Abstract
Background
Bridging of the hernia defect in laparoscopic repair (sIPOM) technique does not fully restore the abdominal wall function. Closure of hernia defect in IPOM-plus technique leads to the restoration of abdominal wall function and improved long-term treatment outcomes. Against the expectations, the studies confirm the formation of intraabdominal adhesions to the mesh. Regardless of the above, the search of the proper technique for mesh implantation and fixation is still ongoing. There have also been attempts to identify groups of patients who may still benefit from IPOM procedure.
Materials and methods
Patients with midline abdominal wall hernias up to 10 cm wide were enrolled in the study except for subxiphoid and suprapubic hernias. Between 2011 and 2014 we performed 82 hernia repairs using the laparoscopic technique with Physiomesh. Patients were divided into sIPOM and IPOM-plus groups. The study included 44M and 38F patients aged 27–84 years. After 12-months and again in August 2015 a survey was posted to all patients with questions regarding potential recurrence.
Results
After 12 months, eight patients (20 %) in sIPOM group reported subjectively perceived recurrence and none in IPOM-plus group (p = 0.002). Six patients (14.3 %) in sIPOM group reported suspected recurrence, as compared to three patients (7.1 %) in IPOM-plus group (p = 0.13). These patients were invited for a follow-up physical examination and sonography. Eventually, four cases of hernia recurrence were confirmed in sIPOM group (10 %) and none in IPOM-plus group (p = 0.018). Other patients presented with mesh bulging.
Conclusions
Laparoscopic ventral hernia repair is generally safe and is associated with the low recurrence rate. Closure of fascial defects before mesh insertion offers better treatment outcomes. Non-closure of fascial defects with only bridging of the hernia defect (sIPOM) causes more frequent recurrence and bulging. As a result, patient satisfaction with treatment is lower, and they are concerned about hernia recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Minimally invasive surgical techniques are continuously developing as a part of efforts, which aim at limiting the perioperative tissue damage. Laparoscopic ventral hernia repair led to the development of material which can be safely inserted within the abdominal wall in a direct contact with intraperitoneal organs [1, 2]. Unprocessed polypropylene or polyester integrates well into the abdominal wall. However, it can cause intestinal erosions or fistulas, lead to intestinal obstruction or hinder the access to peritoneal cavity in future [3–7]. At the same time, a smooth surface of polytetrafluoroethylene (PTFE) does not cause intestinal adhesions, but integrates poorly into the abdominal wall. This gave rise to further technological modifications aiming at development of a universal surgical material. The basic requirement for the perfect mesh used for the intraperitoneal onlay mesh hernia repair (IPOM) is being inert to intestinal surface, which limits the formation of intraperitoneal adhesions [8]. It is also essential that the connective tissue embed into the mesh properly ensuring sufficient long-term tensile strength caused by the intraabdominal pressure.
In order to achieve the discussed effect, contemporary polypropylene and polyester surgical meshes are coated with such anti-adhesives as poliglecaprone, hyaluronic acid, polyethylene glycol, collagen layer, oxidised regenerated cellulose, omega-3 fatty acids, silicone and titanium. Despite all initial hopes, this solution proved to have some disadvantages. Bridging of the hernia defect using standard laparoscopic intraperitoneal onlay mesh repair (sIPOM) technique does not fully restore the abdominal wall function and can cause bulging or seromas [9]. Lack of musculofascial support on the entire mesh surface and its insufficient mesh attachment in IPOM technique causes hernia recurrence and pain due to the increased tension at the implant fixing points [10]. On the other hand, closure of hernia defect in IPOM-plus technique leads to the restoration of abdominal wall function and improved long-term treatment outcomes [11, 12]. Against the expectations, the studies confirm the formation of intraabdominal adhesions to the mesh surface [13, 14]. The disappointment undermined the trust in some products used for IPOM procedures leading to the revival of the classic methods of hernia repair by retromuscular preperitoneal (sublay) mesh implantation [15, 16]. Regardless of the above, the search of the proper technique for mesh implantation and fixation is still ongoing. There have also been attempts to identify groups of patients who may still benefit from IPOM procedure.
