Abstract
Purpose
Parastomal herniation is reported in up to 50 % of patients with a colostomy. A prophylactic stoma mesh has been reported to reduce parastomal hernia rates. The aim of the study was to evaluate the rate of parastomal hernias in a population-based cohort of patients, operated with and without a prophylactic mesh at two different time periods.
Methods
All rectal cancer patients operated with an abdominoperineal excision or Hartmann’s procedure between 1996 and 2012 were included. From 2007, a prophylactic stoma mesh was placed in the retro-muscular plane. Patients were followed prospectively with clinical and computed tomography examinations.
Results
There were no differences with regard to age, gender, pre-operative albumin levels, ASA score, body mass index (BMI), smoking or type of surgical resection between patients with (n = 71) and without a stoma mesh (n = 135). After a minimum follow-up of 1 year, 187 (91 %) of the patients were alive and available for analysis. At clinical and computed tomography examinations, exactly the same parastomal hernia rates were found in the two groups, viz, 25 and 53 %, respectively (p = 0.95 and p = 0.18). The hernia sac contained omentum or intestinal loops in 26 (81 %) versus 26 (60 %) patients with and without a mesh, respectively (p = 0.155). In the multivariate analyses, high BMI was associated with parastomal hernia formation.
Conclusions
A prophylactic stoma mesh did not reduce the rate of clinically or computed tomography-verified parastomal hernias. High BMI was associated with an increased risk of parastomal hernia formation regardless of prophylactic stoma mesh.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Parastomal herniation, defined as an incisional hernia related to an abdominal wall stoma [1], is a common complication after stoma creation and is reported to occur in up to 50 % of patients fitted with a colostomy [2]. Although parastomal hernias are usually asymptomatic, they may cause discomfort, problems with poorly fitting stomal devices, skin excoriations, poor cosmesis and more rarely severe complications such as obstruction, strangulation and perforation [3]. In order to detect parastomal hernias, radiological methods, such as computerised tomography (CT) scan [4, 5] or ultrasonography [6], have been used. Since the risk of developing a parastomal hernia increases with time, at least a 1-year follow-up is proposed in clinical studies to detect most of the cases [7].
Patients with symptomatic parastomal hernias may achieve symptomatic relief with a stomalband, but eventually, up to one third of patients with a parastomal hernia may require surgery due to appearance of symptoms [8]. Suture repair with narrowing of the fascia and re-siting of the stoma have been applied with high recurrence rates, but using a prosthetic mesh is the gold standard of parastomal hernia repair today [9–12]. In 2004, excellent results were reported with a large-pore lightweight prophylactic stoma mesh [13], also after 5 years of follow-up [14]. Two more randomised trials have also supported these results [15, 16]. Even though it seems like a straightforward solution to the problem, the necessity of a prophylactic mesh in order to prevent parastomal hernia has not been proven in a large series of patients. Different clinics and surgeons have their own preferences and indications for the usage of mesh in stoma creation, and there has also been a lack of pre-defined endpoints regarding parastomal hernias. The Swedish national guideline does not comment on prophylactic mesh in patients planned for permanent colostomies.
The aim of this retrospective analysis, based on prospectively collected data, was to evaluate the risk of parastomal hernias in rectal cancer patients operated with and without a prophylactic mesh at two different time periods.
Methods
All patients operated with a Hartmann’s procedure (HA) and abdominoperineal excision (APE) between 1996 and 2012 at the Colorectal Unit, Västmanland’s Hospital Västerås, with a catchment area of 260,000, were included. Data regarding clinical characteristics, demographics, surgery, oncological treatment and follow-up were collected from a comprehensive, prospective database, set up in 1996 [17]. The clinical definition of a parastomal hernia entails a clear bulging around the stoma in the upright position or a palpable defect in the fascia. A radiologist blinded to the presence of a stoma mesh re-evaluated all available CT scans to detect parastomal hernias. One- and 3-year postoperative scans were used, and in addition, the last available CT scan was also assessed. The radiological definition of a parastomal hernia was a combination of that by Moreno-Matias et al. [5] and that used by Jänes et al. [4]. In summary, any intra-abdominal content protruding beyond the peritoneum or the presence of a hernia sac at least 1 year after operation was defined as a parastomal hernia.
