Abstract
Purpose
To identify clinical, biological and pathological risk factors for the incidental discovery of papillary thyroid microcarcinomas (PTMCs) in patients undergoing thyroidectomy for presumed benign conditions.
Methods
Cross sectional, single center study, involving all consecutive patients (N = 3015) who were submitted to thyroid surgery between 2001–2019. All medical files were retrospectively reviewed. A total of 1961 patients in the benign group and 145 patients in PTMC group were analyzed.
Results
No significant differences in age, sex, body mass index, smoking status, thyroid volume or weight and preoperative thyroxine treatment between benign and PTMC groups were observed. Circulating anti- thyroid antibodies, histological thyroiditis and serum thyrotropin (TSH) were significantly associated with PTMC in univariable analysis. Independent risk factors for incidental PTMC by multivariable analysis where possible (OR: 1.51, 95% CI: 0.99–2.28) and certain (OR: 1.74, 95% CI: 1.09–2.78) thyroid autoimmunity (p = 0.002) and higher serum TSH (OR: 1.25, 95% CI: 1.08–1.45, p = 0.03), whereas thyroid lobectomy was associated with a lower risk of PTMC (OR: 0.40, 95% CI: 0.24–0.67, p < 0.001). The most frequent genetic alteration was BRAFV600E mutation, found in 56.3% of PTMC submitted to DNA sequencing. No association between clinical, biological or histological characteristics of PTMC and BRAFV600E mutation was observed.
Conclusions
Thyroid autoimmunity and higher preoperative serum TSH level were independent predictors of PTMC incidentally discovered during thyroid surgery. Larger prospective studies are needed to better identify possible risk factors for papillary thyroid carcinoma initiation and progression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Papillary thyroid carcinoma (PTC) is the most frequent (~80%) thyroid malignancy, with an incidence which has increased worldwide over the past decades. This rise has been, at least in part, attributed to recent widespread use of high-resolution ultrasound (US) and fine needle aspiration cytology (FNA) for thyroid nodules, which has led to the diagnosis of otherwise clinically indolent papillary microcarcinomas (PTMC), that is PTC < 1 cm [1,2,3,4].
PTMCs generally have a good prognosis, are often discovered incidentally during thyroidectomy for presumed benign conditions or at autopsy and thus the adoption of more conservative therapeutic strategies for this entity has been endorsed by recent guidelines [5,6,7]. However, some PTMCs may present with lymph node metastasis and a risk of recurrence, in younger patients, in cases of multifocality, non-incidental detection, aggressive histology, extra-thyroidal extension or in the presence of BRAFV600E mutation, the most frequent genetic alteration of PTC [8,9,10,11]. The minority of PTMCs that showed progression during active surveillance studies were among young patients (<40 years old) with a higher serum thyrotropin (TSH) level [12, 13]. TSH has been associated with advanced stage PTC > 1 cm in a large meta-analysis, and animal models have shown that TSH signaling was required in BRAF-induced thyroid tumorigenesis, suggesting a role for tumor initiation [14, 15]. Hashimoto’s thyroiditis has been associated with increased PTMC incidence in retrospective studies, without however clear evidence as to its role in the clinical behavior of PTMC [16, 17]. Hypothesizing that any clinically significant PTC larger than 1 cm in size has evolved from an initial microcarcinoma stage, the study of risk factors for the occurrence of a papillary microcarcinoma could contribute to a better understanding of the early stages of thyroid tumor initiation and progression.
The primary objective of this study was to identify the clinical, biological, and pathological risk factors for the incidental detection of PTMC in patients undergoing thyroidectomy for presumed benign conditions. We also aimed to analyze whether the presence or absence of these risk factors was associated with a distinct PTMC molecular profile.
Materials and methods
This is a cross-sectional, single center study nested in the prospective ongoing database of the Thoracic Surgery Department of H.U.B.- Hôpital Erasme, including all consecutive patients who underwent thyroid surgery between 2001–2019, whose medical files were retrospectively reviewed. The inclusion criterion for the study was total or hemi (lobectomy) thyroidectomy. The principal criterion for the choice of lobectomy was the absence of clinically significant (> 5 mm) thyroid nodules in the contralateral lobe in the preoperative ultrasound and their increased after 2016 following guidelines advocating more conservative surgery for nodular disease. The exclusion criteria were: previous partial thyroidectomy without available histological proof of benignity, Grave’s disease, presence at histology of a PTC > 1 cm and or all other types of thyroid neoplasms including tumors of undetermined malignant potential, presence of tumor predisposing syndromes (multiple endocrine neoplasia syndrome type 1 or 2, acromegaly), absence of preoperative serum TSH and finally preoperative detection of PTMC by FNA (performed in nodules <1 cm). The strategy for patients’ enrollment in the study is shown in Fig. 1. The study protocol was approved by the Ethics Committee of H.U.B.—Hôpital Erasme (P2014/310, A2020/138). Enrolled patients were divided into two groups for comparison: the benign (control) group and the PTMC group (Fig. 1). For all evaluated patients, the following variables were recorded when available: age, sex, current smoking, body mass index (BMI), thyroxin treatment, thyroid gland volume (ml) measured by preoperative ultrasound (US) performed within the 12 months prior to surgery, thyroid gland weight (gr) reported at histological examination, preoperative serum TSH (mU/L) level (the value closest to the surgery date, within 3 months preoperatively, was recorded), presence of circulating anti-thyroperoxidase (anti-TPO) and/or anti-thyroglobulin (anti-Tg) antibodies (Abs) and presence of histological lymphocytic thyroiditis. Patients who had quit smoking for at least 1 year prior to thyroidectomy were considered non-smokers. For patients treated preoperatively by anti-thyroid drugs, the serum TSH level before the treatment initiation (measured within a maximum of 12 months preoperatively) was recorded.
