Abstract
Background
Enteral feeding devices have gained popularity since the beneficial effects of enteral nutrition have been clarified. Laparoscopic placement of a feeding jejunostomy is the most recently described enteric access route. In order to classify current surgical techniques and assess evidence on safety of laparoscopic feeding jejunostomy, a systematic review was performed.
Methods
The electronic databases Medline, Cochrane, and Embase were searched. Reference lists were checked and requests for additional or unpublished data were sent to authors. Outcome measures were surgical technique and catheter-related complications.
Results
Enteral access for feeding purposes can be effectively achieved by laparoscopic jejunostomy. Laparoscopic jejunostomy can be accomplished by either total laparoscopic or laparoscopic-aided techniques. The most experience was obtained with total laparoscopic placement. Which technique to apply should depend on the surgeon’s expertise. Conversion rate is similar to other laparoscopic procedures. Complications can be serious and therefore strict patient selection should be warranted.
Conclusion
Laparoscopic feeding jejunostomy is a viable method to obtain enteral access with the advantages of minimally invasive surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The enteral route is the preferred route for nutrition administration in malnourished or oncologic patients and for patients in the postoperative period [4, 5, 19, 28]. Various access routes for enteral nutrition are available, but for the purpose of long-term tube feeding preference is given to percutaneous endoscopic gastrostomy or operative gastrostomy or jejunostomy. Since minimally invasive techniques have many advantages, increasing attention is paid to laparoscopic or laparoscopic-assisted placement of a feeding jejunostomy [8, 20, 27, 35, 41]. Laparoscopic feeding jejunostomy was first described 1990 [34]. After several failed attempts to perform a percutaneous endoscopic gastrostomy in a quadriplegic patient on ventilatory support, the authors succeeded in placing a laparoscopic feeding jejunostomy. Following this primary report many others started to apply this technique and described their personal experience. Feeding jejunostomy is, however, associated with serious and less-serious complications [6, 23]. The laparoscopic technique is regarded as a safe procedure and an alternative to open feeding jejunostomy [43].
Following an extensive literature search to identify relevant literature and their references, this systematic review aims to classify current surgical techniques and assess evidence on safety of laparoscopic feeding jejunostomy.
Methods and techniques
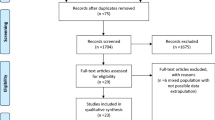
The Embase, Medline, and Cochrane databases from 1981 through April 2004 were searched by two independent reviewers, using the keywords “laparoscopic” and “jejunostomy” with the Boolean operators “and” and “or.” The search was restricted to titles and abstracts. There were no language restrictions. Authors were contacted for additional data on outcomes not reported in publications. Both independent reviewers extracted data. Discrepancies were resolved by discussion and consensus. From each study data were collected on indication for placement, surgical technique, and catheter-related complications. Surgical technique was categorized as total laparoscopic and laparoscopic aided. Outcomes potentially related to placement and usage of feeding jejunostomy included wound infection, dislodgement, obstruction, leakage, bowel perforation, volvulus, and reoperation.
Results
Twenty-three studies were identified [1, 2, 9, 10, 12–15, 17, 22, 25, 29, 30, 32–34, 37–39, 42–44]. Two studies were excluded because only a technique description was given without patient characteristics [22, 44]. Attempts to obtain unpublished data from the authors were unsuccessful. One study was excluded since both laparoscopic gastrostomy and jejunostomy were described and no distinction was made in groups regarding results [11]. Sixteen studies had a prospective study design [1, 2, 9, 10, 12, 15, 17, 22, 25, 29, 32, 33, 34, 38, 42]. The earliest study dated from 1990 [34]. Additional unpublished data were obtained for two of the studies [29, 33].
Underlying pathology
Indications for placement of a feeding jejunostomy differed between studies (Table 1). Nine studies included upper digestive carcinoma. Eight studies included neurological deficit and seven studies trauma resulting in neurological damage. Malnutrition was an indication in four studies. Motility disorders of the digestive tract were mentioned in two studies and gastropareses of different origins in three. In three studies a laparoscopic jejunostomy was placed as an adjunct to surgery and postoperative recovery. Four studies mentioned diverse reasons for applying a feeding jejunostomy.
