Abstract
Background
The primary aim of this prospective study is to report bulging and recurrence rates and to analyze the risk factors responsible for failure, after laparoscopic ventral hernia repair (LVHR) with primary closure of defect (PCD) using a running suture and intraperitoneal mesh placement, at 5-year follow-up. The secondary endpoint is to evaluate 30-day postoperative complications, seroma, and pain.
Methods
PCD failure was defined as the presence of postoperative bulging and/or recurrence. Pain was evaluated using a visual analogue scale (VAS). After surgery, fifty-eight patients underwent clinical examination and computed tomography scan to diagnose bulging, recurrence, and seroma (classified according to the Morales-Conde classification).
Results
At 60 months follow-up, recurrence was observed in five patients (8.6%), while bulging, not needing a surgical treatment, occurred in fifteen patients (25.9%). Chronic obstructive pulmonary disease (COPD) is the only risk factor responsible for both outcomes together, bulging and recurrences (p = 0.029), while other considered risk factors as gender, age, body mass index, diabetes, smoke habits, primary or incisional hernia and the ratio defect width/transverse abdominal axis did not achieve the statistically significance. Clinical seroma was diagnosed at one month in eight patients (13.8%). Seromas were observed at one year of follow-up. During the follow-up, pain reduction occurred.
Conclusion
LVHR has evolved toward more anatomical concepts, with the current trend being the abdominal wall anatomical reconstruction to improve its functionality, reducing seroma rates. Based on results obtained, PCD is a reliable technique with excellent recurrence rate at 5 years follow-up, even when the defect closure may generate tension at the midline. On the other hand, this tension could be related with high bulging rate at long-term, particular in case of patients with COPD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic ventral hernia repair (LVHR) is reported as a safe, reliable, and reproducible minimally invasive technique with low postoperative complication rate, since it was described by Leblanc et al. [1, 2]. However, debate has emerged due to the use of an intra-abdominal mesh as bridge of the defect, which has a negative impact on the abdominal wall functionality, due to it does not allow to restore the abdominal wall midline, and on seroma development, achieving up 100% of cases in some series [3, 4].
The new trend in LVHR is based on the abdominal wall reconstruction concept associated to new techniques related to primary closure of the defect (PCD), which was first described in a large series by Chelala et al. [5]. This approach, named IPOM (intraperitoneal onlay mesh) plus, proved that the midline closure improves the abdominal wall function and patients’ quality of life [6], reducing bulging and seroma rate in comparison to conventional LVHR with standard IPOM technique, at short-term follow-up [7]. However, PCD could be related to an increase of postoperative pain and recurrences, due to tension created from the midline closure [8].
The primary aim of the present study is to analyze the postoperative outcomes after PCD, in terms of recurrences at long-term follow-up, adding the concept of failure of the repair also including the rate of bulging at 5 years, and to report the risk factors related to the failure; the secondary aim is to report the postoperative complications, seroma and pain at one and 5 years after surgery.
Materials and methods
This is a prospective study performed from December 2013 to January 2016, including 60 patients with midline primary or incisional ventral hernia who underwent LVHR with PCD and IPOM.
Institutional review board approval (number: 1002-N-15) and informed consent from all participants were obtained.
Inclusion criteria
Patients over 18 years, with primary or incisional midline ventral hernia (classified according to the European Hernia Society—EHS classification [9]) greater than 3 cm in width and away from bone margins, American Society of Anesthesiologists (ASA) class I, II, or III and after signing the informed consent were included in this study.
Exclusion criteria
Patients with abdominal wall defect width less than 3 cm, with history of previous intraperitoneal mesh placement, ASA IV and/or with contraindications for general anesthesia and with lateral defects were excluded.
