Abstract
Background
Laparoscopic ventral hernia repair (LVHR) has gained popularity, since it can decrease the incidence of surgical site complications while providing similar recurrence rates as open repairs. The role of defect closure in LVHR has been a subject of controversy and has not been fully elucidated. We aimed to compare outcomes of LVHR with and without defect closure in a contemporary cohort.
Methods
Single-institution retrospective review of consecutive adults undergoes elective LVHR for 2–8 cm defects. Demographics, perioperative, and post-operative data were included for analysis. Surgical site events (SSE), surgical site infection (SSI), and recurrence were the main measured outcomes. Abdominal CT scan was used to differentiate true recurrence from pseudo-recurrence.
Results
A total of 783 patients were analyzed. 222 of them had their defects closed (DC), while the remaining 561 defects were not closed (NC) at the discretion/routine of the operating surgeon. Patients were slightly older in the non-closure group, while those in the defect closure group had a significantly higher BMI. There were no other differences in demographics between groups. After a mean follow-up of 12.1 months, the incidence of surgical site events (3.6 vs 14.9%, p < 0.0001) and seromas (0.4 vs 11.5%, p < 0.0001) was significantly lower in the defect closure group. Objectively confirmed recurrences were also significantly lower in the DC group (5.4 vs 14.2%, p = 0.003).
Conclusions
In our experience, the addition of defect closure can reduce the incidence of surgical site events, seroma, and hernia recurrence after LVHR. We advocate for routine closure of defects when laparoscopic repair is chosen for small-to-mid-sized ventral hernias.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Open approaches for ventral hernia repair have proven to be safe, effective, and durable. Nevertheless, large incisions and extensive dissection can lead to significant wound morbidity [1, 2]. Thus, minimally invasive techniques for ventral hernia have gained popularity, since they have lower incidence of surgical site complications and similar recurrence rates when compared to open repairs [3, 4].
The most commonly performed minimally invasive hernia repair is the laparoscopic ventral hernia repair (LVHR), first described in 1993 by LeBlanc and Booth [5]. The traditional LVHR repair is based on the placement of an intraperitoneal mesh that bridges the defect while providing large overlap around the hernia. Therefore, the durability of the repair relies on penetrating fixation of the mesh to the abdominal wall [6, 7].
The role of defect closure in LVHR has been a subject of controversy and has not been fully elucidated. Restoration of the native abdominal wall anatomy has become an important goal of modern hernia repair [8]. Adhering to this principle, several techniques for reapproximation of the hernia defect have been described [9,10,11,12]. Herein, we aimed to compare outcomes of LVHR with and without defect closure in a contemporary single-institution cohort. We hypothesized that closing defects prior to mesh implantation improves wound morbidity and durability of LVHR.
Methods
After obtaining Institutional Review Board approval, consecutive adult patients undergoing elective LVHR for 2–8 cm defects were retrospectively reviewed. Demographic data obtained included: age, gender, body mass index (BMI), American Society of Anesthesiologists (ASA) score, diabetes mellitus, chronic obstructive pulmonary disease (COPD), and smoking status. Perioperative data included hernia defect width, hernia defect area, area of implanted mesh used, and total operative time. The decision to close or not close defects was largely surgeon-dependent.
Post-operative data included length of hospitalization and wound complications, including surgical site event (SSE) or surgical site infection (SSI) as defined by CDC criteria [13]. An SSE was described as any SSI, symptomatic seroma or hematoma, wound cellulitis, or suture abscess [14].
Typical post-operative follow-up includes physical examination at 2–4 weeks, 3 months, 6 months, 1 year, and then annually. Abdominal computed tomography (CT) scans are obtained routinely at the annual visit, or at any time for evaluation of persisting pain, bulging, or obstructive symptoms.
For statistical analysis, we used IBM® SPSS Statistics 20. Categorical variables were compared using Chi-squared test. For continuous variables, normality was determined using Saphiro–Wilk test and groups were compared accordingly using Student’s t test or Mann–Whitney U test.
