Abstract
Purpose
This study aimed at clinical results in terms of postoperative pain and functional recovery of new technique (eTEP) compared to IPOM + for ventral/incisional midline hernias. Recurrence rate, intra/postoperative complications and aesthetic results are secondary aims.
Methods
Data from consecutive patients requiring minimally invasive hernia repair were collected. From January 2015 to September 2018, patients with midline ventral/incisional hernias underwent IPOM + were compared to patients underwent eTEP procedure from October 2018 to December 2019 in a case/control study.
Results
Thirty-nine patients in IPOM + group and 40 in eTEP group were included. No significant differences were identified when hernias types, mean defect area, mean mesh area and intraoperative/postoperative complications (except seroma rate in favor of eTEP group) were compared. Operative time and hospital stay were significantly higher in eTEP group and IPOM + group, respectively. eTEP group showed significantly less pain on 1st, 7th and 30th postoperative days than IPOM + group. Restriction of activities was significantly decreased in eTEP group on the 30th and 180th day after surgery. Significant differences were observed in terms of cosmetic results 30th and 180th days after surgery in favor of eTEP group.
Average follow-up was 15 months in eTEP group and 28 months in IPOM + group. No recurrences were identified in eTEP group and one recurrence in IPOM + group with no significant differences.
Conclusion
Endoscopic retromuscular technique shows significant lower postoperative pain, better functional recovery and cosmesis than IPOM + without differences in intra/postoperative complications (except seroma rate) or recurrences during the follow-up. eTEP requires longer operative time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The introduction of minimally invasive surgery in the early 1990s enabled the possibility of laparoscopic ventral or incisional hernia repair in 1993 [1]. Recent studies have shown that minimally invasive surgery in ventral or incisional hernias is superior to open repair, as it results in reduced blood loss, fewer perioperative complications, and shorter hospital stays [2, 3]. Nevertheless, the laparoscopic technique (lap IPOM) requires traumatic fixation of an intra-abdominal mesh (transabdominal sutures or tackers) and this can lead to several postoperative complications, such as high postoperative pain or fibrous adhesions [4].
The Rives-Stoppa surgical technique, with retromuscular mesh placement, has become a widespread approach for open ventral hernia repair. This is because this approach is associated with low rates of surgical-site infections and recurrence in long-term follow-up [5,6,7]. It also achieves a restoration of the abdominal wall functionality, minimises intra-abdominal complications due to the mesh being placed outside the intra-abdominal cavity, thus avoiding complications that this entails and without generating for future abdominal surgeries [6, 7].
In recent years, some researchers have attempted to use an extraperitoneal approach in ventral or incisional hernia repairs through minimally invasive surgery. Examples of these surgical techniques are as follows:
-
Laparoscopic transabdominal pre-peritoneal access [8, 9]. Here, the pre-peritoneal space is developed laparoscopically and the mesh is placed between the posterior rectus sheaths and peritoneum.
-
Laparoscopic transabdominal retromuscular technique [10,11,12]. Here, the peritoneum and posterior rectus sheath are incised, and a retromuscular space is created. The mesh is extended between the rectus muscle and the posterior rectus sheath.
-
Totally endoscopic retromuscular technique (eTEP) [13, 14]. This access is based on the eTEP technique for inguinal hernias [15].
The present study aimed to assess clinical results, in terms of postoperative pain and functional recovery, of a new minimally invasive surgical technique (eTEP) compared to conventional laparoscopic intraperitoneal mesh placement with defect closure (IPOM +) for ventral or incisional midline hernias. Secondary aims of the study were to understand the recurrence rates, intra- and postoperative complications, and aesthetic results associated with each technique.
Patients and methods
Study design and population
Data from consecutive patients requiring minimally invasive ventral hernia repair were collected from January 2015 to December 2019, from two Spainish centres (Virgen Macarena and Quironsalud Sagrado Corazón Hospitals in Seville, Spain.). Data were entered into a prospectively maintained database and retrospectively analysed. The local institutional review board approved the study.
The distribution of IPOM + or eTEP approaches were studied and grouped according to different time. From January 2015 to September 2018, patients with midline ventral or incisional hernias underwent IPOM + (Control group). From October 2018 to December 2019, patients with midline ventral or incisional hernias underwent the eTEP procedure (Case group). The outcomes of patients who underwent surgery using the eTEP approach were compared with those of patients who had hernia repairs using the conventional IPOM + approach.