Surgical technique
The technique was standardized before the beginning of the study by the two surgeons who performed all cases (J.G.M. and S.M.C). All patients underwent surgery under general anesthesia. Pneumoperitoneum was created at 15 mmHg pressure with a Veress needle in the left upper quadrant. One 12 mm trocar for the 30° optic, and two 5 mm operating trocars were placed in line at the left midclavicular line. After adhesiolysis by blunt dissection and cold scissor, the abdominal wall defect width and length were measured with an intraabdominal ruler after reducing the pneumoperitoneum pressure to 8–9 mmHg.
The hernia sac was not resected in any case. Closure of the hernia defect was performed using a fully intracorporeal continuous suture with a long-term absorbable double-loop suture in polyglyconate 0 (Maxon™, monofilament absorbable suture, Medtronic, Minneapolis, Minnesota, USA) starting 1–2 cm caudal to the defect and ending 1–2 cm cranially to the defect. The running suture was finished cranially to the defect, and both ends of the double-loop suture were knotted together in the subcutaneous tissue, after reducing the pneumoperitoneum to 6–8 mmHg. The two threads were exteriorized from the abdominal cavity through the same small skin incision, but from different fascia incision, using a trocar site closure device (Endo CloseTM, Auto SutureTM, Covidien, Mansfield, Massachusetts, USA) or a suture passer.
In all cases, an intraperitoneal mesh was placed with 5 cm overlap over the original defect and fixed according to the double crown (DC) technique using titanium helical tacks (ProTack fixation device 5 mm; Covidien, Mansfield, Massachusetts, USA) every 2–3 cm. The gap among tacks was sealed with fibrin sealant (Tissucol Duo®, Baxter, Deerfield, Illinois, USA) [10, 11]. Based on the availability in the operative room, type of mesh used was the expanded polytetrafluoroethylene (ePTFE) mesh (DualMesh®, W. L. Gore & Associates, Inc., Newark, Delaware, USA), the polyvinylidene fluoride (PVDF) mesh (DynaMesh®-IPOM, FEG Textiltechnik, Aachen, Germany), and the polypropylene mesh (Ventralight™ Mesh, Bard, Warwick, Rode Island, USA).
After the first 15 patients, the 12 mm trocar closure was performed using the Weck EFx Endo Fascial Closure System (Teleflex Incorporated, Wayne, Pennsylvania, USA) to guarantee a full thickness closure of trocar site and avoiding risk of trocar site hernia.
Study design
Demographic variables [including gender, age, body mass index—BMI, comorbidities, smoke habitus, ASA class, hernia type, distance between rectus muscles (diastasis recti)], intraoperative variables (including defect size, mesh size, number of tacks used, type of mesh, conversion to open surgery and surgical time) and postoperative outcomes were recorded and analyzed.
Those postoperative outcomes include recurrence and bulging rates (both considered as failure of PCD), complications (according to Clavien–Dindo classification [12]), seroma (classified according to the Morales-Conde classification [13]), distance between rectus muscles [diastasis recti] and postoperative pain.
PCD failure was defined when bulging or recurrence occurred. Recurrence was defined when an abdominal wall defect with hernia sac occurred. While bulging was defined as clinical and/or radiological return to the original distance between rectus muscles without the presence of an abdominal wall hernia defect and without requiring surgical treatment.
Postoperative pain was evaluated using the visual analogue scale (VAS) score up to one year after surgery.
A computed tomography (CT) scan was performed preoperatively in all patients to evaluate the hernia content, to identify defects not diagnosed during physical examination, and to measure width and length defect and distance between the rectus muscles.
All patients were scheduled for postoperative physical examination at day 1, day 7, 1 month, 3, 12, and 60 months after surgery. Abdominal CT scan was performed at 1 and 12 months after surgery to evaluate the abdominal wall closure integrity, the presence of diastasis recti, seroma, or recurrence. 60 months after surgery, CT scan was performed in case of suspicion for recurrence or bulging at physical examination.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation and categorical variables as frequencies and percentages. Risk factors responsible for PCD failure are identified by comparing subsamples with and without PCD failure. The non-parametric Mann–Whitney test was used for the comparison between quantitative variables, and the Fisher’s exact test for the qualitative variables. A p value lower than 0.05 was considered statistically significant. Statistical analysis was carried out using the SPSS software (SPSS Inc., Chicago, Illinois, USA).
