Abstract
Temozolomide (TMZ) is given in addition to radiotherapy in glioma patients, but its interaction with the commonly prescribed antiepileptic drug valproic acid (VPA) is largely unknown. Induction of DNA demethylation by VPA could potentially induce expression of the O6-methylguanine-DNA-methyltransferase (MGMT) protein, causing resistance to TMZ and thereby antagonizing its effect. Therefore, this study investigates the interaction between VPA, TMZ, and γ-radiation. Two glioma cell lines were used that differ in TMZ sensitivity caused by the absence (D384) or presence (T98) of the MGMT protein. VPA was administered before (24/48 h) or after (24 h) single doses of γ-radiation; or, after 24 h, VPA treatment was accompanied by a single dose of TMZ for another 24 h. For trimodal treatment the combination of VPA and TMZ was followed by single doses of γ-radiation. In both cell lines VPA caused enhancement of the radiation response after preincubation (DMF0.2 1.4 and 1.5) but not after postirradiation (DMF0.2 1.1 and 1.0). The combination of VPA and TMZ caused enhanced cytotoxicity (DMF0.2 1.7) in both the TMZ-sensitive cell line (D384) and the TMZ-resistant cell line (T98). The combination of VPA and TMZ caused a significant radiation enhancement (DMF0.2 1.9 and 1.6) that was slightly more effective than that of VPA alone. VPA does not antagonize the cytotoxic effects of TMZ. Preincubation with VPA enhances the effect of both γ-radiation and TMZ, in both a TMZ-sensitive and a TMZ-resistant human glioma cell line. VPA combined with TMZ may lead to further enhancement of the radiation response.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
The current standard therapy for patients with newly diagnosed glioblastoma multiforme (GBM) consists of surgery, followed by radiotherapy and temozolomide (TMZ). Compared with radiotherapy alone, radiotherapy with concomitant and adjuvant TMZ improved both median survival and 5-year overall survival [1, 2].
TMZ is an alkylating agent that adds methyl groups to the O6 position of guanine, which eventually leads to cell death [3–5]. The DNA repair protein O6-methylguanine-DNA-methyltransferase (MGMT) is an important mechanism of resistance to TMZ due to its ability to remove the methyl group from the O6 position of guanine [6, 7]. Transcriptional silencing by methylation of the promoter of the MGMT gene is a favorable prognostic factor for patients with GBM treated with radiotherapy and TMZ, as compared with patients treated with radiotherapy alone [8, 9]. Moreover, others and we have demonstrated enhancement of the radiation response by treatment with TMZ in human glioma cells [10–13].
Valproic acid (VPA) is a commonly prescribed antiepileptic drug for the treatment and prevention of seizures in brain tumor patients. Besides its antiseizure property, VPA is reported to inhibit cell proliferation and induce cell differentiation and apoptosis [14, 15]. Furthermore, VPA is an effective inhibitor of histone deacetylase (HDAC) [14–16], which is involved in modulating chromatin structure and gene expression.
Different HDAC inhibitors enhance the radiation response both in vitro and in vivo in various tumor cell types [17–23]. VPA has also been shown to enhance the radiosensitivity of a variety of tumor cell types [24–27], including glioma cell lines [28, 29].
However, less information is available about the interaction of VPA with (γ-)radiation and TMZ. A cause for concern is the DNA demethylation action of VPA [30], which may influence the availability of the DNA repair protein MGMT. Induction of the MGMT protein due to loss of methylation of the MGMT gene promoter might affect the sensitivity of tumor cells to TMZ. If VPA antagonizes the effect of TMZ, it would be contraindicated in GBM patients on radiotherapy plus TMZ.
The present study investigates the interaction of VPA on TMZ and γ-radiation. The experiments were performed using two established glioma cell lines that differ in TMZ sensitivity due to the presence or absence of the MGMT protein.
