Abstract
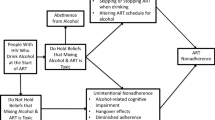
Alcohol consumption has been associated with HIV disease progression; yet, the nature of this association is poorly understood. This study sought to determine the influence of patient beliefs about alcohol on ART adherence, and elucidate clinician beliefs about drinking and taking ART. Most patients (85%) believed alcohol and ART do not mix. The three alcohol consumption groups, light, moderate, and heavy, differed in their beliefs about drinking and ART with 64% of light and 55% of moderate drinkers skipping ART when drinking compared to 29% of heavy drinkers. Beliefs were derived from folk models of alcohol–ART interaction. Patients 50 and older were less likely to skip ART when drinking. Alcohol appears to affect adherence through decisions to forgo ART when drinking not through drunken forgetfulness. Furthermore, over one-half of clinicians believed alcohol and ART should not be taken together. These findings have implications for patient care and physician training.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A high level of adherence to anti-retroviral therapy (ART) is required for therapeutic effectiveness against HIV. Research suggests that 95% of doses must be taken to achieve viral suppression (Paterson, Swindells, & Mohr, 2000), although the exact relationship between adherence to ART and viral suppression has yet to be specified (Bangsberg, Charlebois, & Grant, 2003). Inadequate adherence results in a generally poor long-term prognosis and in the emergence of treatment resistant viral strains, a public health threat. Repeated attempts to identify individual traits or characteristics (e.g., demographics) that correlate with adherence have failed (Reynolds, 2004), although several studies have associated older age with increased adherence (e.g., Hinkin, Hardy, & Hardy, 2004). Attention has thus shifted to potentially improving adherence by identifying modifiable features associated with adherence such as substance use (Ferrando, Wall, Batki, & Sorensen, 1996), depression (Arnsten et al., 2002), forgetfulness (Fong et al., 2003), and isolation (Altice, Mostashari, & Friedland, 2001).
Alcohol consumption among people taking ART is a potentially significant challenge to adherence (Halkitis, Parsons, Wolitski, & Remien, 2003) and one that is modifiable. A previous investigation (Samet, Horton, Traphagen, Lyon, & Freedberg, 2003) found that patients on ART who had a history of alcohol problems also had higher viral load and lower CD4 counts. Another study (Conigliaro, Gordon, McGinnis, & Rabeneck, 2003) identified excessive alcohol use among 33% of their sample of 881 sero-positive veterans. The 20% of their sample labeled as hazardous drinkers and the 33% labeled as binge drinkers were more likely to have detectable viral loads than those without drinking problems. The authors speculate that alcohol may contribute to disease progression through non-adherence. Indeed, recently (Murphy, Marelich, Hoffman, & Steers, 2004) it was found that study participants who were light or non-drinkers were more likely to be adherent. In the Murphy study the major impact of alcohol was to reduce the ability to maintain a pill taking schedule. This is consonant with earlier work (Cook et al., 2001) showing that problem drinkers, (i.e., not alcoholics by DSM 3 criteria, but consuming enough alcohol to cause problems in health and functioning) were slightly more likely to report missed doses (17% vs. 12%) and significantly more likely to take a dose off schedule (45% vs. 26%). Problem drinkers were more likely to be younger and to report taking medication off schedule in association with heavy drinking.
Although the studies discussed above suggest that non-adherent behavior derives from alcohol-induced memory lapses (e.g., Murphy et al., 2004) or from alcohol “blurring” the importance of dose timing, another possible explanation is that patient beliefs about the deleterious effects of drinking alcohol and taking ART may contribute to non-adherence. Beliefs about ART have previously been associated with several aspects of adherence. For example, it was demonstrated (Malcolm, Ng, Rosen, & Stone, 2003) that patients who believed that they must be 90–100% adherent for their medications to work were more adherent than those who did not hold these beliefs. In a repeat-measure study (Spire Duran, & Souville, 2002) it was found that various patient beliefs about ART, both negative and positive, at the study outset were more predictive of adherence at the four month follow-up than any biomedical or regimen characteristics. Earlier investigations (Martini, Nasta, Ricci, Parazzini, & Agnoletto, 2000; Smith, Rapkin, Morrison, & Kammerman, 1997; Weidle, Ganea, & Irwin, 1999) discovered that beliefs about ART efficacy were more strongly related to levels of adherence than beliefs about HIV. A study of prisoner adherence to ART in which most of the participants were active drug users (Altice et al., 2001) found that a belief that using street drugs and taking ART is a toxic combination led to skipping medication doses. The majority of prisoners interviewed (N = 205) believed it would be harmful to take street drugs while on ART; and 33% said they would not take their medications if they planned to get high the same day.
