Abstract
TDP-43 immunoreactive (TDP-43-ir) pathological changes were investigated in the temporal cortex and hippocampus of 11 patients with autosomal dominant familial forms of Alzheimer’s disease (FAD), 169 patients with sporadic AD [85 with early onset disease (EOAD) (i.e before 65 years of age), and 84 with late onset after this age (LOAD)], 50 individuals with Down’s Syndrome (DS) and 5 patients with primary hippocampal sclerosis (HS). TDP-43-ir pathological changes were present, overall, in 34/180 of AD cases. They were present in 1/11 (9%) FAD, and 9/85 (10%) EOAD patients but were significantly more common (p = 0.003) in LOAD where 24/84 (29%) patients showed such changes. There were no demographic differences, other than onset age, between AD patients with or without TDP-43-ir pathological changes. Double immunolabelling indicated that these TDP-43-ir inclusions were frequently ubiquitinated, but were only rarely AT8 (tau) immunoreactive. Only 3 elderly DS individuals and 4/5 cases of primary HS showed similar changes. Overall, 21.7% of AD cases and 6% DS cases showed hippocampal sclerosis (HS). However, only 9% FAD cases and 16% EOAD cases showed HS, but 29% LOAD cases showed HS. The proportion of EOAD cases with both TDP-43 pathology and HS tended to be greater than those in LOAD, where nearly half of all the cases with TDP-43 pathology did not show HS. The presence of TDP-43-ir changes in AD and DS may therefore be a secondary phenomenon, relating more to ageing than to AD itself. Nevertheless, a challenge to such an interpretation comes from the finding in AD of a strong relationship between TDP-43 pathology and cognitive phenotype. Patients with TDP-43 pathology were significantly more likely to present with an amnestic syndrome than those without (p < 0.0001), in keeping with pathological changes in medial temporal lobe structures. HS was also associated more commonly with an amnestic presentation (p < 0.005), but this association disappeared when TDP-43-positive cases were excluded from the analysis. TDP-43 may, after all, be integral to the pathology of AD, and to some extent determine the clinical phenotype present.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The transactive response DNA-binding protein 43 (TDP-43) was first identified as a 414 amino acid (molecular mass 43 kDa) binding partner to the TAR regulatory element in the human immunodeficiency virus type 1. Its structure resembles that of a heterogeneous nuclear ribonucleoprotein, and it may function as a transcription repressor or an initiator of exon skipping in the alternative splicing of mRNA [8, 35].
Accumulations of TDP-43 proteins in the form of neuronal cytoplasmic inclusions (NCI) and/or neuritic changes [dystrophic neurites (DN)] in the cerebral cortex and hippocampus are the signature lesions of patients with different forms of Frontotemporal Lobar Degeneration (FTLD) with TDP-43 pathology (FTLD-TDP) and in those with MND alone (see [5, 20, 25] for recent reviews). Nonetheless, TDP-43 immunoreactive (TDP-43-ir) pathological changes have been reported in various other neurodegenerative disorders such as Alzheimer’s disease (AD) [1, 6, 18, 19, 21, 22, 34], Lewy body dementia (DLB) [2, 29, 36], parkinsonism-dementia complex of Guam (Guam PDC) [15, 17], dementia pugilistica [22], corticobasal degeneration (CBD) [34], progressive supranuclear palsy (PSP) [22, 37] and Perry syndrome [13], with a frequency of up to 40% or more of the cases being affected. Most studies investigating TDP-43-ir pathological changes in AD have focussed upon the prevalence and morphological appearance of such changes as largely seen in the temporal cortex, and in the hippocampus and amygdala [1, 6, 18, 19, 21, 22, 34], although Hu et al. [18] investigated the wider topographical brain distribution of TDP-43 pathological changes in 23 patients with AD.
