Abstract
Background
Parastomal hernia (PSH) is a very frequent complication after creation of a permanent colostomy. The aim of that study is to assess the safety and the long-term efficacy of an intra-peritoneal onlay mesh (IPOM) positioned at the time of primary stoma formation to prevent PSH occurrence.
Materials and methods
That multicentre prospective study concerned 29 consecutive patients operated for cancer of the low rectum between 2008 and 2014. There were 14 men and 15 women with a median age of 73 years (range 39–88) and a BMI of 28 (range 21–43). All the patients had potentially curative abdominoperineal excision associated with IPOM reinforcement of the abdominal wall with a round non-slit composite mesh centred on the stoma site and covering the lateralized colon according to the modified Sugarbaker technique. The major outcomes analysed were operative time, complications related to mesh and PSH incidence. Patients were evaluated at 6-month intervals for the first 2 years and thereafter annually with physical examination and CT scan control. For PSH evaluation, we used the classification of Moreno-Matias.
Results
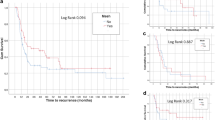
Surgery was performed by laparoscopy in 24 patients and by laparotomy in 5; 17 had a trans-peritoneal colostomy and 12 an extra-peritoneal colostomy. The median size of the mesh was 15 cm (range 12–20), the operative time 225 min. (range 123–311) and the specific time for mesh placement 15 min. (range 10–30). With a median follow-up of 48 months (range 6–88), no mesh infection or complication requiring mesh removal were recorded. No patient developed a true PSH; two of them had a type Ia PSH (only containing the bowel forming the colostomy with a sac < 5 cm) and were totally asymptomatic.
Conclusion
In our series, the incidence of PSH was 7 % and no specific mesh-related complication was noted. Prophylactic mesh reinforcement according to the modified Sugarbaker is an effective technique that addresses the issues related to the occurrence of PSH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Parastomal hernia (PSH) is a major complication after creation of a permanent stoma, no matter what modification of the surgical technique is used [1]. The reported incidence of PSH for permanent colostomy ranges from 4 to 48 % in retrospective studies [1] and from 44 to 93 % in prospective studies [2–4]. Goligher even went so far as to claim that some degree of parastomal herniation is inevitable given enough follow-up time [5]. Surgical procedures for repairing PSH are difficult and associated with high rates of postoperative complications and recurrences [1, 6, 7]. The high prevalence of PSH and the difficulties encountered during repair mean that it is likely the best to prevent its occurrence. Prophylactic mesh placement is the only efficient way to achieve this goal and appears to be a cost-effective strategy in patients with stage I–III rectal cancer [8]. In a recent review article, Aquina concluded that prevention of PSH with mesh might soon become accepted as a standard of care if the results of ongoing trials continue to favour that strategy [9].
In early studies about PSH prevention, the authors used a polypropylene mesh with a central aperture placed by laparotomy in an onlay or sublay position and they showed promising results. However, despite the use of mesh, the incidence of PSH was not negligible and ranged between 0 and 22 % [10]. It is well documented that any implanted synthetic mesh shows a variable amount of shrinkage. Based on animal studies, shrinkage of a mesh with a central hole will give rise to enlargement of this hole [11, 12] that can subsequently be a site prone to develop PSH. Therefore, we considered that intra-peritoneal onlay mesh (IPOM) reinforcement of the abdominal wall according to the modified Sugarbaker technique [13] could be a more reliable option. This technique does not require any extensive dissection and is easy to perform by laparotomy or laparoscopy. In order to assess the results of IPOM placement for PSH prevention, a prospective study was initiated in 2008 among the members of the Club Coelio: a group of 50 Belgian and French surgeons with large experience in laparoscopic surgery. The preliminary results of that study were published in 2012 [14]; the present article reports the long-term results.