The inclusion criteria were as follows:
-
Patients aged between 18 and 80 years old.
-
Midline ventral or incisional hernias less than 8 cm width, with or without rectus diastasis > 2 cm in size.
The exclusion criteria were as follows:
-
Previous mesh placed in retromuscular or intra-abdominal position.
-
Patients with contraindication for general anaesthesia.
-
Incarcerated or strangulated hernias.
Surgical techniques
All the procedures were performed by the same surgeon. Patients were placed in a supine position with both arms lying by their sides. The surgical team stood on the left side of the patient. Two grams of cefuroxime was administered as standard antibiotic prophylaxis during the induction of anaesthesia.
IPOM + technique
A pneumoperitoneum was created using a Veress needle in the left hypochondrium. Trocars were placed on the left side of the abdomen on the left clavicular midline. Three trocars were used: one 10 mm trocar for the 30° optic, and two 5 mm trocars.
Once a pneumoperitoneum had been created, the working pressure was maintained at 14 mm Hg. Adhesiolysis was performed and hernia content was reduced to expose the hernia defect, which was measured using a spinal needle placed through the skin. For this, the pneumoperitoneum working pressure was decreased to 8 mm Hg to reduce hernia size overestimation. The defect closure was performed with non-absorbable, continuous barbed suture (V-Loc™ nº0, Medtronic) (Fig. 1). In patients with rectus diastasis > 2 cm in size, both posterior rectus sheaths were re-approximated with the defect closure, using the same running suture.
A PTFE-c mesh (Omyra® mesh, B. Braun) was used. The mesh size depended on the radius of the defect and rectus diastasis. The radius of the mesh was four times the radius of the defect (including the associated diastasis) in the horizontal and vertical axis. Non-absorbable, helicoidal sutures placed at 3 cm intervals were used for mesh fixation (Protack™, Medtronic) in a double-crown fashion (Fig. 2).
The evacuation of the pneumoperitoneum and the trocar removal was done under direct vision. The 10 mm trocar incision was closed using a 2/0 absorbable suture.
eTEP technique
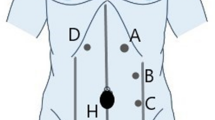
A 2 cm incision was made below the left costal margin and the left anterior rectus sheath was exposed (Fig. 3). This layer was incised as close to lateral edge as possible. A retromuscular space was created using blunt dissection (Fig. 4). One 10 mm balloon trocar was placed for the 30° optic and the retromuscular space was developed using the optic tip and pneumodissection with a pressure of 14 mm Hg (Fig. 5). One 5 mm trocar and one 10 mm trocar were inserted in the left iliac fossa and left hypocondrium, respectively, and a complete left retrorectus space was achieved. The decision where to crossover depends on the defect location. For upper midline defects, the crossover was performed below the level of the umbilicus, developing the contralateral pre-peritoneal and retrorectus spaces in the caudal to cephalad direction. The hernia sac was completely reduced, thereby connecting both right and left retrorectus spaces. However, for lower midline defects, the crossover was developed above the level of the umbilicus (Fig. 6). Once the medial aspect of the left posterior rectus sheath was incised, pre-peritoneal dissection was performed, superficial to the falciform ligament. The right posterior rectus sheath was identified and its medial aspect was incised and released in the cephalad to caudal direction (Fig. 7). The hernia sac was reduced and the upper portion of the right retrorectus space was connected with the lower part of it, completely releasing both right and left retrorectus and pre-peritoneal spaces (Figs. 8, 9).
Once both retrorectus spaces were developed, the hernia defect was measured and the posterior rectus sheaths were re-approximated to the midline. Using a non-absorbable, running barbed suture (V-loc™ nº0, Medtronic), the hernia defect was repaired and the posterior rectus sheaths re-joined (Fig. 10). In case of excessive tension in the midline, both posterior rectus sheaths were kept in place and the peritoneal tears were closed to avoid contact with the intra-abdominal contents. The anterior rectus sheaths were then brought to the midline in an attempt to reconstruct the original midline, using the same suture (Fig. 11).
