Abstract
The aim of this article is to provide a review of six patients with the various stages of obturator hernia and a diagnostic and therapeutic strategy in suspected cases. Obturator hernia is relatively rare and is a diagnostic challenge. It is a significant cause of intestinal obstruction, especially in emaciated elderly women with chronic disease. A palpable groin mass is not common in these patients because the hernia mass is usually concealed beneath the pectineus muscle. The high mortality is directly related to the delayed recognition, with resultant ruptured gangrenous bowel, and to the high incidence of patients with concurrent medical illness. A total of six patients with obturator hernias were treated at this hospital between 1994 and 2004, and one of these patients was diagnosed and treated by elective laparoscopy. We reviewed these six cases and examined the clinical presentation, age, body weight, associated medical conditions, preoperative diagnosis, operative findings, complications, and outcome in this retrospective study. We concluded that we cannot shorten the time from onset of symptoms to admission, but what we can do is to make a rapid evaluation and surgical intervention to reduce the morbidity and mortality from obturator hernia. The approaches to different presentation of obturator hernia and diagnostic role of CT scan are also discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Obturator hernia is relatively rare. It occurs through the obturator canal, adjacent to the obturator vessels and nerve. The condition was first described in 1724 by Arnaud de Ronsil and the first successful obturator hernia repair was performed by Obre in 1851. Reported incidence of obturator hernia ranges from 0.05% to 1.4% of all hernias [1–3]. Obturator hernia is thought to result from progressive laxity of the pelvic floor which may be associated with advanced age, emaciation, increased intraabdominal pressure, and multiparity. The three stages of obturator hernia formation were described by Gray et al. [4]. It is difficult to diagnose preoperatively, and the diagnosis is usually made at laparotomy for intestinal obstruction or peritonitis. For diagnosis and treatment, some authors advocate early performance of laparotomy [1], whereas others prefer preoperative noninvasive diagnostic methods such as computed tomography (CT) [3, 5, 6] or contrast radiographs [7]. Computed tomography has been increasingly used to detect obturator hernia in patients with ileus, thus significantly aiding the surgeons in emergent management.
We present six surgically proven cases of obturator hernia during a 10-year period at this hospital; one of these patients was diagnosed and treated by elective laparoscopy.
In most patients with obturator hernia, emergent operation is performed for treatment of intestinal obstruction with or without a definitive preoperative diagnosis. The average preoperative delay has been reported as 2.2 days for survivors and 5.1 days for fatal cases [8]. We cannot shorten the time from onset of symptoms to admission, but what we can do is to make a rapid evaluation and surgical intervention to reduce the morbidity and mortality associated with obturator hernia. The approaches to different presentations of obturator hernia will be discussed.
Materials and Methods
A total of six patients with obturator hernias were treated at N.C.K.U. hospital between 1994 and 2004. Five of six obturator hernias were treated by emergency laparotomy. The remaining patient underwent laparoscopic diagnosis and repair of the obturator hernia. The first five patients (cases 1–5) visited our emergency room (ER) because of abdominal pain, and the sixth patient (case 6) was referred to our outpatient department (OPD) with a diagnosis of left inguinal hernia. In three of six patients, emergency CT scan was obtained and a preoperative diagnosis of obturator hernia was made. Another two patients were diagnosed at immediate laparotomy, and the remaining patient was diagnosed by elective laparoscopy. We reviewed these cases and examined the clinical presentation, age, body weight, associated medical conditions, preoperative diagnosis, operative findings, complications, and outcome in this retrospective study.