Materials and methods
Study protocol
All the members of the Club Coelio were invited to participate at a non-comparative cohort study based on a prospective maintained database. The patients’ inclusion criteria were (1) cancer of the low rectum requiring elective abdominoperineal excision resulting in a permanent end colostomy, (2) potentially curative resection, (3) ASA I-III patients, (4) no faecal contamination during surgery, (5) elective surgery performed by laparoscopy or by laparotomy and (6) creation of a trans-peritoneal or extra-peritoneal colostomy at the surgeon’s discretion. Exclusion criteria were (1) the absence of patient’s consent, (2) the existence of a metastatic disease with limited expected survival, (3) ASA IV patients, (4) significant bowel spillage during surgery and (5) emergency operation. The patients who met the study criteria had prevention of PSH formation by IPOM reinforcement of the abdominal wall with a non-slit round Parietex® composite mesh centred on the stoma and covering the lateralized colon according to the modified Sugarbaker technique [13]. Parietex® composite is a macroporous polyester mesh coated with an absorbable hydrophilic film made of collagen from porcine origin, polyethylene glycol and glycerol that is suitable for intra-peritoneal placement. The non-absorbable polyester mesh provides long-term reinforcement of soft tissues, and the absorbable hydrophilic film minimizes adhesions to the mesh when in direct contact with the viscera. The preoperative data collected included age, sex, body mass index (BMI) and the existence of risk or co-morbidity factors. The operative data included the type of surgical approach, the type of stoma, the operating time, the specific time for mesh positioning, the size and type of the implanted mesh and the mesh fixation. The total surgical operating time was extracted from the anaesthetist computerized protocol, and the specific time for mesh placement was monitored with a chronometer with the assistance of the theatre nurse. The postoperative data included the hospital length of stay, the postoperative complications and PSH occurrence. The major outcomes of the study were operative time, complications related to mesh and PSH occurrence. Patients were evaluated at the outpatient clinic at 6-month intervals for the first 2 years and thereafter annually with physical examination and CT scan in supine position. The ethical committee had no objection about the systematic use of repeated abdominal CT scan because it was already part of the routine oncological protocol surveillance of patients with rectal carcinoma. For PSH assessment, we used the classification proposed by Moreno-Matias and Serra-Aracil [15] (Table 1). The evaluation of CT scan was done by surgeons with possibility of complementary lecture by the first author in case of doubt.
Surgical technique
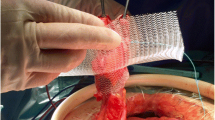
The day before surgery, a stomatherapy nurse marked the ideal site for the colostomy on the patient’s skin. Per-operatively, patients received antibiotic prophylaxis administered intravenously. Once total mesorectal excision was completed, the bowel was divided using endo-GIA® stapler and the staple rows were swabbed with betadine. The proximal end of the bowel was then brought to the outside trans-peritoneally or extra-peritoneally at the site marked by the stomatherapy nurse. No particular attention was paid to create the stoma through or outside the rectus abdominis muscles. The composite mesh was introduced in the peritoneal cavity. To facilitate its positioning, an additional 5-mm port was placed below the right costal margin and the scope was moved from the umbilicus to a right-sided 10-mm port. The mesh was centred on the stoma site with trans-fascial sutures that could be removed or tied at the end of the procedure according to the surgeon’s preference. The exiting bowel was lateralized on the abdominal wall with careful positioning of the mesh not to create any stenosis or angulation of the colon. Finally, the mesh was secured to the abdominal wall by a double crown of helicoidal tacks. In the case of trans-peritoneal colostomy that is easier to perform especially by laparoscopy, the use of a specific Parietex® composite “parastomal” mesh was recommended. That specific mesh exhibits a central band made out of a two-dimensional monofilament polyester fabric coated on both sides with an anti-adhesive film made of collagen. The lateralized colon going to the stoma was only in contact with that central band and protected from mesh erosion (Fig. 1). The mesh must also cover completely the lateralized colon to prevent the possibility of internal hernia. Whenever it is possible, the greater omentum was positioned between the mesh and the surrounding small bowel. The possible contamination of the mesh from the intestinal contents was kept to a minimum by fashioning the colostomy at the last stage of the operation using 3/0 vicryl® after closure of the port sites or closure of the midline incision. At the end of the procedure, the outlet was tested digitally to rule out any compressive effect. All patients were operated by senior surgeons with high expertise in laparoscopic colorectal surgery and ventral hernia repair. Moreover, homogenization of the procedure among the different centres was made by a demonstration video of the surgical technique carried out by the first author.