Methods and materials
Cell lines
Two established glioma cell lines, D384 (astrocytoma grade III) [31] and T98 (GBM), were cultured at 37°C in a humidified atmosphere using (Leibovitch) L15 medium supplied with 10% fetal calf serum, 2 mmol/l l-glutamine, 100 IU/ml penicillin, and 100 IU/ml streptomycin (all from Invitrogen, Breda, The Netherlands). The MGMT protein was detected in the T98 but not in the D384 cell line, which explains the difference in TMZ sensitivity [32]. The D384 cell line was kindly provided by Dr. C.H. Langeveld (Dept. of Neurology, VU University Medical Center Amsterdam, The Netherlands).
Experimental procedures
Experiments were conducted on exponentially growing cells that were seeded before the start of treatments. VPA (Sigma-Aldrich, Zwijndrecht, The Netherlands) was prepared freshly and dissolved in complete culture medium. TMZ (Schering-Plough RS, Houten, The Netherlands) was prepared freshly and dissolved in dimethyl sulfoxide (Sigma-Aldrich) before dilution in culture medium. Final concentrations of the solvent did not affect cell proliferation or clonogenic cell survival. A schematic representation of the treatment protocols showing the timing of administration of the various treatments is presented in Fig. 1. Cells were irradiated at room temperature by single doses of γ-radiation (2–6 Gy) from a 60C source (Gammacell 220; Atomic Energy of Canada, Mississauga, Ontario, Canada). Cell survival was assessed by the clonogenic capacity of single cells.
Schematic representation of the treatment protocols. Cells were incubated with VPA for 24 and 48 h before irradiation (preincubation) or for 24 h after irradiation (postirradiation, delayed plating). For combinations of VPA (48 h) and TMZ (24 h), cells were exposed to 24 h of VPA followed by 24 h coincubation of VPA and TMZ. For the trimodal combination, VPA (48 h) and TMZ (24 h) were added before treatment with γ-radiation. In the combinations with TMZ (with or without γ-radiation) a new dose of VPA was administered daily (2 × 24 h)
Clonogenic assay
Following the experimental treatments, cells were dispersed with trypsin/ethylenediamine tetraacetic acid (EDTA) (Invitrogen) and plated in adequate numbers. The amount of seeded cells (500–50,000 per 25-cm2 culture flask) depended on the estimated survival. After incubation of 10–12 days, the developing cell colonies were fixed with 100% ethanol and stained with 5% Giemsa solution (Merck, Darmstadt, Germany). All colonies in the 25-cm2 culture flasks containing 50 cells or more were counted and considered as cells with unaffected clonogenic capacity. Average plating efficiencies (PE = total number of colonies formed/total number of cells seeded) for D384 and T98 cells were 0.63 ± 0.06 and 0.50 ± 0.030, respectively.
Survival (S) data after dose (D) of radiation, drugs alone, or combinations thereof are presented after correction for the PE of relevant control cells as surviving fractions [SF = S(D)/S(0)]. Thus, raw data for each individual survival curve were normalized for the survival of the associated pre/postirradiation treatment, presenting the effect of radiation treatment alone. Radiation survival data were fitted by a weighted, stratified, linear regression according to the linear-quadratic (LQ) formula S(D)/S(0) = exp-(αD + βD 2) as described by Franken et al. [33] and constructed using GraphPad Prism software (GraphPad Software Inc., La Jolla, CA, USA). All radiation curves showed a relationship between radiation dose and survival (P < 0.05) [33]. Experiments were repeated at least twice, except for the cell line T98 in Fig. 4b and Table 2.
The dose-modifying factor (DMF), the ratio of the radiation dose of the single treatment and the radiation dose for combinations with VPA, TMZ, or both, was calculated at SF level of 0.2. DMF0.2 values were also determined for VPA and TMZ interactions as the ratio of TMZ dose to TMZ dose + VPA.
Results
Effect of VPA on cell proliferation and clonogenic cell survival
Glioma cells were treated with different concentrations of VPA for 24 or 48 h (D384: 0–2.5–5–7.5 mM; T98: 0–1–2.5–5 mM). Exposure to 24 h of VPA in D384 cells resulted in minimal inhibition of cell proliferation (up to 20%). The 48 h incubation with VPA resulted in time- and concentration-dependent inhibition of cell proliferation (up to 68%). VPA did not affect cell proliferation in T98 cells.