However, it is not clear whether the onset and evolution of TDP-43 pathology in AD is associated with longevity, and perhaps reflective of coincidental ‘ageing’ changes, or is a fundamental aspect of the neurodegenerative process of AD per se. In some studies [1, 6] AD patients with TDP-43 pathology were older than those without such pathology. However, all patients were drawn from an elderly cohort. In order to address directly the effect of ageing, we have compared the presence and severity of TDP-43-ir changes in cohorts of patients with early onset sporadic AD (EOAD), late onset sporadic AD (LOAD), and early onset familial AD (FAD) associated with mutations in APP and PSEN-1 genes, or with duplication of APP locus as in individuals with Down’s syndrome (DS) (in whom the full pathological changes of AD develop predictably by the 5th–6th decades of life [26]). If the development of TDP-43-ir changes is a fundamental part of the process of AD per se, then it might be anticipated that similar proportions of EOAD and LOAD individuals would be affected, as well as those with FAD, and individuals with DS.
Hippocampal sclerosis (HS) is a relatively common pathology, occurring in 0.4–26% of elderly individuals, including ones with AD [4, 9, 10, 12, 23, 30, 31, 38], and continues to increase in prevalence into extreme old age, even at a time when prevalence of AD is diminishing [30]. HS in AD is defined by a selective, severe neuronal loss with gliosis in CA1 and/or subiculum regions of the hippocampus with sparing of CA2-CA5 regions, and is ascertained as such when the extent of neuronal loss outweighs the density of extracellular neurofibrillary tangles in that region [1]. The pathogenesis of HS remains poorly understood, though it appears to be unrelated to AD neurofibrillary pathology or cerebrovascular insufficiencies [30], and probably has multiple underlying causes. The relationship between TDP-43 and HS is complex. Both pathologies are more frequently seen in older, than in younger, individuals with or without AD (see also [1, 19]), but the relationship between them remains unclear.
There is also another potentially confounding factor: clinical phenotype. AD is known to be clinically heterogeneous [14, 32, 33]. Memory impairment is regarded as the hallmark of AD. Yet, in some AD patients memory loss is the dominant presenting feature, and is severe before other deficits emerge (amnestic presentation). In other patients, memory loss is more modest, but is accompanied early in the course by cortical features of aphasia and visuospatial disorientation (multidomain presentation). In other patients, memory loss is not a presenting symptom at all, and patients present with problems in language (language presentation), perception or spatial impairment (visual presentation/posterior cortical atrophy). Very occasionally patients present with a behavioural disorder indicative of frontal lobe dysfunction. These cognitive profiles are mirrored by differences in topographical distribution of atrophy. Greater temporal and hippocampal atrophy has, for example, been demonstrated in amnestic patients and greater temporoparietal or parietal atrophy in patients with multidomain and visual presentations, while the amnestic clinical presentation is associated with an older age at onset; multidomain and visual presentations with younger onset disease [32]. Furthermore, Bigio et al. [6] noted that while half of 27 patients with amnestic AD had concomitant TDP-43 pathology, only 3 of 26 other AD cases with language or behavioural changes showed TDP-43 pathology [6]. Nonetheless, there was good correlation between TDP-43 pathological changes and the presence of HS when all 53 patients were considered together [6].
In the current neuropathological series some patients, predominantly in the EOAD cohorts, had previously been classified according to cognitive phenotype at the time of their initial presentation, thereby providing the opportunity to examine the influence of cognitive phenotype on TDP-43 pathology. If the TDP-43 pathology in AD is simply a by-product of ageing then there ought to be no effect of cognitive phenotype within a patient group matched for age. By contrast, if cognitive phenotype is pertinent to the presence of TDP-43 pathology then one would expect to see phenotypic differences in AD patients with and without TDP-43 pathology. We have also been able to investigate the relationship between TDP-43 pathology and HS, and to ascertain whether clinical phenotype is driven by the presence of TDP-43 or HS alone, or whether these have additive effects.
Materials and methods
Patients
The study group consisted of 180 patients with pathologically proven AD. Ninety-six patients had EOAD (i.e onset of illness before 65 years of age), and 84 had LOAD (i.e onset of illness on or after this age) (Table 1). The early onset group was further stratified into 85 patients with sporadic EOAD and 11 patients with familial early onset AD (FAD) (Table 1). The FAD cases comprised 4 with APP mutations (1 with APP692 mutation and 3 with APP717 mutation, 2 Val717Ile and one Val717Gly) and 7 had PSEN-1 mutations (3 with M139V, 2 with Delta 4, 1 with E120K, and 1 with E280G mutations).