Although the physiological effects of consuming alcohol may contribute to patients taking doses off schedule or missing anti-retroviral doses, and drinking may result in individuals forgetting about their medications, it appears at least promising to investigate the potential role that beliefs about drinking alcohol and taking ART may play in adherence practice.
The objective of the study reported here was to assess the nature and content of beliefs of sero-positive African Americans taking ART and the clinicians who treat them concerning the advisability of consuming alcohol while on ART and to determine if and how these beliefs affect adherence practice.
This study focuses on African Americans taking ART because African American ethnicity has been associated with alcohol-related adherence problems (Conigliaro et al., 2003); and also because African Americans have a much higher infection rate than whites and higher morbidity and mortality rates than sero-positive whites (McGinnis, Sharma, & Skanderson, 2003). In particular, African American men aged 40–49 have the highest rate of infection in the United States (Brown, 2005).
Method
Participants and Procedures
The sample (N = 82 patients, 17 clinicians) was drawn from a 5 year ongoing longitudinal qualitative study of ART adherence (N = 137 African Americans with HIV; 30 clinicians providing their treatment). The sample for the study reported here consists of the first 82 participants enrolled in the parent study and the 17 clinicians providing their care. The sample was recruited from the infectious disease clinics of two inner-city hospitals. At one hospital, the infectious disease clinic has a HIV patient load of approximately 1,115 of whom 75–82% are African American and at the other hospital the clinic sees about 1,800 HIV+ patients each year, of whom 60–65% are African American. Eighty percent of patients at both clinics are taking ART. The two HIV clinic populations include 28% active substance users, 10% alcohol abusers, 30% have Hepatitis B, 20–25% Hepatitis C, 20–25% have mental illness, and 5% are homeless.
Clinic personnel informed potential study participants of the study. Individuals interested were asked to call the study office for screening. Patients are paid for their participation in the study. Clinic data (CD4, viral load, length of time on medication, ART regimen) were collected within 2 weeks of each interview from clinic records by trained medical records personnel after HIPAA consent was obtained.
Interviews were conducted in respondents’ homes and in the clinicians’ offices, and were tape recorded and transcribed verbatim.
Responses to each question underwent a process of data reduction called “gisting” in which the central idea or ideas of the response were summarized according to established criteria by trained data analysts (Luborsky, 1994). The gists for each question were then reviewed to identify major themes. All responses to a specific question were sorted by a team of three people. Any gists that did not fit into identified categories were discussed by the entire research team until the differences were resolved or a new category was created.
Measures
To identify the beliefs, categories and reasoning that shape patients’ understanding of the relationship between alcohol and ART, a multi-method approach was adopted.
A set of 10 questions for patients was developed based on an approach utilized earlier (Hunt, Arar, & Larme, 1998) to identify differences and similarities in physician and patient explanatory models. The questions assessed beliefs about drinking alcohol while taking ART and sought to determine if these beliefs were calibrated according to the type of alcohol ingested (beer, wine, hard liquor), amount (1 drink, 2–4 drinks, intoxicated), and whether they affected the timing of an ART dose (take late if drinking, take early if planning to drink; e.g., “Does taking your ART dose before or after you are drinking make a difference?”). Participants were asked specifically if they had deliberately skipped a dose because of drinking alcohol. They were also queried about whether they had discussed their beliefs about drinking and taking ART with their physicians and, if so, what the physician’s responses were.
Substance use (alcohol and street drugs) was assessed using the GAIN Screener (Dennis, 1999) which asks about alcohol and substance use over the past 3 months. The Global Appraisal of Individual Needs (GAIN) is a standardized clinical assessment which has been normed on both adults and adolescents (Dennis, 1999; Dennis, Scott, Godley, & Funk, 2000). It has eight main sections (background, substance use, physical health, risk behavior, mental health, environmental, legal, vocational). It provides approximately one hundred symptom, change score and utilization indices, and is designed to map onto ASAM and DSM-IV. The core indices have Cronbach alphas over 0.85 (most over 0.9).