Results
Twenty-four members of the Club Coelio declined the invitation to participate at the study because they were not performing routinely colorectal surgery. Eightteen members were reluctant to include their patients because of the risk of medico-legal consequence in case of mesh-related complication. Finally, 8 members participated at the study. Three of them only included patients at the end of the study period after publication of the preliminary results. Twenty-nine patients operated between 2008 and 2014 were included in the study. The median number of patients included per surgeon was 2.5 (range 1–12). There were 14 men and 15 women with a median age of 73 years (range 39–88) and a BMI of 28 (range 21–43). Indications for surgery were rectal adenocarcinoma (n = 26), squamous cell anal carcinoma (n = 2) and rectal GIST (n = 1). Five patients had chronic obstructive lung disease or smoking habits, 2 had diabetes mellitus, and 6 patients had obesity (BMI ≥ 30). Surgery was performed by laparoscopy in 24 patients and by laparotomy in 5; 17 had a trans-peritoneal colostomy and 12 an extra-peritoneal colostomy. In case of trans-peritoneal colostomy, the specific Parietex® composite “parastomal” mesh was used in 15 patients (Table 2). The median size of the mesh was 15 cm. (range 12–20). The mesh was secured to the abdominal wall with helicoidal tacks only in 20 patients and with an association of tacks and trans-fascial sutures in 9 patients. The median operative time was 225 min. (range 123–311), and the specific time for mesh placement 15 min. (range 10–30). Postoperative morbidity consisted of 1 urinary infection, 1 paralytic ileus, 5 perineal wound abscesses and 1 acute intestinal obstruction related to incarceration of a small bowel loop in the peritoneal closure of the pelvis floor. No stoma site infection was observed. The median postoperative stay was 14 days (range 7–25). One month after surgery, one patient presented with a mild stoma stenosis that was successfully treated by a single session of dilatation. The median follow-up was 48 months (range 6–88). No patient was lost for follow-up, but 10 died during the follow-up period: 3 for non-oncologic reason and unrelated to the use of the prophylactic mesh and 7 because of metastatic rectal cancer. The median delay between initial operation and death was 40 months (range 8–69). Nineteen patients were still alive in 2015; 16 were in complete remission and 3 had metastasis of their rectal cancer. Five patients required a new operation: 2 for cholelithiasis, 2 for incisional hernia on the midline laparotomy and 1 for intestinal obstruction due to adhesions in the left flank. Each time, the correct positioning and efficacy of the prophylactic mesh was confirmed. No mesh-related complications were encountered and none of the implants had to be removed. No patient had significant complaints related to stoma or problems to seal the appliance. On clinical examination, only one patient had a small stoma bulge already present at the six-month office visit. Systematic CT scan evaluations revealed that 27 patients had no evidence of PSH (Fig. 2) and 2 had a type Ia PSH (Fig. 3). The patient with the clinical stoma bulge was one of the two patients with a type Ia PSH. In both patients, type Ia PSH was evidenced at the 6-month CT Scan evaluation but the following controls showed no radiological evolution with a follow-up of more than 4 years. Those two patients had been operated by laparoscopy: one had a trans-peritoneal and the other an extra-peritoneal colostomy.
