Abstract
Background
Jejunostomy catheters for jejunal feeding are an effective method to improve nutritional status in malnourish patients. However, this procedure is commonly being performed using an open approach, which can be associated with more postoperative pain and prolonged recovery. The objective of this study was to assess the outcomes of patients who underwent placement of feeding jejunostomy using a laparoscopic approach.
Methods
A retrospective review was performed of patients who underwent laparoscopic jejunostomy tube placement between 1998 and 2014. Main outcome measures included indication for catheter placement, rate of conversion rate to open surgery, perioperative and late morbidity and in-hospital mortality.
Results
Two hundred and ninety-nine consecutive patients underwent laparoscopic jejunostomy during the study period. The mean age was 64 years, and 81 % of patients were male. The mean BMI was 26.2 kg/m2. The most common indications for catheter placement were resectable esophageal cancer (78 %), unresectable esophageal cancer (10 %) and gastric cancer (6 %). There were no conversions to open surgery. The 30-day complication rate was 4.0 % and included catheter dislodgement (1 %), intraperitoneal catheter displacement (0.7 %), catheter blockage (1 %) or breakage (0.3 %), site infection requiring catheter removal (0.7 %) and abdominal wall hematoma (0.3 %). The late complication rate was 8.7 % and included jejuno-cutaneous fistula (3.7 %), jejunostomy tube dislodgement (3.3 %), broken or clogged J-tube (1.3 %) and small bowel obstruction (0.3 %). The 30-day mortality was 0.3 % for a patient with stage IV esophageal cancer who died in the postoperative period secondary to respiratory failure.
Conclusion
In this large consecutive series of feeding jejunostomy, the laparoscopic approach is feasible and safe and associated with a low rate of small bowel obstruction and no intraabdominal catheter-related infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic feeding jejunostomy is a well-established technique for administrating enteral nutrition after major upper gastrointestinal operations [1–3]. For patients requiring prolonged nutritional maintenance or supplementation, the enteral route has many proven benefits over parenteral nutrition [4–6]. These benefits include improved immune function, preserved gastrointestinal mucosal integrity, decreased infectious complications and improved postoperative outcomes [4, 5, 7, 8]. Furthermore, enteral feeding avoids the risks associated with central venous catheter infection and sepsis. In the setting of patients with esophagogastric malignancy, or any form of gastric outlet obstruction, gastric feeding is not always optimal. In these circumstances, jejunal feeding is the best route for enteral nutritional.
With advancements in minimally invasive techniques, laparoscopic jejunostomy tube placement has become increasingly common. Jejunostomy tube placement often occurs as an adjunct during staging laparoscopy for patients with upper GI malignancies [9, 10]. The aim of this study was to examine the outcomes of a large series of laparoscopic feeding jejunostomy tube placement.
Methods
A retrospective chart review was performed on patients who underwent laparoscopic feeding jejunostomy between 1998 and 2014. Clinical data collected included patient demographics (age, gender, body mass index); indications for jejunostomy feeding tube placement; comorbidities including coronary artery disease, hypertension, diabetes, dyslipidemia; and history of prior abdominal surgery. Main outcome measures included intraoperative complications, 30-day morbidity and mortality and late (>30 days) complications. Laparoscopic jejunostomy performed for resectable esophageal cancer was performed in conjunction with laparoscopic staging procedure.
A review of the literature was also performed to identify publications reporting outcomes of laparoscopic jejunostomy tube placement. A PubMed search was performed utilizing keywords “laparoscopic,” “jejunostomy” and “feeding jejunostomy.” Non-English publications, case reports and studies with <20 patients were excluded. Three studies were also excluded due to a combined analysis of laparoscopic jejunostomy and gastrostomy catheter placement. A total of 10 articles remained with clinical data on postoperative morbidity and mortality.
Surgical technique
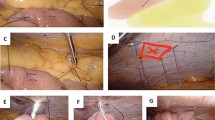
After insufflation, three abdominal trocars are placed. If patients are undergoing feeding jejunostomy placement in conjunction with another minimally invasive surgical procedure, trocar sites may be adjusted and utilized for both operations. The patient is placed in 30° reverse Trendelenburg position, and the greater omentum is reflected superiorly to expose the transverse mesocolon. The proximal jejunum is identified, and a location is selected approximately 30 cm distal to the ligament of Treitz. The selected loop of bowel is sutured to the anterior abdominal wall in the left upper quadrant (Fig. 1) using the Endostitch device (Covidien, Norwalk, Connecticut, USA).
