Abstract
Purpose
The feasibility and potential advantages of laparoscopic diagnosis and repair of incarcerated obturator hernia (OH) is debated. The aim of this retrospective study was to compare short-term complications comparing laparoscopic to open repair of OH.
Methods
A total of 29 preoperatively diagnosed patients underwent surgery for a preoperatively diagnosed OH between January 2006 and July 2017. The patients were divided into a laparoscopic group (11 patients underwent laparoscopic repair; 8 without and 3 with intestinal resection) and an open group (18 patients who underwent open repair; 9 without and 9 with intestinal resection).The outcomes were compared between groups. A risk factor analysis for postoperative complications was performed.
Results
The incidence of postoperative complications was fewer in the laparoscopic group [9.0% vs. 61.1%; (p < 0.001)]. The bleeding amount [1.2 g vs. 40.4 g; (p = 0.087)] and postoperative length of stay [13.3 days vs. 17.1 days; (p = 0.072)] showed a tendency to be favorable in the laparoscopic group. Occult contralateral OH was detected in three patients (27.7%) in the laparoscopic group and one patient (5.5%) in the open group (p = 0.099). Open surgery and intestinal resection were independent risk factors for a postoperative complication. One patient in the open group developed an incarcerated OH on the contralateral side 1 year after the first surgery.
Conclusions
Laparoscopic repair for incarcerated obturator hernia demonstrated more favorable short-term outcomes compared with open repair in terms of a lower incidence of postoperative complications and it was potentially beneficial for detecting and repairing an occult OH on the contralateral side.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obturator hernia (OH) is a rare cause of intestinal obstruction and most frequently occurs in elderly, thin and multiparous females [1,2,3], which results from the laxity of pelvic tissue and decreased fatty tissue around the obturator foramen [1,2,3]. The incidence of OH has been reported to be 0.05–1.4% of all hernias [1, 2]. The diagnosis is often delayed due to difficulty in its detection [1,2,3], and computed tomography is considered a choice of modality for diagnosis [1, 2, 4]. In addition, patients with delayed diagnosis often fall into a serious condition and require intestinal resection, resulting in a high mortality rate [1,2,3, 5]. Traditionally, incarcerated OH is treated by open surgery, while recent reports suggest the feasibility and effectiveness of laparoscopic repair for incarcerated OH [6,7,8,9,10]. However, the number of patients who underwent laparoscopic repair in these reports was relatively small, and the choice of treatment for incarcerated OH remains controversial. Here, we divided the patients with OH into a laparoscopic group and open group and compared the perioperative outcomes of each procedure.
Materials and methods
Study patients
Between January 2006 and July 2017, a total of 710 patients underwent laparoscopic transabdominal preperitoneal repair (TAPP) for inguinal hernia at Fujinomiya City General Hospital. During the same period, 11 patients underwent laparoscopic TAPP for incarcerated OH, and 18 other patients underwent open repair for incarcerated OH; so, the final study group comprised 29 patients preoperatively diagnosed with incarcerated OH. Patients were grouped, based on whether they underwent hernia repair laparoscopically, into the laparoscopic group (n = 11) and open group (n = 18). All the patients except one underwent emergency operation due to the incarcerated lesion. The other patient underwent elective laparoscopic repair after reduction of incarcerated lesion. The choice of procedure, laparoscopic or open repair, was at the surgeon’s discretion. Therefore, patients with severe conditions or patients with severe intestinal dilation were generally allocated to the open procedure in this retrospective study.
We accessed patient’s records so that we could review and compare clinical variables and the outcomes between these two groups. In addition, we performed subgroup analyses in patients with intestinal resection (three patients in the laparoscopic group versus nine patients in the open group) and without intestinal resection (eight patients in the laparoscopic group vs. nine patients in the open group) to accurately assess the outcomes of each procedure that might be impacted by intestinal resection. The study protocol was approved by the institutional review board of Fujinomiya City General Hospital. Informed consent was waived for this retrospective study.