Results
Two out of 60 patients were excluded from the study, one because it was not possible to close the abdominal wall defect intraoperatively, and one due to intraoperative problem related to general anesthesia. In both cases conventional LVHR with IPOM was performed.
Tables 1, 2, and 3 report demographic and intraoperative variables. All patients’ comorbidities were stable and controlled at the time of surgery. Overall, ePTFE mesh was used in 43 patients (74.1%) since it was the mesh available in our center at the time of surgery. Mean mesh overlap over the defect (mesh size to defect size ratio) was 4.63 ± 1.28 cm.
Five years after surgery, five recurrences (8.6%) and fifteen bulging (25.9%) occurred (Table 4). In all these patients, ePTFE mesh was used. In two patients both bulging, and recurrence occurred. Overall patients with PCD failure at five years follow-up were 18 (31%).
Before surgery, the mean abdominal wall defect area in patients without bulging and/or recurrence at five year after surgery was 61.48 ± 68.39 cm2, while in patients with bulging and/or recurrence was 78.38 ± 77.61 cm2 (p = 0.153) (Table 3). After surgery, in patients with postoperative PCD failure, the mean distance between rectus muscles at CT scan at 1 and 12 months was 2.49 ± 1.32 cm (range of 0.5–5.5) and 5.64 ± 2.75 cm (range of 1.36–10.46), respectively (Table 4). Most of the PCD failures occurred 12 months after surgery (12 bulgings and 4 recurrences), not increasing significantly at five years follow-up (15 bulgings and 5 recurrences) (p = 0.547) (Table 4).
A statistical analysis was performed to identify the risk factors responsible for PCD failure, five years after surgery. Chronic obstructive pulmonary disease (COPD) was the only risk factor related to the failure (p = 0.029), while the others considered risk factors such as gender (p = 0.396), age (p = 0.112), BMI (p = 0.373), diabetes (p = 0.736), smoke habits (p = 0.483), primary or incisional hernia (p = 1.000), and the ratio defect width/transverse abdominal axis (p = 0.670) did not achieve a statistically significance difference.
After surgery, two abdominal wall hematomas (3.4%) treated conservatively (Clavien–Dindo I), and two acute incarceration of an interstitial hernia (3.4%), at the 12 mm trocar site, treated surgically (Clavien–Dindo III-b), occurred (Table 4). The interstitial hernias occurred in the first 15 cases, and for this reason Weck EFx Endo Fascial Closure System (Teleflex Incorporated, Wayne, Pennsylvania, USA) for the closure of all the abdominal wall layers was adopted. One month after surgery, clinical seroma, type II or more, occurred in eight patients (13.8%). Seroma did not occur at five years follow-up (Table 4).
In five patients with COPD, two seroma type 0a, one type 1, one type 2a, and one type 2b occurred. Only in patient with seroma type 1, PCD failure was not observed.
1 month after surgery, a reduction of the number of patients with pain and of the mean VAS score was observed (Table 4, Fig. 1). At 5 years, four patients (6.9%) with chronic pain related to specific movement were treated with conventional analgesics.
Discussion
This study was conducted to report postoperative outcomes after LVHR with PCD (IPOM plus) in terms of bulging and recurrence rates up to 5 years follow-up and to report postoperative complications and seroma. We hypothesized that the defect closure could create midline tension and consequently increase postoperative pain, and for this reason we added pain evaluation.