Clinicians (four attending physicians, eight infectious disease fellows, three nurse practitioners, two pharmacists) were asked a set of 10 questions also adapted from the work of Hunt and colleagues (1998). Two questions assessed clinician beliefs concerning the interaction between alcohol and ART. Eight focused on clinician communication with their patients about drinking alcohol and being on ART.
Data Analyses
A random sample of gists was assigned to categories by each research team member to establish inter-rater reliability. Categories were derived from the literature and from thematic analysis. Differences among research team members in assigning these gists to specific codes were discussed until an inter-rater reliability rate of 92% among the three coders was achieved. The remaining gists were then divided among the research team and assigned to the established categories. This process was repeated for each of the 10 questions for the patients and clinicians alike.
Patients were assigned to alcohol use groups (light, moderate, heavy) based on their repeated responses to the GAIN screener items assessing amount of alcohol consumed in the past 3 months, and the number of days on which an individual had consumed five or more drinks at one sitting—taken as an indication of binge drinking. The GAIN Screener was administered during each interview; we averaged these scores over five interviews (18 months) to ensure that seasonal or ritual alcohol consumption did not skew an individual’s rate of consumption.
Simple statistical tests were employed to determine relationships among levels of alcohol consumption, and beliefs about alcohol and ART.
Results
Participant Characteristics
Sample Characteristics
The patient sample was entirely African American, on average middle-aged (mean age 43.3); more than one-half had completed high school, and one-quarter had some post-secondary education. Women made up about a quarter of the sample. Approximately 75% of the sample was unemployed, and 63% of the sample had never been married. The clinician sample ranged in age from 27–62 years old and consisted of about 60% women.
Alcohol Use Groups
Three alcohol use groups were created using data from the GAIN Screener. The light use group (42 %) reported one or no drinks in the last three months and no binge drinking. The moderate drinker group (37.8%) had on average 1–11 drinks in the last 3 months and 1 or fewer episodes of binge drinking; and the heavy drinkers (20.7%) reported more than 12 drinks on average in the last three months and at least one episode of binge drinking.
Patient Beliefs about Drinking Alcohol and Taking ART
Do Alcohol and ART Mix?
Eighty-five percent of patients agreed with the statement “ART and alcohol do not mix” ; and 90% agreed with the statement “It’s common knowledge that you should never drink alcohol with any type of prescription medication.” But when asked specifically about drinking alcohol and taking ART, the picture became more complex. Not surprisingly, those who drank more (heavy drinkers) were more likely to believe that it is harmless to drink alcohol and take ART (47%) compared to light drinkers (10%) or moderate drinkers (26%), χ 2(79, 2) = 8.5, P < 0.01.
Light drinker: “You’re never to suppose to drink alcohol when you’re taking medication. Lots of people do it, but I stopped.”
Light drinker: “My doctor told me that they don’t mix, you’re not supposed to take alcohol when taking the HAART medication – period.”
Moderate Drinker: “You should wait at least two hours after you take your meds to consume alcohol and also don’t drink as much (3 drinks is my limit).”
Heavy drinker: “I don’t know what the impact of alcohol and meds is supposed to be but last weekend I had six martinis and it didn’t affect me at all.”
Patient beliefs about the appropriateness of drinking alcohol when taking ART were also calibrated according to the amount of alcohol ingested. The above figures, which reflect beliefs about taking ART and drinking in general, change somewhat when we specified a dose, “After you take your HIV meds, is it OK to have 1 drink (3–4 drinks, many drinks and become intoxicated?”). In response, 29% of light drinkers thought it was safe to have 1 drink after taking ART, compared to 50% of the moderate drinkers and 69% of the heavy drinkers. For an increased dose of 3–4 drinks, the proportion of patients who thought it was okay dropped for every category of drinker: 17% for light drinkers, 35% for moderate drinkers, and 55% for heavy drinkers. Few patients (9%) thought that becoming intoxicated after taking their ART was okay. This dose-response relationship appears to support the existence of an underlying model of the toxicity of alcohol that increases with the amount consumed.