Surgical procedure of laparoscopic repair
We performed TAPP repair. We used a 10-mm port for the camera (35-degree oblique laparoscope) at the umbilicus incision and two 5-mm ports for performing reduction of the incarcerated intestine and repairing the hernia. After pneumoperitoneum, the patient was set into the Trendelenburg posture. Repair was performed by simple peritoneal closure with or without coverage of foramen obturatum using adjacent tissue (mainly tissue around the uterus or ovary) or by mesh prosthesis. In the patients who required intestinal resection, minilaparotomy was added at the umbilicus incision. Subsequently, the intestine was pulled through and resected. Mesh prosthesis was avoided in patients who underwent intestinal resection due to the risk of infection. In patients with occult inguinal or femoral hernia, we generally repaired these lesions simultaneously using a mesh prosthesis, while in patients who required intestinal resection, occult lesions of the inguinal and femoral hernia were repaired electively at a later date so that we could use a mesh prosthesis.
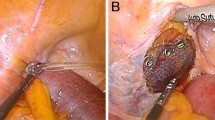
Repairing of OH with mesh prosthesis was performed as follows: after confirming the lesion, reduction was performed by pulling the incarcerated intestine gently (Fig. 1a, b). We cut the peritoneum on the Cooper ligament, and the preperitoneal space around the obturator foramen was dissected (Fig. 2). A prosthetic mesh was then inserted into the dissected space. Tacking the mesh onto the Cooper ligament, the obturator foramen was covered by the mesh, maintaining a 2–3 cm margin (Fig. 3), and the peritoneum was closed with sutures (Fig. 4). In these days, we use absorbable tacker for fixing the mesh. In addition, if an occult OH on the contralateral side was detected, we performed repair to avoid future incarcerations. If coexisting groin hernias were found, standard TAPP repair was performed with dissection of the entire myopectineal orifice of Fruchaud.
Bleeding amount was calculated by totaling the amount which was obtained by measuring the weight of gauze and the suction amount.
Clinical variables assessed
We reviewed the following clinical variables: sex, age, American Society of Anesthesiologists Physical Status (ASA-PS), presence of comorbidities, history of abdominal surgery, internal use of anticoagulant medicine, preoperative white blood cell count, preoperative C-reactive protein value, incarcerated side, and time from onset to surgery. We also reviewed the following perioperative variables: operation time, bleeding amount, postoperative length of stay, whether intestinal resection was performed, whether mesh prosthesis was used, whether repairing of OH on the contralateral side was performed, postoperative complications, mortality and readmission. Complications were classified according to the 2004 grading system of Dindo et al. [11], and complications of grade II or more were considered clinically significant.
Statistical analyses
Study variables are shown as the number and percentage of patients, percentage of cases, or mean values. Between-group differences in nominal variables were analyzed by Pearson’s Chi square test, and differences in continuous variables were analyzed by the Mann–Whitney U test. Multivariable logistic regression analysis was performed to determine independent predictors of outcomes. All statistical analyses were performed with the Statistical Package for the Social Sciences, version 11.5J for Windows 1 (SPSS, Chicago, IL, USA). A p value of < 0.05 was considered significant.
Results
Patient characteristics (Table 1)
The 29 patients included 1 (3.4%) man and 28 (96.6%) women who ranged in age from 64 to 95 years (mean, 84.9 years). One patient was classified as ASA-PS class 1 (3.4%), while 24 patients (82.7%) were classified as class 2 and the other 4 patients were class 3 (13.7%). Regarding comorbidities, one patient had renal failure, four patient had chronic obstructive pulmonary disease and five patients had coronary heart disease or chronic heart failure. Two out of 29 patients (6.8%) had previous history of OH repaired by surgery. Four patients in the laparoscopic group (36.3%) and five patients in the open group (27.7%) had previous history of abdominal surgery. Four patients in the laparoscopic group (36.3%) and three patients in the open group (16.6%) had taken anticoagulant medicine preoperatively. The time from onset to surgery averaged 2.2 days in both groups.
Perioperative outcomes (Table 2)
In all 11 cases with laparoscopic repair, conversion to laparotomy was not required. Operation time was not significantly different between groups (77.0 min in the laparoscopic group and 85.2 min in the open group). Bleeding amount (1.2 g in the laparoscopic group and 40.4 g in the open group (p = 0.087)) and postoperative length of stay (13.3 days in the laparoscopic group and 17.1 days in the open group (p = 0.072)) were more favorable in the laparoscopic group, though they were not statistically significant. Three patients in the laparoscopic group (27.2%) and nine patients (50%) in the open group required intestinal resection. Mesh prosthesis was used in three patients (27.7%) in the laparoscopic and three patients (16.6%) in the open group. Occult OH on the contralateral side was detected intraoperatively and repaired in three patients in the laparoscopic group (27.7%) and in one patient in the open group (5.5%) (p = 0.099).
