Abstract
Effect of thermal water with high mineral content on clinical parameters and quality of life of patients with chronic low back pain was studied. In this randomized controlled, single-blind, follow-up study, 60 patients with chronic low back pain were randomized into two groups. The treatment group received balneotherapy with thermal-mineral water, and the control group bathed in tap water. Changes of the followings were evaluated: visual analogue scale (VAS) for pain, range of motion for the lumbar spine, Oswestry index, EuroQol-5D and Short Form-36 questionnaires. In the treatment group, the mobility of the lumbar spine, the Oswestry index, the VAS scores and the EuroQoL-5D index improved significantly. SF-36 items improved significantly in the treated group compared with baseline except for two parameters. Our study demonstrated the beneficial effect of balneotherapy with thermal mineral versus tap water on clinical parameters, along with improvements in quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Balneology, studying the effects of thermal-mineral water, is a branch of medical science. Balneotherapy or spa therapy—a treatment modality cultivated predominantly in countries with abundant thermal and mineral springs—uses thermal-mineral water for therapeutic purposes. By definition, mineral water contains mineral solutes—cations (such as sodium, potassium, calcium and magnesium) and anions (e.g. sulphate, chloride and bicarbonate) in a concentration of 1 g/L at least [2]. The physical properties of water exerting mechanical and thermal effects combined with the absorption of mineral solutes and with anti-inflammatory effects might have a role in the mechanism of action of mineral water [8], but the latter has not been fully proven yet. Hydrotherapy, a treatment based on the physical properties of water, is being used in almost every country of the world, primarily for the management and rehabilitation of patients with musculoskeletal disorders. In this case, mineral water is not necessary, as hydrotherapy can be implemented using tap water.
Additional branches of balneotherapy include mud therapy and oral administration of mineral water, as well as the therapeutic use of naturally occurring gases [11]. In recent years, evidence-based reports have been published in increasing numbers on the beneficial effect of balneotherapy, primarily in musculoskeletal disorders including rheumatoid arthritis [20], osteoarthritis [9] and fibromyalgia [24]. Additionally, meta-analyses are also available in this field [12]. Moreover, ‘silver level’ evidence has been obtained for the effectiveness of balneotherapy in osteoarthritis [23].
Chronic low back pain is among the most prevalent musculoskeletal abnormalities. During a lifetime, almost 80% of the population is afflicted by low back pain, which resolves over 2–4 weeks in 90%, but recurs within a year in 60–80%. Low back pain is considered ‘chronic’ when it persists longer than 7–12 weeks [13, 22]. Most of the information on the non-pharmacological management of chronic low back pain has been accumulated about exercise therapy. These data show the beneficial effect of this intervention [21]; however, fail to detect any difference between the different modalities of exercise therapy. More recent data are available on the positive effect of alternative remedies including acupuncture and—at a lower level of evidence—manual therapy [18]. Papers published on the effect of thermal-mineral water in chronic low back pain are relatively scarce: the single meta-analysis available so far in English evaluated only five studies [17]. In the meantime, however, additional studies have been published on this subject [1, 15]. In contrast to the majority of earlier projects evaluating spa therapy, our study compared the effects of thermal-mineral water not with medicinal products or other treatment modalities, but with that of tap water. By doing so, we intended to demonstrate the superior therapeutic efficacy of mineral water in comparison with the purely physical effects of tap water.
The primary objective of our research was to ascertain whether the beneficial effect of high-mineral-content thermal water from Mátraderecske spa could be demonstrated in comparison with tap water used as reference. Our secondary aim was to evaluate whether the positive change of clinical condition would translate into a better quality of life and reduced analgesic and NSAID requirements versus baseline, as well as to assess the magnitude of these improvements in comparison with the control group treated with tap water.
Patients and methods
The study was conducted with mineral water from the thermal spring of Mátraderecske, a small village in Northern Hungary. The natural resources of this area also include the only mofetta (volcanic gas eruption) of the country, which is being utilized for therapy with dry carbon dioxide.
The study was implemented between May and November 2010.