According to our protocol, patients with abdominal wall defect width less than 3 cm underwent open repair and therefore they were excluded from the study. Patients with lateral hernias were excluded to obtain a homogeneous sample of patients. Most of the bulgings or recurrences were observed one year after surgery, suggesting that the risk of failure after PCD could be related to the midline tension created during surgery. Even if not statistically significant, mean defect width, length, and area were greater in patients with bulging or recurrence after surgery in comparison to patients without PCD failure. The outcomes obtained are similar, although slightly worse, to those obtained with IPOM plus in literature [7, 8, 14,15,16,17].
Several studies analyze the risk factors related to recurrence, concluding that smoke habits, COPD, BMI, or incisional hernia are involved in developing of failure after ventral hernia repair [18]. Baker et al. reported that the recurrence rate after the closure of defect is related to mesh overlap and the fixation type, being less frequent with permanent fixation [19]. It is also reported an increase of recurrence rate with absorbable tacks in case of conventional IPOM [4, 20]. Hauters et al. concluded that the only factor with a statistically significant impact on recurrence is the mesh-defect size ratio, being important mesh overlap in case of PCD [21]. In our series, nevertheless, an adequate mesh overlap over the PCD was always achieved and meshes were fixed with permanent tackers.
Seroma is responsible for discomfort and/or pain in up to 35% of patients and reoperation for infection or recurrence is required in some cases, for this reason several options have been reported to reduce its incidence [14, 22]. PCD is described as an option to avoid seroma, since in 2007 Chelala et al. first described this technique reporting a low postoperative incidence (2%) [23]. However, other authors reported further advantages of PCD as the abdominal midline reconstruction improving its functionality and patients’ quality of life and decreased postoperative seroma and bulging rates [24,25,26,27].
Nguyen et al. in their systematic review, reported a reduction in seroma and recurrence rates from 11.4% to 0 and from 7.7% to 0, respectively, in favor of PCD [15]. In 2016, was introduced the concept that the midline tension created after defect closure could increase postoperative pain and recurrence rates [28]. Tandon et al. in their meta-analysis, reported that the defect closure is safe when hernia width is smaller than 6 cm, and that it is not possible to draw definitive recommendations in case of defects between 6 and 10 cm in width [28, 29]. Moreover, they concluded that, in case of defects more than 10 cm in width, other surgical techniques, such as component separation, are required to reduce the midline tension [28, 29]. According to Christoffersen et al. a reduction of postoperative seroma and recurrence rates were observed when the midline is closed, due to the reduction of the sac dead space but showing an increase of pain and the surgical response to stress [30].
The recurrence and bulging rates (8.6% and 25.9%, respectively) observed in this study are slightly higher if compared to the literature [7, 8, 15,16,17, 20, 23, 25, 28, 31]. However, for the purpose of the present study, all patients underwent CT scan one month and one year after surgery, and this could be responsible for the higher failure rate diagnosed. Moreover, it is also important to underline that, in the present series, the mean abdominal wall defect size (66.72 ± 71.13 cm2) and follow-up (60 months) are greater if compared to the literature [7, 8, 15,16,17, 20, 23, 25, 28, 31]. In fact, to the best of our knowledge, only three articles, concerning the IPOM plus, report data about abdominal wall defect size greater than that reported in our study, but with shorter follow-up [25, 27, 31].
Also the role of hernia sac, may have influenced our results [7, 23,24,25, 27, 28, 31,32,33,34]. Some authors do not resect the hernia sac [7, 23,24,25, 27, 28, 32, 34], while others advocated the necessity of sac resection to decrease seroma, recurrence, and bulging rates [31, 33]. However, further studies with longer follow-up are necessary to confirm their data, and the present study ended before this evidence [33].
A further technical aspect to consider is the use of a long-term absorbable double-loop suture in polyglyconate. It is reported as polyglyconate suture loses half of its strength at 8 weeks after surgery [35], leading that the use of non-absorbable sutures could improve both bulging and recurrence rates. However, further studies are required investigating about the best suture material.