Technique
Several techniques for placement of feeding jejunostomy were used. One study does not describe method of placement in the jejunostomy group but uses T-fasteners in the gastrostomy group, making it likely the same technique was used in the jejunostomy group [13]. An overview is given in Table 2. The techniques were classified into two groups: the total laparoscopic method and the laparoscopic-aided method, which includes exteriorizing of the small bowel.
Feeding jejunostomy using a total laparoscopic approach was applied in the majority of the studies [1, 2, 9, 10, 25, 30, 32, 33, 34, 39, 42, 43]. A further distinction was made into three different methods of retracting and anchoring the jejunum to the anterior abdominal wall (table 2).
The first technique uses transabdominal sutures [1, 2, 25, 33, 37, 39]. After the usual establishment of a pneumoperitoneum and placement of three trocars, three or four transabdominal sutures are placed in a diamond configuration incorporating seromuscular jejunal wall and anterior abdominal wall. A feeding tube or a needle catheter is inserted through the center of the array of sutures. In one study one of the transabdominal sutures is used [34] to attain a seal around the feeding catheter to prevent leakage. In another study adjacent intracorporeal sutures were placed around the catheter [25, 33]. In the remaining studies, no fixation is used. The transabdominal sutures are tied over bolsters to prevent skin damage. After 2 weeks the jejunum is expected to be adherent to the abdominal wall and the bolsters and sutures are removed. Sangster et al. applied the transabdominal suturing technique only in the beginning of their study [39]. Allen in his study used transabdominal sutures but tied them at fascia level [2].
In four studies T-fasteners are employed that were originally developed for fixation of the anterior gastric wall in percutaneous gastrostomy [9, 10, 13, 30]. The T-fastener consists of a T-bar with a suture attached to its center. It is inserted by a slotted needle and dislodged into the jejunal lumen by a stylet. Four T-fasteners are introduced percutaneously into the jejunum serving to retract and anchor the small bowel to the abdominal wall (Fig. 1A–E). They are placed in a diamond-like configuration. A needle catheter can be placed through the center of the sutures. The authors do not describe if and how they secure the catheter to the jejunum. After 2 weeks the T-fasteners are removed.
(A) The proximal jejunum and the ligament of Treitz are identified by lifting the transverse mesocolon and running the small bowel with the graspers. (B) The T-fastener is introduced percutaneously and discharged into the lumen from the slotted needle by the stylet. (C) Four T-fasteners are used to retract the antimesenteric jejunal wall. A J-wire is introduced into the lumen of the jejunum through an 18-gauge needle. (D) The jejunostomy catheter is placed through the peel-away introducer, which is then removed. (E) The T-fasteners and the jejunostomy catheter are secured to the abdominal wall. The T-fastener sutures are cut 2 weeks later, and the metal T-bars are allowed to pass in the stool. [By permission of BMJ Publishing Group: Duh QY, Senokozlieff-Englehart AL, Siperstein AE (1995) Prospective evaluation of the safety and efficacy of laparoscopic jejunostomy. WJM 162: 117–122.]
Senkal et al. and Nguyen et al. use three trocars for performing jejunostomy [32, 42]. The jejunum is fixated to the abdominal wall by an intracorporeal placed purse-string suture and additional anchoring sutures between jejunum and abdominal wall (Fig. 2).
In laparoscopic-aided feeding jejunostomy, placement of the catheter is established extracorporeally by means of a small abdominal incision through which the jejunum is retracted [12, 14, 15, 17, 29, 37, 38]. Ellis et al. advocate use of a 4-cm-wide abdominal midline incision allowing extraction of the chosen catheter entry site on the jejunum [14]. They propose serosal tunnelling of the feeding catheter to minimise the risk of an enterocutaneous fistula. The jejunum is then fixed to the abdominal wall by interrupted sutures. Rosser and colleagues also use a 4-cm skin incision, but the abdominal fascia is left intact [38] (Fig. 3A–E). With the aid of endoclose and endostitch instruments four sutures are placed in a diamond configuration fixating the small bowel to the fascia. A needle catheter is placed using the Seldinger technique from the center of the fixation points into the jejunum. The sutures are then tightened and tied to the abdominal wall. Several other authors describe a technique using one of the trocar openings through which the jejunum is exteriorized [15, 17, 29, 37]. An enterotomy is then performed and a Foley catheter is inserted and fixated by a purse-string suture. The bowel is fixated to the anterior abdominal wall by several seromuscular sutures.