A 15-gage introducer needle is inserted into the jejunum and followed by placement of a guidewire into the efferent jejunal limb (Fig. 2). The introducer needle is then removed. A 10-French jejunostomy catheter (Barone Jejunostomy set, Cook Medical, Bloomington, IN, USA) is then introduced over the guidewire for approximately 12 inches into the efferent limb. A jejunal Witzel tunnel is constructed around the jejunal catheter entry point (Fig. 3A). The jejunum surrounding the jejunostomy catheter is then secured to the abdominal wall with a purse-string suture and secured using the Ti-knot device (Fig. 3B). An additional anchoring suture is placed 1 cm distal to the catheter insertion site to prevent potential volvulus of the small bowel. Patency and confirmation of intraluminal placement of the feeding catheter are tested by injection of 10 ml of air into the jejunostomy catheter and observe for appropriate insufflation of the small bowel. The jejunostomy catheter is secured to the abdominal wall with 0-silk suture at 3 separate sites.
Enteral feeding is commonly started 24 h after feeding tube placement. Jejunostomy tube is left in place until the patient is able to tolerate oral nutrition and/or improving nutritional parameters.
Results
A total of 299 patients underwent laparoscopic placement of a feeding jejunostomy during the study period. Mean age was 64 years with 81 % of patients being male (Table 1). The majority of patients had undergone previous abdominal surgery (63 %), and hypertension was the most common comorbidity (39 %). The most common indication for catheter placement was resectable esophageal cancer (78 %) followed by unresectable esophageal cancer (10 %) and gastric cancer (6 %).
There were no conversions to open surgery and no intraoperative complications. The 30-day complication rate was 4.0 % (Table 2). Three patients had external catheter dislodgement (1 %), and two patients had intraperitoneal displacement (0.7 %). Three patients experienced catheter blockage requiring a visit to the emergency department (1 %), and one patient had a broken feeding tube requiring replacement (0.3 %). There were two tube-site infections requiring early removal of the catheter (0.7 %) and an abdominal wall hematoma that resolved spontaneously (0.3 %). The in-hospital mortality was 0.3 %. One patient had stage IV esophageal cancer and died in the postoperative period secondary to respiratory failure.
The late complication rate was 8.7 % consisting of eleven patients with jejunal-cutaneous fistulas (3.7 %), nine of which required reoperation; ten patients with J-tube dislodgement (3.3 %); four patients with broken or clogged J-tube (1.3 %); and one patient with small bowel obstruction (0.3 %).
Discussion
Laparoscopic feeding jejunostomy was introduced in 1990 by O’Regan et al. and has subsequently become a well-established technique [2, 11–15]. There are still few large studies reporting outcomes of laparoscopic jejunostomy placement. In this report, we present a large consecutive series of laparoscopic jejunotomy in 299 patients. The most common indication for laparoscopic jejunostomy placement was esophagogastric carcinoma. There were no intraoperative complications, a 30-day morbidity rate of 3.7 % and a low in-hospital mortality rate of 0.3 %. The late complication rate was 8.7 %, comprised primarily of J-tube dislodgement (3.3 %) and jejunal fistula (3.7 %).
Different methods have been described of retracting and anchoring the jejunum to the anterior abdominal wall. Some studies describe the use of T-fasteners [10, 16–19] or transabdominal sutures [11, 20] to keep the jejunum secured. It is currently our preference to use intracorporeal sutures to secure the jejunum to the abdominal wall. This was a change from our initial technique of using transfascial sutures. We noted that transfascial sutures could be inadvertently cut when inserting the introducer needle through the abdominal wall, which resulted in two cases of early intraperitoneal displacement of the jejunostomy tube. Intracorporeal suturing to anchor the jejunum to the anterior wall may reduce the risk of early catheter intraperitoneal displacement. Careful and thorough external suturing and taping of the catheter also lowered our rate of early accidental displacement.
Another complication we experienced in this series was catheter site infection. The majority of our site infections were superficial and self-limiting, but two severe abdominal wall site infections with leakage of jejunal content required early catheter removal (0.7 %). Site infection is commonly cited as a frequent source of postoperative morbidity related to jejunal feeding tubes [10, 21]. A review of the literature reported an infection rate ranging from 0 to 12.5 % (Table 3). In our initial method, upon placement of the jejunostomy catheter, a purse-string suture was then performed around the jejunostomy catheter to secure the tube to the anterior abdominal wall. These severe site infections (2 of 112 cases, 1.8 %) prompted us to alter our technique with placement of a Witzel tunnel around the point of entry of the jejunostomy catheter into the jejunum. Since instituting this technical change, no other severe superficial site infections were encountered. During construction of the Witzel tunnel, care must be taken to avoid suturing too much of the jejunum as it can lead to luminal obstruction at the catheter insertion site. Catheter blockage or clogging was typically caused by inappropriate medication administration through the catheter. Hospital staff must be educated regarding the use of liquid or dissolved medication only. Additionally, the catheter should be flushed after each use to minimize the rate of tube clogging.