The aim of our prospective, single-centre study was to compare two techniques of small and medium midline ventral hernia repair and to analyse early and long-term outcomes of the treatment involving the use of Physiomesh, a physiological tissue separation mesh with dual-side anti-adhesive coating, fixed with the dedicated Securestrap device.
Materials and methods
Patients
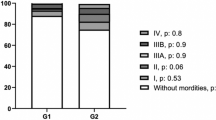
Patients with midline (M according to EHS classification) primary and incisional abdominal wall hernias up to 10 cm wide (W1–W3 according to EHS classification) were enrolled in the study [17]. Patients with subxiphoid and suprapubic hernias (M1 and M5) were excluded from the analysis. Between May 2011 and June 2014, we performed 82 hernia repair procedures using the laparoscopic intraperitoneal onlay mesh (IPOM) technique, which met the above criteria. The study cohort included 44 male and 38 female patients aged 27–84 years (mean age of 49.5; SD 13.7)—Table 1. Informed consent was obtained from all enrolled study participants.
Surgical technique
All procedures were performed by three surgeons who have expertise in laparoscopic techniques. Pneumoperitoneum was created with a Veress needle in the left subcostal region. The surgical technique involved the use of three trocars inserted near the left anterior axillary line—the optical 10 mm trocar at the umbilicus level, and two other inserted more medially 5 cm below and above the optical trocar. This trocar layout and the use of a laparoscope with 30o oblique optics ensured good visualisation of the surgical field and spatial triangulation, which enabled easy instrument and mesh manoeuvring. The intraperitoneal adhesions between the anterior abdominal wall and the greater omentum or intestine were removed. In patients with epigastric hernias, the round and the falciform ligaments of the liver were dissected. In patients with hypogastric hernias, the retromuscular space was dissected by pushing the bladder away. If abundant preperitoneal fat deposition was found, the peritoneum was removed with the adipose tissue so as to expose the smooth and even posterior fascial surface. It ensured a direct contact between the mesh and the fascia, which formed a “landing zone” promoting proper integration of synthetic material into the abdominal wall.
During the first 18 months of the study, the “bridging” technique of laparoscopic ventral hernia repair (sIPOM; standard, classical IPOM) was used, which involved intraperitoneal mesh placement without the closure of hernia defect. These 40 patients formed the sIPOM group. Afterwards, the surgical technique was changed, and hernia defect was closed using single transfascial sutures in each case. It is referred to as IPOM-plus (mesh augmentation; fascial closure) technique. The non-absorbable “0” sutures were used and passed using the suture passer inserted through the tiny skin incisions above the hernia sac. The fascia was included in the suture at 7–10 mm from the edges of hernia defect, and the distance between the consecutive sutures was below 10 mm, with extracorporeal knots inserted into the subcutaneous tissue. When knotting the sutures, the pressure of the pneumoperitoneum was decreased from 12 to 6–8 mmHg, which facilitated tying the knots by lowering the tension. For wider hernias, if laparoscopic closure was not feasible, open-approach closure was performed first, followed by the laparoscopic procedure (hybrid technique). Forty-two patients, in whom hernia defect was closed, constituted the IPOM-plus group—Table 2.
Next, Physiomesh (Ethicon) mesh with double-side anti-adhesive coating of poliglecaprone was inserted. Its size was determined based on the width of the hernia defect so as to ensure at least 5 cm radial margin extending beyond fascial edges. In the centre of the mesh, a suture with approx. 10-cm-long loose ends was placed. Then, the mesh was rolled and inserted into the peritoneal cavity through the 10 mm optical trocar. A suture passer was inserted into the peritoneal cavity through the hernia orifice, grasping the positioning suture previously placed on the mesh and pulling it outside. As a result, a properly positioned mesh could be pulled upwards so as to adhere to the abdominal wall. After ensuring appropriate mesh positioning, its edges were fixed along the upper and lower edges using the transfascial sutures. Next, the mesh was fixed along its edges using the Securestrap (Ethicon) tacker at 2–3 cm intervals, ensuring that the mesh did not displace relative to the hernia defect, when pressing the device against the abdominal wall. Pressing the abdominal wall with the other hand proved to be a useful manoeuvre at this stage. Furthermore, four additional tacks were placed around the hernia defect. The patients were allowed to walk and eat on the first day postoperatively and discharged on the second day postoperatively with the recommendation to use the abdominal elastic binders for the subsequent 4 weeks.