Protocol and study parameters
Sixty patients were randomized—according to a computerized randomization list generated by an independent operator—in equal proportions to treatment with thermal-mineral water (n = 30, mean age: 63.57 ± 8.6 years) or tap water (controls, n = 30, mean age: 64.33 ± 6.6 years). Sex distribution of the study population was 14 males and 46 females. Following randomization, a professional not involved in the study enrolled the patients followed-up at the regional rheumatology outpatient clinic into either of the two groups. The condition of study subjects was appraised before and after the balneotherapy course, as well as during follow-up by a single independent investigator unfamiliar with the treatment received by the examined patients. The physician supervising the treatment was available during balneotherapy sessions, as well as recorded blood pressure, heart rate and potential adverse reactions twice a week.
Fifteen 30-min-long balneotherapy sessions were administered over 3 weeks, 5 days a week, using either thermal-mineral (treatment group) or tap water (control group) of 31°C temperature. In both pool—each one with 1 meter of depth—the participants had the possibility either to sit on seats or to move in a half-sitting or squatting position or to swim, which meant that the patients did not experience cold. Patients knew which type of water they were using, as it was unfeasible to imitate the properties of thermal-mineral water. Appraisal was performed before the first and after the 15th balneotherapy session (on Week 3), as well as 3 and 10 weeks after the end of the balneotherapy course. On these occasions, a detailed history was obtained, fulfilment of inclusion/exclusion criteria was checked, and potential adverse events were recorded along with the visual analogue scale (VAS) scores (mm) of lumbar pain at rest and on exertion. Physical examination was performed, including Schober’s test for mobility of the lumbar spine (in cm), as well as of the range of lateral flexion of the lumbar spine in both directions [7]. Additionally, the subjects completed the disease-specific Oswestry Disability Questionnaire, as well as the EuroQol-5D and SF-36 questionnaires pertinent to quality of life. Daily and weekly consumption of analgesics and NSAIDS taken to relieve chronic lumbar pain was recorded 1 month before as well as during the study and the follow-up period. The subjects received written information and consented to participation in writing before inclusion. The protocol of the study was approved by the competent regional ethics committee (decision N° 101-É-2010/124–128).
Inclusion criteria
Patients with the following conditions were enrolled to the study: ambulatory patients from the catchment area, with chronic low back pain not complicated by severely restricted mobility; men and women aged 40–79 years; non-specific low back pain pre-existing since 12 weeks or longer, with evident tenderness of paravertebral muscles and painful limitation of motion of the lumbar spine; behind the chronic low back pain suspected, segmental limitation of motion, segmental instability or other underlying cause associated with radiologically confirmed or not confirmed spondylosis, discopathy, or spondylarthritis; severity of low back pain on exertion, expressed as a VAS score of 35 mm or greater (on a 100-mm visual analogue scale); and lack of systemic or topical treatment with steroids, physical or balneotherapy within 2 months of inclusion, but exercise therapy was allowed.
Exclusion criteria
Patients with the following conditions were excluded from the study: acute low back pain, organic neurological deficit associated with lumbar pain, suspected vertebral compression of osteoporotic or other aetiology, underlying malignancy, pain resulting from inflammatory spine disease, spondylolisthesis (Grade 2 or higher), history of spine surgery and contraindications to balneotherapy (unstable angina pectoris, poorly controlled hypertension, cardiac decompensation, respiratory insufficiency, endocrine disorder, acute febrile condition, skin infections, other severe genitourinary or other disease, faecal or urinary incontinence, decompensated psychosis or neurosis, and lack of compliance).
Composition of the thermal water
The thermal water used in this study was of extremely high mineral content, characterized by the dominance of sodium hydrogen carbonate and chloride, lithium, bromide, also containing abundant quantities of iodine, fluoride and metaboric acid (Table 1).
Statistical methods
Data were analysed with MS Excel software. Statistical comparisons were made using single-sample (paired) and two-sample t tests. An intention-to-treat (ITT) analysis was performed.
Results
At baseline, there were no substantial differences between the two patient groups as regards their demographical and study parameters.