The clonogenic capacity after 24 h exposure to VPA of D384 cells was minimally affected (and concentration independent), and a reduction in clonogenic capacity of ~24% was found in T98 cells for the higher concentrations. A stronger and concentration-dependent reduction in clonogenic capacity was shown after 48 h of VPA treatment in both D384 (up to 38%) and T98 cells (up to 35%).
Treatment with a dose of 4 Gy of γ-irradiation following exposure to VPA caused a significant decrease in the clonogenic capacity of both cell lines. The reduction in clonogenic capacity at the highest concentrations in D384 was 68% (24 h) and 96% (48 h), and for T98 it was 93% (24/48 h). The maximum radiation enhancement with an acceptable VPA toxicity was 5 mM VPA in D384 and 2.5 mM VPA in T98. These VPA doses were used for further experiments. Average PE for D384 cells treated with 5 mM VPA was 0.89 ± 0.03 (24 h) and 0.87 ± 0.02 (48 h); average PE for T98 cells treated with 2.5 mM VPA was 0.77 ± 0.04 (24 h) and 0.79 ± 0.04 (48 h).
Effect of γ-radiation prior to or following VPA exposure
Cells were exposed to VPA for either 24 or 48 h prior to treatment with γ-radiation. Figure 2a shows that preincubation of D384 cells with 5 mM VPA caused an enhancement of the radiation response for both the 24 h (DMF0.2 of 1.3) and 48 h (DMF0.2 of 1.4) treatment. Treatment with VPA 48 h prior to irradiation was not more effective than preincubation with 24 h VPA. Figure 2b presents the results for the T98 cells. A clear enhancement of the radiation response is demonstrated after preincubation with 2.5 mM VPA for 24 and 48 h (DMF0.2 of 1.7 and 1.5). No difference was found between the curves for exposure to VPA for 24 and 48 h prior to irradiation.
a, b Effect of γ-radiation after preincubation with 24 h and 48 h of VPA in D384 (a, 5 mM) and T98 (b, 2.5 mM) cells. Survival data are corrected for the plating efficiency of relevant preirradiation treatment (control, 24 h VPA and 48 h VPA). Symbols represent mean ± standard error of the mean (SEM) (N = 3). c, d Effect of γ-radiation with or without 24 h VPA (5 mM D384; 2.5 mM T98) postirradiation in D384 (c) and T98 (d) cells. Survival data are corrected for the plating efficiency of relevant postirradiation treatment (control = 24 h delayed plating and 24 h VPA). Symbols represent mean ± SEM (N = 2)
Furthermore, D384 and T98 cells were treated with γ-radiation followed by a 24 h postirradiation treatment with 5 and 2.5 mM VPA, respectively: the results are shown in Fig. 2c (D384) and d (T98). This postirradiation treatment with VPA did not affect the cytotoxic response of either cell line to irradiation (D384, DMF0.2 of 1.1; T98, DMF0.2 of 1.0).
Effect of TMZ after VPA exposure
Cells were exposed to VPA for 48 h, of which the last 24 h were with coincubation with various concentrations of TMZ. D384 (5 mM VPA) and T98 (2.5 mM VPA) cells were treated with a selected range of TMZ concentrations, in accordance with their sensitivity to the drug.
As shown in Fig. 3, the exposure to VPA made cells more sensitive to TMZ and caused enhancement of the cytotoxic response in both cell lines at concentrations higher than 5 μM (D384, DMF0.2 of 1.7) and 125 μM (T98, DMF0.2 of 1.7).
a, b Effect of TMZ following preincubation with VPA in D384 (a) and T98 (b) cells. Cells were exposed to VPA for 48 h (5 mM D384; 2.5 mM T98), of which the last 24 h were with coincubation with various concentrations of TMZ. Survival data are corrected for the plating efficiency of relevant pretreatment (control and 48 h VPA). Symbols represent mean ± SEM (N = 2, D384; N = 3, T98)
Effect of γ-radiation after preincubation with VPA and TMZ
Different concentrations of TMZ were combined with VPA prior to treatment with a dose of 4 Gy γ-radiation to explore suitable conditions for clonogenic cell survival curves. Table 1 shows the effect of treatment with γ-radiation on clonogenic cell survival after preincubation with TMZ or the combination of VPA and TMZ. Clear radiation enhancement is shown after preincubation with VPA in both D384 and T98 cells. No radiation enhancement was found after preincubation with TMZ alone in D384 cells (Table 1). Preincubation with TMZ seems to sensitize T98 cells to radiation treatment, and the effect appears to be concentration independent (Table 1). The contribution (of various concentrations) of TMZ to the trimodal treatment does not further enhance the radiation response caused by VPA alone in either D384 or T98 cells (Table 1).