Between 1996 and 2006, all permanent colostomies were created without the use of a prophylactic mesh. In 2007, based on the first published randomised study [13], a decision was taken to use a prophylactic stoma mesh in all rectal cancer patients operated electively. Two different meshes were used during the study period, the Vipro®(Ethicon, Norderstedt, Germany) mesh cut to 10 × 10 cm from 2007 until 2009 and the Parietex ProGrip™ (TYCO Healthcare) mesh 15 × 9 cm from 2010 onwards.
The study was approved by the local ethics’ committee of Uppsala University, Sweden.
Surgery
In all cases, the abdomen was accessed through a midline incision, and all patients had the stoma site marked on the left anterior rectus abdominis muscle by a stoma nurse. A standard trephine technique was used throughout the study period with the end stoma brought out through the rectus muscle. In patients who received a prophylactic stoma mesh, this was placed between the rectus abdominis muscle and the posterior rectus sheath. The opening was made just to let the bowel pass through the mesh, according to the technique described by Israelsson et al. [18]. The edges of the mesh around the bowel were not cut. The Vipro® mesh was sutured in place using non-absorbable stitches placed in its lateral corners. The midline incision was then closed with a continuous polydioxanone suture, which also included the fixation of the medial part of the mesh and the peritoneum. When a Parietex ProGrip™ mesh was implemented, the stackers were placed towards the rectus abdominis muscle. All procedures were performed by a limited number of experienced colorectal surgeons, and one surgeon (KS) performed or supervised 95 % of the procedures.
Follow-up
All patients were monitored by clinical examinations and radiology according to the follow-up routine, and the data were registered prospectively in the registry. Chest radiography and ultrasonography of the liver were performed as screening for distant metastases from 1996 until 2001. Since 2001, CT was performed at 1- and 3-year post-operative visits. Clinical examination of the abdomen and perineum was performed annually until 5 years had elapsed.
Follow-up was calculated from the date of operation to the date of the appearance of either a clinically or CT-verified parastomal hernia. For patients without a parastomal hernia, the date of the last clinical follow-up or the date of the latest performed CT of the abdomen was selected. All patients alive more than 1 year post-operatively have been assessed by either clinical examination and/or CT, and no patient was lost to follow-up.
Statistical analysis
The data were analysed using the IBM SPSS Statistics, version 21 (Chicago, IL, USA). Differences in proportions were calculated using the chi-square test or the t-test for independent samples. Fisher’s exact test was used for low numbers. A Cox’s proportional hazard regression model was performed in a stepwise fashion based on age, gender, American Society of Anesthesiologists (ASA) score, WHO performance status, cardiovascular disease, diabetes, BMI, smoking, postoperative chemotherapy and prophylactic stoma mesh in order to identify risk factors affecting parastomal hernia formation. To avoid small sample sizes in the multivariate Cox regression analysis, the ASA score and WHO performance status were re-coded into dichotomous variables (ASA 1–2 versus 3–4 and WHO performance grade 1–2 versus 3–4). A p-value of < 0.05 was considered as statistically significant.
Results
Of the 206 patients included, 145 (70 %) had undergone an APE and 61 (30 %) a HA. Their clinical characteristics are presented in Table 1. In total, 71 (34 %) patients had received a prophylactic stoma mesh.
There was no statistical difference between patients with and without a mesh as regards age, gender, preoperative albumin levels, ASA score, body mass index (BMI), smoking, cardiovascular and diabetic disease. There was a small statistical difference concerning the WHO performance scale with fitter patients in the mesh group (Table 1).
The surgical, pathological and follow-up data are presented in Table 2. A resection with a curative intent was performed in 165 (80 %) patients. In total, 71 (34 %) developed surgical complications and 5 (2 %) underwent a re-laparotomy, with no difference between the groups. There were no mesh-related complications, such as abscess, fistula formation, intestinal erosion or obstruction, necessitating mesh removal. The in-hospital mortality was 1.5 %.