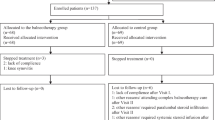
Following randomization, three subjects declined treatment before the start of the balneotherapy. Therefore, the treatment group (using thermal-mineral water) comprised 30, whereas the control group (using tap water) consisted of 27 patients.
The number of patients lost to follow-up was 13 in the treatment and 7 in the control group. In the treatment group, two patients were excluded at Visit 2: one owing to the lack of compliance and another because of abdominal surgery; at Visit 3, additional six patients were withdrawn owing to the lack of compliance; and finally, three patients were excluded at Visit 4 for upper airway infection and additional two for lack of compliance. In the control group, one patient was excluded for the lack of compliance at Visit 2 and additional three at Visit 3, whereas one patient was withdrawn for upper airway infection and further two for lack of compliance at Visit 4. Fourteen excluded patients submitted completed questionnaires: nine in the treatment group (one at Visit 2, five at Visit 3 and three at Visit 4) and five in the control group (one at Visit 2, three at Visit 3 and one at Visit 4). These were processed, and data from every study subject were used for the intention-to-treat analysis (Fig. 1).
By the end of the balneotherapy course, the VAS score of low back pain at rest and on exertion, mobility of the lumbar spine (reflected by lumbar Schober’s sign and lateral flexion in both directions) and disease-specific assessment (using the Oswestry questionnaire) improved significantly in the treatment group, compared to baseline. These improvements persisted until the end of follow-up (as ascertained 3 and 10 weeks after the end of balneotherapy). By contrast, no significant changes occurred in the control group. Between-group differences in the above parameters were significant both at the end of balneotherapy and during follow-up.
In the treatment group, improvement of the quality of life measured by EuroQol-5D index compared to baseline was significant at the end of balneotherapy and for three subsequent weeks of follow-up. Reverse trends were observed for control subjects. The difference between the values measured in the two groups was significant at the end of balneotherapy and throughout the follow-up period (both at 3 and 10 weeks after the end of the balneotherapy course).
The VAS score indicating overall health condition improved significantly in the treatment group by the end of balneotherapy, and this improvement remained significant in comparison with baseline until the end of follow-up. In the control group, significant deterioration was observed. The difference between the two groups was significant both at the end of balneotherapy and during follow-up.
By the end of the balneotherapy course, all components of the SF-36 questionnaire assessing health-related quality of life showed a tendency for improvement in the treatment group and—except for the components indicative of general health and social functioning—this improvement was significant in comparison with baseline. A reverse tendency, which was significant also for these two SF-36 components, was observed in the control group. The difference between the two groups was significant for every component at the end of balneotherapy. This difference remained significant for the majority of components until the end of follow-up (the exceptions were the SF-36 component pertaining to vitality at 3 weeks, as well as the components measuring physical role and social functioning at 10 weeks of follow-up).
In the treatment group, the consumption of analgesics and NSAIDs necessary to relieve chronic low back pain decreased significantly by the end of balneotherapy, and this reduction remained significant (compared to baseline) until the end of follow-up. No significant change could be observed in the control group. The difference between the two groups was not significant at any time point (Table 2).