The developed retrorectus space was measured (length and width) with a rule to use the adequate mesh size to cover it completely. Two different meshes were used. The first type was low-weight polypropylene mesh (Optilene® Mesh elastic, B. Braun). This mesh was rolled and inserted through the 10-mm trocar. The mesh was then properly extended to cover the retrorectus space completely. Cyanocrylate glue (Histoacryl®, B. Braun) was used for mesh fixation (Fig. 12). The other type of mesh was self-adhesive mesh (Parietex Progrip®, Medtronic). This mesh was rolled on its plastic cover to prevent adhesion during placement. Once extended with the grips upwards, the plastic cover was removed and extracted through the 10 mm trocar. The mesh was immediately fixed to the rectus muscles when the pneumoperitoneum was removed. No extra fixation was used. The self-adhesive mesh was used once experience in retromuscular dissection and mesh placement was gained from the first 20 cases.
Once either mesh was properly extended, a suction drain was routinely placed. This drain was removed after 24 h if there was no bleeding. The evacuation of pneumoperitoneum and trocar removal was performed under direct vision. The 10 mm trocar incisions were closed using 2/0 absorbable suture.
In both eTEP and IPOM + groups, an abdominal binder was recommended for 3 months after surgery to reduce seroma formation.
Study outcomes
We aimed to test the hypothesis that the eTEP approach decreases postoperative pain in comparison to the IPOM + procedure, in a homogeneous cohort of patients requiring laparoscopic ventral or incisional hernia repair.
Variables
For each patient, retrospectively, the following demographic, perioperative and postoperative data were collected:
-
Demographics—age, body mass index (BMI), and previous risk factors for hernia recurrence (smoking, immunosuppression, hepatopathy, renal failure, liver disease).
-
Hernia type—The European hernia classification for ventral and incisional hernias was used [16].
The perioperative results collected were as follows:
-
The defect area (cm2).
-
The mesh area used (cm2).
-
The operation time (minutes).
-
Intraoperative complications and conversion to open surgery.
The postoperative results collected were as follows:
-
Length of hospital stay (days).
-
Whether or not patients were readmitted and, if so, the reason for readmission and reoperation.
-
Information on postoperative complications (Clavien–Dindo classification [17]). Seroma was identified by clinical examination and computed tomography (CT) one month after the operation. The seroma classification in laparoscopic ventral hernia repair was used (Morales et al. [18]). Information regarding wound infections, periumbilical skin necrosis and complications was also collected.
-
Postoperative pain. Eurahs quality-of-life (EuraHS-QoL) score for pain [19]) was measured using the Visual Analog Scale (VAS) from 0 (no pain) to 10 (worst pain imaginable). Pain was graded at rest, during activities and during the last week at the site of the hernia, before surgery and on the 1st, 7th, 30th and 90th day after surgery. Pain lasting more than 90 days and requiring medication or intervention was considered chronic pain.
-
Functional recovery post surgery was measured using EuraHS-QoL score for restriction [19], which assesses restriction from daily activities, outside the house, during sport or during heavy labour because of pain or discomfort at the site of the hernia. It was graded using a scale of 0 (no restriction) to 10 (completely restricted) before surgery, then on the 30th and 180th day after surgery.
-
The cosmetic outcome of surgery was measured using EuraHS-QoL score for cosmesis [19]. The shape of the abdomen at the site of the hernia was measured from 0 (very beautiful) to 10 (extremely ugly) before surgery, then on the 30th and 180th day after surgery.
-
Hernia recurrence was assessed by clinical examination at 1 month, 6 months and 1 year postoperatively. At the 1-month and 1-year examinations, CT scans were also performed. After the first postoperative year, patients were reviewed annually.
Statistical analysis
Statistical analyses were performed using SPSS Statistics, version 25.0 for Macintosh (IBM Corp, Armonk, NY). Continuous variables were described as means with standard deviation (SD), and categorical variables were reported as absolute or relative frequencies. Continuous variables were compared using nonparametric tests (Mann–Whitney U and Wilcoxon tests). The Chi-square test was used to evaluate categorical data. Reported p values of < 0.05 were considered statistically significant.
Results
Of the 86 eligible patients, 51 were men and 35 were women. During follow-up, 7 patients were lost. In the final, case–control study, 79 patients were included, with 39 in the IPOM + group (control group) and 40 patients in eTEP group (case group). Both groups were comparable regarding age, BMI and previous risk factors for recurrence, with no differences.