Incidence of postoperative complications (9.0 versus 61.1%) was significantly lower in the laparoscopic group (p < 0.001). Postoperative complications in the open group included paralytic ileus (n = 4, three of four were Clavien–Dindo classification Grade II and the other was Grade IIIa), respiratory failure (n = 2, both of two were Grade IVa), circulatory failure (n = 1, Grade II), hematoma (n = 1, Grade IIIa), wound infection (n = 1, Grade II), persistent inflammatory reaction (n = 1, Grade II), and neurogenic bladder dysfunction (n = 1, Grade II), while the only one in the laparoscopic group was arrhythmia (n = 1, Grade II). Readmission related to the surgery was necessary for one patient in the open group, and the reason was recurrence of OH on the contralateral side. The recurrence occurred 1 year after the first operation.
Comparing the patients with intestinal resection (Table 3)
Among patients who underwent intestinal resection, patient age was significantly higher in the laparoscopic group (p = 0.012). Incidence of postoperative complications (0 versus 100%) was significantly more favorable in the laparoscopic group (p < 0.001).
Comparison of the patients without intestinal resection (Table 4)
Among patients who did not undergo intestinal resection, bleeding amount (p = 0.020) and postoperative length of stay (p = 0.030) were significantly more favorable in the laparoscopic group.
Factors associated with developing postoperative complications (Table 5)
Open surgery (p = 0.027, odds ratio = 24.25) and intestinal resection (p = 0.013, odds ratio = 20.69) were found by logistic regression analysis to be independent risk factors for developing postoperative complications.
Discussion
The feasibility of laparoscopic repair for OH has been reported recently, though the superiority of laparoscopic repair compared with open repair has not been established yet [6,7,8,9,10]. Ng et al. demonstrated shorter postoperative length of stay, fewer complications, and lesser mortality in patients who underwent laparoscopic repair, though in their study only one patient underwent laparoscopic repair with intestinal resection [6]. Hayama et al. suggested the feasibility of laparoscopic repair, while the operation time and postoperative length of stay were longer in the laparoscopic group [9].
In our study, the incidence of postoperative complications in patients who underwent intestinal resection was significantly higher in the open group. This result might be associated with the invasiveness of laparotomy in addition to resection of the intestine. Notably, four out of nine patients who underwent open repair with intestinal resection developed paralytic ileus, which implies the possibility of developing respiratory failure due to aspiration, especially in elderly patients. In patients without intestinal resection, bleeding amount and postoperative length of stay were significantly more favorable in the laparoscopic group. Accordingly, laparoscopic repair might be the treatment of choice for incarcerated OH regardless of the necessity of intestinal resection. However, not all patients with an incarcerated OH will achieve laparoscopic surgery without conversion [10, 12]. The reasons for conversion may include iatrogenic bowel injury, inadequate visualization and the need for bowel resection [13, 14]. Regarding visualization, in our study, all 11 patients who underwent laparoscopic repair did not require conversion. Although patients with severe intestinal dilation had open repair, it seemed that the patients with OH were usually thin with reduced visceral fat, resulting in relatively good visualization under the pneumoperitoneum even if the intestines were moderately dilated. Of course, early diagnosis is essential for achieving good visualization and completing laparoscopic surgery without conversion. Regarding the need for intestinal resection, three patients in the laparoscopic group underwent intestinal resection. In these three patients, we could complete the surgery with minilaparotomy without conversion to open repair. Previous reports suggested the utility of laparoscopic surgery with minilaparotomy in small bowel resection without conversion to laparotomy [15, 16]. Our results suggest that a need for intestinal resection might not be a definitive reason for conversion or choosing open repair.