Biochemical assays
Serum TSH, anti-TPO Abs, and anti-Tg Abs were measured by electrochemiluminescence assay throughout the study period, using the module E (Roche) until 2017 (normal essay range for TSH: 0.4–4.0 μUI/ml, negative threshold for anti-TPO Abs < 34 U/ml, and for anti-Tg Abs < 115 U/ml) and then the Cobas e801 (Roche) module from 2017 and onwards (normal assay range for TSH: 0.27–4.20 mU/L, negative threshold for anti-TPO Abs < 34 kUI/L, and for anti-Tg Abs < 115 kUI/L) according to the manufacturer’s instructions (Roche Diagnostics, Manheim, Germany).
Histological examination methodology and DNA sequencing
The histological examination throughout the study period was performed using a standardized methodology including sectioning of each thyroid lobe in 3 mm slices and microscopic examination of all suspicious regions and nodules and was performed under the supervision of a single experienced pathologist (IS, 40 years of experience). If lymphocytic thyroiditis appeared in the final conclusions of the histology report, it was recorded as present. For the PTMC group, the tumor size (largest diameter in mm, largest foci in case of multifocality), multifocality, bilateral localization, lymph node status, and molecular profile if available were recorded. The molecular profile of PTMC surgically resected between 2010 and 2019 was systematically evaluated using a targeted DNA Next Generation sequencing (NGS) panel, as previously published [18]. Until 2018, the DNA panel was the AmpliSeq Cancer hotspot panel version 2; in 2019 a custom DNA panel targeting mutations in 26 genes implicated in thyroid tumors was used. NGS was performed using Ampliseq Technology and Ion Torrent sequencers (ThermoFisher), as previously described. NGS data analysis was carried out using standard procedures already established in routine in the Department of Pathology and is accredited to ISO15189.
Statistical analysis
Statistical analysis was performed with Stata/SE 17.0. The comparison between study groups was performed using Pearson’s Chi-squared test or Fisher’s exact test for categorical variables and with Student’s t-test and Mann-Whitney-Wilcoxon test for normally and non-normally distributed continuous variables respectively. The risk of PTMC was analyzed by logistic regression according to the different variables. Odd ratios (OR) with 95% confidence intervals (CI) and Wald’s test p-value are presented. Multivariable models for PTMC risk were constructed considering variables associated with p < 0.1 and did not include variables with > 10% missing observations. Multicollinearity was assessed using the variance inflation factor (VIF < 2.5) and a backward selection procedure was used in order to keep only variables that remained significantly associated with the outcome (PTMC). The Akaike information criterion (AIC) between possible final models was considered and the goodness-of-fit was verified (Hosmer-Lemeshow test). Statistical significance was set at p < 0.05.
Results
Among the 3015 patients who underwent thyroid surgery at H.U.B.—Hôpital Erasme, between 2001–2019, 2395 patients underwent total thyroidectomy and 620 patients underwent lobectomy. After applying the study exclusion criteria, a total of 1961 patients in the benign group and 145 patients in the PTMC group were analyzed (Fig. 1).
Incidental PTMC risk analysis according to clinical, biological and histological variables
The clinical, biological, histological characteristics and comparison between the PTMC group and the benign group are shown in Table 1. A higher frequency of incidental PTMC was observed in patients undergoing total thyroidectomy (p = 0.001). Female predominance was observed in both groups, the median age, body mass index and smoking status did not differ significantly between groups. Median thyroid volume and median thyroid weight were smaller in the PTMC group (31 ml (IQR: 19.6–50.0) and 38 g (IQR: 25–66), respectively) compared to the benign group (35 ml (IQR: 20.10–60.00) and 45 g (IQR: 25.00–75.00), respectively) without reaching statistical significance (p = 0.054, p = 0.11 respectively). The presence of anti- TPO and/or anti- Tg Abs was significantly more frequent in the PTMC group (24.3%) compared to the benign group (16.1%) (p = 0.01). Histological lymphocytic thyroiditis was also significantly more frequent in the PTMC group (44.8% in PTMCs versus 30.5% in benign group, p < 0.001). Thyroid autoimmunity (TAI) was defined as certain if patients where positive for both antibodies and histological thyroiditis, as possible if patients were positive for either antibodies or histological thyroiditis and as absent if patients were negative for both antibodies and histological thyroiditis. Presence of possible or certain TAI was also significantly associated with PTMC (p = 0.002). The median preoperative serum TSH level was higher in PTMC group (0.99 (IQR: 0.60–1.54) vs 0.80 (IQR: 0.38–1.32) mU/L in benign group, p < 0.001). Approximately one third of patients were treated preoperatively by thyroxine (mostly in the years before 2009), in both PTMC and benign groups (p = 0.64). TSH levels remained significantly higher (p = 0.049) in the PTMC group compared to benign group, even after exclusion of patients treated by thyroxine and/ or positive for thyroid antibodies (data not shown).