Discussion
According to the literature, the effect of thermal-mineral water is superior to that of tap water, both in inflammatory and in non-inflammatory rheumatologic disorders. The meta-analysis by Harzy et al. [12] confirmed the effectiveness of thermal-mineral water in relieving pain and improving function. As shown by controlled studies conducted with tap water in chronic low back pain, the relief of pain [1], improvement of mobility [1, 15], and mitigation of the tenderness and spasm of paravertebral muscles [1], along with changes in the rating by patients and investigators [15], were more pronounced among patients bathing in thermal-mineral water, than in those using tap water. As regards previous controlled studies into the effect of balneotherapy on chronic low back pain, Guillemin et al. [10] prescribed a 3-week balneotherapy course (underwater jet massage for 15 min in 36°C water, followed by showering for 3 min with water of 31–36°C temperature), and the results were compared with those obtained in outpatients. Taking medicinal products prescribed, as necessary, by the family practitioner was allowed, but any means of physical therapy were prohibited. Evaluations were performed at baseline, on day 26 and 9 months after therapy. Compared to the control group, a number of parameters (such as the VAS score of pain, mobility of the lumbar spine and analgesic consumption) improved immediately after therapy, and this improvement was maintained 9 months later (except for the Waddell Disability Score). In another French study [5], 121 patients with low back pain were assigned to two groups, subjected to either complex spa therapy (balneotherapy for 10 min, mud packs of 45°C temperature for 20 min and high-pressure showering for 2.5 min) or pharmacotherapy only. Study parameters were Schober’s sign, finger-to-floor distance, pain, patients’ rating, the Roland & Morris Disability score, analgesic and NSAID requirements. Except for analgesic consumption and Schober’s sign, the studied measures improved immediately after spa therapy in the treatment group and this improvement remained significant also 6 months later (except for Schober’s sign and NSAID requirements), confirming the prolonged effect of balneotherapy. Hungarian authors reported their results obtained with three balneotherapy modalities—such as thermal-mineral water, underwater jet massage and weight bath—compared to no therapy in patients with low back pain. All three treatment groups improved, and 1 year later, their analgesic consumption was lower than in the control group [14]. The beneficial effect of hydro- and balneotherapy on quality of life—that is, greater improvement on balneotherapy, than on hydrotherapy—has been described already in chronic low back pain [6, 15], fibromyalgia [16], osteoarthritis of the knee [19] and ankylosing spondylitis [4]. The positive clinical effect of saline baths has been reported in dermatological disorders, primarily [3]. In dermatology, balneo-phototherapy with salt water is among the most frequently used treatment modalities of psoriasis [3]. As regards the management of musculoskeletal disease, literature data are available on osteoarthritis, primarily [19]. The anti-inflammatory effect of saline bath is widely known.
Although balneotherapy is a popular treatment modality, the need for increasing the number of evidence on its effectiveness is justified. Treatment with thermal-mineral water, both as an adjunct to pharmacotherapy or as an independent therapeutic measure, may prove a major symptomatic remedy, especially in chronic musculoskeletal disorders. Single-blind design is one of the limitations of the study; however, it was not possible to imitate the properties of thermal-mineral water in order to produce a suitable placebo. Moreover, controlling for the influence of additional therapeutic interventions not prescribed by the study protocol is still questionable.
Conclusion
As its primary objective, our study demonstrated—in comparison with treatment with tap water—the beneficial effect of balneotherapy on clinical parameters in chronic low back pain. Additionally, it had a clearly positive impact on the patients’ quality of life, as well as on their analgesic and NSAID requirements. In view of these results, we can conclude that high-mineral-content thermal water may prove an important therapeutic tool for the management of chronic low back pain.
References