Alcohol Beliefs and Adherence Practice
Slightly more than one-half (51%) of the patients agreed with the statement, “I will not take my meds if I have been drinking”. Again, this sentiment varied according to an individual’s drinking profile: 64% of light drinkers said they would not take their pills if drinking, versus 55% of moderate drinkers and 29% of heavy drinkers. Individuals who said that having one drink is not okay were much more likely to say that they would not take their medications if drinking than those who thought having one drink is fine, χ 2(63, 1) = 7.0, P < 0.01. An even stronger relationship holds for beliefs about the appropriateness of having 3–4 drinks and whether medications would be taken if drinking, χ 2(56, 1) = 12.2, P < 0.01. A significant minority of those who thought having 1 drink or 3–4 drinks (35% and 21% respectively) is okay said nonetheless they would not take their medications if they had been drinking. It is possible that for these individuals drinking is conceptualized as considerably more than 3–4 drinks. When we asked about delayed or skipped medication doses when drinking, the responses again varied by drinking category with 55% and 50% of the light and moderate drinkers respectively saying they would skip or delay their ART dose if drinking, compared to only 37% of heavy drinkers. Thus, beliefs that it is inappropriate to drink and take ART are associated with patient reports of skipping medications when drinking. Individuals who drink more are more likely to take their ART medication when drinking, while those who drink less, when they do drink, are less likely to be adherent.
Moderate drinker: “I just said I’ll take this one now, and then later I won’t take the other pills if I’m going to drink.”
Moderate drinker: “If I know I’m drinking alcohol, I won’t take my meds that day.”
Moderate drinker: “I don’t take my medications if I’m going to consume alcohol. Taking those two things together and not knowing what kind of interaction they’re going to have on each other is not a good thing.”
Heavy drinker: “You might as well not even take the medication. You know that you’re not supposed to take different drugs or alcohol with your medicine. I wouldn’t go to the club knowing that I have to take my meds at 12 and start drinking at 12; the medicine’s not going to work.”
Heavy drinker: “It’s something that should be avoided, but you don’t not take your medicine because you had a drink.”
Heavy drinker: “My doctor knows I drink, but the alcohol didn’t affect my medication, as long as I take my pills twice a day.”
Age, Alcohol Consumption, and Adherence Beliefs
Age was the only demographic factor that discriminated drinking behavior as well as beliefs about alcohol and taking ART. Forty-one percent of people age 50 and older were considered heavy drinkers compared to fifteen percent of those younger than 50, χ 2(82, 2) = 10.8, P < 0.01. Older people were more likely than younger people to regard 1 drink and 3–4 drinks after taking ART as okay (χ 2(67, 1) = 6.2, P < 0.01 and χ 2(60, 1) = 4.9, P < 0.05 respectively). However, both age groups were equally likely to agree that “ART and alcohol do not mix” and “I will not take my meds if I have been drinking”, and their reported adherence scores were not significantly different. Although it did not reach the level of significance (P = 0.07), more people fifty and older reported they would take their medications even if drunk compared to the younger people.
Models of Alcohol and ART Interaction
An analysis of the question, “What do you think about drinking alcohol and taking ART?” revealed four explanatory models of the alcohol/ART interaction: (a) Alcohol can reduce the effectiveness of ART; (b) Alcohol is toxic and should never be mixed with medication; (c) Alcohol can worsen HIV by impairing the immune system; and (d) Alcohol has no impact on HIV or ART.
(1) Thirty-eight percent depicted alcohol as “breaking down” ART rendering it ineffective.
Light drinker: “Alcohol kinda breaks down things and it may break down the meds in the wrong way. I feel like it’s like throwing gasoline on the fire. It’s just from seeing people, how alcohol eats up your liver. I feel it could really cause a problem with your meds not working the way they properly should.”
Light drinker” “According to what I’m told, it weighs against the medications. It kills the medicine in your bloodstream.”
Light drinker: “Drinking alcohol and taking that medication would be like killing the medication that you’re taking. Or it’s like an overdose because you have two different drugs in your system.”
Moderate drinker: “It’s not good. It dilutes the medicine and the medicine doesn’t work. Leave the drink alone if you want to live.”