Outcome measures
After 12 months following surgery, a survey was posted to all patients with questions regarding potential recurrence and other experienced symptoms. The survey was posted again to all patients in August 2015. All patients who reported symptoms of recurrence were invited for a follow-up visit including physical examination and a sonography to verify the diagnosis.
The statistical analysis of the basic data performed using Statistica 7.0 (StatSoft) allowed identification of mean values and standard deviation (±). The t test was used for comparisons, and the values below 0.05 were considered statistically significant.
Results
The mean duration of surgery was 49 min (30–85; SD 14.6) in the sIPOM group and 56 min (45–90; SD 12.8) in the IPOM-plus group. Conversion to open surgery was not necessary in any case. In four patients from IPOM-plus group with hernias over 8 cm wide (W3), hernia defect was closed in an open-approach procedure, which was followed by the laparoscopic mesh insertion and fixing (hybrid technique). There was no case of surgical site infection in any of these patients.
The mean duration of postoperative hospitalisation was 2.2 days (1–18; SD 0.6) and 2.4 days (1–16; SD 0.7) in the sIPOM and IPOM-plus groups, respectively. The hospitalisation was prolonged in a total of two patients from both groups, who developed severe complications requiring reoperation.
One of them was a 55-year-old male with paraumbilical hernia, 4 cm in diameter, treated using the bridging technique (sIPOM group). The patient reported dyspnoea, weakness and malaise on the first day postoperatively. However, his haemodynamic parameters and laboratory findings remained within the normal limits. Due to worsening oxygen saturation parameters as well as present known risk factors for venous thromboembolism (obesity, perioperative immobilisation, laparoscopy, age, family history positive for VTE and the use of abdominal binder), the patient had a cardiologist consult. Suspecting pulmonary embolism, anticoagulant treatment with low molecular weight heparin (LMWH) was commenced. On the subsequent day, the patient became haemodynamically unstable, laboratory tests revealed anaemia (haemoglobin level of 7.2 mg%), and the sonography revealed a large amount of fluid within the abdominal cavity. Emergency reoperation was performed, which involved mesh removal. Intraoperatively, the intraperitoneal haemorrhage from the inferior epigastric vessels within the left hypogastrium, where the mesh was fixed by one of the tacks, was revealed. After haematoma evacuation and bleeding control, the laparotomy wound was sutured without the use of mesh.
The second serious complication occurred on the fourth day postoperatively in a patient from IPOM-plus group, who presented with iatrogenic perforation of the transverse colon due to thermal injury caused probably by touching the intestine with the diathermy forceps. During the laparoscopic repair of the incisional epigastric hernia, adhesions between the abdominal wall and the greater omentum were dissected using the diathermy forceps. No adhesions to the intestine were revealed. The perforation was sutured during the reoperation. However, proper tight closure was not achieved, so colostomy was created 3 days later. The remaining postoperative period was uneventful.
After 12 months following surgery, each patient was requested to provide information regarding known or suspected recurrence. Eight patients (20 %) in the sIPOM group reported subjectively perceived recurrence, as compared to none in the IPOM-plus group (p = 0.002). Six patients (14.3 %) in sIPOM group reported suspected recurrence, as compared to three patients (7.1 %) in IPOM-plus group (p = 0.13). Altogether, 14 patients in the sIPOM group and only 3 patients in the IPOM-plus group expressed doubts so as to the long-term effect of hernia repair surgery (p = 0.002). These patients were invited for a follow-up physical examination and sonography. Eventually, four cases of hernia recurrence were confirmed in the sIPOM group (10 %) including one in a patient reporting suspected (not certain) recurrence as compared to none in the IPOM-plus group (p = 0.018). Other patients presented with mesh bulging within the hernia defect and palpable orifice margins, without the signs of recurrence. Patients from the IPOM-plus group, who reported concerns regarding suspected recurrence—all of them with hernias wider than 4 cm—also presented with bulging and palpable margins of the hernia defect despite its previous closure. The follow-up sonography did not show seroma in any of our patients.