Lastly, as reported for the midline closure after elective abdominal surgery, suture with small tissues bites (less than 5 mm) may result in reduced failure rate [36], also in case ventral hernia repair with PCD; however, this data should be confirmed by further prospective studies.
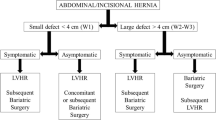
We agree to the literature, that the direct closure of the defect should not be performed in case of defect width of more than 10 cm (W3 according to the EHS classification) due to the tension generates in the midline [28, 29]. These defects would be candidates for techniques such as component separation [28, 29]. Based on the literature, patients with defect width of less than 10 cm would be candidate for a PCD, but results observed in the present series suggest choosing other strategies [7, 8, 15,16,17, 20, 23,24,25, 27, 28, 31, 33]. In case of large primary or incisional W2 hernias (according to the EHS classification), there is an increased risk of failure, so in our opinion, it would be indicated to perform techniques that reduce the midline tension, especially in those patients with risk factors responsible for recurrence. However, PCD is suggested in case of defect width of less than 4 cm (W1 or small-medium primary hernia according to the EHS classification). So as a conclusion, we can state that the IPOM plus is a valid technique, but its efficacy could be affected in case of hernia width larger than 6 cm [8, 28].
For this reason, based on our experience with IPOM plus, in cases of defects between 5 and 10 cm, our group proposed the laparoscopic intracorporeal rectus aponeuroplasty (LIRA) technique, with the aim to reduce the midline tension and postoperative bulging and recurrence rates [37]. Other authors, with the same objective, proposed the endoscopic totally extraperitoneal technique (eTEP), which, beyond the encouraging results obtained, has the advantage to avoid the use of intraperitoneal mesh [38].
The main limitations of the present study are the small sample of patients, the inclusion of both primary and incisional hernia, the lack of the upper limit of hernia defect and of a control group treated with standard IPOM technique. An analysis of meshes behaves was not performed due to the prevalence of ePTFE use and the small sample size.
In conclusions, based on the present study, LVHR has evolved toward a minimally abdominal wall reconstruction to improve its functionality (IPOM plus). PCDt might be considered a reliable technique even if it is important to note that medium-large defect (width ≥ 5 cm) associated with some risk factors could negatively influence the closure integrity. Since the majority PCD failure is observed within 12 months after surgery, the recurrence/bulging mechanism may be related to the surgical technique, due to the tension created and the lack of the healing process at the linea alba, when joining both fibrous edges of the hernia defect. This condition could be related to the higher rate of bulging. For this reason, alternative surgical techniques should be considered in these cases.
References
LeBlanc KA, Booth WV (1993) Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. Surg Laparosc Endosc 3(1):39–41
Van Hoef S, Tollens T (2019) Primary non-complicated midline ventral hernia: is laparoscopic IPOM still a reasonable approach? Hernia 23(5):915–925. https://doi.org/10.1007/s10029-019-02031-6
Susmallian S, Gewurtz G, Ezri T, Charuzi I (2001) Seroma after laparoscopic repair of hernia with PTFE patch: is it really a complication? Hernia 5(3):139–141. https://doi.org/10.1007/s100290100021