(A) Port placement. (B) Diamond-shaped suture placement on small bowel. (C) Initial suture placement. (D) Guidewire, introducer, and peel-away sheath. (E) Jejunostomy tube in place. [By permission of Exerpta Medica Inc. Rosser JC, EB Rodas, Blancaflor J (1999) A simplified technique for laparoscopic jejunostomy and gastrostomy tube placement. Surg 177: 61–65.]
Complications
Complications were registered in 17 studies. One study does not give any data on complications in that study, but additional information from the author states that there were a few umbilical leaks and they abandoned this technique [29].
In all but three studies jejunostomy catheter–related complications were found [1, 33, 37. Wound infection was the most frequent complication and occurred in eight studies. Intraabdominal bleeding requiring packed cells occurred once. Reoperation due to catheter-related complications was needed in four studies [2, 10, 25, 32]. In the study by Duh et al. relaparotomy was performed because of a volvulus of the jejunum, and twice a relaparoscopy was performed for reinsertion of a dislodged catheter [10]. In the group of Hotokezaka et al. replacement took place by a relaparotomy [25]. Small bowel perforation was corrected by a second laparoscopy and an obstructed catheter was replaced by a new one during second laparoscopy in the study by Nguyen et al. [32]. One patient was reoperated because of persistent pain, but no catheter problems were found [2]. Conversion of the laparoscopic procedure to an open procedure is mentioned in two studies [10, 25]. Conversion was necessary because of perforation of the jejunum by instruments and catheter or because of severe adhesions [10, 25]. Length of operating time was estimated in 11 studies.
Mortality is reported in nine studies but deaths occurred only in four studies [9, 10, 25, 39]. One patient died of aspiration pneumonia [25]; the other deaths were not related to placement or usage of feeding jejunostomy.
Conclusion
This is a meta-analysis of studies dealing with laparoscopic jejunostomy. Many of these studies contain small patient numbers and are mainly concerned with technique description. Also, clinical heterogeneity was present. However, we were interested in giving an overview of indications, techniques, and results.
When feeding for a period of exceeding 6 weeks is expected, gastrostomy or jejunostomy is indicated. This can be accomplished by using a percutaneous, endoscopic, or operative technique.
Since its introduction, percutaneous endoscopic gastrostomy is considered the procedure of choice in patients with impaired eating ability but who have a functional gastrointestinal tract [16, 36]. Contraindications for the use of percutaneous endoscopic devices are esophageal disorders and head and neck malignancies. Furthermore, in patients prone to aspiration or who have gastroparesis or gastric outlet obstruction jejunostomy is generally preferred to gastrostomy [26]. In addition, jejunostomy can be performed during upper digestive surgery to enable early postoperative feeding [3, 18, 46]. In this meta-analysis upper digestive malignancy was indeed the most common underlying pathology. Laparoscopic placement has the same advantages as other minimally invasive types of surgery and has a beneficial effect on postoperative recovery [8, 20, 27, 35, 41]. Minimaly invasive access for feeding jejunostomy can be accomplished by a total laparoscopic technique or a laparoscopic-aided technique. An advantage of the laparoscopic aided procedure is the direct visualization and placement of the catheter and avoidance of intracorporeal suturing. An advantage of the total laparoscopic method is the avoidance of mini-laparotomy. Fixation of the jejunum to the abdominal wall can be performed using transabdominal sutures, intracorporeal sutures, or T-fasteners. From this meta-analysis it can only be concluded that the most experience is obtained with the total laparoscopic operative technique. Therefore, which method to use depends on the surgeons’ expertise and the availability of materials.
