 2014;7(11):7999–8007.
Chui MH, Cassol CA, Asa SL, Mete O. Follicular epithelial dysplasia of the thyroid: morphological and immunohistochemical characterization of a putative preneoplastic lesion to papillary thyroid carcinoma in chronic lymphocytic thyroiditis. Virchows Arch : an international journal of pathology. 2013;462(5):557–63. https://doi.org/10.1007/s00428-013-1397-1.
Singh S, Singh A, Khanna AK. Thyroid incidentaloma. Indian J Surg Oncol. 2012;3(3):173–81. https://doi.org/10.1007/s13193-011-0098-y.
Sakorafas GH, Giotakis J, Stafyla V. Papillary thyroid microcarcinoma: a surgical perspective. Cancer Treat Rev. 2005;31(6):423–38. https://doi.org/10.1016/j.ctrv.2005.04.009.
Sciuto R, Romano L, Rea S, Marandino F, Sperduti I, Maini CL. Natural history and clinical outcome of differentiated thyroid carcinoma: a retrospective analysis of 1503 patients treated at a single institution. Ann Oncol : official journal of the European Society for Medical Oncology. 2009;20(10):1728–35. https://doi.org/10.1093/annonc/mdp050.
Slijepcevic N, Zivaljevic V, Diklic A, Jovanovic M, Oluic B, Paunovic I. Risk factors associated with intrathyroid extension of thyroid microcarcinomas. Langenbeck's Arch Surg. 2018. https://doi.org/10.1007/s00423-018-1680-3.
Kwak JY, Kim EK, Youk JH, Kim MJ, Son EJ, Choi SH, et al. Extrathyroid extension of well-differentiated papillary thyroid microcarcinoma on US. Thyroid : official journal of the American Thyroid Association. 2008;18(6):609–14. https://doi.org/10.1089/thy.2007.0345.
Yu X, Song X, Sun W, Zhao S, Zhao J, Wang YG. Independent risk factors predicting central lymph node metastasis in papillary thyroid microcarcinoma. Horm Metab Res = Hormon- und Stoffwechselforschung = Hormones et metabolisme. 2017;49(3):201–7. https://doi.org/10.1055/s-0043-101917.
Qu H, Sun GR, Liu Y, He QS. Clinical risk factors for central lymph node metastasis in papillary thyroid carcinoma: a systematic review and meta-analysis. Clin Endocrinol. 2015;83(1):124–32. https://doi.org/10.1111/cen.12583.
Liu LS, Liang J, Li JH, Liu X, Jiang L, Long JX, et al. The incidence and risk factors for central lymph node metastasis in cN0 papillary thyroid microcarcinoma: a meta-analysis. Eur Arch Otorhinolaryngol : official journal of the European Federation of Oto-Rhino-Laryngological Societies. 2017;274(3):1327–38. https://doi.org/10.1007/s00405-016-4302-0.
Sun W, Lan X, Zhang H, Dong W, Wang Z, He L, et al. Risk factors for central lymph node metastasis in CN0 papillary thyroid carcinoma: a systematic review and meta-analysis. PloS One. 2015;10(10):e0139021. https://doi.org/10.1371/journal.pone.0139021.
Bradley NL, Wiseman SM. Papillary thyroid microcarcinoma: the significance of high risk features. BMC Cancer. 2017;17(1):142. https://doi.org/10.1186/s12885-017-3120-0.
Pisanu A, Saba A, Podda M, Reccia I, Uccheddu A. Nodal metastasis and recurrence in papillary thyroid microcarcinoma. Endocrine. 2015;48(2):575–81. https://doi.org/10.1007/s12020-014-0350-7.
Benvenga S, Guarneri F. Molecular mimicry and autoimmune thyroid disease. Rev Endocr Metab Disord. 2016;17(4):485–98. https://doi.org/10.1007/s11154-016-9363-2.
Miccoli P, Miccoli M, Antonelli A, Minuto MN. Clinicopathologic and molecular disease prognostication for papillary thyroid cancer. Expert Rev Anticancer Ther. 2009;9(9):1261–75. https://doi.org/10.1586/era.09.92.
Koibuchi H, Omoto K, Fukushima N, Toyotsuji T, Taniguchi N, Kawano M. Coexistence of papillary thyroid cancer and Hashimoto thyroiditis in children: report of 3 cases. J Ultrasound Med : official journal of the American Institute of Ultrasound in Medicine. 2014;33(7):1299–303. https://doi.org/10.7863/ultra.33.7.1299.
Li Y, Wang Y, Wu Q, Hu B. Papillary thyroid microcarcinoma co-exists with Hashimoto's thyroiditis: Is strain elastography still useful? Ultrasonics. 2016;68:127–33. https://doi.org/10.1016/j.ultras.2016.02.013.
Soares P, Celestino R, Gaspar da Rocha A, Sobrinho-Simoes M. Papillary thyroid microcarcinoma: how to diagnose and manage this epidemic? Int J Surg Pathol. 2014;22(2):113–9. https://doi.org/10.1177/1066896913517394.
Choi YJ, Yun JS, Kook SH, Jung EC, Park YL. Clinical and imaging assessment of cervical lymph node metastasis in papillary thyroid carcinomas. World J Surg. 2010;34(7):1494–9. https://doi.org/10.1007/s00268-010-0541-1.
Wu ZG, Yan XQ, Su RS, Ma ZS, Xie BJ, Cao FL. How many contralateral carcinomas in patients with unilateral papillary thyroid microcarcinoma are preoperatively misdiagnosed as benign? World J Surg. 2017;41(1):129–35. https://doi.org/10.1007/s00268-016-3701-0.
Kim D, Park JW. Clinical implications of preoperative thyrotropin serum concentrations in patients who underwent thyroidectomy for nonfunctioning nodule(s). J Korean Surg Soc. 2013;85(1):15–9. https://doi.org/10.4174/jkss.2013.85.1.15.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Vita, R., Ieni, A., Tuccari, G. et al. The increasing prevalence of chronic lymphocytic thyroiditis in papillary microcarcinoma. Rev Endocr Metab Disord 19, 301–309 (2018). https://doi.org/10.1007/s11154-018-9474-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-018-9474-z