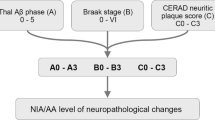
Clinical diagnosis of AD was according to the Manchester Neuropsychological Inventory [32, 33] which contains elements such as the Clinical Dementia Rating and is consistent with International consensus clinical criteria [27]. Neuropathological diagnosis of definite AD was made according to CERAD criteria [28]. All AD patients were demented in life. All AD cases showed numerous diffuse amyloid and neuritic plaques within all neocortical brain regions, and tau (AT8) and ubiquitin (UBQ) immunoreactive NFT within pyramidal neurones of CA1 and subiculum of the hippocampus, and within layer 3 and 5 pyramidal neurones of the temporal, frontal and parietal neocortex indicative of Braak stage 5, or stage 6 when the occipital cortex was also significantly affected [7]. In some patients, occasional dentate gyrus (DG) granule cells were also AT8/UBQ immunopositive. Three of the FAD cases showed occasional Lewy bodies in frontal and temporal cortex, or parahippocampal and insular gyri, and occasionally in midbrain (substantia nigra and locus caeruleus). None of the patients with sporadic AD displayed Lewy bodies within the substantia nigra, amygdala, hippocampus or cerebral cortex. Many of the patients, especially those in the LOAD group, showed variable degrees of cerebrovascular disease, chiefly involving arteriosclerotic changes in small arteries of the deep white matter and within subcortical grey matter regions. In none of the cases however were these changes associated with major infarction or haemorrhage, though local regions of microinfarction or ischaemic change were not uncommon. The numerical differences in gender composition of the EOAD and LOAD groups did not reach statistical significance (χ2 = 1.92, p = 0.165).
Additionally, 50 individuals with DS ranging from newborn to 70 years were investigated (Table 1). Where karyotyping had been performed, all were trisomy 21. Forty-one of these individuals were over the age of 30 years and all displayed some degree of AD-type pathological changes. Finally, 5 cases of primary HS, in which concomitant AD-type pathological changes were absent or failed to meet neuropathological diagnostic criteria for definite AD [28] were also investigated (Table 1). Four of these patients were demented, one showed mild cognitive impairment. Two patients were essentially free of AD-type pathology (one with otherwise normal brain, one with cerebrovascular pathology) with Braak score I/II and CERAD rating of no AD, while the other 3 patients had Braak score III/IV and possible AD.
Two of the FAD cases, all of the EOAD and LOAD cases, and 9 of the DS cases were drawn from the Manchester Brain Bank. The other 9 cases of FAD and 5 with DS were obtained from Institute of Psychiatry Brain Bank, London. Twenty-one of the remaining 36 individuals with DS were obtained from the Thomas Willis Brain Bank, Oxford with the rest being obtained through Professor V P Prasher in Birmingham. The 5 cases with primary HS were also obtained from the Thomas Willis Brain Bank, Oxford. All brains had been obtained at autopsy through appropriate consenting procedures with Local Ethical Committee approval.
Pathological methods
Brains had been fixed in 10% buffered formalin for a period of between 1 and 3 months at least, after which, blocks of tissue were cut from the temporal cortex (Brodmann areas 21/22) and hippocampus (at the level of the geniculate bodies) and processed routinely into paraffin wax. Sections were cut at a thickness of 6μm from all cases, and immunostained by a standard ABC method for TDP-43 using a phospho-independent polyclonal TDP-43 antibody (10782-1-AP, Protein Tech Inc, Chicago, IL) at a dilution of 1:1000 [11]. In those instances where TDP-43 pathological changes had been revealed using the phospho-independent polyclonal TDP-43 antibody (see later), a phospho-dependent rabbit polyclonal antibody pS409/410-2 (Cosmobio Co, Tokyo, Japan) was used, again at a dilution of 1:1000. All cases were also immunostained for phosphorylated tau [mouse monoclonal antibody AT8 (Innogenetics, Ghent, Belgium) 1:750], amyloid β protein [4G8 mouse monoclonal antibody (Covance Research Products Inc., Dedham, MA) 1:3000] and ubiquitin [rabbit polyclonal antibody Z0458 (Dako Cytomation, Ely, UK) 1:750] employing a standard ABC Elite kit (Vector, Peterborough, UK) with DAB as chromogen, as we have described previously [11].
