Abstract
Erroneous beliefs that it is toxic to drink alcohol while taking antiretroviral therapies (ART) used for treating HIV infection, known as alcohol interactive toxicity beliefs, may at least in part account for ART nonadherence among alcohol drinkers. This study was conducted to test a conceptual framework to explain the effects of interactive toxicity beliefs on ART adherence. Computerized surveys were administered to 124 participants receiving HIV care in the southeastern US. Serial mediation model with perceived sensitivity to medicines predicting HIV viral load through three mediating variables: alcohol-ART interactive toxicity beliefs, alcohol-ART avoidance behaviors, and ART adherence. HIV viral load extracted from medical records. Perceived sensitivity to medicines predicted HIV viral load; greater perceptions of medication sensitivity predicted lower HIV viral loads. In addition, there was a significant indirect effect of the serial chain of interactive toxicity beliefs → avoidance behaviors → ART adherence, indicating partial mediation of the relationship between perceived sensitivity to medicines and higher HIV viral load. Perceived sensitivity to medicines provides a conceptual basis for the effects of alcohol-medication interactive toxicity beliefs on ART adherence. Interactive toxicity beliefs are modifiable and can be altered to prevent intentional ART nonadherence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antiretroviral therapies (ART) have transformed HIV infection from a universally fatal disease to a medically manageable chronic illness. ART works to suppress HIV activity and spare damage to the immune system. The hallmark of ART is to suppress HIV replication to a level under which sensitive HIV viral load testing is unable to detect viral activity. Unfortunately, not all people living with HIV are experiencing the full benefits of ART. Alcohol use, for example, impedes ART adherence through multiple mechanisms, including impaired memory, cognitive distortions, hangover effects, and other factors leading to lapses in treatment (Fritz et al., 2010; Hendershot et al., 2009). In addition to alcohol’s role in unintentional nonadherence, recent research has shown that as many as half of people receiving ART who drink alcohol delay or forgo taking their medications when drinking (Fatch et al., 2017; Pellowski et al., 2016). Although ART can certainly have side-effects, which can range from mild to severe, in the absence of liver disease, combining alcohol use with ART is not toxic or harmful. For example, Truvada, a combination of emtricitabine and tenofovir disoproxil fumarate, is among the most commonly used combinations of antiretroviral therapy and its pharmaceutical packaging states “Truvada may cause dizziness. This effect may be worse if you take it with alcohol or certain medicines. Use Truvada with caution. Do not drive or perform other possibly unsafe tasks until you know how you react to it.” Thus, mixing Truvada with alcohol is not completely benign, but does not raise significant toxicity concerns, and there is no warning of health hazards resulting from mixing Truvada with alcohol. Nevertheless, it is common for individuals to believe that it is hazardous to take ART when drinking (Kalichman et al., 2012).
Concerns about mixing ART and alcohol may stem from individual differences in perceived sensitivity to medicines. Among people living with HIV, perceived sensitivity to medicines is associated with ART nonadherence (Horne et al., 2013b), and this association may be mediated by medication concerns (Horne et al., 2013a). Erroneous beliefs that it is toxic to mix ART with alcohol, known as alcohol interactive toxicity beliefs, may at least in part account for the relationship between alcohol use and ART nonadherence and ultimately HIV viral load (Kalichman et al., 2009b, 2012, 2015). Interactive toxicity beliefs may be conceptualized as one facet of a broader medication belief system (Kalichman et al., 2013). In general, beliefs regarding the balance between the perceived necessity of medicines relative to perceived concerns, influence medication uptake and adherence (Horne et al., 2007, 2013a). In addition, individuals who perceive greater sensitivity to medicines may be particularly vulnerable to medication concerns (Nestoriuc et al., 2010), and medication concerns may partially explain the association between perceived sensitivity to medicines and poorer medication adherence (Horne et al., 2013b).
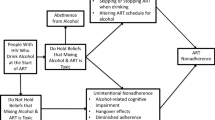
For people who drink alcohol, alcohol-ART interactive toxicity beliefs may explain the association between perceived sensitivity to medicines and ART adherence (Horne et al., 2013b), and ultimately HIV suppression. Specifically, people taking ART who drink, perceive themselves as sensitive to medications, and hold interactive toxicity beliefs may engage in behaviors aimed at avoiding mixing alcohol with ART—such as delaying or stopping medications when drinking—leading to nonadherence and uncontrolled HIV. This chain of associations between interactive toxicity beliefs and alcohol-ART avoidance behaviors may therefore help explain the link between perceived sensitivity to medicine and unsuppressed HIV among patients who drink. In pragmatic terms, interactive toxicity beliefs and their associated behaviors may serve as points of intervention, as beliefs are likely more amenable to change for improving adherence among drinkers than are dispositions such as perceived sensitivity to medicine.
