Abstract
Diffuse intrinsic pontine glioma is a pediatric oncologic disease with dismal prognosis and no effective treatment. Since 2007, our patients have been using valproic acid as prophylactic anticonvulsant. We have undertaken a retrospective study in order to evaluate the influence of valproate in the outcomes of children with this disease in our center. Patients were treated with weekly carboplatin and vincristine and received conformal radiotherapy, either concurrent or sequential. Event-free survival and overall survival of patients not treated with valproic acid were 6.5 and 7.8 months. Accelerated failure time model (a parametric multivariate regression test for time-to-failure data) showed a statistically significant superiority of the median event-free survival of treated patients (6.5 vs. 9.5 months in treated patients; HR 0.54–95 % CI 0.33–0.87; p < 0.05) and also of overall survival (7.8 vs. 13.4 months in treated patients; HR 0.60–95 % CI 0.37–0.98; p = 0.05).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Management of pediatric patients with diffuse intrinsic pontine gliomas (DIPG) remains unsatisfactory. Although considerable effort has been made to improve their outcome, prolonged survival for these patients is still unattainable [1]. Usually less than 10 % of patients with this disease survive 2 years after diagnosis, and there are virtually no patients with prolonged survival. Many novel treatments have been tested, all with similarly disappointing clinical results in phase II trials [2].
Valproic acid (valproate sodium) is an anti-epileptic drug (AED) widely used for treating seizures in children. It has also been used for seizures associated with brain tumors [3]. It does not modify hepatic metabolism of drugs, unlike hepatic enzyme inducing anti-epileptic drugs as phenobarbital or phenytoin. Seizure prophylaxis is controversial in adult and pediatric brain tumor patients [3]. However, a recent metanalysis was not conclusive due to the lack of appropriate clinical data. The decision to start an antiepileptic drug for seizure prophylaxis in children with brain tumors must be guided by assessment of individual risk factors [4]. Seizures are more frequent in pediatric patients with a supratentorial tumor but can nonetheless infrequently occur in posterior fossa tumor patients [3], and their determinants have remained obscure [5]. In our center, we deal with patients that have inadequate access to medical services, including emergency and pre-hospital care, and there have been occasional episodes of deaths supposedly caused by seizures in children with brain tumor under our care. In one of the few reports about this in our country, Kawasaki et al. [6] have described a series of 50 patients with brain tumors and seizures, including two with posterior fossa lesions (one brain stem tumor). We have observed at least four cases of seizures in patients with DIPG in the last 10 years in our center, and their exact cause has been elusive, since they seemed not to be related to predictable factors. Based on these local differences, we considered using prophylactic AED administration to all pediatric patients with brain tumors, including children with posterior fossa tumors.
Since January 2007, valproate sodium at doses 10–15 mg/kg/day every 8–12 h was routinely prescribed for all pediatric brain tumor patients as prophylactic anticonvulsant [7, 8]. After the beginning of prophylactic administration we observed a trend towards longer survival in a subset of our patients. In order to study the possible influence of valproate in the survival of pediatric patients with brain tumors we have undertaken a retrospective cohort study [8]. We also compared this cohort with a historical control from our institution. In this brief report, we focus on the outcomes of children with DIPG. Due to modifications in referral policies in our state, the admission rate of new patients in our center more than doubled from before 2007 to nowadays.
Materials and methods
The institutional review board of our center approved this retrospective study. We reviewed the charts of patients referred to our institution and diagnosed between January 2000 and December 2010 with DIPG (tumor centered in the pons, tumor extension over >50 % of the pontine cross-sectional area, and with or without contrast enhancement), aged 0–17 years. Our institution does not admit patients over 17 years, as a result of Brazilian ministry of health rules. All patients received conventionally fractionated 3-dimensional conformal radiotherapy. Additionally, all patients (except for one in the historical control group) were treated with chemotherapy (after, before or concurrent to radiotherapy) comprised of weekly carboplatin 175 mg/m2 and vincristine 1.5 mg/m2 (as reported elsewhere) [9].