The patients were requested again to provide information of known or suspected recurrence in the long-term postoperative period. The mean duration of the follow-up was 44.65 months (53–33; SD 6.03) in the sIPOM group and 22.2 months (32–17; SD 4.14) in the IPOM-plus group. None of the respondents reported known or suspected recurrence of hernia. However, we could not contact—and hence receive feedback—from one patient in the sIPOM group. Therefore, all four cases of recurrence manifested within the first year postoperatively and occurred only in patients treated using the bridging technique (Fig. 1).
Out of these four cases, three patients had laparoscopic hernia repair reoperation. In two of them, additional hernia was revealed, which had not been diagnosed during the primary procedure. One patient treated for incisional epigastric hernia reported a recurrence, which turned out to be a primary paraumbilical hernia on the edge of the mesh, unspotted during the first surgery. Another patient treated for the primary paraumbilical hernia presented postoperatively with epigastric hernia of the linea alba. The recurring hernia in the two remaining patients treated for the primary paraumbilical hernia 3 and 4 cm wide was located on the inferior edge of the mesh. During the laparoscopic reoperations, we did not observe adhesions to the serous membrane of the intestinal wall. Nevertheless, we observed loose adhesions of the greater omentum to the upper edge of the mesh and tangential to its surface only in its upper part, classified as Mueller I adhesions [18]. The visualised mesh fibres were surrounded by the connective tissue, but the mesh pores did not show signs of deformity as compared to the original product. In two cases, the measurements taken during the reoperation showed that the originally 15 cm length was only 13 cm long. However, it was confirmed intraoperatively that the mesh was slightly deformed, stretched and protruding (bulging) where it bridged the fascial defect.
Discussion
The number of laparoscopic ventral hernia repair procedures increases every year. Taken the abundance of synthetic materials available, the search of the product assuring a safe and secure hernia repair is still ongoing. Recent reports have undermined the long-term efficacy of Physiomesh (Ethicon) [15, 19]. The observed increased recurrence rate is attributed to poor mesh integration into the abdominal wall. The postulated underlying cause is the presence of anti-adhesion coating on both sides of the mesh, which may delay its integration into the inner surface of the abdominal wall [20, 21]. As a result, the mesh detaches easily from the abdominal wall during reoperation. In our material, though, we did not observe impaired mesh integration into the abdominal wall. As the pneumoperitoneum was being created and the surgeon was manipulating the mesh, it remained fixed to the patient tissues. When pulled along the abdominal wall, the mesh did not separate from the peritoneum and fascia. However, it was possible to detach the mesh when pulling it perpendicularly to the abdominal wall. This, though, appears obvious, as Physiomesh has a thin, macroporous structure and attaches to the abdominal wall only along the thin filaments covered with connective tissue. As a result, perpendicular force can detach it, although the vectors of abdominal forces are parallel to the surface of the mesh and abdominal wall [22, 23]. Additionally, as reported by Pawlak et al. [15], the onset of all cases of recurrence was within the first 6 months postoperatively, which may indicate that the connective tissue formation and scar tissue maturation were incomplete. All reoperations due to recurrence in our patients were performed after at least 1 year following the primary repair surgery, which could also affect the observed better integration of the mesh into the peritoneum.
Unfortunately, in hernia repair using the intraperitoneal onlay mesh technique, the synthetic mesh can only integrate into the tissues on one side, unlike the sublay technique or Lichtenstein technique used in inguinal hernia repair [24, 25]. Therefore, it is crucial to protect the mesh from the forces, which may dislocate it before its integration into the abdominal wall is complete. It seems that with Physiomesh, non-closure of hernia defect subjects the mesh to a significant stretch due to the lack of mesh support in its central portion [9]. This may adversely affect mesh integration into the tissues and lead to the recurrence. Pawlak et al. [15] observed recurrences in 20 % of their patients (n = 25) after hernia bridging using Physiomesh (sIPOM). Furthermore, Bradley et al. [26] reported only one case of recurrence in a group of 93 patients after laparoscopic ventral hernia repair using Physiomesh. In our material, within the first year of the follow-up, there were four cases of recurrences (10 %) in the group of patients treated using the sIPOM repair and none in the group of patients with IPOM-plus repair. This may support the hypothesis of the essential role of hernia defect closure prior to mesh implantation.