The current study was undertaken to test a serial mediation model where the predicted effects of perceived sensitivity to medicines on HIV viral load would be mediated by three serially positioned variables: interactive toxicity beliefs → alcohol-ART avoidance behaviors → ART adherence. Based on previous studies, we hypothesized that perceived sensitivity to medicines would be associated with greater interactive toxicity beliefs (Faasse et al., 2015; Horne et al., 2013b), which would be related to behaviors intended to avoid mixing ART and alcohol (Kalichman et al., 2015), leading to poorer adherence (Kalichman et al., 2012), and ultimately unsuppressed HIV viral load. Beyond these expected direct effects, we predicted an indirect effect of the serial mediation of beliefs → avoidance → nonadherence on the association between perceived sensitivity to medicines and HIV suppression among people receiving ART who drink alcohol.
Methods
Setting and participants
This study was conducted at a publicly funded HIV clinic in central Georgia. More than 65% of people living with HIV in rural areas of the US reside in southern states and more than half of people living with HIV in Georgia reside in areas outside of major metropolitan areas. The CDC estimates that 1 in 51 Georgians will become HIV infected in their lifetime (CDC, 2016). The 13 counties served by the participating clinic have poverty rates more than double those nationally (US Census, 2017). A total of 124 men and 74 women who had been diagnosed with HIV infection and were being treated for HIV infection at the clinic completed the study measures between February and April, 2016. The current study only included the 79 men and 45 women who reported current use of alcohol.
Computerized interviews
Demographic and health characteristics
Audio computer-assisted self-interviews (ACASI) collected participant demographic characteristics (i.e., gender, age, years of education, ethnicity, employment status, etc.), history of incarceration, mental health treatment, substance use services, and 11 common ART side-effects asked on 4-point scales, 0 = Not experiencing, 3 = Severely experiencing, summed to a total score (Carrieri et al., 2007), alpha = .83. To assess alcohol use we administered the Alcohol Use Disorders Identification Test (AUDIT), a 10-item scale designed to measure alcohol consumption and identify risks for alcohol abuse and dependence (Saunders et al., 1993). The first three items of the AUDIT represent quantity and frequency of alcohol use and the remaining seven items concern problems incurred from drinking alcohol. Scores on the AUDIT range from 0 to 40 and the AUIDT has demonstrated acceptable internal consistency. Scores of greater than 8 indicate high-risk for alcohol use disorders and problem drinking, with demonstrated specificities between .80 and .90 (Maisto et al., 2000). In the current sample, the AUDIT was internally consistent, alpha = .90. We also asked participants whether they had used other drugs, including marijuana, cocaine/crack, inhalants (e.g., poppers), amphetamines, in the past month.
Perceived sensitivity to medicines
We used the Perceived Sensitivity to Medicines scale to assess participant’s perceptions of their sensitivity to medications, i.e., how they view their body’s reactivity and susceptibly to medication effects and side-effects. Conceptual development and psychometric analyses demonstrate the 5-item scale reliable and valid (Faasse et al., 2015; Horne et al., 2013b). Items include “Even small amounts of medicines can upset my body”, “My body overreacts to medicines” and “I usually have stronger reactions to medicines than most people”. Responses were made on a 5-point scale, from 1 = Strongly disagree to 5 = Strongly disagree, with 3 = Uncertain. Scores represent the sum of item responses, ranging from 5 to 25. The Perceived Sensitivity to Medicines scale was internally consistent in the current sample, alpha = .82.
Alcohol-ART interactive toxicity beliefs
Participants completed three indicators of diverging beliefs that underlie motivations to avoid mixing alcohol and ART, specifically measuring beliefs about the hazards of drinking and taking ART. The items were “Alcohol and HIV medications should never be mixed”, “Alcohol breaks down HIV medications so they will not work right”, and “A person should stop taking their HIV medications if they are going to be drinking”. The interactive toxicity beliefs indicators therefore represent a range of misinformation regarding alcohol consumption in relation to taking ART. Items were responded to on 4-point scales, 1 = Strongly disagree to 4 = Strongly agree.