Heavy drinker: “I don’t drink right after I take my pills, because I figure it’ll kill it. That’s playing with fire.”
(2) Twenty-eight percent articulated a model in which alcohol is considered toxic.
Light drinker” “God forbid it. I’ll probably get sick because alcohol makes medication think there’s more in your system than what’s really there. That’s how a lot of people OD, it thins the bloodline.”
Moderate drinker: “Drinking and drugging and taking your HIV meds is ludicrous, ‘cause HIV meds are toxic. Drugs and alcohol are more toxic. You putting all this stuff in your system at the same time, and your body can’t discern what to get rid of and what to keep.”
Heavy drinker: “Probably nothing, but it can cause problems over time. The medication makes your liver weak and if you drink that’s double jeopardy.”
Heavy drinker: “If you don’t have alcohol in your system, the medication would be more effective. The higher the alcohol content is in your system at the time of taking the medication, the more adverse effect the medication could have on your system.”
(3) A minority (2%) believed that mixing alcohol and ART would make their HIV disease worse.
Moderate drinker: “It’s not OK to do that. You shouldn’t drink when you’re sick, you’ll make it worse.”
Light drinker: “Your body being broke down, so I think that drinking kind of, you know, just kind of breaks down the body a little bit more.”
(4) Fifteen percent believed that drinking alcohol and taking ART would produce no adverse effects.
Heavy drinker: “Doesn’t bother me at all. I think it has a lot to do with what people believe or have heard.”
Heavy drinker: “It doesn’t have a bad effect on me. But I’m not going to act crazy and drink a whole fifth and then take my pills.”
Heavy drinker: “I think it’s OK because it doesn’t say anything about not drinking with that. It did with Sustiva, but not with Trizivir.”
Information about Alcohol and ART Interaction
We next investigated patient communication with their health care providers as a possible source of patient information, and to obtain further data regarding patient attitudes about drinking and taking ART.
Patient–Physician Communication
We first sought to establish if patients had ever discussed the subject of drinking and taking their medications with their physicians, and in those cases where reported discussions had occurred, we obtained patient accounts of these interactions. Seventy-one percent of patients agreed with the statement, “there’s no point in talking to my doctor about alcohol and ART, because I already know that s/he will tell me that I shouldn’t.” There were no differences among the three drinking groups in this regard with about half in each group having discussed alcohol and ART with their physicians.
The patients who did talk with their physician reported a wide range of advice. According to patient accounts, 5% were told not to start ART if still drinking, 47% were told that drinking would make ART ineffective and increase its side effects, 40% were told it was okay in moderation, and 8% didn’t remember what the physician said. Perhaps unsurprisingly, heavy drinkers (78%) were more likely to report that their physicians indicated to them that drinking and taking their medications is not problematic compared to light and moderate drinkers (24% and 35% respectively), χ 2(39, 2) = 6.5, P < 0.05.
Moderate drinker: “Even though he said go ahead and take it (take your medication after drinking alcohol), I didn’t feel right, you know, drinking and then taking the pills. It was a fear of my own, and so I didn’t- there was no point in really telling them because they already told me what to do and what not to do, you know. So, I just didn’t tell him.”
Heavy drinker: “Oh I knew alcohol and medication don’t go together. And so the doctor he didn’t really have to discuss that too much with me.”
Physician Communication with Patients about Drinking, and Their Attitudes about Alcohol and ART
Patient reports of clinician advice are only one-half of the story. What are physician beliefs about drinking and taking ART, and what are they telling their patients?
Clinician/Patient Communication
To assess clinician instructions to patients regarding drinking and taking medications, we first established whether clinicians ever discussed alcohol consumption with their patients. Twenty-five percent of physicians said they regularly discussed alcohol with their patients, one-half reported they sometimes had this discussion, and 25% indicated they rarely mentioned the topic. Clinicians reported a range of advice regarding drinking and taking ART.
Infectious Disease Fellow: “I address altogether smoking, drugs and alcohol. My advice is to quit.”
Attending Physician: “I tell them that they can have their beer or their daily wine, but not to drink excessively.”
Pharmacist: “To be frank, that’s not an issue that I’ve brought up enough.”