Bittner R, Bain K, Bansal VK, Berrevoet F, Bingener-Casey J, Chen D, Chen J, Chowbey P, Dietz UA, de Beaux A, Ferzli G, Fortelny R, Hoffmann H, Iskander M, Ji Z, Jorgensen LN, Khullar R, Kirchhoff P, Köckerling F, Kukleta J, LeBlanc K, Li J, Lomanto D, Mayer F, Meytes V, Misra M, Morales-Conde S, Niebuhr H, Radvinsky D, Ramshaw B, Ranev D, Reinpold W, Sharma A, Schrittwieser R, Stechemesser B, Sutedja B, Tang J, Warren J, Weyhe D, Wiegering A, Woeste G, Yao Q (2019) Update of Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS))-Part A. Surg Endosc 33(10):3069–3139. https://doi.org/10.1007/s00464-019-06907-7
Chelala E, Gaede F, Douillez V, Dessily M, Alle JL (2003) The suturing concept for laparoscopic mesh fixation in ventral and incisional hernias: preliminary results. Hernia 7(4):191–196. https://doi.org/10.1007/s10029-003-0143-z
Mitura K, Skolimowska-Rzewuska M, Garnysz K (2017) Outcomes of bridging versus mesh augmentation in laparoscopic repair of small and medium midline ventral hernias. Surg Endosc 31(1):382–388. https://doi.org/10.1007/s00464-016-4984-9
Suwa K, Okamoto T, Yanaga K (2016) Closure versus non-closure of fascial defects in laparoscopic ventral and incisional hernia repairs: a review of the literature. Surg Today 46(7):764–773. https://doi.org/10.1007/s00595-015-1219-y
Wennergren JE, Askenasy EP, Greenberg JA, Holihan J, Keith J, Liang MK, Martindale RG, Trott S, Plymale M, Roth JS (2016) Laparoscopic ventral hernia repair with primary fascial closure versus bridged repair: a risk-adjusted comparative study. Surg Endosc 30(8):3231–3238. https://doi.org/10.1007/s00464-015-4644-5
Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E, Dietz UA, Eker HH, El Nakadi I, Hauters P, Hidalgo Pascual M, Hoeferlin A, Klinge U, Montgomery A, Simmermacher RK, Simons MP, Smietański M, Sommeling C, Tollens T, Vierendeels T, Kingsnorth A (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13(4):407–414. https://doi.org/10.1007/s10029-009-0518-x
Morales-Conde S, Cadet H, Cano A, Bustos M, Martín J, Morales-Mendez S (2005) Laparoscopic ventral hernia repair without sutures–double crown technique: our experience after 140 cases with a mean follow-up of 40 months. Int Surg 90(3 Suppl):S56-62
Morales-Conde S, Balla A, Alarcón I, Sánchez-Ramírez M (2020) Minimally invasive repair of ventral hernia with one third of tackers and fibrin glue: less pain and same recurrence rate. Minerva Chir 75(5):292–297. https://doi.org/10.23736/S0026-4733.20.08468-0
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196
Morales-Conde S (2012) A new classification for seroma after laparoscopic ventral hernia repair. Hernia 16(3):261–267. https://doi.org/10.1007/s10029-012-0911-8
Morales-Conde S, Suárez-Artacho G, Socas M, Barranco A (2013) Influence of fibrin sealant in preventing postoperative seroma and normalizing the abdominal wall after laparoscopic repair of ventral hernia. Surg Endosc 27(9):3214–3219. https://doi.org/10.1007/s00464-013-2894-7
Nguyen DH, Nguyen MT, Askenasy EP, Kao LS, Liang MK (2014) Primary fascial closure with laparoscopic ventral hernia repair: systematic review. World J Surg 38(12):3097–3104. https://doi.org/10.1007/s00268-014-2722-9
Wiessner R, Vorwerk T, Tolla-Jensen C, Gehring A (2017) Continuous laparoscopic closure of the linea alba with barbed sutures combined with laparoscopic mesh implantation (IPOM Plus Repair) as a new technique for treatment of abdominal hernias. Front Surg 4:62. https://doi.org/10.3389/fsurg.2017.00062