Operative technique for defect closure
Although detailed descriptions of our laparoscopic “shoelace” technique can be found elsewhere [15], a brief review of the operative steps is presented here:
The patient is placed in the supine position with both arms tucked. Access is usually obtained using an optical trocar via left upper subcostal entry. Additional two 5-mm trocars are placed under direct visualization. Those trocars are used for lysis of adhesions, defect closure, and initial mesh positioning. Two additional contralateral trocars are typically placed to facilitate tacking the ipsilateral mesh side. Lysis of adhesions is performed with cold scissors and very limited use of advanced bipolar energy and all sac contents are reduced.
Closure of the defect is performed as follows:
-
1.
An external vertical line is drawn on the skin through the central portion of the defect. Using spinal needles, the superior and inferior edges are identified and marked. Sites for figure-of-eight sutures are marked approximately every 3 cm on the vertical line.
-
2.
Starting at one end, a stab incision is made with a #11 blade. A #1 polypropylene suture is advanced approximately 1 cm lateral from the fascial edge (Fig. 1a) and a Maryland dissector is used to grasp the suture. The suture passer is retrieved and then advanced through the contralateral defect edge to take the suture from the Maryland dissector (Fig. 1b). Using the same incision, one end of the suture is passed and retrieved in the same fashion after a 1 cm longitudinal advancement to obtain a figure-of-eight stitch that will be temporarily grasped with a hemostat (Fig. 1c).
-
3.
Additional figure-of-eight stitches are placed every 3 cm along the previously placed marks (Fig. 1d). After pneumoperitoneum is transiently released, sutures are tied sequentially starting from the ends and advancing centrally being careful to avoid entrapping visceral entrapment (Fig. 1e). Knots are buried in the subcutaneous tissue and the skin is released with a hemostat to prevent skin puckering.

From [15]
Technique for “shoelace” closure of hernia defect.
Intraperitoneal mesh reinforcement was aimed to provide at least 5–7 cm of overlap after defect closure. As a result, we most commonly employed a 15 cm wide mesh in the defect closure group. Circumferential fixation with absorbable tacks is followed by four-to-six trans-abdominal fixation stitches using #1 polypropylene suture. After skin reapproximation of port sites using 4–0 deep dermal sutures, all incisions are closed with topical adhesive. Abdominal binders are typically used in the early post-operative period.
Results
Demographics
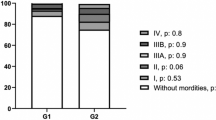
Between 2006 and 2016, 783 patients were identified for analysis. 222 of them had their defects closed (DC) and for the remaining 561 defects were not closed (NC) according to the surgeon’s routine. Patient demographics are summarized in Table 1. There were no differences in gender, ASA score, diabetes mellitus, chronic obstructive pulmonary disease, or smoking status between groups. Patients were slightly older in the non-closure group (57.9 ± 13.1 vs 53.4 ± 16.1, p = 0.01), while those in the defect closure group had a significantly higher BMI (39.8 ± 8.8 vs 34.1 ± 7.5 kg/m2, p = 0.04).
Perioperative and post-operative outcomes
The hernia width and area were similar among the 2 study groups (Table 2). All patients received synthetic prosthetics. There were no differences in the area of implanted mesh between both groups. There were no differences in intra-operative complications. No adverse events were associated with defect closure. Finally, the addition of defect closure was not associated with a significant increase in operative time or length of hospitalization.
Thirty-two percent of patients in the DC group and 23% of patients in the non-closure group had CT scans in the post-operative period. After a mean follow-up of 12.1 months, the incidence of surgical site events was significantly lower in the defect closure group (3.6 vs 14.9%, p < 0.0001). Seromas were particularly less frequent in in the DC group (0.4 vs 11.5%, p < 0.0001). There were no differences in surgical site infections among groups. Hospital stay was not affected by either approach. Objectively confirmed recurrences were significantly lower when the hernia defect was closed (5.4 vs 14.2%, p = 0.003).