Physician Attitudes Concerning Drinking Alcohol while Taking ART
To gain more insight into the type of advice clinicians dispensed, we elicited their attitudes concerning drinking alcohol along with ART. Of the physicians who talked with their patients about alcohol use, 20% said there was no physiological reason that patients could not drink and take ART and advised their patients that it is permissible to drink alcohol in moderation while taking ART. Twenty-seven percent asserted that drinking and taking ART generates harmful physiological interactions. Over one-half (53%) cautioned their patients that irresponsible drinking could lead to missing doses of ART and thus compromising its effectiveness.
Attending Physician: “Physiologically, I don’t think that alcohol really will have a great effect on blood levels or response to the medicines although there may be some small effects.”
Infectious Disease Fellow 1: “I think drinking alcohol increases the risk of non-adherence to therapy through drunkenness.”
Infectious Disease Fellow 2: “A couple problems with drinking are the possibility of missed doses of chronic alcohol consumers and the second problem is the drug interaction with alcohol.”
Infectious disease fellows, along with nurses and pharmacists, tended to hold the most restrictive attitudes about mixing alcohol and ART, and were more likely than attending physicians to believe that alcohol and ART interact physiologically, χ 2(17, 2) = 5.9, P < 0.05. Attending physicians were also the least likely to tell their patients not to drink, χ 2(17, 1) = 3.8, P < 0.05.
Discussion
If alcohol consumption is indeed related to poor disease prognosis, the nature of this relationship is not well understood. Some researchers have suggested that reduced adherence to ART rather than the effects of alcohol per se may account for the disease progression (Conigliaro et al., 2003; Murphy et al., 2004; Samet et al., 2003). Findings from the study reported here support this view and we propose that the link between alcohol consumption and lower adherence may derive from purposive decision making based on beliefs about the appropriateness of drinking and taking ART, not alcohol induced forgetfulness. We found that patients who held beliefs that alcohol and ART medication do not mix often delayed or skipped their ART doses if they had been drinking or were planning on consuming alcohol. This adherence practice is based on rational decision making informed by cultural models of the interaction of alcohol and medication. These findings are similar to a pattern identified earlier (Altice et al., 2001), linking beliefs about toxic interactions between street drugs and ART that led people in that study to skip or delay their medications if planning to get high.
The association of alcohol beliefs and practices with age is a somewhat unexpected finding. Although several studies have associated older age with increased adherence (e.g., Hinkin et al., 2004), we did not expect to find alcohol beliefs as well as consumption rates distributed on the basis of age rather than, for example, education or gender. Two possible factors may help explain these findings. First, older people have had more practice in drinking alcohol along with taking medication and can draw on personal experience in assessing the risks. It is possible that their more extensive experience reassured them that they could safely drink and remember to take their medication. Second, more people under fifty reported the use of street drugs—45% of those under 50 acknowledged using street drugs at least 10 times in the last 3 months compared to 17% of those 50 and over. Younger people may be associating street drug interactions with ART rather than alcohol, because this is their primary experience.
Clinicians also reported a range of beliefs about alcohol consumption and taking anti-retroviral medications, and they communicated a range of advice about drinking to their patients. In this way clinicians may have influenced patient beliefs about drinking and taking their medications, and therefore may have indirectly and inadvertently contributed to patient episodes of non-adherence. However, in many cases patients do not communicate with their physicians about drinking because they assume that their physicians will tell them not to mix alcohol and ART. Patients may retain their beliefs about the deleterious effects of drinking and taking ART even after their physician instructs them to the contrary.
The study reported here is limited by the measure used to determine alcohol consumption. We suspect patient under-reporting of alcohol use. The instrument utilized, the GAIN Screener (1999), was not designed to address alcohol consumption directly but rather was designed as a general risk assessment. However, with a few exceptions, people’s reporting of their alcohol consumption was consistent from one interview to the next, and the alcohol consumption groups we formed meaningfully distinguished beliefs about drinking and taking ART, and adherence practices. Thus, the GAIN captured the relative distribution of drinking behavior over an 18 month period, contributing to our understanding of the relationships between drinking behavior, beliefs about alcohol consumption while taking ART, and adherence practices.
Another limitation to the study findings is that they apply only to African Americans. Research on African American drinking patterns (Herd, 1985) has identified a long history of temperance and rejection of alcohol. This rejection, however, was historically associated with definitions of moral adult behavior and not the pharmaco-kinetic models that underlie the beliefs identified by people in this study. We can not say if the models articulated here are held by non-African Americans.