Discussion
Due to the high frequency of PSH and limited success of repair, attention has been focused on preventing PSH at the outset when a stoma is fashioned. Although there was a report of the use of synthetic mesh at the time of primary stoma formation to prevent PSH formation as early as 1986 [16], there has been a great reluctance in the surgical community to place mesh in a potentially contaminated field because of the apparent risk of infection. It is currently well admitted that a synthetic mesh can be used in a clean contaminated field [17] and prevention of PSH with mesh is becoming a validated procedure [9]. A metaanalysis in 2012 that included the first three published randomized controlled trials (RCT) [2, 3, 18] demonstrated a substantial difference in the incidence of PSH between controls and patients with prophylactic mesh [19]. The incidence was 12 % for those with mesh and 55 % for controls without increased risk of stoma infection, necrosis or stenosis. In addition to an observed decreased incidence of PSH, mesh reinforcement was also associated with a reduced incidence of PSH requiring surgical repair (0 vs. 22 %) [19]. The results of the four RCT published later on were more controversial [4, 20–22]. Two studies concluded that prosthetic reinforcement of stoma was safe but did not significantly reduce the rate of PSH formation [20, 22] and two reported a very high incidence of PSH up to 50 % in the mesh group [4, 22]. In a very recent population-based study comparing two time periods, where the main difference between the compared groups was the use of a prophylactic mesh, the author also concluded that the use of a mesh did not reduce the rate of PSH [23]. All the studies designed to compare the results of using a prophylactic synthetic mesh vs. no mesh at the time of formation of a permanent colostomy [2–4, 20–24] are reported in Table 3. Overall, the average incidence of PSH at the site of an end-colostomy was reduced by the implantation of a prophylactic mesh, but the rates of PSH remained very high in the mesh group (50 vs. 35 %). Despite placement of a prophylactic mesh, several prospective cohort studies also demonstrated that the incidence of PSH was not negligible and ranged from 8 to 25 % [25–27]. The last proposed surgical option was the Stapled Mesh stomA Reinforcement Technique (SMART) that uses a purpose designed circular stapling gun of various diameters to create a precise trephine and simultaneously fixes a mesh sub-peritoneally and circumferentially to the trephine. Once again, the procedure was clinically safe but the incidence of PSH was 19 % with a median follow-up of 21 months [28].
The common denominator of all those RCT or cohort studies was the use of the same surgical technique, i.e. the bowel was brought out through a flat mesh with a central aperture placed in onlay [25], sublay [2, 3, 18, 20, 21, 23, 24, 26, 27], inlay [28] or intra-peritoneal position [4, 22]. Unfortunately, enlargement of the orifice created in the centre of the mesh for the passage of the intestine [29] and augmentation of the size of the abdominal fascia aperture [21, 24] favouring development of PSH was reported in several clinical studies. This phenomenon, due to shrinkage of the mesh, has been well described in experimental studies [11, 12] and obviously explains the high incidence of PSH when a mesh with a central aperture is used for prevention. A few years ago, the same issue was already observed in case of laparoscopic repair of PSH. In the early experience of laparoscopic treatment of PSH, a central keyhole was fashioned in the mesh to allow the bowel to pass through the abdominal wall [30–32]. This technique was referred as the “keyhole technique” as opposed to the “modified Sugarbaker technique” [13] in which a non-slit covering mesh is used to correct the hernia. Early promising results were noted with the keyhole technique [30]. With longer follow-up, an unacceptable high recurrence rate ranging from 38 to 73 % [31–33] was recorded and the cause of recurrence was always the widening of the central hole and herniation through the enlarged aperture [32, 33]. Nowadays, surgeons are well aware of the risks inherent to the “keyhole technique” for PSH repair [7] and many of them shifted to the “modified Sugarbaker technique” and achieved better results [32, 34, 35].