Unfortunately, there is no uniform standard for the closure of hernia defect during IPOM procedures. There are several modifications of sutures placed on the fascial edges and hernia sac. The most commonly used suturing techniques are the ones proposed by Chelala [27, 28], Agrawal [29] and Orenstein [30]. However, none of them meets the criteria recommended for safe abdominal closure with a continuous suture and a suture/wound length (SL:WL) ratio of at least 4:1 [23]. Therefore, in these cases, it should be taken into account that in the long-term perspective, the sutures will eventually rupture the fascia at the edge of the hernia orifice and the defect will reoccur [31–33].
We observed three cases, where despite closure of hernia defect with single transfascial sutures, the defect reoccurred. As a result, the patients reported suspected hernia reoccurrence. However, physical examination and sonography did not confirm the actual hernia, but only bulging due to mesh protrusion in this area. This supports the hypothesis that after a full integration of the mesh into patient tissues, a potential bulging does not affect mesh dislocation and hernia recurrence any longer, unlike in sIPOM method. We did not observe bulging or hernia orifice reopening in patients after open-approach closure (hybrid technique), sutured as recommended by the EHS. Hence, an assumption can be made that the restoration of the midline according to the open-approach suturing standards before the inlay mesh repair of large ventral hernias would also improve treatment outcomes. However, more research into this issue is required. Undoubtedly, repair of large hernias without closure of hernia defect should be abandoned, taken the current state of knowledge [34].
A recurrent incisional hernia resulting from the fracture of low-weight polypropylene mesh is more and more often reported in the literature [32, 35]. The incisional hernioplasty without closing of the anterior myofascial layer, especially in large ventral hernias, should be considered as contraindication for the use of low-weight polypropylene meshes. Therefore, this material should be avoided, and the preference should be given to the heavy-weight polypropylene meshes.
Additionally, the patients should be educated about potential deformation of abdominal wall due to bulging, as some of them interpret bulging as the recurrence of hernia, which may decrease their satisfaction with treatment.
Conclusions
Laparoscopic ventral hernia repair is generally safe, requires short hospitalisation and is associated with the low recurrence and complication rates. Closure of fascial defects before mesh insertion offers better treatment outcomes. Non-closure of fascial defects with only bridging of the hernia defect using standard laparoscopic intraperitoneal onlay mesh repair (sIPOM) causes more frequent recurrence and bulging. As a result, patient satisfaction with treatment is lower, and they are concerned about hernia recurrence. Despite closure of fascial defects using mesh augmentation technique (IPOM-plus), bulging may still develop as the long-term sequela, which can be misinterpreted as the recurrence by the patient.