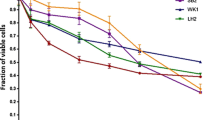
Concentrations of 5 μM TMZ (D384) and 125 μM TMZ (T98) were chosen to investigate the effect of trimodal treatment with VPA, TMZ, and γ-radiation on complete radiation survival curves. D384 and T98 cells were exposed to VPA and TMZ prior to treatment with γ-radiation (2–6 Gy). The cell survival data presented in Fig. 4a show that TMZ had no effect on the radiation response in D384 cells (DMF0.2 of 1.1). A substantial enhancement of the radiation response was demonstrated in D384 cells after preincubation with VPA as a single agent (DMF0.2 of 1.6) or combined with TMZ (DMF0.2 of 1.9). Figure 4b shows that TMZ did not affect the radiation response in T98 cells (DMF0.2 of 1.0). Clear radiation enhancement was caused by VPA as a single agent (DMF0.2 of 1.5) and by the combined drugs (DMF0.2 of 1.6). In both cell lines, preincubation with the combined drugs was slightly more effective for the radiation response than that of VPA alone (Fig. 4a, b).
a, b Effect of γ-radiation after preincubation with 48 h VPA (5 mM D384; 2.5 mM T98), 24 h TMZ (5 μM D384; 125 μM T98), or 48 h VPA of which the last 24 h were with coincubation with TMZ in D384 (a) and T98 (b) cells. Survival data are corrected for the plating efficiency of relevant preirradiation treatment (control, 48 h VPA, 24 h TMZ, or VPA and TMZ combined). Symbols represent mean ± SEM (N = 2, D384) or mean ± standard deviation (SD) (N = 2, T98)
Plating efficiencies corresponding to the data (with 4 Gy) shown in Fig. 4a, b are presented in Table 2. Although TMZ does not contribute to the enhancement of the radiation response in the trimodal treatment combination (Fig. 4a, b), the uncorrected data in Table 2 show that the trimodal combination does benefit from TMZ with respect to overall cell death.
Discussion
The alkylating drug TMZ and the antiepileptic drug VPA are independently known to sensitize for radiation in experimental glioma models [10–13, 28, 29]. However, VPA (frequently prescribed in GBM patients) is a potential antagonist of TMZ [30] and may therefore be contraindicated in GBM patients on radiotherapy plus TMZ. This major clinical concern provided the rationale to investigate the interaction of VPA, TMZ, and γ-radiation in two human glioma cell lines. These cell lines differ in sensitivity to TMZ due to the absence (D384) or presence (T98) of the MGMT protein [32]. Potential demethylation of the promoter region of the MGMT gene by VPA could lead to induction of expression of the MGMT protein, and would cause cells to become (more) resistant to TMZ.
The present study does not support the hypothesis that VPA might antagonize the cytotoxic effects of TMZ. On the contrary, VPA significantly enhances the response to TMZ as well as to γ-radiation in both a TMZ-sensitive and a TMZ-resistant glioma cell line (Figs. 2, 3, 4). This effect is independent of the MGMT protein status. The combination of VPA and TMZ enhances the radiation response, although the contribution of TMZ to the radiation enhancement is minimal (Fig. 4). However, overall cell death is increased in the trimodal over bimodal treatment, which seems to be caused not only by additive cytotoxic effects but also by sensitization of the cytotoxic response to TMZ by pretreatment with VPA (Table 1).