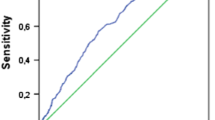
After stratification of patients in four TSH categories, we observed a continuously increasing proportion of patients with PTMC as the serum TSH increased (p = 0.02): 4.4% of patients had a PTMC in the TSH ≤ 0.4 category vs 7.5% of patients in the 0.4 > TSH ≤ 2.5, vs 10.4% in the > 2.5 TSH ≤ 4, vs 13.3% in the TSH > 4 mU/L category (Fig. 2).
Illustration of the proportion (%) of patients with PTMC among different serum TSH categories. A significant (p = 0.02) increase in the % of patients presenting a PTMC was observed in parallel with the increase of TSH among the different categories: 4.4% of patients had a PTMC in the TSH ≤ 0.4 category vs 7.5% in the 0.4 > TSH ≤ 2.5, vs 10.4% in the > 2.5 TSH ≤ 4, vs 13.3% in the TSH > 4 mU/L category
Identification of independent risk factors for incidental PTMC by multivariable analysis
Variables with an association of p < 0.1 with PTMC identified by univariable analysis, except those with > 10% missing observations, were submitted to multivariable analysis (Table 2). Given a strong collinearity relationship between TAI and antibodies and between TAI and histological thyroiditis, we included in the final multivariable model only the TAI variable. In our opinion, TAI was more relevant since it takes into account both the biological and the histological aspect of the condition, making the association when both antibodies and thyroiditis were positive more robust. Presence of possible (OR: 1.51, 95% CI: 0.99–2.28) and certain thyroid autoimmunity (OR: 1.74, 95% CI: 1.09–2.78) (p = 0.002) and higher serum TSH (OR: 1.25, 95% CI: 1.08–1.45, p = 0.03) were significantly associated with the presence of PTMC during surgery. Thyroid lobectomy was associated with a lower risk of PTMC (OR: 0.40, 95% CI: 0.24–0.67, p < 0.001).
Characteristics of papillary thyroid microcarcinomas (PTMC)
We analyzed the histological and molecular characteristics of all PTMC (N = 145) evaluated in this study (Table 3). The median size of the PTMC was 4 mm (IQR: 2–6 mm). 75.9% of patients presented with unifocal PTMC, 24.1% with multifocal, and 11,7% with bilateral microcarcinoma. The most frequent PTMC histological variant was classic variant (48.9%) followed by mixed classic and follicular variant (34.5%). For 76.6% of the patients, as reasonably expected, regional lymph nodes were not available (Nx) for histological analysis. In the remaining patients, lymph node resection was performed at the surgeon’s discretion during surgery: 21.8% of patients did not have histologic evidence of lymph node invasion (N0) and 3.2% of patients had regional lymph node invasion (N1).
All PTMC surgically resected between 2010–2019 (n = 74), underwent DNA sequencing analysis. Among them, n = 10 samples did not have enough material for DNA extraction and sequencing, so final molecular profile analysis was possible for 64 samples (44.1% of the total studied cohort of PTMC), (Table 3). For n = 3 (4.7%) samples the NGS analysis was not contributive for technical reasons (suboptimal sequencing quality). While n = 21 (32.8%) of PTMC carried no mutations, in n = 36 (56.3%) of PTMC a BRAFV600E mutation was detected. Among the latter, one PTMC carried a double BRAFV600E and TERT promoter mutation (Table 3). In n = 4 (6.3%) of PTMC other gene mutations (NRAS, HRAS, CHEK2) were detected.
The tumor size and histological variant did not significantly differ between negative for mutations PTMC and BRAFV600E positive PTMC samples (data not shown). The clinical, biological, and histological variables included in the PTMC risk analysis were analyzed by logistic regression between negative for mutations PTMC and BRAFV600E positive PTMC samples, and no statistically significant differences were found (data not shown).
Discussion
In the present study, we observed that thyroid autoimmunity and serum TSH were independent risk factors for the incidental discovery of PTMC in patients undergoing thyroid surgery for presumed benign conditions. Investigation of very early stages of papillary thyroid cancer could help to better understand tumor initiation and to identify clinically relevant predictors of malignancy. The probability to find an incidental PTMC at surgery was higher when the patients underwent total thyroidectomy versus lobectomy in the present study. The most likely explanation for this finding is that the random probability of finding a microcarcinoma during routine histological examination of one thyroid lobe instead of two diminishes.
The pathogenesis of sporadic, non-radiation-induced, papillary thyroid cancer is still not fully understood. Several risk factors for PTC, such as environmental pollutants, diet, increased BMI, insulin resistance, and a possible protective role of smoking have emerged from epidemiological studies but their underlying pathophysiological role in thyroid carcinogenesis remains undetermined [19,20,21]. Male sex, single or fewer nodules and younger age have also been reported as predictors for malignancy in patients with thyroid nodular disease [22, 23]. We did not observe any association between age, sex, BMI, or smoking status and the risk of incidental PTMC in our study.