Discussion
Minimally invasive approaches for ventral hernia repair continue to gain popularity. Simultaneously, surgical techniques are frequently refined in the search to improve outcomes. The traditional LVHR is commonly performed by placing an intraperitoneal coated mesh to bridge the defect. In this study, we were able to demonstrate that the addition of defect closure significantly decreased the incidence of surgical site events, symptomatic seromas, and hernia recurrences after LVHR.
Restoration of the normal abdominal wall anatomy with reconstruction of the linea alba is one of the pillars of modern open hernia repair. Although this concept has not been fully adopted in LVHR, it has gained popularity and interest in recent years [16, 17]. One of the consequences of a bridged repair is the creation of a large dead space, with the subsequent essentially uniform development of seromas. While the vast majority of those seromas may remain asymptomatic, symptomatic seromas can be found in up to 30% of LVHR; leading some surgeons to suggest that a seroma is an “expected” outcome after this procedure. We feel strongly against this concept, especially since an increasing number of series and a systematic review have shown that seroma rates can be significantly reduced if defect closure is added to LVHR [18, 19]. Although a recent retrospective analysis from AHSQC did not found a benefit from defect closure in terms of 30-day wound morbidity [17], our single-institution data clearly show that obliteration of the dead space with an extracorporeal technique can substantially reduce seroma formation without significant increases in the total operative time. We believe that if a defect cannot be closed, a different (reconstructve) surgical approach should typically be considered.
The role of defect closure on hernia recurrence is controversial. Although a recent multicenter retrospective review did not reveal an impact of defect closure in recurrence, it may have occurred due to specific technique employed [20]. On the other hand, reports and systematic reviews have suggested that the addition of defect closure can decrease the recurrence rates after LVHR [10, 18, 21]. This was also true in our comparative series. With a 1-year average follow-up, objective hernia recurrence was nearly 10% lower when defect closure was performed. One explanation for this can be that defect reapproximation allows for equalized tension along the mesh surface and prevents the friction and shear forces that are expected on the defect edges after a bridged repair. Another reason for this could be that the non-covered surface of a macroporous mesh is contacting peritoneum in its entirety after defect closure, thus allowing for full integration of the mesh with the abdominal wall.
From a mechanical standpoint, our group has previously analyzed the radiologic effects that restoration of the native myofascial anatomy has on the abdominal wall. A compensatory muscle hypertrophy has been observed after linea alba was restored in open repairs, but this effect was not observed in laparoscopic bridged repairs [22]. This ultimately affects other important outcomes of the operation, and reports have shown that defect closure can result in improved patient satisfaction, better cosmetic appearance, and higher functional status scores [20].
This study is limited by its retrospective nature and a relatively short length of follow-up, its main strength relies on being the largest single-institution contemporaneous comparative experiences assessing the benefits of defect closure in LVHR.
Conclusion
In our experience, the addition of defect closure can reduce the incidence of surgical site events and hernia recurrence after LVHR. We advocate for routine closure of defects when laparoscopic repair is chosen for small-to-mid-sized ventral hernias.