References
Schreinemacher MH, Emans PJ, Gijbels MJ, Greve JW, Beets GL, Bouvy ND (2009) Degradation of mesh coatings and intraperitoneal adhesion formation in an experimental model. Br J Surg 96(3):305–313
Litarski A, Pawełczyk J, Majcherek J, Janczak D, Pawłowski L, Rucińska Z, Janczak D (2014) Laparoscopic treatment of abdominal hernia—5 years of experience. Polski Przegląd Chirurgiczny 86(8):353–358
Jenkins ED, Yom V, Melman L, Brunt LM, Eagon JC, Frisella MM, Matthews BD (2010) Prospective evaluation of adhesion characteristics to intraperitoneal mesh and adhesiolysis-related complications during laparoscopic reexploration after prior ventral hernia repair. Surg Endosc 24:3002–3007
Ellis H (2005) Intraabdominal and postoperative peritoneal adhesions. J Am Coll Surg 200:641–644
Muysoms FE, Bontinck J, Pletinckx P (2011) Complications of mesh devices for intraperitoneal umbilical hernia repair: a word of caution. Hernia 15:463–468
ten Broek RPG, Schreinemacher MHF, Jilesen APJ, Bouvy N, Bleichrodt RP, van Goor H (2012) Enterotomy risk in abdominal wall repair: a prospective study. Ann Surg 256:280–287
Schreinemacher MHF, ten Broek RP, Bakkum EA, van Goor H, Bouvy ND (2010) Adhesion awareness: a national survey of surgeons. World J Surg 34:2805–2812
Rickert A, Kienle P, Kuthe A, Baumann P, Engemann R, Kuhlgatz J, von Frankenberg M, Knaebel HP, Büchler MW (2012) A randomised, multi-centre, prospective, observer and patient blind study to evaluate a non-absorbable polypropylene mesh vs. a partly absorbable mesh in incisional hernia repair. Langenbecks Arch Surg 397(8):1225–1234
Schoenmaeckers EJP, Wassenaar EB, Raymakers JTFJ, Rakic S (2010) Bulging of the mesh after laparoscopic repair of ventral and incisional hernias. JSLS 14:541–546
Carter SA, Hicks SC, Brahmbhatt R, Liang MK (2014) Recurrence and pseudorecurrence after laparoscopic ventral hernia repair: predictors and patient-focused outcomes. Am Surg 80(2):138–148
Suwa K, Okamoto T, Yanaga K (2015) Closure versus non-closure of fascial defects in laparoscopic ventral and incisional hernia repairs: a review of the literature. Surg Today. doi:10.1007/s00595-015-1219-y
Pawlak M, Bury K, Śmietański M (2015) The management of abdominal wall hernias—in search of consensus. Videosurg Miniinvasive 10(1):49–56
Bellón JM (2009) Degradation of mesh coatings and intraperitoneal adhesion formation in an experimental model. Br J Surg 96(6):693
Gierej P, Kotulski M, Piotrowicz M (2010) Adhesive complications in a patient after ventral hernia IPOM repair—a case report for Videoforum. Videosurg Miniinvasive Tech 5(4):166–170
Pawlak M, Hilgers RD, Bury K, Lehmann A, Owczuk R, Śmietański M (2015) Comparison of two different concepts of mesh and fixation technique in laparoscopic ventral hernia repair: a randomized controlled trial. Surg Endosc 30(3):1188–1197
Chelala E, Debardemaeker Y, Elias B, Charara F, Dessily M, Allé J-L (2010) Eighty-five redo surgeries after 733 laparoscopic treatments for ventral and incisional hernia: adhesion and recurrence analysis. Hernia 14:123–129
Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E, Dietz UA, Eker HH, El Nakadi I, Hauters P, Pascual MH, Hoeferlin A, Klinge U, Montgomery A, Simmermacher RK, Simons MP, Smietański M, Sommeling C, Tollens T, Vierendeels T, Kingsnorth A (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13(4):407–414
Mueller MD, Tschudi J, Herrmann U, Klaiber C (1995) An evaluation of laparoscopic adhesiolysis in patients with chronic abdominal pain. Surg Endosc 9:802–804
Deeken CR, Matthews BD (2013) Ventralight ST and SorbaFix versus Physiomesh and Securestrap in a porcine model. JSLS 17(4):549–559
Vogels RR, van Barneveld KW, Bosmans JW, Beets G, Gijbels MJ, Schreinemacher MH, Bouvy ND (2015) Long-term evaluation of adhesion formation and foreign body response to three new meshes. Surg Endosc 29(8):2251–2259