Our series is the first one to report the use of the modified Sugarbaker technique for PSH prevention. It appeared to us as an easy technique with numerous advantages. The procedure can be done by laparoscopy or by laparotomy and does not require extensive dissection. It is also a totally aseptic procedure because the mesh is inserted into the abdomen only when the colon used to create the stoma has already been passed through the abdominal wall. In this way, there is no contact at all between the mesh and the staple row of the transected colon thus minimizing the risk of mesh infection. Finally, the modified Sugarbaker technique does not require creating an orifice in the mesh and avoids the described disadvantages related to the contraction of the material. In our study, we used the Parietex® composite mesh that is suitable for intra-peritoneal placement. In the case of trans-peritoneal colostomy, which is easier to perform especially by laparoscopy, the use of the “parastomal” Parietex® composite mesh was recommended. That specific mesh exhibits a central band made out of a two-dimensional monofilament polyester fabric coated on both sides with an anti-adhesive film made of collagen. In this way, not only the viscera but also the lateralized colon going to the stoma are protected and the potential risk of mesh erosion is highly minimized.
The prolonged follow-up period, and the use of clinical and radiological criterion to determine the presence of PSH increase the strength of the results obtained in our study. Several studies demonstrated that CT Scan evaluation is much more accurate than simple clinical examination to determine the true incidence of PSH [3, 23, 36, 37]. Besides, the classification of Moreno-Matias [15] looked particularly interesting because a very good correlation was reported between the radiologic hernia grade and the patient’s symptoms. Grade III hernias are almost always symptomatic, grade II hernias are symptomatic 60 % of the time, grade Ib hernia symptoms are reported in 40 % of cases and grade Ia hernias are almost always asymptomatic [15, 38]. Our study confirmed that placement of a prophylactic mesh is clinically safe with no infection or complication requiring removal of the material. With a median follow-up of 4 years, 27 patients had no PSH and 2 had a type Ia PSH. It must be pointed out that those two patients remained fully asymptomatic with a follow-up of 58 and 51 months, respectively, which is in accordance with the literature data [15, 38]. In the prospective randomized trial conducted by Serra-Aracil about PSH prevention, stage Ia hernias were subclinical and were not recorded as real PSH [3]. However, to prevent the apparition of a large sliding colonic hernia between the mesh and the abdominal wall, great attention should be paid not to leave a too long colonic loop in place when creating the stoma. Another potential pitfall of the technique is that lateralizing the bowel after direct placement of mesh can theoretically lead to severe bowel angulation [39] and possible stoma obstruction at the mesh flap site requiring revision surgery, but we did not encounter this situation. Last but not least, the time demand for the mesh placement represents only 7 % of the total operative time and should not be an argument to limit the use of a prophylactic mesh.
Limitations of our study include the relative small number of patients, the lack of control group and the possibility of biases in patient’s selection. At some exceptions [20, 23, 26, 27], less than 35 patients were also included in most of the previous studies reporting the use of a prophylactic mesh for PSH prevention [2–4, 16, 18, 20, 22, 24, 25]. Besides, indications for APR are decreasing and our inclusion criteria were strictly followed. Our study was designed as a non-comparative study and the major outcome was to assess the safety and effectiveness of the modified Sugarbaker technique for PSH prevention. The incidence of PSH in patients without mesh reinforcement is well known. In addition, according to our exclusion criteria, the characteristics of the two groups would have been very different and would not have allowed a pertinent comparison. It must be emphasized that we reported a series of consecutive patients. All the patients with placement of a prophylactic mesh during the study period were included in the study and no patient enrolled was lost for follow-up. The proven predictive factors of developing a PSH are: age >60, BMI > 25, female gender, APR performed by laparoscopy and fascia aperture >25 mm [9]. The patients included in our study were not at low risk of developing PSH: 21 (73 %) were older than 60, 20 (69 %) had a BMI > 25, 15 (52 %) were female and 24 (83 %) were operated by laparoscopy.