Alcohol-ART avoidance behaviors
Participants completed a measure of behaviors that stem from alcohol-ART interactive toxicity beliefs. This measure explicitly asks about instances of intentionally not taking ART when drinking alcohol (Altice et al., 2001; Sankar et al., 2007). Participants completed six-items concerning actions that they have taken regarding their ART and drinking alcohol (Altice et al., 2001; Kalichman et al., 2009b; Sankar et al., 2007). Items are shown in the results section and were responded to regarding whether participants had performed each of the six actions coded as 0 = Not practiced, 1 = Practiced. Scores represent the summed number of behaviors endorsed.
Medication adherence
We used an established rating scale, The Visual Analogue Scale, to assess ART adherence over the previous month (Giordano et al., 2004). The adherence rating scale asks individuals to indicate the point along a continuum showing how much of their ART they have taken in the past month. For the computerized administration we adapted the response format by using a 100-point slide bar tool anchored by 0%, 50% and 100%. The standard instructions are designed to counter socially desirable response biases by acknowledging that it can be difficult to take ART (Simoni et al., 2006). The instructions read, “We would be surprised if most people take 100% of their medications. Below, 0% means you have taken none of their HIV medications this past month, 50% means you have taken half of your HIV medications this past month and 100% means you have taken every single dose this past month. What percent of your HIV medications did you take?” Participants indicated the percentage of medications taken by clicking their mouse anywhere on the 100-point slide bar continuum. The adherence rating scale used in this study has been found reliable and valid (Finitsis et al., 2016), including significantly associated with HIV viral load (Bangsberg et al., 2001; Giordano et al., 2004; Kalichman et al., 2009a).
HIV viral load and CD4 cell count
Lab reports of HIV viral load and absolute CD4 cell counts were abstracted from electronic medical records. In accordance with HIV treatment guidelines (International Advisory Panel, 2015) we define suppressed HIV viral load as < 200 copies/mL—a threshold that nearly eliminates most cases of apparent viremia caused by HIV viral load blips or assay variability. We used the HIV viral load most proximal to survey completion, coded as 0 = suppressed HIV viral load, and 1 = unsuppressed HIV viral load. We also collected absolute CD4 cell counts to describe participant health status; CD4 cell counts under 500 cells/cc3 indicate immune system impairment and values under 200 cells/cc3 are diagnostic for AIDS. The CD4 cell count most proximal to the survey date was used for sample description.
Procedures
Participants were recruited through targeted convenience sampling. During a scheduled office visit, clinic patients were invited to participate in the study. A total of 257 patients were invited to complete the survey while waiting for their clinical appointment and 198 agreed, yielding a 77% response rate. Following informed consent, participants completed the ACASI and provided permission for the researchers to retrieve their electronic medical records. Participants were compensated for their time to complete the study measures with a $15 cash (ATM) card. The university Institutional Review Boards approved all procedures.
Data analyses
Analyses were performed for the 124 participants reporting current alcohol use on the AUDIT. Our sample size was determined by practical considerations. For descriptive analyses, participants were grouped on the basis of their medical records abstracted HIV viral load: HIV viral load suppressed (< 200 RNA copies/mL, n = 84) and HIV viral load unsuppressed (> 200 RNA copies/mL, n = 40). Descriptive analyses compared HIV viral load suppressed and HIV viral load unsuppressed participants using contingency table X2 tests for categorical variables and independent t-tests for continuous variables. Bivariate associations among continuous variables were examined with Pearson correlation coefficients and point bi-serial correlations for dichotomous HIV viral load in relation to continuous measures. Our main analyses tested the serial mediation model in Fig. 1 that specifies the serial associations between Perceived Sensitivity to Medicines → HIV Viral Load, mediated by Interactive Toxicity Beliefs → Avoiding ART when Drinking → ART Adherence. We used the SPSS PROCESS (v 3.1) macro for mediation analyses to test multiple mediators using bootstrap statistical techniques (Hayes, 2013). Multiple mediator models are appropriately analysed using regression when data are cross-sectional (Judd & Kenny, 1981). The PROCESS macro estimates all paths designated in the model. Specifically, we used the Model 6 Template for multiple (3) mediating variables in an x–y relationship (Hayes, 2013). This model tests the effects of the predictor variable (perceived sensitivity to medicines) on three mediator variables (M1 = alcohol interactive toxicity beliefs, M2 = avoidance behaviors, and M3 = adherence; representing the a paths), the effects of the mediator variables on the outcome (HIV viral load, representing the b paths), and the effects of the predictor variable on the outcome (the c path). PROCESS detects binary outcome variables, such as HIV viral load in this study, and estimates the direct and indirect effects, as well as the paths from the mediating variables to the outcome using logistic regression (Hayes & Mathes, 2009). Thus, coefficients predicting the mediators are estimated using ordinary least squares regression, and paths for the dichotomous outcome are estimated with maximum-likelihood based logistic regression (Hayes, 2013). Our model included participant gender, race, years since testing HIV positive, and experiencing medication side-effects as control variables. These control variables were selected to remove confounding effects of known health disparities in race and gender among people living with HIV, the effects of time on HIV disease progression, and the effects of medication side-effects on ART adherence. We report 95% confidence intervals (CI) for the indirect effects of sensitivity to medicines on HIV viral load via alcohol-ART interactive toxicity beliefs, alcohol-ART avoidance behaviors, and adherence that were estimated from 5000 bootstrap resamples. To examine the robustness of our results, we also repeated the analysis without covariates. There were no missing data for any variables included in the model. All analyses report exact p-values with respect to statistical significance.