A radiosensitizing effect of VPA in glioma cell lines has been reported earlier [28, 29]. Camphausen et al. [28] showed enhancement of the radiation response in glioma cells in response to VPA exposure both before and after irradiation; VPA exposure before irradiation, without postirradiation exposure, caused less or no radiosensitization. Additional studies in mice showed that VPA starting 3 days before irradiation resulted in enhancement of the radiosensitivity of xenografts [28]. Subsequently, this group investigated the effect of VPA exposure after irradiation, without pre-exposure, and found that exposure to VPA after irradiation of glioma cells induces significant radiosensitization [29]; however, combining VPA both before and after irradiation was more efficient in enhancing radiosensitivity [29].
The present study corroborates that VPA before irradiation positively affects the radiosensitivity of glioma cell lines. However, in contrast to the above-mentioned studies [28, 29], VPA did not enhance the radiation response when given after irradiation. These conflicting results might be due to the fact that different protocols were used to investigate VPA exposure after irradiation. During colony formation our cells were plated in VPA-free medium following a 24 h postirradiation exposure to VPA, while in the other protocols medium containing VPA was used [28, 29].
Besides its activity as an antiepileptic drug, VPA is an HDAC inhibitor [14–16]. Inhibition of HDAC promotes histone acetylation that loosens up the chromatin structure, thereby increasing DNA accessibility. Relaxation of the chromatin structure by treatment with HDAC inhibitors increases the cytotoxicity of several anticancer drugs that target DNA in a variety of tumor cell lines [34]. Studies on glioma cell lines have shown that VPA does increase sensitivity to chemotherapeutic drugs [35, 36]. VPA induces histone acetylation, resulting in increased accessibility of DNA; thereby, VPA could allow demethylases to erase methylation of specific genes [30]. If the promoter of the MGMT gene is demethylated by VPA, TMZ-sensitive cell lines might turn into TMZ-resistant cell lines, thereby counteracting TMZ use during chemoradiotherapy of glioma patients.
However, we found no antagonistic effect of VPA on TMZ in glioma cells. On the contrary, we found a synergistic effect of VPA combined with TMZ. This effect may be caused by VPA loosening up the chromatin, thereby enabling TMZ increased accessibility to the DNA, leading to more methylation, e.g., DNA damage. Our results are supported by others. Sasai et al. [37] combined VPA with 5-aza-2′-deoxycytosine (a DNA methyltransferase inhibitor and a demethylating agent in dividing cells); this combination failed to induce expression of the MGMT protein in glioma cell extracts. Also, Fu et al. [38] recently reported that combined treatment of VPA and TMZ had a synergistic effect on the induction of autophagic cell death in glioma cells both in vitro and in vivo.
The suggestion (arising from this and other studies) that VPA may be a clinically relevant sensitizer of TMZ is tempered by the in vitro experiments of Ständer et al. [39]; this group showed that anticonvulsant drugs fail to potentiate chemotherapy-induced cytotoxicity in human glioma cells at clinically obtained plasma levels. However, most in vitro studies use concentrations of VPA in a higher dose range, mostly from 1 up to 10 mM. Furthermore, the toxic effect of VPA combined with TMZ may give rise to concern about hematotoxic and hepatotoxic side-effects [40–42], although clinically relevant interactions have only rarely been observed [1].
Based on in vitro data, VPA does not antagonize the cytotoxic effect of TMZ and is therefore not contraindicated during chemoradiotherapy of glioma patients. Although promising as a sensitizer of both chemotherapy and radiotherapy, further studies with VPA are warranted. On the other hand it may be more worthwhile to investigate other more sensitive HDAC inhibitors in combination with TMZ and radiation to provide drugs that will be better and more suitable for future clinical application.