A member of our team reviewed magnetic resonance images (MRI) for tumor site and characteristics. Some of the images from patients diagnosed before 2006 were not available for review, so we used the description of the radiological report to classify the tumors. Usual image parameters (MacDonald’s criteria) were used to analyze MRI and judge disease progression [10]. Since this was a retrospective study, imaging frequency was not standardized and varied among patients. The general protocol was imaging every 3 months, but this was not strictly followed. The primary study endpoint for treatment efficacy was time to treatment failure, measured from the diagnosis, from which event-free survival percentage was computed. Failure events included tumor progression (defined by clinical or radiologic deterioration; when radiological progression was detected, the event was assigned to the patient only if it was accompanied with clinical worsening, to avoid pseudo progression [11]), or death due to any cause. The secondary efficacy endpoint was time to death due to any cause, from which overall survival (OS) was computed. The primary objective of the statistical analysis was to determine whether the valproate treatment produced a difference in the median event-free survival. Based on the hazard function (Figs. S1a, d), the data was assumed to have exponential distribution. As a result, the more appropriate accelerated failure assumption was used to model the data. Model diagnostics showed the Weibull survival distribution with a fixed shape parameter of 2 was the better choice. Asymptotic log-rank test was performed as comparison. Data descriptive statistics and statistical calculations were performed on R 2.12 for Mac OSX (R Foundation for Statistical Computing, 2010). Accelerating factor (γ), and hazard ratio (HR) with 95 % confidence interval (95 % CI) were calculated.
Results
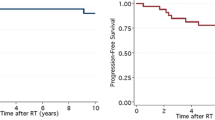
Between 2000 and 2010, 30 patients were diagnosed with DIPG, 12 between 2000–2006 and 18 in 2007–2010. Ten patients were excluded because they did not receive radiotherapy, five from the 2000–2006 group and five from the 2007–2010 group. One patient was excluded because he was treated with a subtherapeutically small dose of radiotherapy (18 Gy). Nineteen patients were included. Median age was 7.7 years, ranging from 6.4 to 10.5 years. There were 8 males and 11 females. Thirteen patients received valproate, only one of these from the 2000–2006 period. The non-treated group included six patients. There were no differences between the two groups regarding demographical data. There were no episodes of pseudo progression. Median event-free survival of patients was 6.5 months in the non-treated group, and 9.5 months in the valproate-treated group (Fig. 1b). Median survival of patients in the non-treated group was 7.8 months, whereas in the valproate-treated group it was 13.4 months (Fig. 1a). Accelerated failure time model showed a statistically significant better median event-free survival in treated group (γ = 1.87 95 % CI 1.14–3.1; HR 0.54–95 % CI 0.33–0.87; p = 0.021). Overall survival was barely statistically different between groups (γ = 1.67 95 % CI 1.02–2.7; HR 0.60–95 % CI 0.37–0.98; p = 0.05). Asymptotic log-rank test did not show a significant difference between groups regarding any of the outcomes (p = 0.13 and 0.19) (Fig. 2).
a–c MRI images of representative cases of diffuse intrinsic pontine glioma. Upper images are T1-weighted, gadolinium-enhanced, and bottom images are FLAIR. a depicts case 14 (Table 1), b case 11, and c case 13
Discussion
The event-free and overall survival of the patients treated with valproic acid was unexpectedly better than our historical control and what is currently achieved with standard care. In reported trials, the median time to progression ranged from 5 to 8.8 months, without a clear trend toward improvement over time, and overall survival ranged from 7 to 16 months (8 to 11 months evaluating only studies for which clinical and radiological eligibility criteria were specified) [2]. These results were compared with a parametric univariate test. Comparison with a non-parametric univariate test, however, was not statistically significant.
End-points for assessment of therapeutic efficacy in brain tumors often give rise to controversy. In curative-intent therapy the overall survival is the main gold standard. In palliative-intent treatment the aim is prolonging OS while maintaining or improving quality of life. However, in the initial evaluation of drugs for the treatment of brain tumors surrogate end-points have been used with increasing frequency. The use of well-established surrogate end-points can likely reflect clinical benefit and speed up drug development [12]. Progression-free survival (PFS) is a popular surrogate end-point validated for high-grade gliomas phase II trials. PFS is hard to evaluate in patients with DIPG, but its value as a surrogate end-point has been demonstrated [13]. Progression is defined by different criteria in clinical trials of patients with DIPG [2], and this can modify the measured outcome. In order to avoid confusion with pseudo response, pseudo progression, and because the usual radiological measure assessments are difficult in DIPG, we used a clinicoradiological progression definition. Clinical progression was registered as an event, but radiological progression was registered as event only if correlated with clinical worsening. Moreover, clinical deterioration due to reversible causes (e.g. hydrocephalus) was not registered as an event (only if it occurred in the setting of a true clinicoradiological worsening). Since this was a retrospective evaluation, there was no rigid protocol of image or clinical monitoring. In our practice, we try to obey a schedule of imaging every 3 months, but local socio-economical limitations impair our ability to comply with this protocol. As a result, monitoring varied between patients. We acknowledge that this may have introduced a bias in the progression date estimate.