No significant differences were identified when ventral or incisional hernias types were compared across the groups (Table 1). There were 21 patients with ventral hernias (53.8%), and 18 patients with incisional hernias (46.2%) in the eTEP group. There were 14 patients with ventral hernias (35%) and 26 patients with incisional hernias (65%) in IPOM + group. Similarly, no significant differences were identified when the mean defect area and mean mesh area were compared (Table 1). The mean defect width was 4.6 cm in the eTEP group and 5.2 cm in the IPOM + group, showing no significant difference (p = 0.1).
There was no need to convert to open surgery, and no intraoperative complications identified, in the eTEP group. However, two jejunal serosa tears after laparoscopic adhesiolysis, and one injury to the inferior epigastric vessels due to tackers fixation, were identified intraoperatively in the IPOM + group (3.8%). The serosal tears were solved using sero-serosa sutures and the epigastric bleeding was stopped using electrocautery. No significant differences were shown between both groups.
Operative time was significantly higher (p < 0.05) in the eTEP group (106.8 ± 20.5 min) than the IPOM + group (61.4 ± 18 min).
Regarding the length of hospital stay, significant differences were shown between the groups, In the eTEP group, the average stay was 1.3 ± 0.7 days (range 1–5 days) compared to 1.8 ± 0.7 days (range 1–5 days) in the IPOM + group (p < 0.05).
No differences were observed in terms of readmission and reoperation between both groups.
The postoperative complications observed were as follows:
-
One postoperative retrorectus haematoma (2.6%) in the eTEP group which required reoperation for haematoma removal (Clavien–Dindo grade IIIb).
Other complications (Clavien–Dindo grade 1):
-
Five patients experienced abdominal distention and vomiting in the IPOM + group (12.5%), were readmitted, and paretic ileus was diagnosed. With conservative treatment (no oral intake, nasogastric aspiration and proper hydration and nutrition), the ileus was solved in these 5 patients. No significant differences were shown (p = 0.2) between both groups.
-
Seroma was diagnosed in 4 patients in the eTEP group (10.3%) and 14 in the IPOM + group (35%) after one postoperative month, with significant differences (p = 0.01). All seromas were Type 1 when assessed by seroma classification and resolved three months after surgery. No specific treatment was required.
-
One limited umbilical burned skin was identified in eTEP group. The devitalised navel skin was removed and the wound was healed using a povidone iodine dressing.
-
No wound infections were identified during the follow-up period.
Regarding postoperative pain measured before surgery, then on the 1st, 7th, 30th and 90th day after surgery, no significant differences were observed when both groups were compared before surgery. eTEP group showed significantly less pain on 1st, 7th and 30th postoperative days than IPOM + group (p < 0.05). No significant differences were identified when 90th day postoperative pain was compared (Table 2). There were two patients in the IPOM + group that experienced pain after 90 days post-surgery that required medication, whereas there were none in the eTEP group.
In our study, evaluation of functional recovery (activity restrictions) demonstrated no significant differences between the IPOM + and eTEP groups preoperatively. Functional recovery was significantly improved in the eTEP group compared to the IPOM + group on the 30th and 180th day after surgery (Table 3 and Fig. 13). In the eTEP group, activity restrictions one month after surgery were significantly less than preoperative restrictions, and restrictions continued to decrease six months after surgery (Table 4). In the IPOM + group, activity restrictions one month after surgery were significantly higher than preoperative restrictions. However, 6 months after surgery, they were significantly lower than preoperative and one month postoperative surgery restrictions (Table 4).
Cosmetic results were compared preoperatively, then one and 6 months after surgery using Eurahs quality-of-life score for cosmesis. Significant differences were observed between the groups preoperatively, and on the 30th and 180th day after surgery, in favour of the eTEP group (p < 0.05) (Table 5).
The average follow-up was 15.9 ± 4.5 months in the eTEP group (range 11–24 months) and 28.3 ± 3.8 months in the IPOM + group (range 23–35 months). During the follow-up, no recurrences were identified in the eTEP group, but there was one recurrence in the IPOM + group (2.5%). This difference between groups was not significant.