Elevated serum TSH has been reported as a risk factor for PTC > 1 cm and was associated with advanced diseases states [14]. Regarding micro PTC, the evidence on TSH as a risk factor, remains inconclusive, with conflicting data in the literature, with some studies showing a significant association and others not [24,25,26,27,28,29]. However, during active surveillance studies for papillary microcarcinomas, serum TSH was significantly associated with disease progression [12]. However, TSH has not yet been incorporated into algorithms for management of thyroid nodular disease. In our study, serum TSH was found to be an independent predictor of malignancy (OR: 1.25, 95% CI: 1.08–1.45).
The exact role of TSH, a well-known growth and proliferation factor for thyrocytes, and TSH signaling in thyroid tumorigenesis, as to whether they are involved in tumor initiation or tumor progression is not established. In in vivo transgenic mice models, TSH signaling was required for BRAFV600E-induced thyroid tumorigenesis but also conferred more aggressive features in BRAFV600E-induced thyroid tumors [15, 30]. In vitro, it was shown that TSH induced DNA damage in human thyrocytes, probably by increasing intracellular levels of reactive oxygen species (ROS) [31].
The concomitant presence of Hashimoto thyroiditis and PTMC has long been described in the literature with a prevalence varying from 8–34%, but whether thyroiditis is a cause or a consequence of microcarcinoma and whether it modifies or not its clinical behavior is still debated [17, 32]. One of the possible underlying mechanisms could be the increase in oxidative stress as a result of chronic immune cell infiltrates in the thyroid, which may cause DNA damage, genomic instability and may interfere with DNA repair mechanisms [33, 34]. Slijepcevic et al., reported that Hashimoto thyroiditis was an independent predictor (OR:1.54, 95% CI: 1.15–2.05) for PTMC [16]. Similarly, in this study, histological thyroiditis was strongly associated (p < 0.001) with the incidental discovery of PTMC during thyroidectomy. The presence of possible and certain thyroid autoimmunity, as defined above, were independent risk factors for PTMC (OR: 1.51, 95% CI: 0.99–2.28 for possible TAI and OR: 1.74, 95% CI: 1.09–2.78 for certain TAI). Carlos et al. observed no association in multivariable analysis between Hashimoto, or Grave’s disease with incidental PTMC, but not specific diagnostic (biological, antibody titers, histology, iconography) criteria for these conditions were applied by the authors, so conclusions should be interpreted with caution [35]. We hereby did not include Grave’s disease due to the difficulty in correctly interpreting serum TSH as a risk factor for cancer in these patients having TSH receptor antibodies that stimulate thyrocytes and increase intracellular cAMP signaling. However, Grave’s disease could be a model per se to study carcinogenesis in relation to inflammatory cytokines specifically associated with this condition.
In this study, detection rate of BRAFV660E mutation among the analyzed PTMC (n = 64) was 56.3%, a rate similar to that of larger (>1 cm) size PTC reported in the TCGA (Thyroid Cancer Genome Atlas) study [36]. Other groups have reported a prevalence of BRAFV660E mutation in small series (number of patients varying from 55 to 195) of incidental PTMC ranging from 17.6–46% in association with multifocality, tumor size, and unfavorable histology; however, BRAFV660E association with tumor aggressive features or recurrence for incidental PTMC has not always been consistent [37,38,39,40]. We did not find any association between the different risk factors for PTMC assessed in this study and the presence of BRAFV600E mutation, an analysis probably hampered by the small number of patients with molecular profile available. Above data, in accordance with the literature, suggest that BRAFV660E is a frequent and early molecular event in thyroid carcinogenesis but factors other than mutational status, such as microenvironment/epigenetic factors, might contribute to the progression of papillary microcarcinoma to larger, clinically significant tumors.
The limitations of the study rely on its cross sectional single-center nature, the relatively small number of PTMC patients, and the lack of molecular characterization of the totality of microcarcinomas.
In conclusion, we identified thyroid autoimmunity and higher preoperative TSH level as independent predictors of PTMC incidentally discovered during thyroid surgery. Lobectomy reduced the probability of finding a PTMC in this study. Prospective studies are essential to confirm these results and to identify other risk factors that contributing to PTMC initiation. Comparison of the clinical characteristics and of the molecular profiles between PTMCs and larger size PTCs could be relevant to assess which factors and which gene alterations may promote progression from micro cancer to a more aggressive clinically significant tumor stage.