A variety of complications are associated with placement and usage of a postoperative feeding jejunostomy, including mortality [6, 23]. Complication rates of 0–26% are reported [7, 17, 21, 24, 31, 44, 45]. In a large study reviewing more than 2000 applications, 1% jejunostomy-related reoperations are reported [31]; the authors claim that securing the catheter and confirming the correct catheter position by a contrast study could have prevented approximately half of these reoperations, but others could not confirm this statement [23]. In the current meta-analysis 69 complications were found (17%). This is comparable to complication rates of open surgery. Two studies report higher rates of 36–50% [10, 25]. This was explained by the fact that these complications were largely related to complications of preexisting disease. Wound infection and catheter dislodgement were the most common. Major complications necessitating relaparotomy occurred in 1.8%.This finding is in accordance with rates found in open surgery for feeding jejunostomy [6, 23].
The conversion rate was high in the studies by Duh and Hotokezaka because of adhesions and accidental enterotomies [10, 25]. In other studies there was no need for conversion, but this can be largely explained by the fact that patients in whom severe adhesions were expected from previous operations were excluded [10]. Conversion rate in laparoscopic jejunostomy is comparable to conversion rates reported in other laparoscopic procedures.
Laparoscopic jejunostomy can be adequately performed in different ways, of which the total laparoscopic method is the most frequently described. The surgeon’s expertise should determine the appropriate operative technique. The conversion rate is acceptable. The morbidity rate of laparoscopic feeding jejunostomy is comparable to that of open surgery. Still, serious complications do occur and strict patient selection is therefore warranted. Laparoscopic feeding jejunostomy is a viable method to obtain enteral access with the advantages of minimally invasive surgery.
References
MH Albrink J Foster AS Rosemurgy (1992) ArticleTitleLaparoscopic feeding Jejunostomy: also a simple technique Surg Endosc 6 259–260 Occurrence Handle1465736
JW Alien A Ali J Wo (2002) ArticleTitleTotally laparoscopic feeding jejunostomy Surg Endoscopy 16 1802–1805 Occurrence Handle10.1007/s00464-001-9125-3
R Biffi M Lotti S Ceneiarelli (2000) ArticleTitleComplications and long-term outcome of 80 oncology patients undergoing needle catheter jejunostomy placement for early postoperative enteral feeding Clin Nutr 19 277–279 Occurrence Handle10.1054/clnu.2000.0108 Occurrence Handle10952800
M Braga L Gianotti L Nespoli (2002) ArticleTitleNutritional approach in malnourished surgical patients Arch Surg 137 174–180 Occurrence Handle10.1001/archsurg.137.2.174 Occurrence Handle11822956
M Braga A Vignali L Gianotti (1996) ArticleTitleImmune and nutritional effects of early enteral nutrition after major abdominal operations Eur J Surg 162 105–112 Occurrence Handle8639722
RS Date WDB Clements R Gilliland (2004) ArticleTitleFeeding jejunostomy: is there enough evidence to justify its routine use? Dig Surg 21 142–145 Occurrence Handle10.1159/000077454 Occurrence Handle15044815
A Gottardi ParticleDe L Krähenbühl J Farhadi (1999) ArticleTitleClinical experience of feeding through a needle catheter jejunostomy after major abdominal operations Eur J Surg 165 1055–1060 Occurrence Handle10.1080/110241599750007892 Occurrence Handle10595610
S Delgado AM Lacy X Filella (2001) ArticleTitleAcute phase response in laparoscopic and open colectomy in colon cancer: randomized study Dis Colon Rectum 44 638–646 Occurrence Handle11357021