References
Stupp R, Mason WP, van den Bent MJ et al (2005) European Organisation for Research and Treatment of Cancer Brain Tumor and Radiotherapy Groups; National Cancer Institute of Canada Clinical Trials Group. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Stupp R, Hegi ME, Mason WP et al (2009) European Organisation for Research and Treatment of Cancer Brain Tumour and Radiation Oncology Groups; National Cancer Institute of Canada Clinical Trials Group. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10:459–466
Kaina B, Ziouta A, Ochs K et al (1997) Chromosomal instability, reproductive cell death and apoptosis induced by O6-methylguanine in Mex-, Mex + and methylation-tolerant mismatch repair compromised cells: facts and models. Mutat Res 381:227–241
D’Atri S, Tentori L, Lacal PM et al (1998) Involvement of the mismatch repair system in temozolomide-induced apoptosis. Mol Pharmacol 54:334–341
Hirose Y, Katayama M, Stokoe D et al (2003) The p38 mitogen-activated protein kinase pathway links the DNA mismatch repair system to the G2 checkpoint and to resistance to chemotherapeutic DNA-methylating agents. Mol Cell Biol 23:8306–8315
Brennand J, Margison GP (1986) Reduction of the toxicity and mutagenicity of alkylating agents in mammalian cells harboring the Escherichia coli alkyltransferase gene. Proc Natl Acad Sci USA 83:6292–6296
Gerson SL (2004) MGMT: its role in cancer aetiology and cancer therapeutics. Nat Rev Cancer 4:296–307
Hegi ME, Diserens AC, Godard S et al (2004) Clinical trial substantiates the predictive value of O-6-methylguanine-DNA methyltransferase promoter methylation in glioblastoma patients treated with temozolomide. Clin Cancer Res 10:1871–1874
Hegi ME, Diserens AC, Gorlia T et al (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 352:997–1003
Van Rijn J, Heimans JJ, van den Berg J et al (2000) Survival of human glioma cells treated with various combination of temozolomide and X-rays. Int J Radiat Oncol Biol Phys 47:779–784
Chakravarti A, Erkkinen MG, Nestler U et al (2006) Temozolomide-mediated radiation enhancement in glioblastoma: a report on underlying mechanisms. Clin Cancer Res 12:4738–4746
Van Nifterik KA, van den Berg J, Stalpers LJ et al (2007) Differential radiosensitizing potential of temozolomide in MGMT promoter methylated glioblastoma multiforme cell lines. Int J Radiat Oncol Biol Phys 69:1246–1253
Kil WJ, Cerna D, Burgan WE et al (2008) In vitro and in vivo radiosensitization induced by the DNA methylating agent temozolomide. Clin Cancer Res 14:931–938
Göttlicher M, Minucci S, Zhu P et al (2001) Valproic acid defines a novel class of HDAC inhibitors inducing differentiation of transformed cells. EMBO J 20:6969–6978
Kostrouchová M, Kostrouch Z, Kostrouchová M (2007) Valproic acid, a molecular lead to multiple regulatory pathways. Folia Biol (Praha) 53:37–49
Phiel CJ, Zhang F, Huang EY et al (2001) Histone deacetylase is a direct target of valproic acid, a potent anticonvulsant, mood stabilizer, and teratogen. J Biol Chem 276:36734–36741
Camphausen K, Scott T, Sproull M et al (2004) Enhancement of xenograft tumor radiosensitivity by the histone deacetylase inhibitor MS-275 and correlation with histone hyperacetylation. Clin Cancer Res 10:6066–6071
Kim JH, Shin JH, Kim IH (2004) Susceptibility and radiosensitization of human glioblastoma cells to trichostatin A, a histone deacetylase inhibitor. Int J Radiat Oncol Biol Phys 59:1174–1180
Chinnaiyan P, Vallabhaneni G, Armstrong E et al (2005) Modulation of radiation response by histone deacetylase inhibition. Int J Radiat Oncol Biol Phys 62:223–229
Entin-Meer M, Rephaeli A, Yang X et al (2005) Butyric acid prodrugs are histone deacetylase inhibitors that show antineoplastic activity and radiosensitizing capacity in the treatment of malignant gliomas. Mol Cancer Ther 4:1952–1961
Karagiannis TC, Harikrishnan KN, El-Osta A (2005) The histone deacetylase inhibitor, Trichostatin A, enhances radiation sensitivity and accumulation of gammaH2A. X. Cancer Biol Ther 4:787–793