Discussion
Since Leblanc et al. published the first report about laparoscopic techniques for repair of ventral or incisional hernias in 1993 [1], this minimally invasive surgery has been improved during recent years. Since Agarwal et al. [20] published the first paper on laparoscopic defect closure (DC) in 2009, this technique has become widespread. The DC performed in IPOM + shows different advantages when compared to defect bridging (no defect closure):
-
Pseudohernia or prosthetic hernia. This occurs when the mesh protrudes through the hernia defect. This effect disappears by closing the hernia hole and the patient reports greater stability of the abdominal wall when exerting themselves [21].
-
Decreased dead space between the hernia sac and mesh. The DC achieves a significant reduction in the dead space and postoperative seroma rate is improved [21, 22].
-
Increased mesh-peritoneum contact surface area. When the defect is closed, the entire surface of the mesh placed intra-abdominally stays in contact with peritoneum and the mesh ingrowth is increased. Several studies have shown that this significantly reduces long-term hernia recurrence [23].
-
Full abdominal wall reconstruction. One of the main goals of hernia surgery is to reconstruct the original abdominal wall anatomy. When hernia DC is performed, both rectus muscles are placed in their original position, achieving an abdominal wall functionality improvement [23].
The main drawback regarding DC in the IPOM + technique is the excessive tension that can be generated in the midline, depending on the hernia size. This issue could be the reason that postoperative acute and chronic pain is increased when the IPOM + technique is used rather than defect bridging [24]. In their meta-analysis published in 2016, Tandon et al. showed that defects < 6 cm in width could be safely closed without increasing postoperative pain or recurrences, when compared to conventional laparoscopic ventral hernia repair [25].
Other limitations in the IPOM + technique are as follows:
-
Intraperitoneal mesh placement: the placement of the mesh intraperitoneally means that is in intimate contact with the loops; therefore, there is an associated risk of adhesions and fistulae [26, 27]. If meshes coated with anti-adhesive barriers are used, the incidence of these complications is reduced, but even so, the risk of adhesions and fistulae persists.
-
Traumatic mesh fixation (helicoidal sutures) requires the use of traumatic devices (helicosutures) that can cause adhesions and are a non-negligible source of acute and chronic pain [26]. It has been found that the incidence of chronic pain related to the use of tackers ranges between 1.8% and 28% in some published series, indicating that they may cause long-term complications with difficult solutions [28].
The new eTEP technique tries to solve these previous disadvantages in a number of ways:
-
1.
Mesh is placed outside of the abdominal cavity, meaning there is no risk of adhesions or fistulae.
-
2.
Coated mesh is not necessary. Uncoated mesh could be used, decreasing costs of the procedure.
-
3.
The hernia defect is closed. When posterior and anterior layers are closed with a running suture, DC is performed with the advantages previously explained.
-
4.
Traumatic fixations are not needed. Placing the mesh in a retromuscular position achieves two important principles in ventral hernia surgery:
-
Diffusion of intra-abdominal pressure in each cm2 of the implanted mesh. This uniform distribution of intra-abdominal pressure ensures its immediate fixation to the abdominal wall with working pressure [29].
-
Since the placed mesh is covered on both sides (rectus muscle above and posterior rectus sheaths below), the prosthetic ingrowth will be increased when compared to intraperitoneal mesh placement [29].
-
In our trial, the operation time for the eTEP procedure is statistically longer than the IPOM + technique due to the learning curve regarding this new surgical procedure. Surgical time is shortened as experience is gained (Fig. 14).
Our study shows than the eTEP technique is less painful on the 1st, 7th and 30th days post surgery, with better functional recovery in terms of activity restrictions than IPOM + . The differences were significant. No traumatic fixations and DC without tension in the midline could explain the differences in terms of postoperative pain and activities restrictions.
Differences between both groups in term of hospital stay are probably caused by less post-operative pain and quicker functional recovery in the eTEP group when compared to IPOM + group.
Regarding postoperative complications, paretic ileus was only seen in the IPOM + group (12.5%). Extensive adhesiolysis and the size of prosthetic mesh in contact with loops, could explain this complication [30].
Postoperative seroma was diagnosed in 35% of patients in the IPOM + group in this study, higher than previously published in the literature [30]. The main reason that could explain this issue is that the hernia sac is not completely closed with the running suture and a small dead space above the closed defect is left. All seromas were solved with conservative treatment.
No significant differences regarding chronic pain were identified between both groups. The use of tackers fixation could be the reason for the chronic pain in two patients in the IPOM + group patients.