A third limitation is that we were unable to link individual clinician–patient communications to patient understandings about drinking and taking ART, and therefore we are unable to ascertain the influence of clinician beliefs and communication about mixing alcohol and ART on patient beliefs.
The findings from this study suggest an approach to enhancing adherence somewhat different from those who urge more surveillance of alcohol use as a means of improving adherence (e.g., Conigliaro et al., 2003; Petry, 1999). Although the public health goal of reducing alcohol consumption is clearly an important one, it should perhaps be pursued in a setting outside the clinician/patient encounter focused on ART adherence. Given that the National Institutes of Health website on AIDS treatment guidelines recommends that only patients with both HIV and Hepatitis B be advised to avoid or limit their alcohol intake, and given the tenacious belief among patients about the toxic interaction of alcohol and medication, warnings about drinking alcohol are likely to have the effect demonstrated here of causing people to unnecessarily skip or delay their medication if drinking rather than forgo drinking itself. Instead, effective interventions to promote adherence among those who consume alcohol should directly confront these beliefs and the underlying models that support them with discussions that address the safety of consuming alcohol while on ART. In doing so, however, the validity of patient beliefs concerning “toxic” interactions between alcohol and some medication needs to be confirmed while explaining that this is not the case for ART. Failure to acknowledge the partial validity of these beliefs can lead to patients rejecting the advice, as was illustrated here.
A second implication of the findings presented here stems from the fact that some views clinicians themselves hold concerning the relationship between ART and alcohol must be seen as either a source or a reinforcement of patient beliefs about “toxic” interactions. The personal beliefs of some clinicians may inadvertently serve to support the patient’s model of toxicity and thus to endorse implicitly their practice of delaying or skipping their ART doses when drinking. Thus, clinician training needs to be improved so that their knowledge about consuming alcohol and being on ART conforms to AIDS treatment guidelines, and also so that they communicate appropriately to patients the relationship between drinking and taking anti-retroviral medications. Findings from this study were shared with the attending physicians at each clinic, both of which now integrate discussions of alcohol and ART interactions and adherence into their training programs.
References
Altice, F., Mostashari, F., & Friedland, G. (2001). Trust and the acceptance of and adherence to antiretroviral therapy. JAIDS Journal of Acquired Immune Deficiency Syndromes, 28, 47–58.
Arnsten, J. H., Demas, P. A., Grant, R. W., Fourevitch, M. N., Farzadegan, H., & Howard, A. A., et al. (2002). Impact of active drug use on antiretroviral therapy adherence and viral suppression in HIV-infected drug users. Journal of General Internal Medicine, 17, 377–381.
Bangsberg, D. R., Charlebois, E. D., & Grant, R. (2003). High levels of adherence do not prevent the accumulation of drug resistance mutations to HIV antiretroviral therapy. AIDS, 17, 1925–1932.
Brown, D. (2005). U.S. survey indicates Blacks hardest hit by HIV Infection. Washington Post, February, 26, 3.
Conigliaro, J., Gordon, A. J., McGinnis, K. A., & Rabeneck, L. (2003). How harmful is hazardous alcohol use and abuse in HIV infection: Do health care providers know who is at risk? JAIDS Journal of Acquired Immune Deficiency Syndromes, 33, 521–525.
Cook, R. L., Sereika, S. M., Hunt, S. C., Woodward, W. C., Erlen, J. A., & Conigliaro, J. (2001). Problem drinking and medication adherence among person with HIV infection. Journal of General Internal Medicine, 16, 83–88.
Dennis, M. (1999). Global appraisal of individual needs (GAIN): Administration guide for the GAIN and related measures. [On Line]. Bloomington, IL: Chestnut Health Systems.
Dennis, M. L., Scott, C. K., Godley, M. D., & Funk, R. (2000). Predicting outcomes in adult and adolescent treatment with case mix vs. level of care: Findings from the drug outcome monitoring study. Drug and Alcohol Dependence, 60, s51.
Ferrando, S. J., Wall, T. L., Batki, S. L., & Sorensen, J. L. (1996). Psychiatric morbidity, illicit drug use and adherence to Zidovudine (AZT) among injection drug users with HIV disease. American Journal of Drug and Alcohol Abuse, 22(4), 475–87.