A common late complication is jejunal-cutaneous fistula, particularly when the tube is required for long-term enteral access. We encourage removal of the tube as soon as patients can tolerate oral intake to prevent development of this complication. In our experience, the Witzel technique has led to a decrease in the rate of late fistula formation. J-tube dislodgement was the second most common late complication (3.5 %). The longer the J-tube is left in place, the higher the likelihood of becoming dislodged. Several studies have examined outcomes of feeding gastrostomy and show that tube-related complications are common in patients receiving long-term home enteral nutrition [22, 23]. The reason for dislodgement of the catheter is related to the displacement of the sutures that were used to secure the jejunostomy catheter to the abdominal wall. It is important to instruct the patient and their family members who care for the tube to correctly tape the catheter to the abdominal wall and also alert the healthcare provider when these sutures become dislodge from the abdominal wall.
In a review of the literature, we found 10 publications reporting the outcome of laparoscopic jejunostomy tube placement (Table 3). Published rates of postoperative mortality ranged from 0 to 11 %; however, the majority of studies reported no mortalities. The conversion rate to open surgery ranged between 0 and 12.5 % [24]. The overall morbidity rate ranged between 4 and 25 %. The most common complications described were similar to those reported in our study: catheter dislodgement (0–20 %), catheter blockage (0–13 %), site infection (0–12.5 %) and leaks (0–2.6 %) [1, 2, 9, 10, 17, 21, 25–28].
There are some limitations in this study. This study is a retrospective review and therefore may lack the rigor in data collection as in a prospective study. Preoperative factors such as neoadjuvant chemoradiation were not collected, which may have an impact on the risk of higher perioperative complications. The current technique was not applied uniformly throughout the entire series. Alterations in technique were applied throughout the clinical series in response to the development of certain complication. Despite these limitations, this study reports the outcomes of one of the largest series of laparoscopic jejunostomy catheter placement to date.
Conclusion
In this large consecutive series of feeding jejunostomy, we found laparoscopic placement of the feeding jejunostomy to be safe with a low perioperative morbidity. Jejunostomy placement during laparoscopic staging is a safe and feasible technique that ensures optimization of nutritional status for management of patients with esophagogastric malignancy. Several important alterations in technique were implemented in this series in an effort to reduce the morbidity associated with laparoscopic placement of feeding jejunostomy catheter.
References
Nguyen NT, Schauer PR, Wolfe BM, Ho HS, Luketich JD (2000) Laparoscopic needle catheter jejunostomy. Br J Surg 87:482–483
Han-Geurts IJ, Lim A, Stijnen T, Bonjer HJ (2005) Laparoscopic feeding jejunostomy: a systematic review. Surg Endosc 19:951–957
Torres Junior LG, de Vasconcellos Santos FA, Correia MI (2014) Randomized clinical trial: nasoenteric tube or jejunostomy as a route for nutrition after major upper gastrointestinal operations. World J Surg 9:2241–2246.