Balogh Z, Ördögh J, Gász A, Német L, Bender T (2005) Effectiveness of balneotherapy in chronic low back pain—a randomized single-blind controlled follow-up study. Forsch Komplementarmed Klass Naturheilkd 12:196–201
Bender T, Karagülle Z, Bálint G, Gutenbrunner C, Bálint P, Sukenik S (2005) Hydrotherapy, balneotherapy, and spa treatment in pain management. Rheumatol Int 25:220–224
Brockow T, Schiener R, Franke A, Resch KL, Peter RU (2007) A pragmatic randomized controlled trial on the effectiveness of low concentrated saline spa water baths followed by ultraviolet B (UVB) compared to UVB only in moderate to severe psoriasis. J Eur Acad Dermatol Venereol 21:1027–1037
Codish S, Dobrovinsky S, Abu Shakra M, Flusser D, Sukenik S (2005) Spa therapy for ankylosing spondylitis at the Dead Sea. Isr Med Assoc J 7:443–446
Constant F, Collin JF, Guillemin F, Boulangé M (1995) Effectiveness of spa therapy in chronic low back pain: a randomised cinical trial. J Rheumatol 22:1315–1320
Constant F, Guillemin F, Clooin JF, Boulange M (1998) Spa therapy appears to improve the quality of life of sufferers from chronic low back pain. Med Care 36:1309–1314
Domján L, Nemes T, Bálint GP, Tóth Z, Gömör B (1990) A simple method for measuring lateral flexion of the dorsolumbar spine. J Rheumatol 17:663–665
Fioravanti A, Cantarini L, Guidelli GM, Galeazzi M (2010) Mechanisms of action of spa therapies in rheumatic diseases: what scientific evidence is there? Rheumatol Int. [Epub ahead of print]
Forestier R, Desfour H, Tessier JM, Françon A, Foote AM, Genty C et al (2010) Spa therapy in the treatment of knee osteoarthritis: a large randomised multicentre trial. Ann Rheum Dis 69:660–665
Guillemin F, Constant F, Collin JF, Boulange M (1994) Short and long-term effect of spa therapy in chronic low back pain. Br J Rheumatol 33:148–151
Gutenbrunner C, Bender T, Cantista P, Karagülle Z (2010) A proposal for a worldwide definition of health resort medicine, balneology, medical hydrology and climatology. Int J Biometeorol 54:495–507
Harzy T, Ghani N, Akasbi N, Bono W, Nejjari C (2009) Short- and long-term therapeutic effects of thermal mineral waters in knee osteoarthritis: a systematic review of randomized controlled trials. Clin Rheumatol 28:501–507
Koes BW, Van Tulder MW, Thomas S (2006) Diagnosis and treatment of low back pain. BMJ 332:1430–1434
Konrad K, Tatrai T, Hunka A, Vereckei E, Korondi I (1992) Controlled trial of balneotherapy in treatment of low back pain. Ann Rheum Dis 51:820–822
Kulisch A, Bender T, Németh A, Szekeres I (2009) Effect of thermal water and adjunctive electrotherapy on chronic low back pain: a double-blind, randomized, follow-up study. J Rehabil Med 41:73–79
Langhorst J, Musical F, Klose P, Häuser W (2009) Efficacy of hydrotherapy in fibromyalgia syndrome—a meta-analysis of randomized controlled clinical trials. Rheumatology (Oxford) 48:1155–1159
Pittler MH, Karagulle MZ, Karagulle M, Ernst E (2006) Spa therapy and balneotherapy for treating low back pain: meta-analysis of randomized trials. Rheumatology 45:880–884
Rubinstein SM, van Middelkoop M, Kuijpers T, Ostelo R, Verhagen AP, de Boer MR et al (2010) A systematic review on the effectiveness of complementary and alternative medicine for chronic non-specific low-back pain. Eur Spine J 19:1213–1228
Sherman G, Zeller L, Avriel A, Friger M, Harari M, Sukenik S (2009) Intermittent balneotherapy at the Dead Sea area for patients with knee osteoarthritis. Isr Med Assoc J 11:88–93
Sukenik S, Flusser D, Abu-Shakra M (1999) The role of spa therapy in various rheumatic diseases. Rheum Dis Clin North Am 25:883–897
van Middelkoop M, Rubinstein SM, Verhagen AP, Ostelo RW, Koes BW, van Tulder MW (2010) Exercise therapy for chronic nonspecific low-back pain. Best Pract Res Clin Rheumatol 24:193–204
Van Tulder M (2002) Low back pain. Best Pract Res Clin Rheumatol 16:761
Verhagen A, Bierma-Zeinstra S, Lambeck J, Cardoso JR, de Bie R, Boers M et al (2008) Balneotherapy for osteoarthritis. A cochrane review. J Rheumatol 35:1118–1123
Zijlstra TR, van de Laar MA, Bernelot Moens HJ, Taal E, Zakraoui L, Rasker JJ (2005) Spa treatment for primary fibromyalgia syndrome: a combination of thalassotherapy, exercise and patient education improves symptoms and quality of life. Rheumatology (Oxford) 44:539–546
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tefner, I.K., Németh, A., Lászlófi, A. et al. The effect of spa therapy in chronic low back pain: a randomized controlled, single-blind, follow-up study. Rheumatol Int 32, 3163–3169 (2012). https://doi.org/10.1007/s00296-011-2145-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-011-2145-y