The eTEP technique improves cosmesis results. The shape of the abdomen and at the site of the hernia could be more damaged in control group. In the IPOM + group, patients complained of midline fatty tissue bulging after DC, increasing the cosmetic discomfort at the site of the midline hernia. Both anterior and posterior rectus sheaths were closed simultaneously during the DC. In eTEP group, the anterior and posterior rectus sheaths were brought to the midline in two planes using two running sutures, improving the distribution of midline fatty tissue.
This drawback and no hernia sac resection, could make cosmetic results worse in IPOM + group.
The main limitations of the study are as follows:
-
Small sample size and short follow-up.
-
Two surgical techniques were compared consecutively during two periods of time and no changes in perioperative care, anesthetic management or enhanced recovery protocols were performed. Patients in the eTEP group underwent surgery after patients in IPOM + group and, thus, could benefit from the previous experience gained in minimally invasive ventral hernia repair and complications.
Conclusion
The endoscopic retromuscular technique in ventral or incisional hernia repair (eTEP) shows significantly lower postoperative pain, better functional recovery and cosmesis than IPOM + . Additionally, there are no differences in intra- or postoperative complications (except seroma rate) or recurrences during the follow-up. However, eTEP requires longer operative time.
Data availability
Data are available in IBM SPSS Statistics Base version 25.0 tables and Microsoft excel 16.4.
References
LeBlanc KA, Booth WV (1993) Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. SurgLaparoscEndosc 3(1):39–41
Olmi S, Scaini A, Cesana GC, Erba L, Croce E (2007) Laparoscopic versus open incisional hernia repair: an open randomized controlled study. SurgEndosc 21(4):555–559
Misra MC, Bansal VK, Kulkarni MP, Pawar DK (2006) Comparison of laparoscopic and open repair of incisional and primary ventral hernia: results of a prospective randomized study. SurgEndosc 20(12):1839–1845
Beldi G, Wagner M, Bruegger LE, Kurmann A, Candinas D (2011) Mesh shrinkage and pain in laparoscopic ventral hernia repair: a randomized clinical trial comparing suture versus tack mesh fixation. SurgEndosc 25:749–755
Stoppa RE (1985) The treatment of complicated groin and incisional hernias. WJS 5:545–554
Novitsky YW, Porter JR, Rucho ZC, Getz SB, Pratt BL, Kercher KW et al (2006) Open preperitonealretrofascial mesh repair for multiply recurrent ventral incisional hernias. J Am CollSurg 203:283–289
Maman D, Greenwald D, Kreniske J, Royston A, Powers S, Bauer J (2012) Modified Rives-Stoppa technique for repair of complex incisional hernias in 59 patients. Ann PlastSurg 68:190–193
Miserez M, Penninckx F (2002) Endoscopic totally preperitoneal ventral hernia repair. SurgEndosc 16:1207–1213
BellidoLuque JA, BellidoLuque A, Gomez Menchero J, Suarez Grau JM, García Moreno J, Tejada Gomez A, Jurado G (2017) Safety and effectiveness of self-adhesive mesh in laparoscopic ventral hernia repair using transabdominal preperitoneal route. J SurgEndosc 31(3):1213–1218
Schroeder AD, Debus ES, Schroeder M, Reinpold WM (2013) Laparoscopic transperitonealsublay mesh repair: a new technique for the cure of ventral and incisional hernias. SurgEndosc 27:648–654
Schwarz J, Reinpold W, Bittner R (2017) Endoscopic mini/less open sublay technique (EMILOS)—a new technique for ventral hernia repair. Langenbecks Arch Surg 402:173–180
Nguyen DK, Chen DC (2017) Laparoendoscopic stapled Rives Stoppasublay technique for extraperitoneal ventral hernia repair. EurSurg 49:175–179
Belyansky I, Daes J, Radu VG, Balasubramanian R, Reza Zahiri H, Weltz AS, Sibia US, Park A, Novitsky Y (2018) A novel approach using the enhanced-view totally extraperitoneal(eTEP) technique for laparoscopic retromuscular hernia repair. SurgEndosc 32(3):1525–1532
Radu VG, Lica M (2019) The endoscopic retromuscular repair of ventral hernia: the eTEP technique and early results. Hernia 23(5):945–955