References
H. Lim, S.S. Devesa, J.A. Sosa, D. Check, C.M. Kitahara, Trends in thyroid cancer incidence and mortality in the United States, 1974–2013 thyroid cancer incidence and mortality trends thyroid cancer incidence and mortality trends. JAMA 317, 1338–1348 (2017). https://doi.org/10.1001/jama.2017.2719
R. Reinke, J.S. Mathiesen, S.R. Larsen, C.H. Hahn, H.B. Pedersen, J. Bentzen, S. Schytte, C. Godballe, S.C. Londero, Incidental and non-incidental papillary thyroid microcarcinoma in Denmark 1996–2015: A national study on incidence, outcome and thoughts on active surveillance. Cancer Epidemiol. 60, 46–50 (2019). https://doi.org/10.1016/j.canep.2019.03.011
H.S. Ahn, H.J. Kim, H.G. Welch, Korea’s thyroid-cancer “epidemic”—screening and overdiagnosis. N. Engl. J. Med. 371, 1765–1767 (2014). https://doi.org/10.1056/NEJMp1409841
C. La Vecchia, M. Malvezzi, C. Bosetti, W. Garavello, P. Bertuccio, F. Levi, E. Negri, Thyroid cancer mortality and incidence: a global overview. Int. J. Cancer. 136, 2187–2195 (2015). https://doi.org/10.1002/ijc.29251
B.R. Haugen, E.K. Alexander, K.C. Bible, G.M. Doherty, S.J. Mandel, Y.E. Nikiforov, F. Pacini, G.W. Randolph, A.M. Sawka, M. Schlumberger, K.G. Schuff, S.I. Sherman, J.A. Sosa, D.L. Steward, R.M. Tuttle, L. Wartofsky, 2015 American Thyroid Association Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association Guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26, 1–133 (2016). https://doi.org/10.1089/thy.2015.0020
I. Sugitani, Y. Ito, D. Takeuchi, H. Nakayama, C. Masaki, H. Shindo, M. Teshima, K. Horiguchi, Y. Yoshida, T. Kanai, M. Hirokawa, K.Y. Hames, I. Tabei, A. Miyauchi, Indications and strategy for active surveillance of adult low-risk papillary thyroid microcarcinoma: Consensus statements from the Japan association of endocrine surgery task force on management for papillary thyroid microcarcinoma. Thyroid 31, 183–192 (2021). https://doi.org/10.1089/thy.2020.0330
G. Mauri, L. Hegedüs, S. Bandula, R.L. Cazzato, A. Czarniecka, O. Dudeck, L. Fugazzola, R. Netea-Maier, G. Russ, G. Wallin, E. Papini, European thyroid association and cardiovascular and interventional radiological society of Europe 2021 clinical practice guideline for the use of minimally invasive treatments in malignant thyroid lesions. Eur. Thyroid J. 10, 185–197 (2021). https://doi.org/10.1159/000516469
F. Li, G. Chen, C. Sheng, A.M. Gusdon, Y. Huang, Z. Lv, H. Xu, M. Xing, S. Qu, BRAFV600E mutation in papillary thyroid microcarcinoma: a meta-analysis. Endocr. Relat. Cancer. 22, 159–168 (2015). https://doi.org/10.1530/ERC-14-0531
Y. Chen, P.M. Sadow, H. Suh, K.E. Lee, J.Y. Choi, Y.J. Suh, T.S. Wang, C.C. Lubitz, BRAF(V600E) is correlated with recurrence of papillary thyroid microcarcinoma: A systematic review, multi-institutional primary data analysis, and meta-analysis. Thyroid Off. J. Am. Thyroid Assoc. 26, 248–255 (2016). https://doi.org/10.1089/thy.2015.0391
G. Tallini, D. de Biase, C. Durante, G. Acquaviva, M. Bisceglia, R. Bruno, M.L. Bacchi Reggiani, G.P. Casadei, G. Costante, N. Cremonini, L. Lamartina, D. Meringolo, F. Nardi, A. Pession, K.J. Rhoden, G. Ronga, M. Torlontano, A. Verrienti, M. Visani, S. Filetti, BRAF V600E and risk stratification of thyroid microcarcinoma: a multicenter pathological and clinical study. Mod. Pathol. 28, 1343–1359 (2015). https://doi.org/10.1038/modpathol.2015.92
H. Mehanna, T. Al-maqbili, B. Carter, E. Martin, N. Campain, J. Watkinson, C. McCabe, K. Boelaert, J.A. Franklyn, Differences in the recurrence and mortality outcomes rates of incidental and nonincidental papillary thyroid microcarcinoma: A systematic review and meta-analysis of 21 329 person-years of follow-up. J. Clin. Endocrinol. Metab. 99, 2834–2843 (2014). https://doi.org/10.1210/jc.2013-2118
H.I. Kim, H.W. Jang, H.S. Ahn, S. Ahn, S.Y. Park, Y.L. Oh, S.Y. Hahn, J.H. Shin, J.-H. Kim, J.S. Kim, J.H. Chung, T.H. Kim, S.W. Kim, high serum TSH level is associated with progression of papillary thyroid microcarcinoma during active surveillance. J. Clin. Endocrinol. Metab. 103, 446–451 (2018)
Y. Ito, A. Miyauchi, M. Kihara, T. Higashiyama, K. Kobayashi, A. Miya, Patient age is significantly related to the progression of papillary microcarcinoma of the thyroid under observation. Thyroid 24, 27–34 (2014). https://doi.org/10.1089/thy.2013.0367
D.S.A. McLeod, K.F. Watters, A.D. Carpenter, P.W. Ladenson, D.S. Cooper, E.L. Ding, Thyrotropin and thyroid cancer diagnosis: A systematic review and dose-response meta-analysis. J. Clin. Endocrinol. Metab. 97, 2682–2692 (2012)
A.T. Franco, R. Malaguarnera, S. Refetoff, X.-H. Liao, E. Lundsmith, S. Kimura, C. Pritchard, R. Marais, T.F. Davies, L.S. Weinstein, M. Chen, N. Rosen, R. Ghossein, J.A. Knauf, J.A. Fagin, Thyrotrophin receptor signaling dependence of Braf-induced thyroid tumor initiation in mice. Proc. Natl Acad. Sci. USA 108, 1615–1620 (2011). https://doi.org/10.1073/pnas.1015557108
