Abstract
Background
Obturator hernia (OH), a rare cause of acute small bowel obstruction, requires immediate surgical intervention to prevent serious complications and mortality. We assessed the safety and efficacy of laparoscopic surgery in patients with incarcerated OH presenting with acute abdomen in an emergency setting.
Methods
Data pertaining to patients diagnosed with incarcerated OH between 2011 and April 2015 at our hospital were reviewed. Patients’ characteristics, operation details and postoperative outcomes were retrospectively analyzed.
Results
All ten patients diagnosed with incarcerated obturator hernia during the reference period were females (average age 72.1 ± 11.8 years; average weight 44.1 ± 6.9 kg; average body mass index 17.8 ± 2.1 kg/m2; average operating time 63 ± 15 min; average hospital stay 6.2 ± 6.6 days). Twelve occult hernias, including six contralateral OHs, two ipsilateral femoral hernias and two bilateral femoral hernias were detected in six patients (60 %), which were simultaneously repaired after laparoscopic exploration. Nine patients (90 %) were successfully treated with synthetic mesh by laparoscopic technique. Only one case required intraoperative conversion to open surgery due to strangulated intestine with perforation. Wound infection was reported in one patient who had undergone bowel resection, but with an eventual complete recovery. Postoperative period was uneventful in the other nine patients. No recurrence or complications were reported on follow-up (mean duration of follow-up: 6–54 months).
Conclusion
In this study, laparoscopic technique was associated with a reduced duration of hospital stay and fewer complications. In addition to being a safe and minimally invasive strategy, it allowed for simultaneous diagnosis and treatment of occult hernias during the same procedure. The approach may be a better option for the treatment of incarcerated OH and occult hernias in selected patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Obturator hernia (OH) accounts for 0.07–1 % of all hernias [1]. It tends to occur in elderly, emaciated and multiparous females. Owing to its nonspecific clinical presentation, the diagnosis is often delayed and patients are likely to present with acute intestinal obstruction. Delayed surgical intervention is associated with high mortality, ranging between 11 and 50 % [2, 3]. However, the application of abdominal computed tomography (CT) readily affords a definitive preoperative diagnosis, allowing for early surgical intervention and thereby helps reduce the incidence of complications, such as those that may necessitate lower bowel resection or even death [4, 5].
Exploratory laparotomy with hernia repair and intestinal resection, if necessary, has been the traditional treatment strategy in these patients. However, the laparoscopic approach is increasingly being employed owing to its safety, feasibility and favorable outcomes [6–8]. Nevertheless, the laparoscopic approach has not been widely accepted. In this study, we sought to further evaluate the safety and efficacy of this approach.
Methods
We conducted a retrospective analysis of data pertaining to patients that underwent emergency laparoscopic hernia repair for incarcerated OH at our hospital (Department of Hernia and Abdominal Wall Surgery, Beijing Chao-Yang Hospital, Capital Medical University) between 2011 and April 2015. Patient characteristics, operative details, methodology of repair, duration of hospital stay, incidence of complications, mortality and recurrence were reviewed. This study was approved by Institutional Ethnic Committee of Beijing Chao-Yang Hospital, and a written informed consent was obtained from all participants.
Results
A total of ten patients underwent emergency laparoscopic surgery for incarcerated OH during the reference period. Baseline patient characteristics are summarized in Table 1. Out of the ten patients, only one patient required conversion to laparotomy due to strangulated intestine with perforation. All patients were females. The mean age was 72.1 ± 11.8 years (range 57–86 years); the mean weight was 44.1 ± 6.9 kg (range 35–53 kg); the mean body mass index was 17.8 ± 2.1 kg/m2 (range 14.1–20.8 kg/m2); and the mean number of pregnancies was 2.4 ± 1.8 (range 1–7). Two patients had a history of previous abdominal operation. The mean preoperative period after the onset of symptoms was 2.5 ± 2.4 days (range 1–9 days).