Results
Table 1 shows the demographic and health characteristics of the current sample. Participants were diagnosed with HIV infection for more than 11 years on average. In terms of current health status, 12% of the sample showed evidence of advanced HIV disease with CD4 cell counts under 200 and 33% had unsuppressed HIV viral loads. As expected, individuals with unsuppressed HIV viral loads demonstrated poorer ART adherence and lower CD4 cell counts. In addition, participants with suppressed HIV viral load had higher perceived sensitivity to medicines scores.
Alcohol-ART avoidance behaviors
Table 2 shows the number and proportions of participants with suppressed and unsuppressed HIV viral loads reporting behaviors related to intentional nonadherence when drinking. The most frequently occurring behaviors were waiting to take ART after drinking (53%) and not mixing alcohol and HIV medications because it is not safe (39%). In addition, nearly one in three participants indicated that they wait to drink if they have taken their ART and nearly one in four indicated that they stop taking ART when drinking alcohol. There were two alcohol-ART avoidance behaviors for which participants grouped as suppressed HIV viral load versus unsuppressed HIV viral load were significantly different, “I skip taking my HIV medications if I will be drinking alcohol” and “If I know I am going to be drinking alcohol, I won’t take my medications that day.” In both cases, participants with unsuppressed HIV viral load were more likely to avoid mixing alcohol and ART.
Bivariate correlations among model variables
Table 3 shows the Pearson correlations among model variables. Perceived sensitivity to medicines scores were significantly related to interactive toxicity beliefs and inversely related to HIV viral load. As expected, interactive toxicity beliefs were significantly associated with alcohol-ART avoidance behaviors. In addition, alcohol-ART avoidance behaviors were significantly inversely related to ART adherence, and adherence was inversely related to HIV viral load. This pattern of associations was consistent with testing the proposed mediation model.
Perceived sensitivity to medicines and HIV viral load serial mediation model
We tested the serial mediation model using multiple regression analyses that included medication sensitivity (independent variable), HIV viral load (dependent variable), and alcohol interactive toxicity beliefs, alcohol-ART avoidance behaviors, and ART adherence (mediating variables). Results of the regression model are shown in Fig. 1. The full model was significant in predicting HIV viral load, Model X2 = 22.53, p = .01, using McFadden estimated R2 the model accounted for 15.77% of the variance in HIV viral load.
For tests of direct effects, results showed that increased perceived sensitivity to medicines relates to lower odds of detectable HIV viral load, b = − .089 (se = .052), p = .09, 95% CI − .193 to .014. The direct effect of perceived sensitivity to medicines on alcohol interactive toxicity beliefs was significant, b = .122, t = 2.26, p = .02, but not alcohol-ART avoidance behaviors, b = − .020, t = -0.63, p = .52, and not ART adherence, b = − .030, t = 0.05, p = .95. Alcohol interactive toxicity beliefs were significantly related to alcohol-ART avoidance behaviors, b = .246, t = 4.45, p = .01, and alcohol-ART avoidance behaviors were in turn related to ART adherence, b = -4.017, t = -2.31, p = .02, and ART adherence was related to lower odds of detectable HIV viral load, b = − .033, t = -3.72, p = .01.
The mediation effects of the three serial mediators were tested using 5000 bootstrap resamples. The indirect effect of perceived sensitivity to medicines on HIV viral load through the three serially aligned mediators (Interactive Toxicity Beliefs → Avoiding ART when Drinking → ART Adherence) on HIV viral load was significant, b = − .004, se .003, 95% CI − .0158 to − .0003. All other possible mediation paths were included in the model and none of the other indirect effects were significant.