Results
Cases 1–5
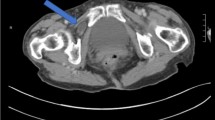
All patients were old thin women with a mean age of 79.8 years (range: 70–88 years) and a mean weight of 37.3 kg (range: 30–42.4 kg). Of the presenting complaints, all were those of intestinal obstruction and two were related to Howship-Romberg’s sign (thigh or groin pain of the affected site). The interval between onset of symptoms and operation ranged from 1 to 10 days (mean 5.2 days). The concomitant conditions included chronic obstructive pulmonary disease, inguinal hernia, abdominal aortic aneurysm, kyphoscoliosis, and unresectable Klaskin tumor. No patients had had previous abdominal surgery. The patients were hospitalized for 1 to 3 days prior to their surgery; five of the six patients underwent emergency laparotomy for intestinal obstruction or peritonitis. Obturator hernia was diagnosed in three patients preoperatively from CT scans that demonstrated a low-density mass between the pectineus and external obturator muscles (Fig. 1). All three patients underwent celiotomy as soon as possible after CT scans were obtained. Midline incisions were performed in these five patients. There were two left and three right obturator hernias. Incarcerated ileums were found in the hernial sac, and all patients required resection of nonviable intestine. No perforation of small bowel was noted during the operations. The obturator canal defects were repaired with synthetic mesh because peritoneal contamination was not severe. The emergent celiotomies (cases 1–5) were performed by different surgeons, and no standard mesh size was used in the repair of the obturator hernia. In every case, the mesh was anchored in the preperitoneal space. All these patients received antibiotic treatment postoperatlvely. No wound infection was noted postoperatively. Four of five patients recovered uneventfully. One patient (case 4) died of bronchopneumonia 14 days postoperatively. Details of these five cases are shown in Table 1.
Case 6
A 62-year-old woman underwent THR (total hip replacement) for a right osteoarthritic hip one year earlier. A protruding mass over the left parapubic area was noted six months later. The patient had had several episodes of intermittent lower abdominal pain associated with nausea during previous months, but it relieved spontaneously. At physical examination, the only abnormal finding was a questionable lump over the left parapubic region. Because of the symptoms and the apparent left parapubic hernia, an exploratory laparoscopy was performed. A left obturator hernia without incarcerated content, a peritoneal dimple over the internal opening of the obturator canal, was identified. A laparoscopic transabdominal preperitoneal (TAPP) approach was chosen to repair the obturator hernia [9]. The entrance of preperitoneal connective tissue and fat into the canal was noted after the peritoneal flap was further dissected down to most inferior aspect of the obturator hernial sac. After the herniated prepritoneal fat was pulled out, the skeketionzed obturator forman defect was repaired with a piece of 3 × 5 inch polypropylene mesh. The prosthesis was fixed with staples and the peritoneum was approximated over the mesh. The total operative time was 75 min. The patient was discharged uneventfully the following day. No recurrence of the hernia and no similar symptoms have been noted during follow-up.
Discussion
Obturator hernia is associated with multiple predisposing factors. In women, a wider pelvis and more triangular obturator canal opening with a greater transverse diameter may increase the risk for development of an obturator hernia. Obturator hernia occurs most frequently in emaciated patients between 70 and 90 years of age. The loss of protective preperitoneal fat and lymphatic tissue from aging or malnutrition makes a larger space around the vessels and nerve, facilitating the formation of a hernia. Some concomitant condition (e.g., chronic constipation, COPD, ascites, kyphoscoliosis) and multiparty also predispose patients to herniation by increasing intraabdominal pressure and relaxing the peritoneum [10, 11].
The anatomic stages of the formation of obturator hernia have been described in detail elsewhere [4, 12, 13]. During the first stage, pre-peritoneal fat enters the pelvic orifice of the obturator canal, forming a pilot fat plug. The second stage begins with a peritoneal dimple through the canal and progresses to the formation of a peritoneal sac. The third stage of obturator hernia begins with the onset of symptoms produced by herniation of viscera into this sac. A palpable groin mass is not common in these patients because the hernia mass is usually concealed beneath the pectineus muscle. The symptoms of intestinal obstruction may be acute or intermittent if the hernial content reduces into the peritoneal cavity spontaneously. In another review, one third of patients had intermittent symptoms before surgical repair [14]. Such intermittent relief of intestinal obstruction by reduction of the hernia is also an important clue for diagnosis. There is a high frequency of Richter hernia of small bowel (41% to 100%) [11, 14, 15] in these cases; the symptoms are often mild initially and x-ray investigation may be inconclusive. If the Richter type of hernia does not reduce spontaneously, the obstruction may be partial or complete.