For selected AD cases, double immunolabelling was performed. In one instance, TDP-43 immunoreaction was firstly performed (using the phospho-independent TDP-43 antibody) with DAB as the chromogen. This was followed by UBQ immunoreaction employing mouse monoclonal UBQ antibody (NCL-UBIQm, Vision Biosciences, Newcastle, UK, 1:50), with Vector Elite secondary antibody kit with very intense purple (VIP) as the chromogen. In the second instance, TDP-43 immunoreaction was firstly performed, as above, with DAB as revealing agent. This was followed by AT8 immunoreaction with VIP as the chromogen. In both instances, sections were again lightly counterstained with haematoxylin.
In some of these latter AD cases double immunofluorescence microscopy was performed using TDP-43 and AT8 antibodies sequentially. TDP-43 signal was visualised using tetramethyl rhodamine labelled secondary antibody and AT8 with the fluorescein signal amplification kit (Perkin Elmer, UK). Sections were washed thoroughly in phosphate buffered saline and mounted in aquamount (Merck, UK). Control sections incubated without primary antibody exhibited no significant background staining. Fluorescent signals from sections were scanned using a Leica SP2 laser confocal microscope with Leica LCS software.
Using the phospho-independent TDP-43 antibody, the severity of TDP-43 pathological changes in the DG, CA1, CA2/3, CA4/5 and subiculum regions of the hippocampus, and in the entorhinal cortex, fusiform gyrus (FG) and temporal neocortex was rated in each area according to 0 = absent; 0.5 = rare; 1 = mild; 2 = moderate; 3 = severe; 4 = very severe. Individual scores in each area were then summated to give an overall pathology score for each case.
All cases were examined for the presence of HS, this being graded semiquantitatively according to 0 = absent; 1 = mild; 2 = moderate; 3 = severe.
Apolipoprotein E genotyping
DNA was extracted from frozen brain tissue (cerebellar cortex or frontal cortex) where this was available using a standard phenol–chloroform procedure, and genotyped for Apolipoprotein E (APOE) genotypes as described previously [32].
Classification of cognitive phenotype
Seventy-eight patients, mostly those presenting before 65 years, had previously been ascertained, and prospectively assessed, through the Cerebral Function Unit at Salford Royal Hospitals Foundation Trust. They had been classified according to their cognitive profile at the time of clinical presentation, based on clinical history and findings on neuropsychological examination presentation, and included amnestic, multidomain, visual, language and frontal/behavioural phenotypes [32]. All classifications were carried out prior to and without knowledge of pathological findings. The relationship between TDP-43 pathology and clinical phenotype was examined using these classification data.
