Abstract
Background
Hernias around ostomies are a very common complication, exceeding 50%. Only a few studies deal with the prophylactic use of mesh to prevent parastomal hernia revealing promising results.
Patients and methods
Twenty-two patients undergoing elective rectal surgery with a permanent colostomy—one with an ileostomy and two needing surgical correction of a preexisting colostomy—were enrolled in a prospective study. A specially designed mesh made of polyvinylidene fluoride with a central whole and a funnel arising (Dynamesh IPST®) was prophylactically implanted using an intraperitoneal onlay technique. The patients were followed for a median of 11 (range 2–19) months by clinical examination every 3 months.
Results
No infection or any other adverse effect was observed, and no parastomal hernia or stoma protrusion could be detected clinically. Twelve patients had a routine computed tomography after 6 months, which also excluded any hernia formation.
Conclusion
The prophylactic use of Dynamesh IPST® is a safe and effective procedure preventing stoma complications such as hernia formation or prolapse, at least in the short run.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parastomal hernias are a common consequence of ostomies [1–4]. Sometimes, the frequency exceeds 50% if technical diagnostic tools such as computed tomography (CT) are used [5]. Clinical symptoms are a growing protrusion, pain, obstruction, or incarceration. Problems with stoma care sometimes exclude patients from any social activity. The combination of high frequency and clinical impairment have led to the question how to prevent parastomal hernias. Although the correct surgical technique is an inevitable precondition, surgical dogmas such as transrectal positioning have not been unequivocally proven [6–10]. From a pathogenetic point of view, the parastomal hernia should be interpreted as a special kind of incisional hernia, which is a biological disease based on disturbances of collagen synthesis [3, 11, 12]. Therefore, technical changes alone cannot dramatically reduce hernia incidence, which is clearly demonstrated for the epidemiology of incisional hernias. Also, the necessity of mesh-based techniques is generally accepted for the treatment of parastomal hernias [4].
So the only effective way to prevent fascial dehiscence around the stoma followed by parastomal hernia is by using mesh to augment the abdominal wall and prevent fascial dehiscence around the stoma. The availability of mesh with a central whole and a dome around it, which can be used intraperitoneally, was the precondition for a prospective study that should evaluate the rate of parastomal hernias after prophylactic implantation as well as the frequency of mesh-related complications.
Patients, materials, and methods
A twenty-five (nine women and sixteen men) patients were prospectively followed after different surgical procedures resulting in a permanent terminal colostomy or ileostomy. Surgical treatment and underlying diseases are summarized in Table 1. All elective patients between March 2006 and August 2007 who needed a permanent colostomy or ileostomy were enrolled and followed up prospectively every 3 months. No major contamination occurred during the primary procedure. Emergency cases were the only patients excluded during the study period.
Demographic and surgical data are given in Table 2.
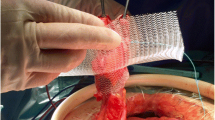
Dynamesh IPST® (FEG-Textiltechnik, Aachen, Germany) is a real mesh structure warp-knitted by polyvinylidene fluoride (PVDF) with a small amount of polypropylene on the parietal side. It has been experimentally shown that the mesh is well incorporated and effectively prevents adhesions to intestinal structures [13]. The mesh has some elasticity in both directions, comparable with the human abdominal wall [14]. The bowel loop is pulled through the central funnel, which has a diameter of 2 cm. The funnel is oriented to the abdominal cavity and must fit tightly around the bowel so that a stoma prolapse as well as the parastomal hernia should be prevented. The mesh is fixed by tacks only at the edges and around the stoma itself, as shown in Fig. 1, after laparoscopic implantation. The bowel loop pulled through the funnel is not fixed at the mesh. Dynamesh IPST® was used laparoscopically as well as in open procedures.
Final mesh position and fixation. Details of the surgical technique are given in “Patients, materials, and methods”
Results
As shown in Table 2, median follow-up was 11 months. One patient with liver metastases of a sigmoid carcinoma and ileus died in the early postoperative course due to hepatic failure. No parastomal hernia could be detected clinically up to that time. A CT scan was performed in 12 patients, which excluded a parastomal or incisional herniation. Furthermore, no outlet obstruction or evacuation problem occurred. Despite the fact that we used only meshes with a central whole diameter of 2 cm and sometimes the patients were quite obese [body mass index (BMI) ranged to 38], the large bowel could always be pulled through the funnel without any stenosis. Therefore, it should be emphasized that the funnel must fit tightly around the bowel, otherwise a prolapse through the funnel may occur. Funnels with larger diameters of 3 and 4 cm are commercially available but should be reserved for very obese patients with a dramatically thickened mesocolon.