All our patients had intestinal obstruction. Only five patients (50 %) had a positive Howship–Romberg sign. Preoperative CT examination confirmed the diagnosis of incarcerated obturator hernia in all patients.
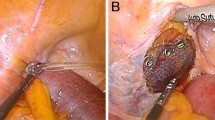
During the process of the operative, six (60 %) right and four (40 %) left unilateral obstructed obturator hernias were detected. Six patients (60 %) were found to have occult contralateral obturator hernias, out of which four patients also had groin hernias (two ipsilateral femoral hernias and two bilateral femoral hernias) which were simultaneously repaired after laparoscopic exploration. Nine patients (90 %) were successfully treated with mesh, while one patient underwent surgical repair with direct simple suture as intestinal segmentectomy had to be performed (Table 2).
The mean operating time was 63 ± 15 min (range 40–90 min), and the mean length of hospital stay was 6.2 ± 6.6 days (range 3–24 days). There was no mortality in our group. No major complications were reported. Wound infection occurred in one patient who had undergone bowel resection and who eventually made a full recovery after 19 days of daily dressing change. The postoperative period was uneventful in the other nine patients. No major complications, recurrence or mortality were observed during the follow-up period, ranging from 6 to 54 months (31 ± 15 months) (Table 3).
Discussion
Obturator hernias account for 0.05–0.4 % of all abdominal wall hernias and are a rare cause of small bowel obstruction first reported by Ronsil in 1724 [9, 10]. The clinical presentation is often nonspecific which results in difficultly in arriving at preoperative diagnosis, leading to a high mortality rate of 11–50 % [2, 3]. Howship–Romberg sign is a characteristic sign caused by the compression of obturator nerve by the contents of the hernia sac, which is presented in 37–60 % of the patients [11–13]. The pain usually radiates from the groin to the knee and is typically exacerbated by adduction and internal rotation of the thigh and relieved by leg flexion. In our study, all ten patients underwent emergency surgery for intestinal obstruction. Of these, only five patients (50 %) had a positive Howship–Romberg’s sign, which disappeared spontaneously during the postoperative course.
Obturator hernia is six to nine times more common in women as compared to that in men, because of wider pelvis and greater diameter of the obturator foramen [14]. These women are typically in the older age group, thin and multiparous, with coexisting chronic disorders such as chronic bronchitis, chronic obstructive pulmonary disease and constipation. The laxity of pelvic tissues, decreased pre-peritoneal fat covering the obturator foramen and increased pressure of the abdominal cavity are the risk factors associated with OH.
All patients in this study were in the elderly age group (mean age 72.1 ± 11.8 years; range 57–86 years), thin (mean BMI 17.8 ± 2.1 kg/m2; range 14.1–20.8 kg/m2) and multiparous women (mean obstetric history was 2.4 ± 1.8 times, range 1–7 times). In view of these typical characteristics, obturator hernia should be suspected in old and emaciated women with suspected intestinal obstruction and radiating pain over medial aspect of thigh, even those without previous abdominal operation. Delayed diagnosis is associated with a high morbidity and mortality [15]. Therefore, rapid preoperative diagnosis followed by appropriate surgical intervention is essential in these patients.
Computed tomography has a high diagnostic accuracy of >90 % and is regarded as the most useful diagnostic tool in suspected cases of OH [10, 11, 16, 17]. However, results of CT imaging are not always consistent with intraoperative findings [18], and in such cases, an accurate diagnosis may only be possible intraoperatively. In all our patients, the diagnosis was readily made with the use of preoperative CT. However, twelve occult hernias were definitely diagnosed laparoscopically. Indeed, the laparoscopic technique may be a sensitive diagnostic tool.
The standard treatment approach for obstructed OH is early surgery. The traditional approach remains open surgery, usually with lower middle incision, in order to obtain a definitive diagnosis and gain enough exposure to identify the hernia sac entering the defect and to perform bowel resection, if necessary. However, recently, the laparoscopic approach is being performed increasingly.