After 12 months of follow-up, 187 patients (91 %) were alive and all were available for the analysis of parastomal hernia formation. The median follow-up time was 31 (12–202) months to the date of the appearance of either a clinically or CT-verified parastomal hernia or to the date of the last corresponding examinations in patients without a parastomal hernia. CT scans were available in 141 (75 %) patients.
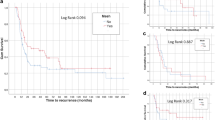
Parastomal hernia
There was no difference in the parastomal hernia frequency diagnosed on clinical examination or diagnosed on the CT scans as regards the usage of prophylactic stoma mesh or not (Table 3). When clinical and CT scan examinations were combined, there were still no differences observed. The hernia sac contained omentum or intestinal loops in 26 (81 %) versus 26 (60 %) patients with and without a mesh, respectively (p = 0.155). Four patients underwent an elective operation because of a parastomal hernia, with no difference between the groups (Table 3). There was no difference in the parastomal hernia rate between the two time periods 2007–2009 (Vipro mesh, n = 45) and 2010–2011 (ProGripmesh, n = 26; p = 0.647). In the Cox multivariate analysis presented in Table 4, the presence of a prophylactic stoma mesh did not affect the risk of parastomal hernia formation. A high BMI was the only independent risk factor for parastomal hernia formation when the analysis was performed with parastomal hernia detected at clinical examination and/or CT (Table 4). In an additional Cox regression analysis, risk factors for parastomal hernia formation at only clinical presentation were smoking (adjusted hazard ratio [HR] = 3.11, 95 % confidence interval [CI] = 1.22–7.94) and BMI (HR = 1.09, 95 % CI = 1.00–1.18).
Discussion
Prophylactic stoma mesh did not reduce the rate of parastomal hernias in this population-based study comparing two time periods, where the main difference between the compared groups was the use of a prophylactic mesh. No serious stoma-related complications occurred and no mesh was removed during the follow-up period. BMI was the only independent risk factor for parastomal hernia formation in the multivariate analysis. Patients with a prophylactic mesh were more fit (lower WHO performance score) but were more often treated with postoperative chemotherapy, which could explain the high frequency of parastomal hernia in the mesh group; however, in the multivariate analysis, chemotherapy was not associated with the development of a parastomal hernia.
To our knowledge, this study with 206 patients included is the largest on parastomal hernia mesh prophylaxis and exceeded the 129 patients in three small and heterogeneous, randomised studies [13, 15, 16]. These trials varied in case mix, age of participants, inclusion of emergency operations or not, type of stoma, type of mesh and its placement and outcome measures. The presented CT-verified parastomal hernia rate of 53 % in patients without a prophylactic mesh is comparable with previous reports [3, 7, 19]. A parastomal hernia rate of 53 % in patients with a prophylactic mesh is, however, remarkably much higher than in the small randomised clinical trials [14, 16] but somewhat lower than that reported in a recent small retrospective study with a parastomal hernia rate of 59 % detected with CT [20]. A parastomal hernia rate of 50 % in patients with a prophylactic mesh, compared with 94 % without, was also reported in a recent randomised trial; however, the mesh was placed in an intraperitoneal/inlay position [21]. In the present study, the mesh was, in all cases, placed in the retro-muscular plane and by a small number of experienced colorectal surgeons according to a standardised surgical technique.
It has been proposed that patients with a prophylactic mesh and a parastomal hernia may experience less discomfort [14]. At clinical examination in the present study, a parastomal hernia was detected in 25 % of the patients, without any difference between the groups. Most probably, only patients with obvious hernias and patients having local discomfort were detected, and in addition, there was no difference in the stoma-related re-operation rates between the groups. Furthermore, in the majority of patients with a prophylactic mesh, the stoma sac contained either omentum or intestinal loops (81 %), contradicting less discomfort and smaller hernias in the mesh group. The low rate of surgical correction of stomal hernias in Sweden reflects, in all probability, the restrictive policy common in this country, which in turn is based on a limited number of patients suffering from severe discomfort and characterized by old age and different co-morbidities: the policy is also coloured by the bad results previously achieved after stomal hernia surgery.