Braga M, Gianotti L, Nespoli L, Radaelli G, Di Carlo V (2002) Nutritional approach in malnourished surgical patients: a prospective randomized study. Arch Surg 137:174–180
Kudsk KA, Tolley EA, DeWitt RC, Janu PG, Blackwell AP, Yeary S, King BK (2003) Preoperative albumin and surgical site identify surgical risk for major postoperative complications. JPEN J Parenter Enteral Nutr 27:1–9
Gianotti L, Braga M, Vignali A, Balzano G, Zerbi A, Bisagni P, Di Carlo V (1997) Effect of route of delivery and formulation of postoperative nutritional support in patients undergoing major operations for malignant neoplasms. Arch Surg 132:1222–1229 (discussion 1229–1230)
Moore FA, Feliciano DV, Andrassy RJ, McArdle AH, Booth FV, Morgenstein-Wagner TB, Kellum JM Jr, Welling RE, Moore EE (1992) Early enteral feeding, compared with parenteral, reduces postoperative septic complications. The results of a meta-analysis. Ann Surg 216:172–183
Moore FA, Moore EE, Haenel JB (1995) Clinical benefits of early post-injury enteral feeding. Clin Intensive Care 6:21–27
Jenkinson AD, Lim J, Agrawal N, Menzies D (2007) Laparoscopic feeding jejunostomy in esophagogastric cancer. Surg Endosc 21:299–302
Ben-David K, Kim T, Caban AM, Rossidis G, Rodriguez SS, Hochwald SN (2013) Pre-therapy laparoscopic feeding jejunostomy is safe and effective in patients undergoing minimally invasive esophagectomy for cancer. J Gastrointest Surg 17:1352–1358
O’Regan PJ, Scarrow GD (1990) Laparoscopic jejunostomy. Endoscopy 22:39–40
Jimenez Rodriguez RM, Lee MR, Pigazzi A (2012) Trocar guided laparoscopic feeding jejunostomy: a simple new technique. Surg Laparosc Endosc Percutan Tech 22:e250–e253
Ilczyszyn A, El-Medani F, Gupta S (2012) Laparoscopic feeding jejunostomy: description of a modified technique with results. Surgeon 10:59–62
Ellis LM, Evans DB, Martin D, Ota DM (1992) Laparoscopic feeding jejunostomy tube in oncology patients. Surg Oncol 1:245–249
Eltringham WK, Roe AM, Galloway SW, Mountford RA, Espiner HJ (1993) A laparoscopic technique for full thickness intestinal biopsy and feeding jejunostomy. Gut 34:122–124
Duh QY, Way LW (1993) Laparoscopic jejunostomy using T-fasteners as retractors and anchors. Arch Surg 128:105–108
Duh QY, Senokozlieff-Englehart AL, Siperstein AE, Pearl J, Grant JP, Twomey PL, Gadacz TR, Prinz RA, Wolfe BM, Soper NJ et al (1995) Prospective evaluation of the safety and efficacy of laparoscopic jejunostomy. West J Med 162:117–122
Edelman DS, Unger SW (1994) Laparoscopic gastrostomy and jejunostomy: review of 22 cases. Surg Laparosc Endosc 4:297–300
Murayama KM, Johnson TJ, Thompson JS (1996) Laparoscopic gastrostomy and jejunostomy are safe and effective for obtaining enteral access. Am J Surg 172:591–594 (discussion 594–595)
Bobowicz M, Makarewicz W, Polec T, Kopiejc A, Jastrzebski T, Zielinski J, Jaskiewicz J (2011) Totally laparoscopic feeding jejunostomy—a technique modification. Videosurg Miniinv 6:256–260
Allen JW, Ali A, Wo J, Bumpous JM, Cacchione RN (2002) Totally laparoscopic feeding jejunostomy. Surg Endosc 16:1802–1805
Crosby J, Duerksen D (2005) A retrospective survey of tube-related complications in patients receiving long-term home enteral nutrition. Dig Dis Sci 50:1712–1717
Alivizatos V, Gavala V, Alexopoulos P, Apostolopoulos A, Bajrucevic S (2012) Feeding tube-related complications and problems in patients receiving long-term home enteral nutrition. Indian J Palliat Care 18:31–33
Himpens JM (2013) Comment on: laparoscopic sleeve gastrectomy compared to other bariatric surgical procedures: a systematic review of randomized trials. Surg Obes Relat Dis 9:829–830
Liu YY, Liao CH, Chen CC, Tsai CY, Liu KH, Wang SY, Fu CY, Yeh CN, Yeh TS (2014) Single-incision laparoscopic-assisted jejunostomy tube placement. J Laparoendosc Adv Surg Tech Part A 24:22–27
Senkal M, Koch J, Hummel T, Zumtobel V (2004) Laparoscopic needle catheter jejunostomy: modification of the technique and outcome results. Surg Endosc 18:307–309
Sangster W, Swanstrom L (1993) Laparoscopic-guided feeding jejunostomy. Surg Endosc 7:308–310
Hotokezaka M, Adams RB, Miller AD, McCallum RW, Schirmer BD (1996) Laparoscopic percutaneous jejunostomy for long term enteral access. Surg Endosc 10:1008–1011
Acknowledgments
This study was supported in part by a grant from Cook Medical.
Disclosures
Dr. Ninh Nguyen received an educational grant paid to the Department of Surgery, University of California, Irvine from Cook Group Inc. (Cook Medical). Dr. Monica Young, Dr. Hung Troung, Alana Gebhart and Anderson Shih have no conflict of interests or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Young, M.T., Troung, H., Gebhart, A. et al. Outcomes of laparoscopic feeding jejunostomy tube placement in 299 patients. Surg Endosc 30, 126–131 (2016). https://doi.org/10.1007/s00464-015-4171-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4171-4