The key advantage of the laparoscopic approach is its minimally invasive nature, while the high cost and the relatively longer duration of surgery are some of the disadvantages [19]. A recent study [6] demonstrated the superiority of the laparoscopic approach over the open approach. The median operative time for laparoscopic versus open surgery was 68 and 65 min (P = 0.690), and the median hospital stay was 5 and 19 days (P = 0.007), respectively. Further, the incidence of major complications (P = 0.004) and mortality (P = 0.049) was significantly lower with laparoscopic surgery.
The subgroup analysis [6] which was performed on patients presenting with intestinal obstruction in emergency also revealed the advantage of the laparoscopic approach. There was no significant difference in operative time (60 vs. 70 min, P = 0.217) and the median hospital stay (12 vs. 5 days, P = 0.019), and the overall complications (5 vs. 0 patients, P = 0.041) were significantly lower in the laparoscopic group.
We employed the transabdominal preperitoneal approach for the reduction in incarcerated hernia sac and to assess the bowel viability. Our results were compared with the previously published data [6] and showed acceptable results (Table 4). The mean operating time had not been extended (63 vs. 60 min); the hospitalization time was obviously shorter (6.2 vs. 12 days). We confirmed the diagnosis intraoperatively and simultaneously repaired the occult hernias. All our patients had no major complications and are completely recovered. There were no deaths or instances of recurrence during the follow-up period.
Although the consensus has not yet been reached, an increasing number of studies [7, 20–22] have reported successful laparoscopic management of incarcerated obturator hernia with acceptable results. Because of the low incidence of incarcerated OH, we were unable to compare laparoscopy with open surgery in the management of this condition. Instead, we had to compare our outcomes with reported literature.
The laparoscopic approach may not be applicable to all the emergency cases. In one patient in the present study, a conversion to laparotomy had to be performed, as the time from onset of symptoms to surgery was 9 days, and a diagnosis of intestinal strangulation with perforation was made on laparoscopy. After the necrosis bowel was resected with lower middle incision, the pre-peritoneal space was separated. We resected the redundant hernia sac with high ligation and sutured adjacent tissue to close the defect. The medical history of the patient will determine the choice of the surgical approach. According to our data, laparoscopy is likely to be more effective in patients who are presented within 2 days of onset of symptoms. These results need to be confirmed by further studies involving a larger sample size.
Conclusion
In this study, use of laparoscopic technique was associated with a reduced duration of hospital stay and fewer complications. In addition to being a safe and minimally invasive strategy, it allowed for simultaneous diagnosis and treatment of occult hernias during the same procedure. The approach may be a better option for the treatment of incarcerated OH and occult hernias in selected patients.
References
Mantoo SK, Mak K, Tan TJ (2009) Obturator hernia: diagnosis and treatment in the modern era. Singap Med J 50(9):866–870
Lo CY, Lorentz TG, Lau PW (1994) Obturator hernia presenting as small bowel obstruction. Am J Surg 167(4):396–398
Yokoyama Y, Yamaguchi A, Isogai M, Hori A, Kaneoka Y (1999) Thirty-six cases of obturator hernia: does computed tomography contribute to postoperative outcome? World J Surg 23(2):214–216 discussion 217