All statistical tests were performed using SPSS 15.0
Results
Single label immunohistochemistry
Investigations of the temporal cortex and hippocampus using the phospho-independent TDP-43 antibody showed no TDP-43 immunostaining in 142 (79%) of the AD patients except for a variable degree of physiological nuclear staining. However, some degree of TDP-43-ir pathological changes was observed in the other 38 patients. In 34 of patients (19% of the total), there were a few, ranging to many, small clusters of TDP-43-ir granules, or sometimes more solid, rounded inclusions, present in DG granule cells of the hippocampus (Fig. 1a). In these same patients, TDP-43-ir inclusions were sometimes, but not often, seen within pyramidal cells in areas CA1, CA2/3 and CA4/5, or more commonly within the subiculum, these usually resembling extracellular, rather than intracellular, NFT (Fig. 1b). However, in these 34 patients, the most striking TDP-43-ir pathology was seen in the FG where variable numbers of rounded TDP-43-ir cytoplasmic inclusions, or more diffuse granular TDP-43 deposits, were observed in small neurones of layer II (Fig. 1c). Similar structures were less commonly seen in neurones of deeper layers of the FG and occasionally NII were also observed (Fig. 1d). Such changes within the FG were moderate to severe in 26 patients but mild or rare in 8 patients. Similar changes were also present, but usually to a lesser extent, in the lateral extent of the entorhinal cortex and the most medial part of the inferior temporal gyrus, but these gradually petered out in frequency within the rest of the inferior temporal gyrus, becoming rare or absent in middle and superior temporal gyri. This pattern of TDP-43-ir pathological changes has been well described previously in AD [1, 6, 18, 19, 21, 22, 34] and other disorders [2, 13, 15, 17, 22, 29, 34, 36, 37] and is considered here to represent ‘typical’ TDP-43 changes for comparative purposes.
Neuronal cytoplasmic inclusion (NCI) pathology in the hippocampus in AD. TDP-43 immunostaining using Proteintech anti TDP-43 antibody reveals densely granular TDP-43-ir NCI within granule cells of the dentate gyrus (DG) (a) and within small pyramidal cells of the entorhinal cortex (EC)/fusiform gyrus (FG) (c) where occasional intranuclear inclusions are seen (d). Some pyramidal cells of area CAI are also TDP-immunoreactive but these are mostly extracellular (b). Use of phosphodependent anti TDP-43 antibody, pS409/410 shows similar NCI within the DG (e) and FG (f). These are also ubiquitinated (g), but not immunoreactive to AT8 antibody to phosphorylated tau proteins, though occasional tau-positive neurones are present (h)
In 4 other AD patients, no neurones within the DG, entorhinal cortex, FG or temporal neocortex were affected, though incidental TDP-43-ir pyramidal neurones (one or two cells per section) were very occasionally seen within area CA1, CA2/3, CA4/5, or (usually) subiculum alone in these cases. Similar changes were noted on equivalent sections from the same cases using the phospho-dependent TDP-43 antibody, pS409/410 (Fig. 1e, f), but without the physiological staining of nuclei. No TDP-43-ir changes were observed within glial cells in either grey or white matter in any of the 38 patients with neuronal TDP-43 pathology.
UBQ immunostaining showed similar (to TDP-43) appearing UBQ-ir inclusions in the FG and adjoining parts of the inferior temporal gyrus and entorhinal cortex, with approximately the same level of frequency as those which were TDP-43-ir (Fig. 1g). AT8 (tau) immunopositive (AT8-ir) neurones were rare within this region (Fig. 1h).
Of the 50 individuals with DS, 7 showed no AD-type pathological changes; all were aged <20 years. Two individuals, aged 23 and 27 years, showed rare to moderate numbers of diffuse amyloid plaques within the temporal neocortex (but not in the hippocampus) but no neurofibrillary changes. All of the 41 persons over 30 years of age showed some degree of plaque and tangle formation, this being similar or greater in degree of severity to that seen in AD in 35 individuals, all of whom were over 50 years of age. In the other 6 individuals (35–50 years) numerous diffuse and some neuritic amyloid plaques were seen within the temporal neocortex and hippocampus, but neurofibrillary changes were uncommon and usually seen only within the hippocampus and/or entorhinal cortex. Only 3 individuals (aged 54, 59 and 61 years) (7%) of the 41 with ‘evolving’ or ‘fully developed’ AD pathology showed (minor) TDP-43-ir pathological changes, having the same topographic distribution within the hippocampus and temporal cortex as was seen in the 34 affected AD patients referred to previously. These 3 individuals also showed HS.
Of the 5 patients with primary HS, 4 showed TDP-43-ir pathological changes of the kind seen in AD within a similar topographic location in the hippocampus and temporal cortex. These were mild in 2 cases, moderate in one case and severe in one case. Three of the 4 positive cases had possible AD by CERAD, but the other was normal. The TDP-43 negative case had cerebrovascular lesions.