Susmallian reported that 20 of the 293 (6.82%) patients who underwent repair of a bilateral or recurrent inguinal hernia had an occult obturator hernia; further, 14 of these 20 patients had a bilateral lesion [3]. In our study, occult OH on the contralateral side was detected and repaired in 4 out of 29 patients (13.7%). In addition, 2 out of 29 patients had previous history of incarcerated OH on the contralateral side, and 1 patient developed recurrence of incarceration on the contralateral side 1 year after surgery. These data suggest that surgeons should check for the presence of an occult OH on the contralateral side and should repair it simultaneously, to avoid future complications and surgery [3]. Laparoscopic repair is considered a suitable procedure in checking for the presence of occult lesions on the contralateral side [9, 10, 17]. Actually, in our study, 3 out of 11 patients (27.7%) who underwent laparoscopic repair had an occult OH that was detected and repaired on the contralateral side, while this occurred in only 1 out of 18 patients (5.5%) in the open repair group. Recently, the feasibility of total extraperitoneal (TEP) technique has also been reported [18, 19].
OH usually occurs in elderly patients [1,2,3], many of whom take anticoagulant drugs. In our study, 7 out of 29 patients (24.1%) had taken anticoagulant medicine preoperatively, and 1 of these 7 patients, in the open repair group, developed postoperative hematoma. The patient had taken warfarin, and the hematoma developed postoperatively in her abdominal wall. Furthermore, she required blood transfusion due to the hematoma. A previous report suggested that patients with anticoagulant drugs had a significantly higher risk for postoperative bleeding following laparoscopic and open inguinal hernia repair [20]. Emergency operation is the standard treatment for incarcerated OH. On the other hand, from the standpoint of postoperative bleeding, including hematoma, a reduction of the incarcerated intestine followed by heparinization and elective surgery might be one option [21]. However, if the incarcerated intestine has irreversible ischemic changes or perforation, it is contraindicated to perform the reduction, and the patient will require an emergency operation. CT imaging provides useful information for not only diagnosis of OH [1, 2, 4], but also assessing ischemic changes of the intestine [22,23,24]. Reduced contrast enhancement of the bowel wall and elevation of bowel wall attenuation in an unenhanced image are highly predictive of ischemia [22, 23]. Surgeons should be meticulous when performing non-operative reduction of incarceration by referring to CT images in addition to the general condition and abdominal symptoms of the patients.
There were some limitations associated with this study. First, the present study was retrospective in nature and was performed in a single center. Second, the choice of procedure, laparoscopic or open, was at the surgeon’s discretion, and patients with severe conditions or with severe intestinal dilation generally had the open procedure. Surgeon expertise on laparoscopy might be another bias in the selection of the approach. In addition, the study population, in particular the number of patients who underwent laparoscopic repair with intestinal resection, was small and more intestinal resections were performed in the open group. Therefore, further study is needed to establish the superiority of laparoscopic repair for severe OH cases.
In conclusion, laparoscopic repair for OH showed more favorable outcomes compared with open repair in selected patients. Laparoscopic repair is considered as the treatment of choice for selected patients with OH due to its lower incidence of postoperative complications and usefulness for detecting and repairing occult OH on the contralateral side.
References
Chang SS, Shan YS, Lin YJ, Tai YS, Lin PW (2005) A review of obturator hernia and a proposed algorithm for its diagnosis and treatment. World J Surg 29:450–454
Petrie A, Tubbs RS, Matusz P, Shaffer K, Loukas M (2011) Obturator hernia: anatomy, embryology, diagnosis, and treatment. Clin Anat 24:562–569
Susmallian S, Ponomarenko O, Barnea R, Paran H (2016) Obturator hernia as a frequent finding during laparoscopic pelvic exploration: a retrospective observational study. Medicine (Baltimore) 95:e4102. https://doi.org/10.1097/MD.0000000000004102