Other authors considered that improvement of the techniques currently employed for PSH prevention is needed and proposed the use of a 3D inversely funnel-shaped mesh made of polyvinylidene fluoride (PVDF) in intra-peritoneal position [40, 41]. This preformed device by design protects the notoriously endangered fascia gap at the ostomy site not only through local reinforcement but also by means of actual overlap along the diverted bowel and into the abdominal cavity. The first published study on the topic with regard to a 3D funnel mesh revealed immaculate results but only included 22 patients with a follow-up period of 11 months [40]. In a more recent study on 80 patients with a median follow-up of 21 months, PSH developed in 3 patients (3.75 %) and ostomy-related complication in 7 (8.75 %) but no mesh-related complications were encountered and none of the implants had to be removed [41]. Although PVDF is a non-coated mesh, no mesh-related complication was documented in a study with 344 cases of intra-peritoneally positioned implants [42]. However, it has to be stated that another publication described severely adverse events with regard to this material [43]. On animal model, it was also proven that PVDF mesh shrinks and that the percentage of shrinkage is equivalent to the percentage observed with a polypropylene mesh [44]. Therefore, the narrow funnel encircling the exiting colon might be an issue with longer follow-up because of a potential risk of fibrosis, stenosis or erosion.
Specific recommendations regarding the rationale of the material or the surgical technique for prosthetic reinforcement of stomas are lacking. Future trials will have to focus on the different techniques that include mesh implants, probe their advantages and evaluate the differences in outcome between these strategies.
Conclusion
Our study, with a median follow-up of 4 years, demonstrates that prevention of PSH by IPOM reinforcement of the abdominal wall at the time of stoma formation is a safe procedure and reduces the risk of developing PSH without added sceptic complications. The modified Sugarbaker technique is as easy to perform by laparoscopy than by laparotomy, does not require extensive dissection and is a totally aseptic procedure. It could be a more reliable surgical option than the “keyhole” technique usually used for PSH prevention. That last technique is marred by a high incidence of PSH and is not ideal either for treatment or prevention of PSH because retraction of the material currently induces a progressive widening of the central aperture that predispose to herniation. Further studies are mandatory to compare the different available techniques and meshes for PSH prevention.
References
Carne P, Robertson G, Frizelle F (2003) Parastomal hernia. Br J Surg 90:784–793
Jänes A, Cengiz Y, Israelsson L (2009) Preventing parastomal hernia with a prosthetic mesh: a 5-year follow-up of a randomized study. World J Surg 33:118–121
Serra-Aracil X, Bombardo-Junca J, Moreno-Matias J et al (2009) Randomized controlled prospective trial of the use of a mesh to prevent parastomal hernia. Ann Surg 249:583–587
Lopez-Cano M, Lozoya-Trujillo R, Quiroga S et al (2012) Use of a prosthetic mesh to prevent parastomal hernia during laparoscopic abdominoperineal resection: a randomized controlled trial. Hernia 16:661–667
Goligher JC, Duthie HL, Nixon HH (1984) Surgery of the anus, rectum and colon. Baillière Tindall, London
Helgstrand F, Rosenberg J, Kehlet H, Jorgensen LN, Wara P, Bisgaard T (2013) Risk of morbidity, mortality, and recurrence after parastomal hernia repair: a nationwide study. Dis Colon Rectum 56:1265–1272