In the valproate-treated group, 6 out of 13 patients had a progression time higher than 10 months (300 days), and two patients had a surprisingly long progression-free survival. In contrast, only 1 out of 6 patients not treated with valproate had a progression-free survival longer than 300 days (Table 1). We hypothesize that valproate seizure prophylaxis could have been at least partially responsible for this observed effect. Treatment of seizures with valproic acid has been associated with better survival in adult and pediatric high-grade brain tumor patients that received standard care [14, 15]. Published data do not clearly indicate if valproate has an intrinsic antitumor activity [15]. Valproate could inhibit hepatic microsomal enzymes, leading to higher plasma concentrations of chemotherapy agents [15], but high doses are often needed for this effect and it is unlikely to have clinical impact. Recently, valproate administration to heavily pre-treated children with brain tumor was shown to be safe [16]. In a very recent report, Weller et al. [17] reappraised the EORTC/NCIC glioblastoma temozolomide clinical trial data, showing that patients treated with temozolomide and radiotherapy, as well as with valproic acid, have had a significant survival advantage. A retrospective single-center study and meta-analysis of published data has also confirmed a statistically significant survival advantage in patients with newly diagnosed glioblastoma treated with valproate [18]. Barker et al. [19] have reviewed retrospectively the RTOG data upon glioblastoma patients treated with external beam radiation and have found that valproic acid use correlated with longer survival in patients treated with radiation. In contrast, we have published evidence that showed lack of statistically significant survival advantage in children with malignant brain tumors when treated with prophylactic valproic acid [5].
Valproic acid has epigenetic modulating properties through the inhibition of histone deacetylases (HDAC). Blocking the deacetylation of histones leads to the silencing of a great number of cellular genes. Preclinical and clinical data has shown that valproate inhibits tumor growth and has activity against a varied number of animal tumor models and human cancers [20]. Antiangiogenic properties, secondary to its HDAC inhibitor properties could be one of the mechanisms of the in vivo antiproliferative action of valproate on animal tumor models [21]. Valproic acid induced cytotoxicity and apoptosis, and suppressed invasiveness in glioma cells. The action of valproic acid seems to be cell type-specific, and includes up-regulation of metastasis suppressor reversion-inducing cysteine-rich protein with Kazal motifs (RECK) as well as inhibition of matrix metalloproteinase-2 (MMP-2), both involved in glioma progression [22]. Valproic acid can sensitize human glioma cells to temozolomide and gamma-radiation induced cytotoxicity [23].
Little is known about the molecular landscape of DIPG. However, a recent study has undertaken a genome-wide analysis of single-nucleotide polymorphisms (SNPs) in tumor tissue from DIPG patients. Focal amplifications of PDGFRA and MET genes (and others from ras pathway), and RB gene were frequently found in these tumors [24]. Using whole-genome sequencing followed by targeted sequencing, the Pediatric Cancer Genome Project group has identified single-nucleotide substitutions affecting a conserved domain of both H3F3A and HIST1H3B genes (encoding histones H3.3 and H3.1) [25]. These data imply that DIPG have a unique genetic and molecular signature, and that modified histones are part of this hallmark. It is still unclear what functional modifications are caused by the histone mutations, but large-scale gene expression profile alterations are possible. Thus, epigenetic modulation by drugs like valproic acid is an attractive new therapeutic target in DIPG. Vorinostat, a HDAC-inhibitor drug that has been tested in a phase I trial by the Children’s Oncology Group (COG) [26], is currently being tested in a phase I/II COG trial enrolling patients with DIPG (NCT01189266).