Mediation model controlling for potential confounds
We repeated the serial mediation model controlling for gender, race, years since testing HIV positive, and ART side effects. Results showed the full model remained significant in predicting HIV viral load, Model X2 = 24.92, p = .01, McFadden R2 indicated that the model explained 17.71% of the variance. Examination of control variables in relation to viral load showed that there were no significant effects of gender, b = − .307, p = .52; race, b = − .258, p = .62; years since testing HIV positive, b = .016, p = .57; or side-effects, b = − .610, p = .17. The tests of direct effects showed that perceived sensitivity to medicines significantly predicted HIV viral load, b = − .119 (se = .056), p = .03, 95% CI − .230 to − .009. The direct effect of perceived sensitivity to medicines predicting alcohol interactive toxicity beliefs was also significant, b = .125, t = 2.23, p = .02, but not alcohol-ART avoidance behaviors, b = − .026, t = − .77, p = .44, and not ART adherence, b = − .163, t = − .25, p = .79. Alcohol interactive toxicity beliefs significantly predicted alcohol-ART avoidance behaviors, b = .230, t = 3.99, p = .01, alcohol-ART avoidance behaviors predicted ART adherence, b = -4.461, t = -2.47, p = .01, and ART adherence predicted HIV viral load, b = − .035, t = -3.70, p = .00 = 1. The indirect effect of perceived sensitivity to medicines on HIV viral load through the three serially aligned mediators (Interactive Toxicity Beliefs → Avoiding ART when Drinking → ART Adherence) on HIV viral load was significant, b = − .004, se .004, 95% CI − .0200 to − .0002. All other possible mediation paths were included in the model and again none of the other indirect effects were significant.
Discussion
Results supported our hypothesis that interactive toxicity beliefs would fit within a broader framework of perceived sensitivity to medicines. However, perceived sensitivity to medicines itself is part of an even broader framework of mental representations or more general beliefs (social representations) about medicines as a class of treatment (Horne et al., 1999). In particular, individuals who are suspicious of pharmaceuticals, perceiving them to be fundamentally harmful and over-prescribed by doctors (Horne et al., 1999) characterize a ‘world-view’ of suspicions about chemicals in food and the environment (Gupta & Horne, 2001). Thus, how people vary in their perceptions of personal sensitivity to the effects of medicines relates to their use of medicines. Believing that one is more sensitive than other people to the effects of medicines leads to a reluctance to start medications (Horne et al., 2013b). Beliefs about medications, perceptions of the self in relation to medicines, and other personal attributes, such as drinking alcohol, can be thought of as ‘pharmaceutical schema’, that is how ideas about pharmaceuticals are organized. Future research is needed to test these concepts as predictors of medication refusal and intentional ART nonadherence.
Cognitive-perceptual processes regarding the interplay between medicines and bodily sensations offer a unifying framework for understanding the more narrowly focused beliefs about mixing alcohol with medications. We found that direct effects of perceived sensitivity to medicines on HIV viral load were mediated by the serial effects of beliefs and behaviors. Greater perceptions of medication sensitivity were associated with stronger beliefs that it is harmful to mix alcohol with ART, which in turn lead to behaviors directed at intentionally altering taking medication to avoid mixing alcohol with ART, which in turn predicts ART nonadherence and higher HIV viral loads. The indirect effects in our serial mediation model did not fully account for the relationship between perceived sensitivity and HIV viral load, however, indicating that our framework is incomplete and there are likely other explanatory variables for the relationship in addition to interactive toxicity beliefs.
Our findings are consistent with several other studies that have shown that alcohol-ART interactive toxicity beliefs are prevalent among people living with HIV and lead to intentional medication nonadherence (Altice et al., 2001; Fatch et al., 2017; Kalichman et al., 2012; Sankar et al., 2007). Interactive toxicity beliefs may originate from overgeneralizing the true risks of mixing alcohol with other medications, such as sedatives, anti-depressants, and some over-the-counter remedies (Jalbert et al., 2008). Adding to confusion may be reports in the early years of HIV treatment concerning adverse interactions between some drugs in one class of ART (Protease Inhibitors) and some illicit drugs (McCance-Katz et al., 2013). Individuals are also likely to hear that it is harmful for people with liver disease to mix alcohol with ART. These messages, however, are likely distorted given that all patients with compromised liver functions are advised not to drink at all, regardless of mixing alcohol with ART. Medication beliefs can underlie behaviors aimed to avoid mixing alcohol and ART, as has been demonstrated specifically for interactive toxicity beliefs and ART adherence among alcohol drinkers (Pellowski et al., 2016) and other drug users (Kalichman et al., 2015). In the current study, we tested perceived sensitivity to medicines as a broader construct to develop the first conceptual framework to encompass interactive toxicity beliefs, alcohol-ART avoidance behaviors, and ART adherence.