Double labelling immunohistochemistry
Double labelling immunohistochemistry showed that most of the TDP-43-ir inclusions within the DG granule cells were also UBQ-ir (on line supplementary Fig. 1a) but not AT8-ir (on line supplementary Fig. 1b). Likewise, most of the TDP-43-ir inclusions within the outer layer of the FG were also UBQ-ir, but none was AT8-ir (not shown). AT8-ir neurones in the deeper layers of the FG were UBQ-ir, but not TDP-43-ir (not shown). The occasional TDP-43-ir inclusions within CA1 and subiculum were not AT8-ir. Double immunofluoresce microscopy confirmed that most of the TDP-43-ir inclusions within either the DG granule cells (on line supplementary Fig. 2a), or the outer layer of the FG (on line supplementary Fig. 2b), were not AT8-ir, though partial colocalisation did occur in rare cells in both regions (on line supplementary Fig. 2a).
Comparisons between TDP-43 positive and TDP-43 negative early and late onset AD patients
Twenty-four out of 84 (29%) LOAD patients, but only 9/85 (10%) EOAD cases, 1/11 (9%) FAD and 3/41 (7%) of the older DS cases, showed topographically ‘typical’ TDP-43 pathological changes (as defined above). The prevalence of TDP-43 pathology in LOAD was significantly higher than in EOAD (χ2 = 8.91; p = 0.003), and DS (χ2 = 6.21; p = 0.013), but did not reach significance when compared to FAD (p = 0.278, Fisher’s exact test), presumably due to lack of statistical power resulting from low numbers. Within the EOAD group, TDP-43 positive and TDP-43 negative cases did not differ in terms of gender composition (χ2 = 0.182, p = 0.670), mean age at onset of disease (p = 0.174) or the mean duration of illness (p = 0.222), Similarly, within the LOAD group TDP-43 positive and negative cases did not differ in terms of gender composition (χ2 = 0.122, p = 0.727), mean age at onset of disease (p = 0.314) or mean duration of illness (p = 0.397).
In the total group of 34 ‘typical’ TDP-43 positive cases, measurements of severity of TDP-43 pathological changes showed no correlation with age at onset of disease (p = 0.652) or duration of illness (p = 0.714).
Relationship between TDP-43 pathology and hippocampal sclerosis
Overall, 21.7% AD cases and 6% DS cases showed HS. However, within the AD group, only 1 (9%) FAD cases and 14 (16.5%) EOAD cases, but 24 (28.6%) LOAD cases, showed HS (Table 1). The proportion of patients in the LOAD with HS tended to be greater (χ2 = 3.55, p = 0.067) than that in EOAD (Table 1).
The proportion of patients in both EOAD and LOAD with TDP-43 pathology that also had HS (i.e 8/9 (89%) cases in EOAD and 13/24 (54%) cases in LOAD) was significantly greater than that in both these groups that were without TDP-43 pathology but still had HS (i.e 6/76 (8%) cases in EOAD and 11/60 (18%) cases in LOAD) (χ2 = 38.3, p = 0.000 and χ2 = 10.8, p = 0.003, respectively) (Table 1).
There was also a trend for the proportion of cases in EOAD that had TDP-43 pathology and HS [8/9 (89%) cases] to be greater than the proportion in LOAD, where only 13/24 (54%) such cases also had HS (χ2 = 3.41, p = 0.065). Conversely, the proportion of cases in the EOAD without either TDP-43 pathology or HS (70/85 cases, 82%) was significantly greater than that in LOAD (49/84 cases, 58%) (χ2 = 11.7, p = 0.001). Moreover, 10/11 (90%) FAD cases and 44/50 (88%) DS showed neither TDP-43 pathology nor HS. However, the proportion of cases in LOAD group with HS, but without TDP-43 pathology (11/24 cases, 46%), did not differ from that in EOAD (6/14 cases, 43%) (χ2 = 0.032, p = 0.859).