Haraguchi M, Matsuo S, Kanetaka K, Tokai H, Azuma T, Yamaguchi S, Kanematsu T (2007) Obturator hernia in an ageing society. Ann Acad Med Singap 36(6):413–415
Kammori M, Mafune K, Hirashima T, Kawahara M, Hashimoto M, Ogawa T, Ohta H, Hashimoto H, Kaminishi M (2004) Forty-three cases of obturator hernia. Am J Surg 187(4):549–552. doi:10.1016/j.amjsurg.2003.12.041
Ng DC, Tung KL, Tang CN, Li MK (2014) Fifteen-year experience in managing obturator hernia: from open to laparoscopic approach. Hernia 18(3):381–386. doi:10.1007/s10029-013-1080-0
Hayama S, Ohtaka K, Takahashi Y, Ichimura T, Senmaru N, Hirano S (2015) Laparoscopic reduction and repair for incarcerated obturator hernia: comparison with open surgery. Hernia 19(5):809–814. doi:10.1007/s10029-014-1328-3
Liu WY, Liu XH (2015) Laparoscopic technique in treatment of obturator hernia. China J Hernia Abdom Wall Surg (Electronic Edition) 9(3):261–262
Francis WW (1995) Obturator hernia needs a laparotomy, not a diagnosis. Am J Surg 170(3):309
Dundamadappa SK, Tsou IY, Goh JS (2006) Clinics in diagnostic imaging (107). Singap Med J 47(1):89–94 quiz 95
Nasir BS, Zendejas B, Ali SM, Groenewald CB, Heller SF, Farley DR (2012) Obturator hernia: the Mayo Clinic experience. Hernia 16(3):315–319. doi:10.1007/s10029-011-0895-9
Katoh T, Kawamoto R, Kusunoki T (2011) A case of obturator hernia with overlooked Howship-Romberg sign and treated as sciatica. Nihon Ronen Igakkai Zasshi 48(2):176–179
Nakayama T, Kobayashi S, Shiraishi K, Nishiumi T, Mori S, Isobe K, Furuta Y (2002) Diagnosis and treatment of obturator hernia. Keio J Med 51(3):129–132
Shapiro K, Patel S, Choy C, Chaudry G, Khalil S, Ferzli G (2004) Totally extraperitoneal repair of obturator hernia. Surg Endosc 18(6):954–956. doi:10.1007/s00464-003-8212-z
Jayant K, Agarwal R, Agarwal S (2014) Richter type of incarcerated obturator hernia; misery still continues. Pol Przegl Chir 86(10):490–492. doi:10.2478/pjs-2014-0087
Kohi S, Sato N, Mori Y, Uehara T, Tamura T, Minagawa N, Torigoe T, Shibao K, Higure A, Yamaguchi K (2013) A review of 13 cases of obturator hernia. J uoeh 35(4):273–277
Khaladkar SM, Kamal A, Garg S, Kamal V (2014) Bilateral obturator hernia diagnosed by computed tomography: a case report with review of the literature. Radiol Res Pract 2014:625873. doi:10.1155/2014/625873
Hodgins N, Cieplucha K, Conneally P, Ghareeb E (2013) Obturator hernia: a case report and review of the literature. Int J Surg Case Rep 4(10):889–892. doi:10.1016/j.ijscr.2013.07.012
Haith LR Jr, Simeone MR, Reilly KJ, Patton ML, Moss BE, Shotwell BA (1998) Obturator hernia: laparoscopic diagnosis and repair. Jsls 2(2):191–193
Hunt L, Morrison C, Lengyel J, Sagar P (2009) Laparoscopic management of an obstructed obturator hernia: should laparoscopic assessment be the default option? Hernia 13(3):313–315. doi:10.1007/s10029-008-0438-1
Lynch NP, Corrigan MA, Kearney DE, Andrews EJ (2013) Successful laparoscopic management of an incarcerated obturator hernia. J Surg Case Rep. doi:10.1093/jscr/rjt050
Ramser M, Messmer AS, Zbinden I, Von Holzen U, Nebiker CA (2014) Incarcerated obturator hernia-laparoscopic repair with intraoperative view of the corona mortis. J Surg Case Rep. doi:10.1093/jscr/rju081
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Drs. Jing Liu, Yilin Zhu, Yingmo Shen, Sujun Liu, Minggang Wang, Xuefei Zhao, Yusheng Nie and Jie Chen have no conflicts of interest or financial ties to disclose.
Additional information
Jing Liu and Yilin Zhu have contributed equally to this work
Rights and permissions
About this article
Cite this article
Liu, J., Zhu, Y., Shen, Y. et al. The feasibility of laparoscopic management of incarcerated obturator hernia. Surg Endosc 31, 656–660 (2017). https://doi.org/10.1007/s00464-016-5016-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5016-5