Howship-Romberg sign refers to pain along the distribution of the obturator nerve caused by compression of the nerve by the hernia sac. It is reportedly present in 15%–50% of obturator hernia patients [14]. Because osteoarthritis is common in elderly patients, the Howship-Romberg sign is often overlooked or misinterpreted [14, 16], leading to referred of these patients to neurologists and orthopedic surgeons. Furthermore, if incarceration of intestine develops, the severity of the intraabdominal symptoms generally masks the less acute symptoms of obturator neuropathy. Thus, a positive Howship-Romberg sign is not always noted, and the correct preoperative diagnosis is not often made [11]. In our series, two of the six patients had undergone total hip replacement for treatment of osteoarthritis (case 1 & 5). The Howship-Romberg sign and the related pain were neglected in two patients (case 3 & 5) preoperatively.
In those patients with atypical or ambiguous presentation of obturator hernia, several imaging modalities have been described as helping to establish the diagnosis, including barium enema fluoroscopy, ultrasonography [17, 18], herniography [19], and computed tomography. The herniography described by Gullmo is the only effective diagnostic method when the hernia is not incarcerated [19] (Fig. 2). Some authors indicate that emergency CT scan is useful for the diagnosis of obturator hernia, particularly in elderly patients presenting with ileus of unknown origin [3, 5, 6, 7]. Yokoyama et al. reported that CT scan facilitated the correct preoperative diagnosis of obturator hernia, but it did not decrease the rate of bowel necrosis or of postoperative morbidity and mortality [20]. This is so because in most cases more than 3 days (average 4.5 days) have passed from the onset of symptoms to surgery. Thus the duration of symptoms is one of the major factors affecting the rate of bowel resection. However, early diagnosis with CT scans and surgery produced good results in another series of patients [5].
There is often a delay in diagnosis and surgical intervention of obturator hernia, despite the presence of a bowel obstruction. In most cases, resuscitation was first performed and medical treatment was tried for the intestinal obstruction. Some surgeons have hesitated to operate because of the patients’ advanced age, their underlying disease, and their generally debilitated condition [21]. The delay undoubtedly contributes to the need for resection of the gangrenous bowel (25%–75%) [14, 22, 23] and the associated high mortality rate (12%–70%) [14, 24]. Thus published reports show that the high mortality is directly related to the delayed recognition with resultant ruptured gangrenous bowel, and the high incidence of concurrent medical illness. In other reviews of obturator hernia, the rate of correct preoperative diagnosis ranged from 21.5% to 31.3% [22]. In our series, the preoperative CT scans performed on three patients led to a definitive diagnosis of obturator hernia leading to immediate operative intervention.
It has been said that obturator hernia needs a laparotomy, not a diagnosis [1]. In other words, early surgical intervention is needed when complete obstruction or peritonitis have developed, not prolonged preoperative evaluation. The obturator hernia might be in the third stage, with partial or complete herniation, at the time of admission. When clinical features suggest strangulation, exploratory laparotomy should not be delayed (Fig. 2). However, initial nonspecific symptoms and vague clinical signs seldom facilitate the decision to perform emergency operation in elderly patients with poor general health. In the absence of a strong indication for emergent operation, uncertainty may lead to delayed surgical intervention, which contributes to high mortality. Emergency CT scan is minimally invasive and readily available. Obtaining such a study requires only a short period of time in our institute. Therefore, in patients who may have obturator hernia but for whom urgent laparotomy is not needed for bowel obstruction or peritonitis, emergency CT scan could lead to rapid diagnosis and early surgical intervention. Because the diagnosis is often delayed until laparotomy for complete bowel obstruction or peritonitis becomes necessary, CT of the abdomen, including the pelvic area, is strongly recommended.