Results of the current study should be interpreted in light of its methodological limitations. We sampled participants receiving services from a publicly funded HIV care provider and our sample was one of convenience. Thus, our participants cannot be considered representative of people living with HIV. In addition, the study was conducted in just one state in the southeastern US, and is therefore also geographically constrained. We specifically focused on individuals living with HIV who self-report alcohol use. The limitations of self-reported drinking are well known and likely resulted in removing people from our study who did not openly acknowledge their drinking. We also relied on self-reported measures for all of the other social and behavioral variables in this study. Although we used measures delivered by computerized interviews, the results are still subject to reporting biases. In addition, our measure of interactive toxicity beliefs consisted of only three indicators. In addition, the results while statistically significant were of modest magnitude and should be considered preliminary and in need of independent replication. Finally, the study design was cross-sectional and therefore does not allow for directional or causal inferences among variables. With these limitations in mind, we believe that the current findings have implications for designing interventions aimed to address intentional nonadherence among people receiving ART who drink alcohol.
While the indirect effects of the serial mediators in our model were significant, they did not fully account for the relationship between perceived medicine sensitivity and HIV viral load. The model has thus far only been evaluated in one sample with a small to moderate effect. Our findings therefore require independent replication with larger sample sizes and in different geographical regions. Furthermore, other behaviors and psychological processes may contribute to the model and call for additional study. For example, Horne et al. (2013b) suggested that perceived sensitivity to medicines is one of several potential features of an individual’s underlying schema of the physical and functional self and is likely to impact self-regulation through ongoing somatic sensations and functional changes. Each of these processes may impact ART adherence and may interact with beliefs about alcohol and other drug use in relation to taking ART.
Our model, albeit with preliminary support, also points to windows of opportunity for interventions. Perceived sensitivity to medicines bolsters the very foundation for taking medicines—that they will have an impact on bodily systems. Perceptions of sensitivity are therefore potentially beneficial for optimizing adherence and treatment outcomes. Interactive toxicity beliefs and their associated intentional nonadherence behaviors undermine, but do not entirely negate, these associations. Interactive toxicity beliefs are modifiable, and likely more malleable than dispositions such as perceived sensitivities, and altering underlying beliefs can be translated into behavioral intentions and behavior (Ajzen & Fishbein, 1980). Direct communication with patients who drink alcohol should emphasize both the safety of ART when taken in proximity to alcohol and the potency of ART when taken as directed. Left unchecked, interactive toxicity beliefs and their association with alcohol-ART avoidance behaviors will erode confidence in medicines and undermine ART adherence.
References
Ajzen, I., & Fishbein, M. (1980). Understanding attitudes and predicting social behavior. Englewood Cliffs, NJ: Prentice-Hall.