Bernardi K, Olavarria OA, Holihan JL, Kao LS, Ko TC, Roth JS, Tsuda S, Vaziri K, Liang MK (2020) Primary fascial closure during laparoscopic ventral hernia repair improves patient quality of life: a multicenter, blinded randomized controlled trial. Ann Surg 271(3):434–439. https://doi.org/10.1097/SLA.0000000000003505
Holihan JL, Li LT, Askenasy EP, Greenberg JA, Keith JN, Martindale RG, Roth JS, Liang MK, Ventral Hernia Outcomes Collaborative (2016) Analysis of model development strategies: predicting ventral hernia recurrence. J Surg Res 206(1):159–167. https://doi.org/10.1016/j.jss.2016.07.042
Baker JJ, Öberg S, Andresen K, Rosenberg J (2018) Decreased re-operation rate for recurrence after defect closure in laparoscopic ventral hernia repair with a permanent tack fixated mesh: a nationwide cohort study. Hernia 22(4):577–584. https://doi.org/10.1007/s10029-018-1776-2
Christoffersen MW, Brandt E, Helgstrand F, Westen M, Rosenberg J, Kehlet H, Strandfelt P, Bisgaard T (2015) Recurrence rate after absorbable tack fixation of mesh in laparoscopic incisional hernia repair. Br J Surg 102(5):541–547. https://doi.org/10.1002/bjs.9750
Hauters P, Desmet J, Gherardi D, Dewaele S, Poilvache H, Malvaux P (2017) Assessment of predictive factors for recurrence in laparoscopic ventral hernia repair using a bridging technique. Surg Endosc 31(9):3656–3663. https://doi.org/10.1007/s00464-016-5401-0
Morales-Conde S, Gómez-Menchero J, Alarcón I, Balla A (2020) Retroprosthetic seroma after laparoscopic ventral hernia repair is related to mesh used? J Laparoendosc Adv Surg Tech A 30(3):241–245. https://doi.org/10.1089/lap.2019.0646
Chelala E, Thoma M, Tatete B, Lemye AC, Dessily M, Alle JL (2007) The suturing concept for laparoscopic mesh fixation in ventral and incisional hernia repair: Mid-term analysis of 400 cases. Surg Endosc 21(3):391–395. https://doi.org/10.1007/s00464-006-9014-x
Clapp ML, Hicks SC, Awad SS, Liang MK (2013) Trans-cutaneous Closure of Central Defects (TCCD) in laparoscopic ventral hernia repairs (LVHR). World J Surg 37(1):42–51. https://doi.org/10.1007/s00268-012-1810-y
Palanivelu C, Jani KV, Senthilnathan P, Parthasarathi R, Madhankumar MV, Malladi VK (2007) Laparoscopic sutured closure with mesh reinforcement of incisional hernias. Hernia 11(3):223–228. https://doi.org/10.1007/s10029-007-0200-0
Agarwal BB, Agarwal S, Mahajan KC (2009) Laparoscopic ventral hernia repair: innovative anatomical closure, mesh insertion without 10-mm transmyofascial port, and atraumatic mesh fixation: a preliminary experience of a new technique. Surg Endosc 23(4):900–905. https://doi.org/10.1007/s00464-008-0159-7
Orenstein SB, Dumeer JL, Monteagudo J, Poi MJ, Novitsky YW (2011) Outcomes of laparoscopic ventral hernia repair with routine defect closure using “shoelacing” technique. Surg Endosc 25(5):1452–1457. https://doi.org/10.1007/s00464-010-1413-3
Tandon A, Pathak S, Lyons NJ, Nunes QM, Daniels IR, Smart NJ (2016) Meta-analysis of closure of the fascial defect during laparoscopic incisional and ventral hernia repair. Br J Surg 103(12):1598–1607. https://doi.org/10.1002/bjs.10268
Balla A, Alarcón I, Morales-Conde S (2020) Minimally invasive component separation technique for large ventral hernia: which is the best choice? A systematic literature review. Surg Endosc 34(1):14–30. https://doi.org/10.1007/s00464-019-07156-4
Christoffersen MW, Westen M, Rosenberg J, Helgstrand F, Bisgaard T (2020) Closure of the fascial defect during laparoscopic umbilical hernia repair: a randomized clinical trial. Br J Surg 107(3):200–208. https://doi.org/10.1002/bjs.11490