In other words, cases of EOAD with TDP pathology are more likely also to show HS than are cases of LOAD with TDP-43 pathology; in LOAD nearly half of all cases with HS were TDP-43 negative. However, cases of both EOAD and LOAD without TDP-43 pathology are equally likely to show HS. Cases of EOAD (irrespective of cause) and DS are, therefore, more likely to be without either TDP-43 pathology or HS than are cases of LOAD.
Although the severity score for HS in those cases that also had TDP-43 pathology (mean score = 2.12) was numerically greater compared to those cases without TDP-43 pathology (mean HS score = 1.9) this difference was not statistically significant (p = 0.307). The severity score for HS did not correlate significantly (p = 0.877) with that for TDP-43 pathology in those 22 combined EOAD and LOAD cases showing both TDP-43 pathology and HS.
As mentioned 4/5 cases of primary HS showed TDP-43 pathological changes, though the severity of the TDP-43 pathology did not obviously relate to the extent of HS (which was very severe in all 4 cases).
Relationship between TDP-43 pathology, hippocampal sclerosis and APOE ε4
As found by others [6], the APOE ε4 allele frequency in the TDP-43 positive group was not significantly different from that in the TDP-43 negative group in either EOAD or LOAD (χ2 = 0.31, p = 0.576 and χ2 = 0.039, p = 0.843, respectively) (Table 1). Likewise, comparisons between APOE ε4 allele frequency in EOAD and LOAD TDP-43 positive groups, and between APOE ε4 allele frequency in EOAD and LOAD TDP-43 negative groups were non-significant (χ2 = 0.0, p = 0.985 and χ2 = 1.62, p = 0.203, respectively) (Table 1). Nevertheless, the severity of TDP-43 pathological changes in FG in patients with APOE ε4 allele was significantly greater (Mann–Whitney U = 12.5, p = 0.032) than that in those patients without APOE ε4 allele. Similar comparisons within the FAD and DS groups were not performed as there was only a single TDP-43 positive case in the former group and 3 such cases in the latter group.
As reported by others [23] the APOE ε4 allele frequency in HS positive cases was significantly greater than that in HS negative cases both overall [31/66 alleles (0.47) vs. 79/242 alleles (0.33); χ2 = 4.64, p = 0.031] in both EOAD and LOAD (Table 1). The APOE ε2 allele frequency in HS positive cases was numerically less than that in HS negative cases but there were too few ε2 alleles in the HS positive group for meaningful statistical analysis.
Relationship between TDP-43 pathology, hippocampal sclerosis and cognitive phenotype
Cognitive phenotypic information at the time of patients’ clinical presentation was available for 78 AD cases. 11 (14%) of cases were classified as ‘amnestic’ and 59 (76%) as multidomain. Rarer, focal presentations accounted for 10%: 4 (5%) visual, 2 language (2.5%) and 2 frontal (2.5%). The high proportion of multidomain presentations reflects the high prevalence of this phenotype in EOAD [32].
Comparisons between patients with and without TDP-43 pathology revealed a striking finding. 7/11 (64%) of TDP-43 positive cases had an amnestic presentation, but only 4/67 (6%) of TDP-43 negative cases had this presentation. The difference is highly significant (χ2 = 25.9, p < 0.0001). Conversely, the multidomain presentation accounted for only 2/11 (18%) of TDP-43 positive cases but 57/67 (85%) of TDP-43 negative cases, the difference again being highly significant (χ2 = 22.9, p < 0.0001). Non-amnestic focal presentations (language, visual, frontal) were rare in both groups, so were non-discriminatory. TDP-43 positive and negative cases did not differ in age at onset of illness.
HS too was more common in cases with amnestic than non-amnestic presentations (χ2 = 8.00, p = 0.005). However, when TDP-43 positive cases were removed from the analysis, the effect of HS on phenotype was no longer significant. By contrast when HS positive cases were removed from the analysis the effect of TDP-43 on phenotype continued to be highly significant, TDP-43 positivity being strongly associated with amnestic presentation: amnestic versus multidomain comparison (χ2 = 20.76, p < 0.001). There was no statistically significant additive effect of TDP-43 and HS on likelihood of an amnestic presentation. There were particular features regarding the presentation of the TDP-43-negative, HS positive cases, which on the whole tended to be associated with the more common ‘multidomain presentation.