Infectious complications have not been observed with this procedure. One patient after correction of a colostomy with stenosis and parastomal hernia and ileocecal resection due to Crohn’s disease of the colon and ileum developed a secondary small-bowel perforation with diffuse stercal peritonitis. She was further treated by daily planned reoperations for 1 week. The abdominal wall could be closed afterwards, leaving the prophylactic mesh in place, and the procedure was followed by primary wound healing. During a 1-year follow-up, the patient felt well and showed no signs of infection or other stoma-related complications. White blood cell count and serum levels of C-reactive protein routinely taken at the first follow-up 3 months postoperatively showed that all other patients also proved to be infection free.
Operating time was not lengthened by the intraperitoneal implantation of the prophylactic mesh, as shown in Table 2. In fact, the time demand for this procedure is less than 5 min.
Discussion
Prevention of parastomal hernias represents a primary and important aim when a permanent stoma is necessary. For pathogenetic reasons, a mesh-based augmentation seems to be inevitable to reach that aim [3, 11, 12]. In 2004 a randomized study showed the dramatic reduction of parastomal hernia formation after retromuscular positioning of an incised mesh [15, 16]. However, the number of patients studied was very small. Since that time, a few further prospective studies appeared, also demonstrating a very low incidence of parastomal hernias or other stoma complications associated with the procedure [17–19]. The meshes were implanted in a retromuscular or prefascial position. An often-used argument against the procedure is possible infection when the bowel, which is contaminated at the stapled end, is pulled through and comes into contact with the mesh. Only two minor infections have been observed in one series of 24 patients [18]. Other complications, such as stoma stenosis or prolapse, have not been described.
The technique in our series differs from the above-mentioned techniques by intraperitoneal positioning and application of a specially designed mesh that should not only prevent the hernia by overlapping the abdominal wall around the stoma but should also prevent a prolapse because the funnel is directed against the abdominal cavity, at least if the dome fits tightly around the bowel. The bowel pulled through that dome should be permanently kept in place as long as the bowel is tightly surrounded by the funnel. However, the outlet should be tested digitally to rule out any compressive effect. Until now, expectations have been completely fulfilled, and no hernia or other stomal complications have been observed. Despite the tight fitting of the mesh around the stomal loop, stenosis has not been observed.
Concerning the development of parastomal hernias, it should be kept in mind that the hernia can be detected in about 50% of cases during the first year postoperatively [5, 17]. Therefore, the absence of any hernia in our series clearly shows the short-term efficacy of the technique despite the low number of patients. The lack of any mesh-related infectious complications is also in accordance with previously published studies. Especially for incisional hernia repairs, intraperitoneal mesh placement during laparoscopic procedures was shown to be associated with a lower infection rate compared with open procedures, which are based on a retromuscular or prefascial mesh positioning [20–22]. Therefore, the intraperitoneal position may be more suitable if the mesh material allows direct contact with the viscera. Dynamesh IPST® is a real mesh structure made of PVDF, which is an inert material and has been shown not to induce adhesions to the bowel [13]. The small amount of polypropylene on the parietal side provides strong mesh incorporation and fixation. Recently, we demonstrated that PVDF is very suitable for laparoscopic correction of parastomal hernias using a sandwich technique with two meshes [23]. Despite local infections in two cases of that series, the meshes could be saved and kept in place without further problems [23]. Also, after performing more than 300 personal laparoscopic procedures for incisional hernias using PVDF, resistance to infections proved to be very high, supporting previously published results with other mesh materials. The clinical course of the patient after bowel injury and peritonitis treated by planned reoperations, which is described in the “Results” section also clearly demonstrates the resistance of the mesh material against infections, at least if the mesh is placed intraperitoneally, although that is only a case report of a single patient with gross contamination. In the meantime, we do not hesitate to use the prophylactic mesh in emergency cases with peritonitis if a takedown of the stoma is not planned. The Swedish group suggests similar principles and clearly recommends the general use of prophylactic mesh in emergency cases with major contamination [17]. They even implant prophylactic mesh in cases with a nonpermanent stoma.
A further advantage of the intraperitoneal onlay mesh (IPOM) technique is that there is no need to separate the abdominal wall layers. Local complications, such as hematomas or seromas, as a precondition of a later infection do not occur. Also, the time demand for mesh implantation is reduced using the IPOM technique compared with a retromuscular or prefascial location.