Altice, F., Mostashari, F., & Friedland, G. (2001). Trust and the acceptance of and adherence to antiretroviral therapy. Journal of Acquired Immune Deficiency Syndrome, 28, 47–58. https://doi.org/10.1097/00126334-200109010-00008
Bangsberg, D. R., Hecht, F. M., Charlebois, E. D., Chesney, M., & Moss, A. (2001). Comparing objective measures of adherence to HIV antiretroviral therapy: Electronic medication monitors and unannounced pill counts. AIDS and Behavior, 5, 275–281. https://doi.org/10.1023/a:1011396711486
Carrieri, M. P., Villes, V., Raffi, F., Protopopescu, C., Preau, M., Salmon, D., et al. (2007). Self-reported side-effects of anti-retroviral treatment among IDUs: A 7-year longitudinal study. International Journal of Drug Policy, 18, 288–295. https://doi.org/10.1016/j.drugpo.2007.01.014
CDC. (2016). Lifetime risk of HIV diagnosis. Retrieved 2016, from http://www.cdc.gov/nchhstp/newsroom/2016/croi-press-release-risk.html
Faasse, K., Grey, A., Horne, R., & Petrie, K. J. (2015). High perceived sensitivity to medicines is associated with higher medical care utilisation, increased symptom reporting and greater information-seeking about medication. Pharmacoepidemiol Drug Safety, 24, 592–599. https://doi.org/10.1002/pds.3751
Fatch, R., Emenyonu, N. I., Muyindike, W., Kekibiina, A., Woolf-King, S., & Hahn, J. A. (2017). Alcohol interactive toxicity beliefs and ART nonadherence among HIV-infected current drinkers in Mbarara, Uganda. AIDS and Behavior, 21, 1812–1824. https://doi.org/10.1007/s10461-016-1429-3
Finitsis, D. J., Pellowski, J. A., Huedo-Medina, T. B., Fox, M. C., & Kalichman, S. C. (2016). Visual analogue scale (VAS) measurement of antiretroviral adherence in people living with HIV (PLWH): A meta-analysis. Journal of Behavioral Medicine, 39, 1043–1055. https://doi.org/10.1007/s10865-016-9770-6
Fritz, K., Morojele, N., & Kalichman, S. (2010). Alcohol: The forgotten drug in HIV/AIDS. Lancet, 376, 398–400. https://doi.org/10.1016/s0140-6736(10)60884-7
Giordano, T. P., Guzman, D., Clark, R., Charlebois, E. D., & Bangsberg, D. (2004). Measuring adherence to antiretroviral therapy in a diverse population using a visual analogue scale. HIV Clinical Trials, 5, 74–79. https://doi.org/10.1310/jfxh-g3x2-eym6-d6ug
Gupta, K., & Horne, R. (2001). The influence of health beliefs on the presentation and consultation outcome in patients with chemical sensitivities. Journal of Psychosomatic Research, 50, 131–137. https://doi.org/10.1016/s0022-3999(00)00218-x
Hayes, A. F. (2013). Model templates for PROCESS for SPSS and SAS. New York: Guilford Press.
Hayes, A. F., & Mathes, J. (2009). Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behavior Research Methods, 41, 929–936.
Hendershot, C. S., Stoner, S. A., Pantalone, D. W., & Simoni, J. M. (2009). Alcohol use and antiretroviral adherence: Review and meta-analysis. Journal of Acquired Immune Deficiency Syndromes, 52, 180–202. https://doi.org/10.1097/qai.0b013e3181b18b6e
Horne, R., Chapman, S. C., Parham, R., Freemantle, N., Forbes, A., & Cooper, V. (2013a). Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: A meta-analytic review of the Necessity-Concerns Framework. PLoS ONE, 8, e80633. https://doi.org/10.1371/journal.pone.0080633
Horne, R., Cooper, V., Gellaitry, G., Date, H. L., & Fisher, M. (2007). Patients’ perceptions of highly active antiretroviral therapy in relation to treatment uptake and adherence: The utility of the necessity-concerns framework. Journal of Acquired Immune Deficiency Syndromes, 45, 334–341. https://doi.org/10.1097/qai.0b013e31806910e3
Horne, R., Faasse, K., Cooper, V., Diefenbach, M. A., Leventhal, H., Leventhal, E., et al. (2013b). The perceived sensitivity to medicines (PSM) scale: An evaluation of validity and reliability. British Journal of Health Psychology, 18, 18–30. https://doi.org/10.1111/j.2044-8287.2012.02071.x
Horne, R., Weinman, J., & Hankins, M. (1999). The beliefs about medicines questionnaire: The development and evaluation of a new method for assessing the cognitive representation of medication. Psychology and Health, 14, 1–24. https://doi.org/10.1080/08870449908407311
International Advisory Panel on, HIV Care Continuum Optimization. (2015). IAPAC guidelines for optimizing the HIV care continuum for adults and adolescents. Journal of the International Association of Providers of AIDS Care, 14, S3–S34. https://doi.org/10.1177/2325957415613442
Jalbert, J. J., Quilliam, B. J., & Lapane, K. L. (2008). A profile of concurrent alcohol and alcohol-interactive prescription drug use in the US population. Journal of General Internal Medicine, 23, 1318–1323. https://doi.org/10.1007/s11606-008-0639-4
Judd, C. M., & Kenny, D. A. (1981). Process analysis: Estimating mediation in treatment evaluations. Evaluation Review, 5, 602–619. https://doi.org/10.1177/0193841x8100500502
Kalichman, S. C., Amaral, C. M., Swetzes, C., Jones, M., Macy, R., Kalichman, M. O., et al. (2009a). A simple single-item rating scale to measure medication adherence: Further evidence for convergent validity. Journal of the International Association of Physicians in AIDS Care, 8, 367–374. https://doi.org/10.1177/1545109709352884
Kalichman, S. C., Amaral, C. M., White, D., Swetsze, C., Kalichman, M. O., Cherry, C., et al. (2012). Alcohol and adherence to antiretroviral medications: Interactive toxicity beliefs among people living with HIV. Journal of the Association of Nurses in AIDS Care, 23, 511–520. https://doi.org/10.1016/j.jana.2011.11.005
Kalichman, S. C., Amaral, C. M., White, D., Swetsze, C., Pope, H., Kalichman, M. O., et al. (2009b). Prevalence and clinical implications of interactive toxicity beliefs regarding mixing alcohol and antiretroviral therapies among people living with HIV/AIDS. AIDS Patient Care STDS, 23, 449–454. https://doi.org/10.1089/apc.2008.0184
Kalichman, S. C., Grebler, T., Amaral, C. M., McNerey, M., White, D., Kalichman, M. O., et al. (2013). Intentional nonadherence to medications among HIV positive alcohol drinkers: Prospective study of interactive toxicity beliefs. Journal of General Internal Medicine, 28, 399–405.