References
Novitsky YW, Fayezizadeh M, Majumder A et al (2016) Outcomes of posterior component separation with transversus abdominis muscle release and synthetic mesh sublay reinforcement. Ann Surg 264:226–232
Cobb WS, Warren JA, Ewing JA et al (2015) Open retromuscular mesh repair of complex incisional hernia: predictors of wound events and recurrence. J Am Coll Surg 220:606–613
Sauerland S, Walgenbach M, Habermalz B et al (2011) Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev CD007781
Al Chalabi H, Larkin J, Mehigan B, McCormick P (2015) A systematic review of laparoscopic versus open abdominal incisional hernia repair, with meta-analysis of randomized controlled trials. Int J Surg 20:65–74
LeBlanc KA, Booth WV (1993) Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. Surg Laparosc Endosc 3:39–41
Majumder A, Fayezizadeh M, Hope WW, Novitsky YW (2016) Evaluation of a novel permanent capped helical coil fastener in a porcine model of laparoscopic ventral hernia repair. Surg Endosc 30:5266–5274
Muysoms F, Vander Mijnsbrugge G, Pletinckx P et al (2013) Randomized clinical trial of mesh fixation with “double crown” versus “sutures and tackers” in laparoscopic ventral hernia repair. Hernia 17:603–612
Criss CN, Petro CC, Krpata DM et al (2014) Functional abdominal wall reconstruction improves core physiology and quality-of-life. Surgery 156:176–182
Orenstein SB, Dumeer JL, Monteagudo J et al (2011) Outcomes of laparoscopic ventral hernia repair with routine defect closure using “shoelacing” technique. Surg Endosc 25:1452–1457
Zeichen MS, Lujan HJ, Mata WN et al (2013) Closure versus non-closure of hernia defect during laparoscopic ventral hernia repair with mesh. Hernia 17:589–596
Palanivelu C, Jani KV, Senthilnathan P et al (2007) Laparoscopic sutured closure with mesh reinforcement of incisional hernias. Hernia 11:223–228
Agarwal BB, Agarwal S, Mahajan KC (2009) Laparoscopic ventral hernia repair: innovative anatomical closure, mesh insertion without 10-mm transmyofascial port, and atraumatic mesh fixation: a preliminary experience of a new technique. Surg Endosc 23:900–905
Mangram AJ, Horan TC, Pearson ML et al (1999) Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 20:250–278; quiz 279–280
Majumder A, Winder JS, Wen Y et al (2016) Comparative analysis of biologic versus synthetic mesh outcomes in contaminated hernia repairs. Surgery 160:828–838
Orenstein SB, Novitsky YW (2016) Laparoscopic ventral hernia repair with defect closure. In Novitsky YW (ed) Hernia surgery: current principles. Springer, pp 231–240
Wennergren JE, Askenasy EP, Greenberg JA et al (2016) Laparoscopic ventral hernia repair with primary fascial closure versus bridged repair: a risk-adjusted comparative study. Surg Endosc 30:3231–3238
Papageorge CM, Funk LM, Poulose BK et al (2017) Primary fascial closure during laparoscopic ventral hernia repair does not reduce 30-day wound complications. Surg Endosc 31:4551–4557
Chelala E, Barake H, Estievenart J et al (2016) Long-term outcomes of 1326 laparoscopic incisional and ventral hernia repair with the routine suturing concept: a single institution experience. Hernia 20:101–110
Tandon A, Pathak S, Lyons NJ et al (2016) Meta-analysis of closure of the fascial defect during laparoscopic incisional and ventral hernia repair. Br J Surg 103:1598–1607
Clapp ML, Hicks SC, Awad SS, Liang MK (2013) Trans-cutaneous closure of central defects (TCCD) in laparoscopic ventral hernia repairs (LVHR). World J Surg 37:42–51
Nguyen DH, Nguyen MT, Askenasy EP et al (2014) Primary fascial closure with laparoscopic ventral hernia repair: systematic review. World J Surg 38:3097–3104
De Silva GS, Krpata DM, Hicks CW et al (2014) Comparative radiographic analysis of changes in the abdominal wall musculature morphology after open posterior component separation or bridging laparoscopic ventral hernia repair. J Am Coll Surg 218:353–357
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
LAMDC, HJM, and HLE declare no conflict of interest. YWN is a consultant for Intuitive Surgical, CR Bard, and Cooper Surgical.
Rights and permissions
About this article
Cite this article
Martin-del-Campo, L.A., Miller, H.J., Elliott, H.L. et al. Laparoscopic ventral hernia repair with and without defect closure: comparative analysis of a single-institution experience with 783 patients. Hernia 22, 1061–1065 (2018). https://doi.org/10.1007/s10029-018-1812-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-018-1812-2