Kulkarni SR, Punamiya AR, Naniwadekar RG, Janugade HB, Chotai TD, Vimal Singh T, Natchair A (2013) Obturator hernia: a diagnostic challenge. Int J Surg Case Rep 4:606–608
Zhang H, Cong JC, Chen CS (2010) Ileum perforation due to delayed operation in obturator hernia: a case report and review of literatures. World J Gastroenterol 16:126–130
Ng DC, Tung KL, Tang CN, Li MK (2014) Fifteen-year experience in managing obturator hernia: from open to laparoscopic approach. Hernia 18:381–386
Ramser M, Messmer AS, Zbinden I, Von Holzen U, Nebiker CA (2014) Incarcerated obturator hernia-laparoscopic repair with intraoperative view of the corona mortis. J Surg Case Rep. https://doi.org/10.1093/jscr/rju081
Otowa Y, Kanemitsu K, Sumi Y, Nakamura T, Suzuki S, Kuroda D, Kakeji Y (2014) Laparoscopic trans-peritoneal hernioplasty (TAPP) is useful for obturator hernias: report of a case. Surg Today 44:2187–2190
Hayama S, Ohtaka K, Takahashi Y, Ichimura T, Senmaru N, Hirano S (2015) Laparoscopic reduction and repair for incarcerated obturator hernia: comparison with open surgery. Hernia 19:809–814
Liu J, Zhu Y, Shen Y, Liu S, Wang M, Zhao X, Nie Y, Chen J (2017) The feasibility of laparoscopic management of incarcerated obturator hernia. Surg Endosc 31:656–660. https://doi.org/10.1007/s00464-016-5016-5
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Leitch MK, Yunaev M (2016) Difficult diagnosis: strangulated obturator hernia in an 88-year-old woman. BMJ Case Rep. https://doi.org/10.1136/bcr-2016-215428
Ghosheh B, Salameh JR (2007) Laparoscopic approach to acute small bowel obstruction: review of 1061 cases. Surg Endosc 21(11):1945–1949
O’Connor DB, Winter DC (2012) The role of laparoscopy in the management of acute small-bowel obstruction: a review of over 2000 cases. Surg Endosc 26:12–17
Kohga A, Kawabe A, Hasegawa Y, Yajima K, Okumura T, Yamashita K, Isogaki J, Suzuki K, Komiyama A (2017) Ileo-ileal intussusception caused by lymphangioma of the small bowel treated by single-incision laparoscopic-assisted ileal resection. World J Gastroenterol 23:167–172
Kohga A, Yamashita K, Hasegawa Y, Yajima K, Okumura T, Isogaki J, Suzuki K, Kawabe A, Komiyama A (2017) Torsion of atypical Meckel’s diverticulum treated by laparoscopic-assisted surgery. Case Rep Med. https://doi.org/10.1155/2017/4514829
Wada Y, Ohtsuka H, Adachi K (2015) Laparoscopic views of obturator hernia. J Gastrointest Surg 19:1925–1926
Karashima R, Kimura M, Taura N, Shimokawa Y, Nishimura T, Baba H (2016) Total extraperitoneal approach for incarcerated obturator hernia repair. Hernia 20:479–482
Sasaki A, Takeuchi Y, Izumi K, Morimoto A, Inomata M, Kitano S (2016) Two-stage laparoscopic treatment for strangulated inguinal, femoral and obturator hernias: totally extraperitoneal repair followed by intestinal resection assisted by intraperitoneal laparoscopic exploration. Hernia 20:483–488
Köckerling F, Roessing C, Adolf D, Schug-Pass C, Jacob D (2016) Has endoscopic (TEP, TAPP) or open inguinal hernia repair a higher risk of bleeding in patients with coagulopathy or antithrombotic therapy? Data from the Herniamed Registry. Surg Endosc 30(5):2073–2081
Kohga A, Kawabe A, Cao Y, Yajima K, Okumura T, Yamashita K, Isogaki J, Suzuki K (2017) Elective laparoscopic repair after reduction might be useful strategy for incarcerated obturator hernia: a case report. J Surg Case Rep. https://doi.org/10.1093/jscr/rjx180
Geffroy Y, Boulay-Coletta I, Jullès MC, Nakache S, Taourel P, Zins M (2014) Increased unenhanced bowel-wall attenuation at multidetector CT is highly specific of ischemia complicating small-bowel obstruction. Radiology 270:159–167
Millet I, Taourel P, Ruyer A, Molinari N (2015) Value of CT findings to predict surgical ischemia in small bowel obstruction: a systematic review and meta-analysis. Eur Radiol 25:1823–1835
Kohga A, Kawabe A, Yajima K, Okumura T, Yamashita K, Isogaki J, Suzuki K, Muramatsu K (2017) CT value of the intestine is useful predictor for differentiate irreversible ischaemic changes in strangulated ileus. Abdom Radiol (NY). https://doi.org/10.1007/s00261-017-1227-z
Acknowledgements
This work was supported by departmental resources only.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Kohga, A., Kawabe, A., Okumura, T. et al. Laparoscopic repair is a treatment of choice for selected patients with incarcerated obturator hernia. Hernia 22, 887–895 (2018). https://doi.org/10.1007/s10029-018-1747-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-018-1747-7