A variety of operative approaches have been advocated for the repair of the defect, including the Cheatle-Henry retropubic approach [15], a preperitoneal approach, an inguinal approach [25], and an intraabdominal approach. Laparoscopy is another alternative to diagnose, reduce, and repair an obturator hernia [2, 9, 26, 27]. This less invasive surgical approach may provide some benefits for these high-risk patients, such as short hospital stay, less ileus, reduced postoperative pain, and fewer pulmonary complications. However, there is still much concern as to whether laparoscopic bowel anastomosis can be performed safely and quickly. Without conclusive historical or physical findings — especially when there is no evidence of acute complete intestinal obstruction — the laparoscopic approach may offer a mini-invasive method to identify and treat obturator hernia (Fig. 2). In our case 6, the patient presented with a vague parapubic lump and less acute nonspecific symptoms. We therefore elected to perform an exploratory laparoscopy. A transabdominal preperitoneal (TAPP) approach was chosen to diagnose and treat the obturator hernia at laparoscopy.
In patients with strangulated obturator hernia, the time between onset of symptoms of intestinal obstruction and surgical intervention is perhaps even more important than a definitive diagnosis. Obturator hernia should be suspected when an elderly, emaciated, chronically ill woman without previous abdominal operation presents with symptoms of bowel obstruction or uncertain pain over the thigh and hip. In those cases presenting with complete bowel obstruction or peritonitis, an immediate laparotomy is indicated, even without a preoperative diagnosis. As discussed above, if the decision to proceed to surgical intervention is delayed because of equivocal findings, an emergency CT scan might be helpful. The rapid evaluation and appropriate treatment of these patients must be accomplished within hours and not days (Fig. 2).
Conclusions
Obturator hernia is relatively rare and is a diagnostic challenge. Obturator hernia is a significant cause of intestinal obstruction, especially in emaciated elderly women with chronic disease. Patients often undergo surgical repair only when they experience bowel obstruction caused by incarcerated or strangulated small intestine. If the surgical intervention is delayed, a complicated postoperative course and even death are common because of advanced age, underlying disease, the generally debilitated condition.
Diagnostic and therapeutic strategies of suspected obturator hernia depend on the clinical findings: prevailing peritonitis or complete obstruction of the bowel result should lead to emergent laparotomy; prevailing abdominal cramping pain or ileus without peritonitis allows time for emergent CT scan of the abdomen including the pelvic area. Laparoscopy may be considered in selected situations.
The importance of early surgical intervention is highlighted because it is the only hope to lower the high morbidity and mortality associated with this condition. A treatment decision can be made as a result of detailed history taking, physical examination, and emergent CT scan. Understanding the pathogenesis of obturator hernia may also help with recognition of this condition in its various presentations and thus avoid delayed surgical intervention.
References
DW Ziegler JE. Rhoads (1995) ArticleTitleObturator hernia needs a laparotomy, not a diagnosis Am. J. Surg. 170 67–68 Occurrence Handle10.1016/S0002-9610(99)80256-6 Occurrence Handle7793500
CG Jorge RD Manuel ED Alexandro et al. (1998) ArticleTitleIncarcerated obturator hernia successfully treated by laparoscopy Surg. Laparosc. Endosc. 8 71–73 Occurrence Handle10.1097/00019509-199802000-00017 Occurrence Handle9488576
R Ijiri H Kanamaru H Yokoyama et al. (1996) ArticleTitleObturator hernia: the usefulness of computed tomography in diagnosis Surgery 119 137–140 Occurrence Handle8571197
SW Gray JE Skandalakis RE Soria et al. (1974) ArticleTitleStrangulated obturator hernia Surgery 75 20–27 Occurrence Handle4808720