Kim IA, Shin JH, Kim IH et al (2006) Histone deacetylase inhibitor-mediated radiosensitization of human cancer cells: class differences and the potential influence of p53. Clin Cancer Res 12:940–949
Entin-Meer M, Yang X, VandenBerg SR et al (2007) In vivo efficacy of a novel histone deacetylase inhibitor in combination with radiation for the treatment of gliomas. Neuro Oncol 9:82–88
Karagiannis TC, Kn H, El-Osta A (2006) The epigenetic modifier, valproic acid, enhances radiation sensitivity. Epigenetics 1:131–137
Chen X, Wong P, Radany E, Wong JY (2009) HDAC inhibitor, valproic acid, induces p53-dependent radiosensitization of colon cancer cells. Cancer Biother Radiopharm 24:689–699
Blattmann C, Oertel S, Ehemann V et al (2010) Enhancement of radiation response in osteosarcoma and rhabomyosarcoma cell lines by histone deacetylase inhibition. Int J Radiat Oncol Biol Phys 78:237–245
Debeb BG, Xu W, Mok H et al (2010) Differential radiosensitizing effect of valproic acid in differentiation versus self-renewal promoting culture conditions. Int J Radiat Oncol Biol Phys 76:889–895
Camphausen K, Cerna D, Scott T et al (2005) Enhancement of in vitro and in vivo tumor cell radiosensitivity by valproic acid. Int J Cancer 114:380–386
Chinnaiyan P, Cerna D, Burgan WE et al (2008) Postradiation sensitization of the histone deacetylase inhibitor valproic acid. Clin Cancer Res 14:5410–5415
Detich N, Bovenzi V, Szyf M (2003) Valproate induces replication-independent active DNA demethylation. J Biol Chem 278:27586–27592
Balmforth AJ, Ball SG, Freshney RI et al (1986) D-1 dopaminergic and beta-adrenergic stimulation of adenylate cyclase in a clone derived from the human astrocytoma cell line G-CCM. J Neurochem 47:715–719
Van Nifterik KA, van den Berg J, van der Meide WF et al (2010) Absence of the MGMT protein as well as methylation of the MGMT promoter predict the sensitivity for temozolomide. Br J Cancer 103:29–35
Franken NA, Rodermond HM, Stap J et al (2006) Clonogenic assay of cells in vitro. Nat Protoc 1:2315–2319
Kim MS, Blake M, Baek JH et al (2003) Inhibition of histonedeacetylase increases cytotoxicity to anticancer drugs targeting DNA. Cancer Res 63:7291–7300
Ciusani E, Balzarotti M, Calatozzolo C et al (2007) Valproic acid increases the in vitro effects of nitrosureas on human glioma cell lines. Oncol Res 16:453–463
Das CM, Aguilera D, Vasquez H et al (2007) Valproic acid induces p21 and topoisomerase-II (alpha/beta) expression and synergistically enhances etoposide cytotoxicity in human glioblastoma cell lines. J Neurooncol 85:159–170
Sasai K, Akagi T, Aoyanagi E et al (2007) O6-methylguanine-DNA methyltransferase is downregulated in transformed astrocyte cells: implications for anti-glioma therapies. Mol Cancer 6:36
Fu J, Shao CJ, Chen FR et al (2010) Autophagy induced by valproic acid is associated with oxidative stress in glioma cell lines. Neuro Oncol 12:328–340
Ständer M, Dichgans J, Weller M (1998) Anticonvulsant drugs fail to modulate chemotherapy-induced cytotoxicity and growth inhibition of human malignant glioma cells. J Neurooncol 37:191–198
Oberndorfer S, Piribauer M, Marosi C et al (2005) P450 enzyme inducing and non-enzyme inducing antiepileptics in glioblastoma patients treated with standard chemotherapy. J Neurooncol 72:255–260
Grewal J, Dellinger CA, Yung WK (2007) Fatal reactivation of hepatitis B with temozolomide. N Engl J Med 356:1591–1592
Neyns B, Hoorens A, Stupp R (2008) Valproic acid related idiosyncratic drug induced hepatotoxicity in a glioblastoma patient treated with temozolomide. Acta Neurol Belg 108:131–134
Acknowledgment
TMZ was a generous gift from Schering-Plough RS. This work was supported by the Dutch Cancer Society (grant no. VU 2000-2149).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Van Nifterik, K.A., Van den Berg, J., Slotman, B.J. et al. Valproic acid sensitizes human glioma cells for temozolomide and γ-radiation. J Neurooncol 107, 61–67 (2012). https://doi.org/10.1007/s11060-011-0725-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-011-0725-z