N. Slijepcevic, V. Zivaljevic, J. Marinkovic, S. Sipetic, A. Diklic, I. Paunovic, Retrospective evaluation of the incidental finding of 403 papillary thyroid microcarcinomas in 2466 patients undergoing thyroid surgery for presumed benign thyroid disease. BMC Cancer 15, 330 (2015). https://doi.org/10.1186/s12885-015-1352-4
R. Vita, A. Ieni, G. Tuccari, S. Benvenga, The increasing prevalence of chronic lymphocytic thyroiditis in papillary microcarcinoma. Rev. Endocr. Metab. Disord. 19, 301–309 (2018). https://doi.org/10.1007/s11154-018-9474-z
M. Le Mercier, N. D’Haene, N. De Nève, O. Blanchard, C. Degand, S. Rorive, I. Salmon, Next-generation sequencing improves the diagnosis of thyroid FNA specimens with indeterminate cytology. Histopathology 66, 215–224 (2015). https://doi.org/10.1111/his.12461
C.M. Kitahara, E.A. Platz, L.E. Beane Freeman, A.W. Hsing, M.S. Linet, Y. Park, C. Schairer, A. Schatzkin, J.M. Shikany, A.B. De González, Obesity and thyroid cancer risk among U.S. men and women: A pooled analysis of five prospective studies. Cancer Epidemiol. Biomarker. Prev. 20, 464–472 (2011). https://doi.org/10.1158/1055-9965.EPI-10-1220
C.M. Kitahara, M.S. Linet, L.E. Beane Freeman, D.P. Check, T.R. Church, Y. Park, M.P. Purdue, C. Schairer, A. Berrington de González, Cigarette smoking, alcohol intake, and thyroid cancer risk: a pooled analysis of five prospective studies in the United States. Cancer Causes Control CCC 23, 1615–1624 (2012). https://doi.org/10.1007/s10552-012-0039-2
G. Pellegriti, F. Frasca, C. Regalbuto, S. Squatrito, R. Vigneri, Worldwide increasing incidence of thyroid cancer: Update on epidemiology and risk factors, J. Cancer Epidemiol. 2013 (2013). https://doi.org/10.1155/2013/965212.
T. Rago, E. Fiore, M. Scutari, F. Santini, G. Di Coscio, R. Romani, P. Piaggi, C. Ugolini, F. Basolo, P. Miccoli, A. Pinchera, P. Vitti, Male sex, single nodularity, and young age are associated with the risk of finding a papillary thyroid cancer on fine-needle aspiration cytology in a large series of patients with nodular thyroid disease. Eur. J. Endocrinol. 162, 763–770 (2010). https://doi.org/10.1530/EJE-09-0895
J. Luo, C. McManus, H. Chen, R.S. Sippel, Are there predictors of malignancy in patients with multinodular goiter? J. Surg. Res. 174, 207–210 (2012). https://doi.org/10.1016/j.jss.2011.11.1035
R. Negro, R. Valcavi, F. Riganti, K. a Toulis, E. Colosimo, M. Bongiovanni, P. Grassi, L. Giovanella, G. Gardini, S. Piana, Thyrotropin values in patients with micropapillary thyroid cancer versus benign nodular disease. Endocr. Pract. 19, 651–655 (2013). https://doi.org/10.4158/EP12385.OR
A. Mao, N. An, J. Wang, Y. Wu, T. Wang, Z. Wang, H. Guan, J. Wang, Association between preoperative serum TSH and tumor status in patients with papillary thyroid microcarcinoma. Endocrine 73, 617–624 (2021). https://doi.org/10.1007/s12020-021-02690-5
C. Zafon, G. Obiols, J.A. Baena, J. Castellví, B. Dalama, J. Mesa, Preoperative thyrotropin serum concentrations gradually increase from benign thyroid nodules to papillary thyroid microcarcinomas then to papillary thyroid cancers of larger size. J. Thyroid Res. 2012, e530721 (2011). https://doi.org/10.1155/2012/530721
L. Shi, Y. Li, H. Guan, C. Li, L. Shi, Z. Shan, W. Teng, Usefulness of serum thyrotropin for risk prediction of differentiated thyroid cancers does not apply to microcarcinomas: results of 1,870 Chinese patients with thyroid nodules. Endocr. J. 59, 973–980 (2012). https://doi.org/10.1507/endocrj.EJ12-0154
M. Gerschpacher, C. Göbl, C. Anderwald, A. Gessl, M. Krebs, Thyrotropin serum concentrations in patients with papillary thyroid microcancers. Thyroid 20, 389–392 (2010). https://doi.org/10.1089/thy.2009.0139
A.A. Tam, D. Ozdemir, C. Aydın, N. Bestepe, S. Ulusoy, N. Sungu, R. Ersoy, B. Cakir, Association between preoperative thyrotrophin and clinicopathological and aggressive features of papillary thyroid cancer. Endocrine 59, 565–572 (2018). https://doi.org/10.1007/s12020-018-1523-6
F. Orim, A. Bychkov, M. Shimamura, M. Nakashima, M. Ito, M. Matsuse, T. Kurashige, K. Suzuki, V. Saenko, Y. Nagayama, S. Yamashita, N. Mitsutake, Thyrotropin signaling confers more aggressive features with higher genomic instability on BRAF(V600E)-induced thyroid tumors in a mouse model. Thyroid Off. J. Am. Thyroid Assoc. 24, 502–510 (2014). https://doi.org/10.1089/thy.2013.0038
A. Kyrilli, D. Gacquer, V. Detours, A. Lefort, F. Libert, L. Twyffels, L. Van Den Eeckhaute, A. Strickaert, C. Maenhaut, X. De Deken, J.E. Dumont, F. Miot, B. Corvilain, Dissecting the role of thyrotropin in the DNA damage response in human thyrocytes after 131I, γ radiation and H2O2. J. Clin. Endocrinol. Metab. 105 (2020). https://doi.org/10.1210/clinem/dgz185.