Smokers had an increased risk of developing a parastomal hernia at clinical examination. Smoking is a well-known risk factor for complications after surgery and has also been identified as a risk factor for recurrence after inguinal hernia surgery [22]. Smoking has been shown to decrease tissue oxygenation and impair proliferative response [23], which could result in larger parastomal hernias. Whether smoking has a causative effect in stomal hernia formation is unknown, but the multivariate analysis found no association with parastomal hernias.
Two different mesh sizes have been used during the study period, from 2007 to 2009, a 10 × 10 mesh was used, as described by Jänes et al. [14], and from 2010 onward, a 15 × 9-cm mesh, both being lightweight polypropylene meshes. There was no difference in the rate of parastomal hernia incidence between these two time periods. In the study by Serra-Aracil et al. [16], a 15 × 15-cm mesh was used and could be one explanation for having a parastomal hernia rate of 22 %; however, patients with a BMI above 35 kg/m2 and patients with disseminated disease were excluded, contrary to the present study.
Placing a prophylactic mesh in the retro-muscular plane was safe, and there were no stoma-related complications, as also previously reported [2, 14, 16, 19]. The mesh is, nevertheless, costly and the procedure prolongs the operative time. Hopefully, the ongoing randomised trials will clarify the role of prophylactic stoma mesh in preventing parastomal hernia.
The groups with and without a mesh were comparable in respect to clinical and surgical characteristics, but the low number of patients included (even though this is the largest study to date) and its retrospective non-randomised design are the main limitations of the present study. Parastomal hernia definition on CT is difficult and might have identified some false negative cases; however, the radiologist was blinded to the presence of mesh, and in addition, there was no difference in the parastomal hernia rates between the two groups at clinical examination. There were more patients in the no-stoma mesh group that only underwent clinical examinations, which explains the fact that the stoma hernia rate was lower when clinical and CT examinations were combined in the two groups. When clinical and CT examinations were compared separately, however, the hernia rates with or without a prophylactic stoma mesh were exactly the same, 25 and 53 %, respectively.
Conclusion
Half of the patients with a permanent colostomy developed a parastomal hernia, regardless of whether a prophylactic stoma mesh was implemented or not during the index operation. High BMI is a risk factor for parastomal hernia formation. Placement of a prophylactic stoma mesh outside clinical trials is now not recommended at our department until convincing results from large randomised trials have been presented.
References
Pearl RK (1989) Parastomal hernias. World J Surg 13(5):569–572
Shabbir J, Chaudhary BN, Dawson R (2012) A systematic review on the use of prophylactic mesh during primary stoma formation to prevent parastomal hernia formation. Color Dis 14(8):931–936. doi:10.1111/j.1463-1318.2011.02835.x
Shabbir J, Britton DC (2010) Stoma complications: a literature overview. Color Dis 12(10):958–964. doi:10.1111/j.1463-1318.2009.02006.x
Janes A, Weisby L, Israelsson LA (2011) Parastomal hernia: clinical and radiological definitions. Hernia 15(2):189–192. doi:10.1007/s10029-010-0769-6
Moreno-Matias J, Serra-Aracil X, Darnell-Martin A, Bombardo-Junca J, Mora-Lopez L, Alcantara-Moral M, Rebasa P, Ayguavives-Garnica I, Navarro-Soto S (2009) The prevalence of parastomal hernia after formation of an end colostomy. A new clinico-radiological classification. Color Dis 11(2):173–177. doi:10.1111/j.1463-1318.2008.01564.x
Gunnarsson U, Strigard K (2012) 3D intrastomal ultrasonography, an instrument for detecting stoma-related fistula. Tech Coloproctol 16(3):233–236. doi:10.1007/s10151-012-0821-x