QY Duh LW Way (1993) ArticleTitleLaparoscopic jejunostomy using T-fasteners as retractors and anchors Arch Surg 128 105–108 Occurrence Handle8418772
QY Duh AL Senokozlieff-Englehart AE Siperstein (1995) ArticleTitleProspective evaluation of the safety and efficacy of laparoscopic jejunostomy West J Med 162 117–122 Occurrence Handle7725683
QY Dun AL Senokozlieff-Englehart YS Choe (1999) ArticleTitleLaparoscopic gastrostomy and jejunostomy, safety and cost with local vs general anesthesia Arch Surg 134 151–156 Occurrence Handle10.1001/archsurg.134.2.151 Occurrence Handle10025454
SA Dűzgűn M Bozer A Coskun (2002) ArticleTitlesimplified laparoscopic technique for enteral access in cancer patients Hepatogastroenterology 49 1002–1005 Occurrence Handle12143187
DS Edelman SW Unger (1994) ArticleTitleLaparoscopic gastrostomy and jejunostomy: review of 22 cases Surg Laparos Endosc 4 297–300
LM Ellis DB Evans D Martin (1992) ArticleTitleLaparoscopic feeding jejunostomy tube in oncology patients Surg Oncol 1 245–249 Occurrence Handle10.1016/0960-7404(92)90071-R Occurrence Handle1341257
WK Eltringham AM Roe SW Galloway (1993) ArticleTitleA laparoscopic technique for full thickness intestinal biopsy and feeding jejunostomy Gut 34 122–124 Occurrence Handle8432441
MB Faries JL Rombeau (1999) ArticleTitleUse of gastrostomy and combined gastrojejunostomy tubes for enteral feeding World J Surg 23 603–607 Occurrence Handle10227931
R Gedaly P Briceño R Ravelo (1997) ArticleTitleLaparoscopic jejunostomy with an 18-mm trocar Surg Laparosc Endosc 5 420–422 Occurrence Handle10.1097/00019509-199710000-00012
SJ Gerndt MB Orringer (1994) ArticleTitleTube jejunostomy as an adjunct to esophagectomy Surgery 115 164–169 Occurrence Handle8310404
L Gianotti M Braga A Vignali (1997) ArticleTitleEffect of route of delivery and formulation of postoperative nutritional support in patients undergoing major operations for malignant neoplasms Arch Surg 132 1222–1230 Occurrence Handle9366716
F Glaser GA Sannwald HJ Buhr (1995) ArticleTitleGeneral stress response to conventional and laparoscopic cholecystectomy Ann Surg 221 372–380 Occurrence Handle7726672
DC Gore M DeLegge A Gervin (1996) ArticleTitleSurgically placed gastro-jejunostomy tubes have fewer complications compared to feeding jejunostomy tubes J Am Coll Nutr 15 144–146 Occurrence Handle8778143
GPH Gui ACT Fiennes CVN Cheruvu (1997) ArticleTitleIntracorporeal laparoscopic-guided feeding jejunostomy Ann R Coll Surg Engl 79 462–463 Occurrence Handle9422878
IJM Han-Geurts C Verhoef HW Tilanus (2004) ArticleTitleRelaparotomy following complications of feeding jejunostomy in esophageal surgery Dig Surg 21 192–196 Occurrence Handle10.1159/000079345 Occurrence Handle15218234
IV JH Holmes SI Brundage PC Yuen (1999) ArticleTitleComplications of surgical feeding jejunostomy in trauma patients J Trauma 4 1009–1012
M Hotokezaka RB Adams AD Miller (1996) ArticleTitleLaparoscopic percutaneous jejunostomy for long term enteral access Surg Endosc 10 1008–1011 Occurrence Handle10.1007/s004649900225 Occurrence Handle8864096
WR Jarnagin QY Duh SJ Mulvihill (1992) ArticleTitleThe efficacy and limitations of percutaneous endoscopic gastrostomy Arch Surg 127 261–264 Occurrence Handle1550470
T Kloosterman BM Blomberg Particlevon P Borgstein (1994) ArticleTitleUnimpaired immune functions after laparoscopic cholecystectomy Surgery 115 424–428 Occurrence Handle8165532
FA Moore DV Feliciano RJ Andrassy (1992) ArticleTitleEarly enteral feeding compared with parenteral reduces postoperative septic complications: the results of a meta-analysis Ann Surg 216 172–183 Occurrence Handle1386982