Our patients received a low valproate dose, and trials that successfully demonstrated surrogate markers of epigenetic inhibition by valproate in human patients have used higher doses [20]. Nevertheless, chronic oral administration of 10–20 mg/kg/day of valproate to children can achieve sustained therapeutic range plasma concentrations [27]. The patients reported here had not any measure of surrogate markers of epigenetic inhibition, or of valproate plasma levels. Currently, clinical trials are investigating the use of valproic acid alone or associated with oral chemotherapy for children with brain tumors (NCT01861990, NCT00879437, NCT00107458, NCT00513162). They use different doses and administration schemes. Carboplatin has shown effectiveness in patients with progressive or recurrent brain tumors, especially in patients with low-grade glioma, and its combination with a microtubule-targeting drug as vincristine or vinblastine further enhances the survival outcome of these patients [28]. Both carboplatin and microtubule targeting drugs have shown recently to possess antiangiogenic effect when administered in low, frequent doses (metronomic CT schedule) [29]. No chemotherapy drug scheme has been shown to be effective in DIPG patients and there is no recommended treatment for this group of patients besides palliative-intent radiotherapy [11]. We have been offering compassive non-protocol carboplatin-vincristine-based treatment additionally to radiotherapy to patients diagnosed with DIPG since 2000.
Our study supports a survival-prolonging effect of valproic acid in patients with DIPG. However, it carries inherent limitations, including its retrospective nature, lack of comparative study of drug exposure and a small number of patients. Clearly, further information is needed to make sure valproic acid may have a role in the treatment of DIPG. We think that data from the ongoing clinical trials that enrolled patients with DIPG must be carefully analyzed. This would provide enough information to move forward to plan clinical trials of chemotherapy combinations associated with valproate for diffuse intrinsic pontine tumor patients.
References
Jenkin RD, Boesel C, Ertel I et al (1987) Brain-stem tumors in childhood: a prospective randomized trial of irradiation with and without adjuvant CCNU, VCR, and prednisone. A report of the Children’s Cancer Study Group. J Neurosurg 66(2):227–233
Hargrave D, Bartels U, Bouffet E (2006) Diffuse brainstem glioma in children: critical review of clinical trials. Lancet Oncol 7:241–248
Wells EM, Gaillard WD, Packer RJ (2012) Pediatric brain tumors and epilepsy. Semin Pediatr Neurol 19(1):3–8
Tremont-Lukats I, Ratilal B, Armstrong T et al (2008) Antiepileptic drugs for preventing seizures in people with brain tumors. Cochrane Database Syst Rev 16(2):CD004424
Weller M, Stupp R, Wick W (2012) Epilepsy meets cancer: when, why, and what to do about it? Lancet Oncol 13(9):e375–e382
Kawasaki M, Hernández-Fustes OJ, Machado S, Aguiar LR, Mattar F, Panfilio CB, Hernández-Cossio O (1999) Epilepsia y tumor cerebral. Rev Neurol 28(11):1047–1049
Felix FH, de Araujo OL, da Trindade KM et al (2013) Survival of children with malignant brain tumors receiving valproate: a retrospective study. Childs Nerv Syst 29(2):195–197
Felix FH, Trompieri NM, de Araujo OL, da Trindade KM, Fontenele JB (2011) Potential role for valproate in the treatment of high-risk brain tumors of childhood-results from a retrospective observational cohort study. Pediatr Hematol Oncol 28:556–570
Packer RJ, Lange B, Ater J et al (1993) Carboplatin and vincristine for recurrent and newly diagnosed low-grade gliomas of childhood. J Clin Oncol 11(5):850–856
Macdonald DR, Cascino TL, Schold SC Jr, Cairncross JG (1990) Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol 8(7):1277–1280
Chassot A, Canale S, Varlet P et al (2012) Radiotherapy with concurrent and adjuvant temozolomide in children with newly diagnosed diffuse intrinsic pontine glioma. J Neurooncol 106(2):399–407
Brandes AA, Franceschi E, Gorlia T et al (2012) European Organisation for Research and Treatment of Cancer Brain Tumour Group. Appropriate end-points for right results in the age of antiangiogenic agents: future options for phase II trials in patients with recurrent glioblastoma. Eur J Cancer 48(6):896–903