M Nishina C Fujii R Ogino et al. (2001) ArticleTitlePreoperative diagnosis of obturator hernia by computed tomography in six patients J. Emerg. Med. 20 277–280 Occurrence Handle10.1016/S0736-4679(01)00281-5 Occurrence Handle11267817
R Terada S Ito H Kidogawa et al. (1999) ArticleTitleObturator hernia: the usefulness of emergent computed tomography for early diagnosis J. Emerg. Med. 17 883–886 Occurrence Handle10.1016/S0736-4679(99)00100-6 Occurrence Handle10499707
JM Bergstein RE. Condon (1996) ArticleTitleObturator hernia: current diagnosis and treatment Surgery 119 133–136 Occurrence Handle8571196
A. Gunnar (1984) ArticleTitleStrangulated obturator hernia Acta Chir. Scand. 150 337–339 Occurrence Handle6377785
SS Chang YS Tai PW. Lin (2003) ArticleTitleObturator hernia diagnosed and treated by laparoscopy: a case report Formosa. J. Surg. 36 244–247
FA Rogers (1964) Strangulated obturator LM Nyhus JN Harkins (Eds) Hernia Lippincott Philadelphia 637–644
KJ Bjork P Mucha DR. Cahill (1988) ArticleTitleObturator hernia Surg. Gynecol. Obstet. 167 217–222 Occurrence Handle3413651
LJ Skandalakis J Androulakis GL Colborn et al. (2000) ArticleTitleObturator hernia. Embryology, anatomy, and surgical applications Surg. Clin. North Am. 80 71–84 Occurrence Handle10.1016/S0039-6109(05)70398-4 Occurrence Handle10685145
CJ Callaghan RH. Whitaker (2002) ArticleTitleObturator canal fat plug: a pre-hernia condition? Clin Anat 15 276–279 Occurrence Handle10.1002/ca.10025 Occurrence Handle12112355
AW Yip AK AhChong KH Lam (1993) ArticleTitleObturator hernia: a continuing diagnostic challenge Surgery 113 266–269 Occurrence Handle8441961
SW Gray JE Skandalakis RE Soria et al. (1974) ArticleTitleStrangulated obturator hernia Surgery 75 20–27 Occurrence Handle4808720
FA. Rogers (1960) ArticleTitleStrangulated obturator hernia Surgery 48 394–403 Occurrence Handle14438359
T Yokoyama Y Munakata M Ogiwara et al. (1997) ArticleTitlePreoperative diagnosis of strangulated obturator hernia using ultrasonography Am. J. Surg. 174 76–78 Occurrence Handle10.1016/S0002-9610(97)00025-1 Occurrence Handle9240958
H Kanzaki S Kameoka S Imai et al. (1989) ArticleTitleThree cases of obturator hernia diagnosed preoperatively by ultrasonography. Nippon Rinsho Geka Igakkai Zasshi J. Jpn. Soc. Clin. Surg. 50 2488–2499
A. Gullmo (1980) ArticleTitleHerniography: the diagnosis of hernia in the groin and incompetence of the pouch of Douglas and pelvic floor Acta Radiol. Suppl. 361 71
Y Yokoyama A Yamaguchi M Isogai et al. (1999) ArticleTitleThirty-six cases of obturator hernia; does computed tomography contribute to postoperative outcome? World J Surg. 23 214–216
PH Schmidt WJ Bull KM Jeffery et al. (2001) ArticleTitleTypical versus atypical presentation of obturator hernia Am. Surg. 67 191–195 Occurrence Handle11243549
SN Sinha AE. DeCosta (1983) ArticleTitleObturator hernia Aust. N. Z. J. Surg. 53 349–351 Occurrence Handle6577852
MJ Hershman DT Reilly RI. Swift (1986) ArticleTitleStrangulated obturator hernia: delayed diagnosis is still the rule J. R. Coll. Surg. Edinb. 31 282–283 Occurrence Handle3795147
E. Cubillo (1983) ArticleTitleObutrator hernia diagnosed by computed tomography Am. J. Roentgenol. 140 735–736
A Somell I Ljungdahl L. Spangen (1976) ArticleTitleThigh neuralgia as a symptom of obturator hernia Acta Chir. Scand. 142 457–459 Occurrence Handle1007792
JG Tucker RA Wilson BJ Ramshaw et al. (1995) ArticleTitleLaparoscopic herniorrhaphy: technical concerns in prevention of complications and early recurrence Am. Surg. 61 36–39 Occurrence Handle7832379
Y Miki J Sumimura T Hasegawa et al. (1998) ArticleTitleA new technique of laparoscopic obturator hernia repair: report of a case Surg. Today 28 652–656 Occurrence Handle10.1007/s005950050201 Occurrence Handle9681618
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chang, SS., Shan, YS., Lin, YJ. et al. A Review of Obturator Hernia and a Proposed Algorithm for its Diagnosis and Treatment. World J. Surg. 29, 450–454 (2005). https://doi.org/10.1007/s00268-004-7664-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-004-7664-1