Hansson BM, Slater NJ, van der Velden AS et al (2012) Surgical techniques for parastomal hernia repair: a systematic review of the litterature. Ann Surg 255:685–695
Lee L, Saleem A, Landry T, Latimer E, Chaudhury P, Feldman L (2014) Cost effectiveness of mesh prophylaxis to prevent parastomal hernia in patients undergoing permanent colostomy for rectal cancer. Am Coll Surg 218:82–91
Aquina C, Iannuzzi J, Probst C et al (2014) Parastomal hernia: a growing problem with new solutions. Dig Surg 31:366–376
Tam K, Wei P, Kuo L, Wu C (2010) Systematic review of the use of a mesh to prevent parastomal hernia. World J Surg 34:2723–2729
Moisidis E, Curiskis JI, Brooke-Cowden GL (2000) Improving the reinforcement of parastomal tissues with Marlex® mesh: laboratory study identifying solutions to stomal aperture distortion. Dis Colon Rectum 43:55–60
Muller-Stich B, Mehrabi A, Kenngott A et al (2009) Is a circular polypropylene mesh appropriate for application at the esophageal hiatus? Results from an experimental study in a porcine model. Surg Endosc 23:1372–1378
Muysoms F (2007) Laparoscopic repair of parastomal hernias with a modified Sugarbaker technique. Acta Chir Belg 107:476–480
Hauters P, Cardin JL, Lepere M, Valverde A, Cossa JP, Auvray S (2012) Prevention of parastomal hernia by intraperitoneal onlay mesh reinforcement at the time of stoma formation. Hernia 16:655–660
Moreno-Matias J, Serra-Aracil X, Darnell-Martin A et al (2009) The prevalence of parastomal hernia after formation of an end colostomy. A new clinico-radiological classification. Colorectal Dis 11:173–177
Bayer I, Kyzer S, Chaimoff C (1986) A new approach to primary strengthening of colostomy with Marlex mesh to prevent paracolostomy hernia. Surg Gynecol Obstet 163:579–580
Kelly M, Behrman S (2002) The safety and efficacy of prosthetic hernia repair in clean-contaminated and contaminated wounds. Am Surg 68:524–528
Hammond T, Huang A, Prosser K, Frye J, Williams N (2008) Parastomal hernia prevention using a novel collagen implant: a randomised controlled phase 1 study. Hernia 12:475–481
Wijeyekoon S, Gurusamy K, El-Gendy K, Chan C (2010) Prevention of parastomal herniation with biologic/composite prosthetic mesh: a systematic review and meta-analysis of randomized controlled trials. J Am Coll Surg 211:637–645
Fleshman A, Beck D, Hyman N et al (2014) Prospective, multicenter, randomized, controlled study of non-cross-linked porcine acellular dermal matrix fascial sublay for parastomal reinforcement in patients undergoing surgery for permanent abdominal wall ostomies. Dis Colon Rectum 57:623–631
Lambrecht J, Larsen S, Reiertsen O, Vaktskjold A, Julsrud L, Flatmark K (2015) Prophylactic mesh at end-colostomy construction reduces parastomal hernia rate: a randomized trial. Colorect Dis 17:191–197
Vierimaa M, Klintrup K, Biancari F et al (2015) Prospective randomized study on the use of a prosthetic mesh for prevention of parastomal hernia of permanent colostomy. Dis Colon Rectum 58:943–949
Nikberg M, Sverrisson I, Tsimogiannis K, Chabok A, Smedh K (2015) Prophylactic stoma mesh did not prevent parastomal hernias. Int J Colorectal Dis. doi:10.1007/s00384-015-2293-8
Ventham N, Brady R, Stewart R et al (2012) Prophylactic mesh placement of permanent stomas at index operation for colorectal cancer. Ann R Coll Surg Engl 94:569–573
Gogenur I, Mortensen J, Harvald T et al (2006) Prevention of parastomal hernia by placement of a polypropylene mesh at the primary operation. Dis Colon Rectum 49:1131–1135
Vijayasekar C, Marimuthu K, Jadhav V et al (2008) Parastomal hernia: is prevention better than cure ? Use of preperitoneal polypropylene mesh at the time of stoma formation. Tech Coloproctol 12:309–313
Biswas A, Marimuthu K, Mathew G (2015) Prevention of parastomal hernia using pre-peritoneal mesh—long term outcome of a prospective study. Acta Chir Belg 115:15–19