Hargrave D, Chuang N, Bouffet E (2008) Conventional MRI cannot predict survival in childhood diffuse intrinsic pontine glioma. J Neurooncol 86(3):313–319
Masoudi A, Elopre M, Amini E et al (2008) Influence of valproic acid on outcome of high-grade gliomas in children. Anticancer Res 28(4C):2437–2442
Oberndorfer S, Piribauer M, Marosi C et al (2005) P450 enzyme inducing and non-enzyme inducing antiepileptics in glioblastoma patients treated with standard chemotherapy. J Neuro-Oncol 72:255–260
Wolff J, Kramm C, Kortmann R et al (2008) Valproic acid was well tolerated in heavily pretreated pediatric patients with high-grade glioma. J Neurooncol 90(3):309–314
Weller M, Gorlia T, Cairncross JG et al (2011) Prolonged survival with valproic acid use in the EORTC/NCIC temozolomide trial for glioblastoma. Neurology 77:1156–1164
Guthrie GD, Eljamel S (2012) Impact of particular antiepileptic drugs on the survival of patients with glioblastoma multiforme. J Neurosurg. doi:10.3171/2012.10.JNS12169
Barker CA, Bishop AJ, Chang M, Beal K, Chan TA (2013) Valproic acid use during radiation therapy for glioblastoma associated with improved survival. Int J Radiat Oncol Biol Phys 86(3):504–509
Duenas-Gonzalez A, Candelaria M, Perez-Plascencia C et al (2008) Valproic acid as epigenetic cancer drug: preclinical, clinical and transcriptional effects on solid tumors. Cancer Treat Rev 34(3):206–222
Michaelis M, Michaelis UR, Fleming I et al (2004) Valproic acid inhibits angiogenesis in vitro and in vivo. Mol Pharmacol 65(3):520–527
Chen Y, Tsai YH, Tseng SH (2012) Valproic acid affected the survival and invasiveness of human glioma cells through diverse mechanisms. J Neurooncol 109(1):23–33
Van Nifterik KA, Van den Berg J, Slotman BJ, Lafleur MV, Sminia P, Stalpers LJ (2012) Valproic acid sensitizes human glioma cells for temozolomide and γ-radiation. J Neurooncol 107(1):61–67
Paugh BS, Broniscer A, Qu C, Miller CP, Zhang J, Tatevossian RG, Olson JM, Geyer JR, Chi SN, da Silva NS, Onar-Thomas A, Baker JN, Gajjar A, Ellison DW, Baker SJ (2011) Genome-wide analyses identify recurrent amplifications of receptor tyrosine kinases and cell-cycle regulatory genes in diffuse intrinsic pontine glioma. J Clin Oncol 29(30):3999–4006
Wu G, Broniscer A, McEachron TA, Lu C, Paugh BS, Becksfort J, Qu C, Ding L, Huether R, Parker M, Zhang J, Gajjar A, Dyer MA, Mullighan CG, Gilbertson RJ, Mardis ER, Wilson RK, Downing JR, Ellison DW, Zhang J (2012) Baker SJ; St. Jude Children’s Research Hospital–Washington University Pediatric Cancer Genome Project. Somatic histone H3 alterations in pediatric diffuse intrinsic pontine gliomas and non-brainstem glioblastomas. Nat Genet 44(3):251–253
Hummel TR, Wagner L, Ahern C, Fouladi M, Reid JM, McGovern RM, Ames MM, Gilbertson RJ, Horton T, Ingle AM, Weigel B, Blaney SM (2013) A pediatric phase 1 trial of vorinostat and temozolomide in relapsed or refractory primary brain or spinal cord tumors: a children’s oncology group phase 1 consortium study. Pediatr Blood Cancer 60(9):1452–1457
Su JM, Li XN, Thompson P et al (2011) Phase 1 study of valproic acid in pediatric patients with refractory solid or CNS tumors: a children’s oncology group report. Clin Cancer Res 17(3):589–597
Friedman HS, Krischer JP, Burger P et al (1992) Treatment of children with progressive or recurrent brain tumors with carboplatin or iproplatin: a Pediatric Oncology Group randomized phase II study. J Clin Oncol 10(2):249–256
Mabeta P, Pepper MS (2009) A comparative study on the anti-angiogenic effects of DNA-damaging and cytoskeletal-disrupting agents. Angiogenesis 12(1):81–90
Conflict of interest
The authors declare no potential sources of conflicts of interest and state that the manuscript is not being considered for publication elsewhere and will not be submitted elsewhere while under consideration for this journal.
Author information
Authors and Affiliations
Corresponding author
Additional information
Francisco Helder Cavalcante Felix was also responsible for statistical analysis.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Felix, F.H.C., de Araujo, O.L., da Trindade, K.M. et al. Retrospective evaluation of the outcomes of children with diffuse intrinsic pontine glioma treated with radiochemotherapy and valproic acid in a single center. J Neurooncol 116, 261–266 (2014). https://doi.org/10.1007/s11060-013-1280-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-013-1280-6