U. Feldt-Rasmussen, Hashimoto’s thyroiditis as a risk factor for thyroid cancer. Curr. Opin. Endocrinol. Diabetes Obes. 27, 364 (2020). https://doi.org/10.1097/MED.0000000000000570
R. Ameziane-El-Hassani, M. Schlumberger, C. Dupuy, NADPH oxidases: New actors in thyroid cancer? Nat. Rev. Endocrinol. 12, 485–494 (2016). https://doi.org/10.1038/nrendo.2016.64
N.G. Nicolson, T.C. Brown, R. Korah, T. Carling, Immune cell infiltrate-associated dysregulation of DNA repair machinery may predispose to papillary thyroid carcinogenesis. Surgery 167, 66–72 (2020). https://doi.org/10.1016/j.surg.2019.02.024
J. de Carlos, A. Ernaga, A. Irigaray, J.J. Pineda, A. Echegoyen, P. Salvador, E. Anda, Incidentally discovered papillary thyroid microcarcinoma in patients undergoing thyroid surgery for benign disease. Endocrine 77, 325–332 (2022). https://doi.org/10.1007/s12020-022-03089-6
N. Agrawal, R. Akbani, B.A. Aksoy, A. Ally, H. Arachchi, S.L. Asa, J.T. Auman, M. Balasundaram, S. Balu, S.B. Baylin, M. Behera, B. Bernard, R. Beroukhim, J.A. Bishop, A.D. Black, T. Bodenheimer, L. Boice, M.S. Bootwalla, J. Bowen, R. Bowlby, C.A. Bristow, R. Brookens, D. Brooks, R. Bryant, E. Buda, Y.S.N. Butterfield, T. Carling, R. Carlsen, S.L. Carter, S.E. Carty, T.A. Chan, A.Y. Chen, A.D. Cherniack, D. Cheung, L. Chin, J. Cho, A. Chu, E. Chuah, K. Cibulskis, G. Ciriello, A. Clarke, G.L. Clayman, L. Cope, J.A. Copland, K. Covington, L. Danilova, T. Davidsen, J.A. Demchok, D. DiCara, N. Dhalla, R. Dhir, S.S. Dookran, G. Dresdner, J. Eldridge, G. Eley, A.K. El-Naggar, S. Eng, J.A. Fagin, T. Fennell, R.L. Ferris, S. Fisher, S. Frazer, J. Frick, S.B. Gabriel, I. Ganly, J. Gao, L.A. Garraway, J.M. Gastier-Foster, G. Getz, N. Gehlenborg, R. Ghossein, R.A. Gibbs, T.J. Giordano, K. Gomez-Hernandez, J. Grimsby, B. Gross, R. Guin, A. Hadjipanayis, H.A. Harper, D.N. Hayes, D.I. Heiman, J.G. Herman, K.A. Hoadley, M. Hofree, R.A. Holt, A.P. Hoyle, F.W. Huang, M. Huang, C.M. Hutter, T. Ideker, L. Iype, A. Jacobsen, S.R. Jefferys, C.D. Jones, S.J.M. Jones, K. Kasaian, E. Kebebew, F.R. Khuri, J. Kim, R. Kramer, R. Kreisberg, R. Kucherlapati, D.J. Kwiatkowski, M. Ladanyi, P.H. Lai, P.W. Laird, E. Lander, M.S. Lawrence, D. Lee, E. Lee, S. Lee, W. Lee, K.M. Leraas, T.M. Lichtenberg, L. Lichtenstein, P. Lin, S. Ling, J. Liu, W. Liu, Y. Liu, V.A. LiVolsi, Y. Lu, Y. Ma, H.S. Mahadeshwar, M.A. Marra, M. Mayo, D.G. McFadden, S. Meng, M. Meyerson, P.A. Mieczkowski, M. Miller, G. Mills, R.A. Moore, L.E. Mose, A.J. Mungall, B.A. Murray, Y.E. Nikiforov, M.S. Noble, A.I. Ojesina, T.K. Owonikoko, B.A. Ozenberger, A. Pantazi, M. Parfenov, P.J. Park, J.S. Parker, E.O. Paull, C.S. Pedamallu, C.M. Perou, J.F. Prins, A. Protopopov, S.S. Ramalingam, N.C. Ramirez, R. Ramirez, B.J. Raphael, W.K. Rathmell, X. Ren, S.M. Reynolds, E. Rheinbay, M.D. Ringel, M. Rivera, J. Roach, A.G. Robertson, M.W. Rosenberg, M. Rosenthal, S. Sadeghi, G. Saksena, C. Sander, N. Santoso, J.E. Schein, N. Schultz, S.E. Schumacher, R.R. Seethala, J. Seidman, Y. Senbabaoglu, S. Seth, S. Sharpe, K.R.M. Shaw, J.P. Shen, R. Shen, S. Sherman, M. Sheth, Y. Shi, I. Shmulevich, G.L. Sica, J.V. Simons, R. Sinha, P. Sipahimalani, R.C. Smallridge, H.J. Sofia, M.G. Soloway, X. Song, C. Sougnez, C. Stewart, P. Stojanov, J.M. Stuart, S.O. Sumer, Y. Sun, B. Tabak, A. Tam, D. Tan, J. Tang, R. Tarnuzzer, B.S. Taylor, N. Thiessen, L. Thorne, V. Thorsson, R.M. Tuttle, C.B. Umbricht, D.J. Van