Pascual G, Sotomayor S, Rodríguez M, Bayon Y, Bellón JM (2015) Tissue integration and inflammatory reaction in full-thickness abdominal wall repair using an innovative composite mesh. Hernia. doi:10.1007/s10029-015-1383-4
Deeken CR, Thompson DM Jr, Castile RM, Lake SP (2014) Biaxial analysis of synthetic scaffolds for hernia repair demonstrates variability in mechanical anisotropy, non-linearity and hysteresis. J Mech Behav Biomed Mater 38:6–16
Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, Köckerling F, Kukleta J, LeBlanc K, Lomanto D, Misra MC, Morales-Conde S, Ramshaw B, Reinpold W, Rim S, Rohr M, Schrittwieser R, Simon Th, Smietanski M, Stechemesser B, Timoney M, Chowbey P (2014) Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society [IEHS])—Part 2. Surg Endosc 28:353–379
Takács I, Horváth S, Molnár Á, Gáspár S, Hajós R, Meczker Á, Kóbor P, Lantos J, Jávor S, Balatonyi B, Szekeres G, Röth E, Wéber G (2011) Comparative immunohistochemical study of tissue integration of macroporous and laminar surgical meshes. Histol Histopathol 26(7):821–830
Mitura K (2016) Different approach to laparoscopic IPOM ventral hernia surgery—what has the last decade taught us? Pol Przegl Chir. 88(1):54–61
Bradley JF III, Williams KB, Wormer BA, Tsirline VB, Walters AL, Sing RF, Belyansky I, Heniford BT (2012) Preliminary results of surgical and quality of life outcomes of Physiomesh in an international, prospective study. Surg Technol Int 22:113–119
Chelala E, Thoma M, Tatete B, Lemye AC, Dessily M, Alle JL (2007) The suturing concept for laparoscopic mesh fixation in ventral and incisional hernia repair: mid-term analysis of 400 cases. Surg Endosc 21:391–395
Chelala E, Baraké H, Estievenart J, Dessily M, Charara F, Allé JL (2015) Long-term outcomes of 1326 laparoscopic incisional and ventral hernia repair with the routine suturing concept: a single institution experience. Hernia. 21 June 2015. [Epub ahead of print]
Agarwal BB, Agarwal S, Gupta MK, Mishra A, Mahajan KC (2008) Laparoscopic ventral hernia meshplasty with “double-breasted” fascial closure of hernia defect: a new technique. J Laparoendosc Adv Surg Tech 18:222–229
Orenstein SB, Dumeer JL, Monteagudo J, Poi MJ, Novitsky YW (2011) Outcomes of laparoscopic ventral hernia repair with routine defect closure using “shoelacing” technique. Surg Endosc 25:1452–1457
Muysoms FE, Antoniou SA, Bury K, Campanelli G, Conze J, Cuccurullo D, de Beaux AC, Deerenberg EB, East B, Fortelny RH, Gillion JF, Henriksen NA, Israelsson L, Jairam A, Jänes A, Jeekel J, López-Cano M, Miserez M, Morales-Conde S, Sanders DL, Simons MP, Śmietański M, Venclauskas L, Berrevoet F, European Hernia Society (2015) European Hernia Society guidelines on the closure of abdominal wall incisions. Hernia 19(1):1–24
Millbourn D, Cengiz Y, Israelsson LA (2009) Effect of stitch length on wound complications after closure of midline incisions: a randomized controlled trial. Arch Surg 144(11):1056–1059
Palanivelu C, Jani KV, Senthilnathan P et al (2007) Laparoscopic sutured closure with mesh reinforcement of incisional hernias. Hernia 11:223–228
Strey CW (2014) Triple-step laparoscopic incisional hernia repair: midline suture closure supported by dorsal component separation and intraperitoneal onlay mesh reinforcement. World J Surg 38(12):3276–3279
Zuvela M, Galun D, Djurić-Stefanović A, Palibrk I, Petrović M, Milićević M (2014) Central rupture and bulging of low-weight polypropylene mesh following recurrent incisional sublay hernioplasty. Hernia 18(1):135–140
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Kryspin Mitura, Marzena Skolimowska-Rzewuska and Karolina Garnysz have no conflict of interest.
Rights and permissions
About this article
Cite this article
Mitura, K., Skolimowska-Rzewuska, M. & Garnysz, K. Outcomes of bridging versus mesh augmentation in laparoscopic repair of small and medium midline ventral hernias. Surg Endosc 31, 382–388 (2017). https://doi.org/10.1007/s00464-016-4984-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4984-9