Israelsson LA (2008) Parastomal hernias. Surg Clin N Am 88(1):113–125. doi:10.1016/j.suc.2007.10.003
Shellito PC (1998) Complications of abdominal stoma surgery. Dis Colon Rectum 41(12):1562–1572
Kasperk R, Klinge U, Schumpelick V (2000) The repair of large parastomal hernias using a midline approach and a prosthetic mesh in the sublay position. Am J Surg 179(3):186–188
Morris-Stiff G, Hughes LE (1998) The continuing challenge of parastomal hernia: failure of a novel polypropylene mesh repair. Ann R Coll Surg Engl 80(3):184–187
Rubin MS, Schoetz DJ Jr, Matthews JB (1994) Parastomal hernia. Is stoma relocation superior to fascial repair? Arch Surg 129(4):413–418, discussion 418-419
Stephenson BM, Phillips RK (1995) Parastomal hernia: local resiting and mesh repair. Br J Surg 82(10):1395–1396
Janes A, Cengiz Y, Israelsson LA (2004) Preventing parastomal hernia with a prosthetic mesh. Arch Surg 139(12):1356–1358. doi:10.1001/archsurg.139.12.1356
Janes A, Cengiz Y, Israelsson LA (2009) Preventing parastomal hernia with a prosthetic mesh: a 5-year follow-up of a randomized study. World J Surg 33(1):118–121. doi:10.1007/s00268-008-9785-4, discussion 122-113
Hammond TM, Huang A, Prosser K, Frye JN, Williams NS (2008) Parastomal hernia prevention using a novel collagen implant: a randomised controlled phase 1 study. Hernia 12(5):475–481. doi:10.1007/s10029-008-0383-z
Serra-Aracil X, Bombardo-Junca J, Moreno-Matias J, Darnell A, Mora-Lopez L, Alcantara-Moral M, Ayguavives-Garnica I, Navarro-Soto S (2009) Randomized, controlled, prospective trial of the use of a mesh to prevent parastomal hernia. Ann Surg 249(4):583–587. doi:10.1097/SLA.0b013e31819ec809
Smedh K, Olsson L, Johansson H, Aberg C, Andersson M (2001) Reduction of postoperative morbidity and mortality in patients with rectal cancer following the introduction of a colorectal unit. Br J Surg 88(2):273–277
Israelsson LA (2005) Preventing and treating parastomal hernia. World J Surg 29(8):1086–1089. doi:10.1007/s00268-005-7973-z
Carne PW, Robertson GM, Frizelle FA (2003) Parastomal hernia. Br J Surg 90(7):784–793. doi:10.1002/bjs.4220
Ventham NT, Brady RR, Stewart RG, Ward BM, Graham C, Yalamarthi S, Jones M, Daniel T (2012) Prophylactic mesh placement of permanent stomas at index operation for colorectal cancer. Ann R Coll Surg Engl 94(8):569–573. doi:10.1308/003588412X13373405386493
Lopez-Cano M, Lozoya-Trujillo R, Quiroga S, Sanchez JL, Vallribera F, Marti M, Jimenez LM, Armengol-Carrasco M, Espin E (2012) Use of a prosthetic mesh to prevent parastomal hernia during laparoscopic abdominoperineal resection: a randomized controlled trial. Hernia 16(6):661–667. doi:10.1007/s10029-012-0952-z
Burcharth J, Pommergaard HC, Bisgaard T, Rosenberg J (2014) Patient-related risk factors for recurrence after inguinal hernia repair: a systematic review and meta-analysis of observational studies. Surg Innov. doi:10.1177/1553350614552731
Sorensen LT (2012) Wound healing and infection in surgery: the pathophysiological impact of smoking, smoking cessation, and nicotine replacement therapy: a systematic review. Ann Surg 255(6):1069–1079. doi:10.1097/SLA.0b013e31824f632d
Acknowledgments
The authors wish to thank Dr. Staffan Täckström, Radiological Department, Västmanland’s Hospital Västerås, for reviewing the CT scans.
Compliance with ethical standards
The study was approved by the local ethics’ committee of Uppsala University, Sweden (Dnr 2013/467), and followed the Declaration of Helsinki guidelines.
Funding
This study was supported by a research grant from the County of Västmanland, Sweden.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nikberg, M., Sverrisson, I., Tsimogiannis, K. et al. Prophylactic stoma mesh did not prevent parastomal hernias. Int J Colorectal Dis 30, 1217–1222 (2015). https://doi.org/10.1007/s00384-015-2293-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-015-2293-8