Williams N, Hotouras A, Bhan C, Murphy J, Chan C (2015) A case-controlled pilot study assessing the safety and efficacy of the Stapled Mesh stomA Reinforcement Technique (SMART) in reducing the incidence of parastomal herniation. Hernia 19:949–954
Lopez-Cano M, Serra-Aracil X (2015) Parastomal hernia prevention through laparoscopic modified Sugarbaker technique with composite mesh (Physiomesh). Cir Esp 91:331–334
Hansson B, De Hingh I, Bleichrodt R (2007) Laparoscopic parastomal hernia repair is feasible and safe: early results of a prospective clinical study including 55 consecutive patients. Surg Endosc 21:989–993
Safadi B (2004) Laparoscopic repair of parastomal hernias: early results. Surg Endosc 18:676–680
Muysoms F, Hauters P, Van Nieuwenhove Y, Huten N, Claeys D (2008) Laparoscopic repair of parastomal hernias: a multi-centre retrospective review and shift in technique. Acta Chir Belg 108:400–404
Hansson B, Bleichrodt R, de Hingh I (2009) Laparoscopic parastomal hernia repair using a keyhole technique results in a high recurrence rate. Surg Endosc 23:1456–1459
Mancini G, Mcclusky D, Khaitan L et al (2007) Laparoscopic parastomal hernia repair using a non-slit mesh technique. Surg Endosc 21:1487–1491
Hansson B, Morales-Conde S, Mussack T et al (2013) The laparoscopic modified Sugarbaker technique is safe and has a low recurrence rate: a multicenter cohort study. Surg Endosc 27:494–500
Gurmu A, Matthiessen P, Nilsson S et al (2011) The inter-observer reliability is very low at clinical examination of parastomal hernia. Int J Colorectal Dis 26:89–95
Cingi A, Cakir T, Sever A, Aktan AO (2006) Enterostomy site hernias: a clinical and computerized tomographic evaluation. Dis Colon Rectum 49:1559–1563
Seo Su Han, Kim Hee Jung, Seung Yeop Oh, Lee Jei Hee, Suh Kwang Wook (2011) Computed tomography classification for parastomal hernia. J Korean Surg Soc 81:111–114
Leblanc K, Bellanger D, Withaker J, Hausmann M (2005) Laparoscopic parastomal hernia repair. Hernia 9:140–144
Berger D (2008) Prevention of parastomal hernias by prophylactic use of a specially designed intraperitoneal onlay mesh (Dynamesh IPST). Hernia 12:243–246
Kohler G, Hofmann A, Lechner M et al (2015) Prevention of parastomal hernias with 3D funnel meshes in intraperitoneal onlay position by placement during initial stoma formation. Hernia. doi:10.1007/s10029-015-1380-7
Berger D, Bientzle M (2009) Polyvinylidene fluoride: a suitable mesh material for laparoscopic incisional and parastomal hernia repair! A prospective, observational study with 344 patients. Hernia 13:167–172
Fortelny R, Petter-Puchner A, Glaser K, Offner F, Benesch T, Rohr M (2010) Adverse effects of polyvinylidene fluoride-coated polypropylene mesh used for laparoscopic intraperitoneal onlay repair of incisional hernia. Br J Surg 97:1140–1145
Junge K, Binnebösel M, Rosch R, Jansen M, Kämmer D, Otto J, Schumpelick V, Klinge U (2009) Adhesion formation of a polyvinylidenfluoride/polypropylene mesh for intra-abdominal placement in a rodent animal model. Surg Endosc 23:327–333
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The study was not funded and the authors Philippe Hauters, Jean-Luc Cardin, Marc Lepere, Alain Valverde, Jean-Pierre Cossa, Sylvain Auvray, Dominique Framery, Constantin Zaranis declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Hauters, P., Cardin, JL., Lepere, M. et al. Long-term assessment of parastomal hernia prevention by intra-peritoneal mesh reinforcement according to the modified Sugarbaker technique. Surg Endosc 30, 5372–5379 (2016). https://doi.org/10.1007/s00464-016-4891-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4891-0