Den Berg, F. Vandin, U. Veluvolu, R.G.W. Verhaak, M. Vinco, D. Voet, V. Walter, Z. Wang, S. Waring, P.M. Weinberger, N. Weinhold, J.N. Weinstein, D.J. Weisenberger, D. Wheeler, M.D. Wilkerson, J. Wilson, M. Williams, D.A. Winer, L. Wise, J. Wu, L. Xi, A.W. Xu, L. Yang, L. Yang, T.I. Zack, M.A. Zeiger, D. Zeng, J.C. Zenklusen, N. Zhao, H. Zhang, J. Zhang, J. Zhang, W. Zhang, E. Zmuda, L. Zou, Integrated genomic characterization of papillary thyroid carcinoma. Cell 159, 676–690 (2014). https://doi.org/10.1016/j.cell.2014.09.050
C. Ugolini, R. Giannini, C. Lupi, G. Salvatore, P. Miccoli, A. Proietti, R. Elisei, M. Santoro, F. Basolo, Presence of BRAF V600E in very early stages of papillary thyroid carcinoma. Thyroid 17, 381–388 (2007). https://doi.org/10.1089/thy.2006.0305
G. Tallini, D. de Biase, C. Durante, G. Acquaviva, M. Bisceglia, R. Bruno, M.L. Bacchi Reggiani, G.P. Casadei, G. Costante, N. Cremonini, L. Lamartina, D. Meringolo, F. Nardi, A. Pession, K.J. Rhoden, G. Ronga, M. Torlontano, A. Verrienti, M. Visani, S. Filetti, BRAF V600E and risk stratification of thyroid microcarcinoma: a multicenter pathological and clinical study. Mod Pathol 28, 1343–1359 (2015). https://doi.org/10.1038/modpathol.2015.92
M.T. Samà, E. Grosso, C. Mele et al. Molecular characterisation and clinical correlation of papillary thyroid microcarcinoma. Endocrine 71, 149–157 (2021). https://doi.org/10.1007/s12020-020-02380-8
E. Aliyev, M.J. Ladra-González, M. Sánchez-Ares, I. Abdulkader-Nallib, M. Piso-Neira, G. Rodríguez-Carnero, P. Vieiro-Balo, R. Pérez-Becerra, F. Gude-Sampedro, F. Barreiro-Morandeira, C.V. Alvarez, J.M. Cameselle-Teijeiro, Thyroid papillary microtumor: Validation of the (updated) Porto proposal assessing sex hormone receptor expression and mutational BRAF gene status. Am. J. Surg. Pathol. 44, 1161–1172 (2020). https://doi.org/10.1097/PAS.0000000000001522
Acknowledgements
We thank all of our patients for participating in this study, Prof Matteo Cappello for their long-standing help and devotion to the management of thyroid cancer patients. A.K. and B.C. are members of European Reference Centers for Rare Endocrine Diseases (ENDO-ERN).
Author information
Authors and Affiliations
Contributions
The study conception and design were performed by A.K. and B.C. Data collection and analysis were performed by A.K., R.S., V.C., N.B., M.R., histological examination and molecular profile analysis was conducted by Nicky D’Haene, Isabelle Salmon, final statistical analysis was conducted by J.B. The manuscript including text, tables, and figure, was written by A.K. All authors commented on previous versions of the text and read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
This retrospective study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Ethics Committee of the Université Libre de Bruxelles, H.U.B.—Hôpital Erasme (P2014/310, A2020/138) approved this study (P2014/310, A2020/138).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kyrilli, A., Schoinochoriti, R., Chatzopoulos, V. et al. Thyrotropin (TSH) and thyroid autoimmunity are predictive factors for the incidental discovery of papillary thyroid microcarcinoma during thyroidectomy. Endocrine (2024). https://doi.org/10.1007/s12020-024-03907-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12020-024-03907-z