In conclusion, the prophylactic use of an IPOM to prevent parastomal hernias proved to be safe and effective, with no hernias after a mean observation period of 11 months. Infectious complications have not been observed to this point, nor has outlet obstruction. The procedure can easily be performed laparoscopically or during an open procedure for permanent terminal large- or small-bowel ostomies.
References
Leslie D (1984) The parastomal hernia. Surg Clin North Am 64:407–415
Cheung MT (1995) Complications of an abdominal stoma: an analysis of 322 stomas. Aust N Z J Surg 65:808–811
Kasperk R, Willis S, Klinge U, Schumpelick V (2002) Update on incisional hernia. Parastomal hernia. Chirurg 73:895–898
Carne PW, Robertson GM, Frizelle FA (2003) Parastomal hernia. Br J Surg 90:784–793
Cingi A, Cakir T, Sever A, Aktan AO (2006) Enterostomy site hernias: a clinical and computerized tomographic evaluation. Dis Colon Rectum 49:1559–1563
Leong AP, Londono-Schimmer EE, Phillips RK (1994) Life-table analysis of stomal complications following ileostomy. Br J Surg 81:727–729
Londono-Schimmer EE, Leong AP, Phillips RK (1994) Life table analysis of stomal complications following colostomy. Dis Colon Rectum 37:916–920
Ortiz H, Sara MJ, Armendariz P, de Miguel M, Marti J, Chocarro C (1994) Does the frequency of paracolostomy hernias depend on the position of the colostomy in the abdominal wall? Int J Colorectal Dis 9:65–67
Ortiz H (1995) Does the difference in muscle structure of the rectus abdominis muscle of patients wearing a colostomy or ileostomy explain the different frequency of parastomal hernias? Int J Colorectal Dis 10:55
Sjodahl R, Anderberg B, Bolin T (1988) Parastomal hernia in relation to site of the abdominal stoma. Br J Surg 75:339–341
Klinge U, Si ZY, Zheng H, Schumpelick V, Bhardwaj RS, Klosterhalfen B (2001) Collagen I/III and matrix metalloproteinases (MMP) 1 and 13 in the fascia of patients with incisional hernias. J Invest Surg 14:47–54
Klinge U, Conze J, Krones CJ, Schumpelick V (2005) Incisional hernia: open techniques. World J Surg 29:1066–1072
Klinge U, Klosterhalfen B, Ottinger AP, Junge K, Schumpelick V (2002) PVDF as a new polymer for the construction of surgical meshes. Biomaterials 23:3487–3493
Junge K, Klinge U, Prescher A, Giboni P, Niewiera M, Schumpelick V (2001) Elasticity of the anterior abdominal wall and impact for reparation of incisional hernias using mesh implants. Hernia 5:113–118
Janes A, Cengiz Y, Israelsson LA (2004) Randomized clinical trial of the use of a prosthetic mesh to prevent parastomal hernia. Br J Surg 91:280–282
Janes A, Cengiz Y, Israelsson LA (2004) Preventing parastomal hernia with a prosthetic mesh. Arch Surg 139:1356–1358
Israelsson LA (2005) Preventing and treating parastomal hernia. World J Surg 29:1086–1089
Gogenur I, Mortensen J, Harvald T, Rosenberg J, Fischer A (2006) Prevention of parastomal hernia by placement of a polypropylene mesh at the primary operation. Dis Colon Rectum 49:1131–1135
Marimuthu K, Vijayasekar C, Ghosh D, Mathew G (2006) Prevention of parastomal hernia using preperitoneal mesh: a prospective observational study. Colorectal Dis 8:672–675
Cassar K, Munro A (2002) Surgical treatment of incisional hernia. Br J Surg 89:534–545
Le Blanc KA (2005) Incisional hernia repair: laparoscopic techniques. World J Surg 29:1073–1079
Pierce RA, Spitler JA, Frisella MM, Matthews BD, Brunt LM (2007) Pooled data analysis of laparoscopic vs. open ventral hernia repair: 14 years of patient data accrual. Surg Endosc 21:378–386
Berger D, Bientzle M (2007) Laparoscopic repair of parastomal hernias: a single surgeon’s experience in 66 patients. Dis Colon Rectum 50:1661–1668
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Berger, D. Prevention of parastomal hernias by prophylactic use of a specially designed intraperitoneal onlay mesh (Dynamesh IPST®). Hernia 12, 243–246 (2008). https://doi.org/10.1007/s10029-007-0318-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-007-0318-0