Palanivelu C, Rangarajan M, Parthasarathi R, Madankumar MV, Senthilkumar K (2008) Laparoscopic repair of suprapubic incisional hernias: suturing and intraperitoneal composite mesh onlay. A retrospective study. Hernia 12(3):251–256. https://doi.org/10.1007/s10029-008-0337-5
Martin-Del-Campo LA, Miller HJ, Elliott HL, Novitsky YW (2018) Laparoscopic ventral hernia repair with and without defect closure: comparative analysis of a single-institution experience with 783 patients. Hernia 22(6):1061–1065. https://doi.org/10.1007/s10029-018-1812-2
Ahonen-Siirtola M, Nevala T, Vironen J, Kössi J, Pinta T, Niemeläinen S, Keränen U, Ward J, Vento P, Karvonen J, Ohtonen P, Mäkelä J, Rautio T (2018) Laparoscopic versus hybrid approach for treatment of incisional ventral hernia: a prospective randomized multicenter study of 1-month follow-up results. Hernia 22(6):1015–1022. https://doi.org/10.1007/s10029-018-1784-2
Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, Köckerling F, Kukleta J, Leblanc K, Lomanto D, Misra MC, Bansal VK, Morales-Conde S, Ramshaw B, Reinpold W, Rim S, Rohr M, Schrittwieser R, Simon T, Smietanski M, Stechemesser B, Timoney M, Chowbey P, International Endohernia Society (IEHS) (2014) Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS)-part 1. Surg Endosc 28(1):2–29. https://doi.org/10.1007/s00464-013-3170-6
Mäkelä P, Pohjonen T, Törmälä P, Waris T, Ashammakhi N (2002) Strength retention properties of self-reinforced poly L-lactide (SR-PLLA) sutures compared with polyglyconate (Maxon) and polydioxanone (PDS) sutures. An in vitro study. Biomaterials 23(12):2587–2592. https://doi.org/10.1016/s0142-9612(01)00396-9
Deerenberg EB, Harlaar JJ, Steyerberg EW, Lont HE, van Doorn HC, Heisterkamp J, Wijnhoven BP, Schouten WR, Cense HA, Stockmann HB, Berends FJ, Dijkhuizen FPH, Dwarkasing RS, Jairam AP, van Ramshorst GH, Kleinrensink GJ, Jeekel J, Lange JF (2015) Small bites versus large bites for closure of abdominal midline incisions (STITCH): a double-blind, multicentre, randomised controlled trial. Lancet 386(10000):1254–1260. https://doi.org/10.1016/S0140-6736(15)60459-7
Gómez-Menchero J, Guadalajara Jurado JF, Suárez Grau JM, Bellido Luque JA, García Moreno JL, Alarcón Del Agua I, Morales-Conde S (2018) Laparoscopic intracorporeal rectus aponeuroplasty (LIRA technique): a step forward in minimally invasive abdominal wall reconstruction for ventral hernia repair (LVHR). Surg Endosc 32(8):3502–3508. https://doi.org/10.1007/s00464-018-6070-y
Bellido Luque J, Gomez Rosado JC, Bellido Luque A, Gomez Menchero J, Suarez Grau JM, Sanchez Matamoros I, Nogales Muñoz A, Oliva Mompeán F, Morales Conde S (2021) Endoscopic retromuscular technique (eTEP) vs conventional laparoscopic ventral or incisional hernia repair with defect closure (IPOM +) for midline hernias. A case-control study. Hernia 25(4):1061–1070. https://doi.org/10.1007/s10029-021-02373-0
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Julio Gómez-Menchero, Andrea Balla, Ana Fernández Carazo, and Salvador Morales-Conde have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gómez-Menchero, J., Balla, A., Fernández Carazo, A. et al. Primary closure of the midline abdominal wall defect during laparoscopic ventral hernia repair: analysis of risk factors for failure and outcomes at 5 years follow-up. Surg Endosc 36, 9064–9071 (2022). https://doi.org/10.1007/s00464-022-09374-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09374-9