Kalichman, S. C., Kalichman, M. O., Cherry, C., Hoyt, G., Washington, C., Grebler, T., et al. (2015). Intentional medication nonadherence because of interactive toxicity beliefs among HIV-positive active drug users. Journal of Acquired Immune Deficiency Syndromes, 70, 503–509.
Maisto, S. A., Conigliaro, J., McNeil, M., Kraemer, K., & Kelley, M. E. (2000). An empirical investigation of the factor structure of the AUDIT. Psychological Assessment, 12, 346–353. https://doi.org/10.1037//1040-3590.12.3.346
McCance-Katz, E. F., Gruber, V. A., Beatty, G., Lum, P. J., & Rainey, P. M. (2013). Interactions between alcohol and the antiretroviral medications ritonavir or efavirenz. Journal of Addiction Medicine, 7, 264–270. https://doi.org/10.1097/adm.0b013e318293655a
Nestoriuc, Y., Orav, E. J., Liang, M. H., Horne, R., & Barsky, A. J. (2010). Prediction of nonspecific side effects in rheumatoid arthritis patients by beliefs about medicines. Arthritis Care Research, 62, 791–799. https://doi.org/10.1002/acr.20160
Pellowski, J. A., Kalichman, S. C., Kalichman, M. O., & Cherry, C. (2016). Alcohol-antiretroviral therapy interactive toxicity beliefs and daily medication adherence and alcohol use among people living with HIV. AIDS Care, 28, 963–970. https://doi.org/10.1080/09540121.2016.1154134
Sankar, A., Wunderlich, T., Neufeld, S., & Luborsky, M. (2007). Sero-positive African Americans’ beliefs about alcohol and their Impact on anti-retroviral adherence. AIDS and Behavior, 11, 195–203. https://doi.org/10.1007/s10461-006-9144-0
Saunders, J. B., Aasland, O. G., Babor, T. F., DeLaFuente, J. R., & Grant, M. (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption II. Addictions, 88, 791–804. https://doi.org/10.1111/j.1360-0443.1993.tb02093.x
Simoni, J., Kurth, A. E., Pearson, C., Pantalone, D. W., Merrill, J., & Frick, P. (2006). Self-report measures of antiretroviral therapy adherence: A review with recommendations for HIV research and clinical management. AIDS and Behavior, 10, 227–331. https://doi.org/10.1007/s10461-006-9078-6
US Census. (2017). Quick facts: Georgia. Available from the US Census https://www.census.gov/quickfacts/GA. Accessed September 1, 2017.
Funding
This project was supported by National Institute of Alcohol Abuse and Alcoholism Grant R01-AA023727.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Seth C. Kalichman, Rob Horne, Harold Katner, and Dominica Hernandez declare that they have no conflicts of interest.
Human and animal rights and Informed consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research ethics committee (IRB) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all participants included in this study.
Rights and permissions
About this article
Cite this article
Kalichman, S.C., Horne, R., Katner, H. et al. Perceived sensitivity to medicines, alcohol interactive toxicity beliefs, and medication adherence among people living with HIV who drink alcohol. J Behav Med 42, 392–400 (2019). https://doi.org/10.1007/s10865-018-9987-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-018-9987-7