Daes J (2012) The enhanced view-totally extraperitoneal technique for repair of inguinal hernia. SurgEndosc 26:1187–1188
Muysoms FE et al (2009) Classification of primary and incisional abdomianal wall hernias. Hernia 13(4):407–414
Clavien PA, Barkun J et al (2009) Clavien-Dindo classification of surgical complications. Five-years of experience. Ann Surg 250(2):187–196
Morales-Conde S et al (2012) A new classification for seroma after laparoscopic ventral hernia repair. Hernia 16(3):261–267
Muysoms FE, Vanlander A, Ceulemans R, Kyle-Leinhase I, Michiels M, Jacobs I, Pletinckx P, Berrevoet F (2016) A prospective, multicenter, observational study on quality of life after laparoscopic inguinal hernia repair with ProGrip laparoscopic, self-fixating mesh according to the European Registry for Abdominal Wall Hernias Quality of Life Instrument. Surgery 160(5):1344–1357
Agarwal BB, Agarwal S, Mahajan KC (2009) Laparoscopic ventral hernia repair: innovative anatomical closure, mesh insertion without 10-mm transmyofascial port, and atraumatic mesh fixation: a preliminary experience of a new technique. SurgEndosc 23(4):900–905
Papanivelu C, Jani KV et al (2007) Laparoscopic sutured closure with mesh reinforcement of incisional hernia. Hernia 11:223–228
Suwa K, Okamoto T, Yanaga K (2016) Closure versus non-closure of fascial defects in laparoscopic ventral and incisional hernia repairs: a review of literature. Surg Today 46(7):764–773
Mitura K et al (2017) Outcomes of bridging versus mesh augmentation in laparoscopic repair of small an medium midline ventral hernias. Surgendosc 31:382–388
Wennergen JE, Askenasy EP, Greenberg JH, Holihan J, Keith J, Liang MK, Martindale RG, Trott S, Plymale M, Roth JS (2016) Laparoscopic ventral hernia repair with primary fascial closure vs. Bridged repair: a risk-adjusted comparative study. SurgEndosc 30:3231–3238
Tandon A, Pathak S, Lyons NJR, Nunes QM, Daniels IR, Smart NJ (2016) Meta-analysis of closure of the fascial defect during laparoscopic incisional and ventral hernia repair. BJS 103:1598–1607
Henniford BT, Park A, Ramshaw BJ, Woeller G (2003) Laparoscopic repair of ventral hernias: nine years experience with 850 consecutive cases. Ann Surg 238:391–400
Prasad P, Tantia O, Patle NM et al (2011) Laparoscopic ventral hernia repair: a comparative study of transabdominal preperitoneal versus intraperitoneal onlay mesh repair. J LaparoendoscAdvSurg Tech 21(6):477–483
Henniford BT et al (2016) Guidelines for laparoscopic ventral hernia repair. SurgEndosc 30(8):3161–3162
Prasad P et al (2011) Laparoscopic transabdominal preperitoneal repair of ventral hernia: a step towards physiological repair. Indian J Surg 73(6):403–408
Earle D, Roth JS, Saber A, Haggerty S et al (2016) SAGES guidelines for laparoscopic ventral hernia repair. SurgEndosc 30:3163–3183
Acknowledgement
This study complies with the current laws of Spain, in which it has been performed.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors Juan Bellido Luque, Juan Carlos Gomez Rosado, Araceli Bellido Luque, Julio Gomez Menchero, Juan Manuel Suarez Grau, Inmaculada Sanchez Matamoros, Angel Nogales Muñoz, Fernando Oliva Mompeán, Salvador Morales Conde declare that they have no conflict of interest. Conflict of interest is recorded in the potential conflict of interest disclosure forms.
Ethics approval
Approval was obtained from the ethics committee of University of Seville (Spain), Virgen de la Macarena Hospital. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data and photographs.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 191300 KB)
Rights and permissions
About this article
Cite this article
Bellido Luque, J., Gomez Rosado, J.C., Bellido Luque, A. et al. Endoscopic retromuscular technique (eTEP) vs conventional laparoscopic ventral or incisional hernia repair with defect closure (IPOM +) for midline hernias. A case–control study. Hernia 25, 1061–1070 (2021). https://doi.org/10.1007/s10029-021-02373-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-021-02373-0