JB Morris JL Mullen JC. Yu (1992) ArticleTitleLaparoscopic-guided Jejunostomy Surgery 112 96–99 Occurrence Handle1535734
Murayama km TJ Johnson JS Thompson (1996) ArticleTitleLaparoscopic gastrostomy and jejunostomy are safe and effective for obtaining enteral access Am J Surg 172 591–595 Occurrence Handle10.1016/S0002-9610(96)00246-2 Occurrence Handle8942569
JG Myers CP Page RM Stewart (1995) ArticleTitleComplications of needle catheter jejunostomy in 2,022 consecutive applications Am J Surg 170 547–551 Occurrence Handle10.1016/S0002-9610(99)80013-0 Occurrence Handle7491998
NT Nguyen PR Schauer BM Wolfe (2000) ArticleTitleLaparoscopic needle catheter jejunostomy Br J Surg 87 482–483 Occurrence Handle10.1046/j.1365-2168.2000.01415.x Occurrence Handle10759747
AE Nicolau M Beuran V Veste (2003) ArticleTitleLaparoscopic jejunostomy in malnourished surgical patients Chirurgia (Bucur) 98 275–281
PJ O’Regan GD Scarrow (1990) ArticleTitleLaparoscopic Jejunostomy Endoscopy 22 39–40 Occurrence Handle2137776
AG Pedersen OB Petersen P Wara (2001) ArticleTitleRandomized clinical trial of laparoscopic versus open appendicectomy Br J Surg 88 200–205 Occurrence Handle10.1046/j.1365-2168.2001.01652.x Occurrence Handle11167866
JL Ponsky MWL Gauderer (1981) ArticleTitlePercutaneous endoscopic gastrostomy: a nonoperative technique for feeding gastrostomy Gastrointes Endosc 27 9
S Ramesh TCB Dehn (1996) ArticleTitleLaparoscopic feeding jejunostomy Br J Surg 83 1090 Occurrence Handle8869310
JC Rosser EB Rodas J Blancafor (1999) ArticleTitleA simplified technique for laparoscopic jejunostomy and gastrostomy tube placement Am J Surg 177 61–65 Occurrence Handle10.1016/S0002-9610(98)00298-0 Occurrence Handle10037310
W Sangster L Swanstrom (1993) ArticleTitleLaparoscopic-guided feeding jejunostomy Surg Endosc 7 308–310 Occurrence Handle10.1007/BF00725946 Occurrence Handle8351602
MG Sarr (1999) ArticleTitleAppropriate use, complications and advantages demonstrated in 500 consecutive needle catheter jejunostomies Br J Surg 86 557–561 Occurrence Handle10.1046/j.1365-2168.1999.01084.x Occurrence Handle10215836
PR Schauer J Luna AA Ghiatas (1993) ArticleTitlePulmonary function after laparoscopic cholecystectomy Surgery 114 389–399 Occurrence Handle8342140
M Senkal KH Bauer M Kemen (1998) ArticleTitleLaparoskopische Feinnadelkatheterjejunostomie Zentralbl Chir 123 1306–1308 Occurrence Handle9880853
M Senkal J Koch T Hummel (2004) ArticleTitleLaparoscopic needle catheter Jejunostomy: modification of the technique and outcome results Surg Endosc 2004; 18 307–309
DV Shatz EJ Block M Kligman (1994) ArticleTitleLaparoscopic suturing technique for enteral access procedures Surg Endosc 8 717–718 Occurrence Handle10.1007/BF00678575 Occurrence Handle8059315
RN Sonawane MM Thombare A Kumar (1997) ArticleTitleTechnical complications of feeding jejunostomy: a critical analysis Trop Gastroenterol 18 127–128 Occurrence Handle9385860
SE Wakefield NJ Mansell RJ Baigrie (1995) ArticleTitleUse of a feeding jejunostomy after oesophagogastric surgery Br J Surg 82 811–813 Occurrence Handle7627518
JL Zapas S Karakozis JR Kirkpatrick (1998) ArticleTitleProphylactic jejunostomy: a reappraisal Surgery 124 715–720 Occurrence Handle10.1067/msy.1998.92380 Occurrence Handle9780993
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Han-Geurts, I.J.M., Lim, A., Stijnen, T. et al. Laparoscopic feeding jejunostomy: A systematic review. Surg Endosc 19, 951–957 (2005). https://doi.org/10.1007/s00464-003-2187-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-003-2187-7