Fong, O. W., Ho, C. F., Fung, L. Y., Lee, F. K., Tse, W. H., & Yuen, C. Y., et al. (2003). Determinants of adherence to highly active antiretroviral therapy (HAART) in Chinese HIV/AIDS patients. HIV Medicine, 4, 133–138.
Halkitis, P. N., Parsons, T. I., Wolitski, R. J., & Remien, R. H. (2003). Characteristics of HIV antiretroviral treatments, access and adherence in an ethnically diverse sample of men who have sex with men. AIDS Care, 15, 89–102.
Herd, D. (1985). Ambiguity in Black drinking norms: An ethnohistorical interpretation. In L. A. Bennet & G. M. Ames, (Eds.), The American experience with alcohol, (pp. 149–170). New York: Plenum Press.
Hinkin, C. H., Hardy, D. J., & Hardy, K. I. (2004). Medication adherence in HIV-infected adults: Effect of patient age, cognitive status, and substance abuse. AIDS, 18, S19–S25.
Hunt, L. M., Arar, N. H., & Larme, A. C. (1998). Contrasting patient and practitioner perspectives in Type 2 diabetes management. Western Journal of Nursing Research, 20, 656–682.
Luborsky, M. (1994). Identifying themes and patterns. In A. Sankar & J. Gubrium, (Eds.), Qualitative methods in aging research, (pp. 189–210). New York: Sage.
Malcolm, S., Ng, J., Rosen, R., & Stone, V. (2003). An examination of HIV/AIDS patients who have excellent adherence to HAART. AIDS Care, 15, 251–261.
Martini, M., Nasta, P., Ricci, E., Parazzini, F., & Agnoletto, V. (2000). Perceptions of disease and therapy are factors influencing adherence to antiretroviral therapy. Sexually Transmitted Infections, 76, 496–497.
McGinnis, K. A., Sharma, M. J., & Skanderson, R. (2003). Understanding racial disparities in HIV using data from the veterans aging Cohort 3-Site Study and VA administrative data. American Journal of Public Health, 93, 1728–1733.
Murphy, D. A., Marelich, W. D., Hoffman, D., & Steers, W. N. (2004). Predictors of antiretroviral adherence. AIDS Care, 16, 471–484.
Paterson, D. L., Swindells, S., & Mohr, J. (2000). Adherence to protease inhibitor therapy outcomes in patients with HIV infection. Annals of Internal Medicine, 133, 21–30.
Petry, N. (1999). Alcohol use in HIV patients: What we don’t know may hurt us. International Journal of STD & AIDS, 10, 561–570.
Reynolds, N. R. (2004). Adherence to antiretroviral therapies: State of the science. Current HIV Research, 2, 207–214.
Samet, J. H., Horton, N. J., Traphagen, E. T., Lyon, S. M., & Freedberg, K. A. (2003). Alcohol consumption and HIV disease progression: Are they related? Alcoholism: Clinical and Experimental Research, 27, 862–867.
Smith, M. Y., Rapkin, B. D., Morrison, A., & Kammerman, S. (1997). Zidovudine adherence in persons with AIDS: The relation of patient beliefs about medication to self-termination of therapy. Journal of General Internal Medicine, 12, 216–223.
Spire, B., Duran, S., & Souville, M. (2002). Adherence to highly active antiretroviral therapies (HAART) in HIV-infected patients: From a predictive to a dynamic approach. Social Science & Medicine, 54, 1481–1496.
Weidle, P. J., Ganea, C. E., & Irwin, K. L. (1999). Adherence to antiretroviral medications in an inner-city population. JAIDS Journal of Acquired Immune Deficiency Syndromes, 22, 498–502.
Acknowledgment
We gratefully acknowledge the support of the National Institute of Allergy and Infectious Diseases (NIAID: R01 # AI49113) for this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sankar, A., Wunderlich, T., Neufeld, S. et al. Sero-positive African Americans’ Beliefs about Alcohol and Their Impact on Anti-retroviral Adherence . AIDS Behav 11, 195–203 (2007). https://doi.org/10.1007/s10461-006-9144-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-006-9144-0