Discussion
Intracellular accumulations of TDP-43 have been reported as characterising the pathological changes of many cases of FTLD and MND [5, 20, 25]. In the present study such changes were present in 21% of AD cases. In most (19%), TDP-43-ir granules, or sometimes more solid, rounded NCI were seen in the DG granule cells. However, the most striking TDP-43 pathology was seen in the FG and medial parts of the ITG and lateral parts of the EC where numerous, rounded TDP-43-ir NCI, or more diffuse granular TDP-43 deposits, were observed in small neurones of layer II. Occasional TDP-43-ir lentiform NII were also observed. Double labelling microscopy showed that while the majority of these TDP-43-ir pathological changes in both the DG and FG were UBQ immunopositive, there was little or no colocalisation with tau proteins. Conversely, in the CA1 and subiculum, and temporal neocortex only occasional tau/NFT containing pyramidal cells showed TDP-43 colocalisation. These anatomical and morphological observations are similar to those reported by others [1, 2, 6, 18, 19, 21, 22, 34].
Previous studies of AD have typically found a higher proportion of patients with TDP-43 pathological changes than in the present study. For example, Amador-Ortiz et al. [1] noted TDP-43 pathological changes in the brains of 23% of 74 patients with AD (mean age at death, 79 years). Uryu et al. [34] reported such changes in 26% of 182 patients (mean age at death, 77.5 years). Arai et al. [2] found 36–56%, respectively, of a Japanese (53 patients, mean age at death 83, years) and Canadian (25 patients, mean age at death, 81 years) series of patients to be affected by TDP-43 pathological changes. Kadokura et al. [21] noted 31% of 16 patients (mean age 75 years) to be affected. King et al. [22] observed TDP-43 pathology in 58% of 19 cases of AD (mean age 77.4 years). Finally, Bigio et al. [6] noted TDP-43 pathological changes in 14 of 27 cases of AD (mean age 78.6 years). A plausible explanation for variations in findings lies in differences in age composition of the various cohorts. In previous studies the mean age at death (77.5–83 years) was higher than in the present study (71.6 years), suggesting that they are likely to represent older cohorts. The finding in the present study of a significantly higher prevalence of TDP-43-ir pathological changes in LOAD, compared to EOAD, draws attention to the potential importance of age as a determining factor. Our observations are in keeping with those of Josephs et al. [19] who found an effect of age on TDP-43 pathology in AD. They are also consistent with the report by Geser et al. [16] of TDP-43 pathology in 29% of brains of healthy controls and people with psychiatric illnesses over 65 years of age, but no such changes in younger people.
To our knowledge, there has been only one previous study investigating the presence and distribution of TDP-43-ir pathological changes in FAD and in DS [24] In that study, 42 patients with FAD [30 with PSEN-1 mutations (including 7 with A246E, 13 with C410Y, 3 with L286V and 4 with M146L mutation), 3 with PSEN-2 mutations, 3 with an APP mutation (Val717Ile) and 6 others where no mutation (in these genes) was found though all 6 cases showed autosomal dominant inheritance] and 14 with DS due to trisomy 21. TDP-43-ir changes of the kind seen in sporadic AD were found in the hippocampus and temporal lobe (but none in the frontal cortex) of 6/42 (13%) cases of FAD, and in 2/14 (13%) individuals with DS. TDP-43-ir changes did not colocalise with tau tangle-bearing neurones. Present observations of TDP-43-ir changes in temporal lobe structures of 1/11 (9%) FAD cases and 3/37 (8%) DS cases are consistent with the earlier report [24], and show that such changes are relatively rare in younger persons with AD irrespective of genetic aetiology.
HS is a relatively common finding, occurring in 0.4 to 26% of elderly individuals, including ones with AD [5, 6, 9, 10, 12, 23, 30, 31, 38], and continues to increase in prevalence into extreme old age, even at a time when prevalence of AD is diminishing [30]. The pathogenesis of HS remains poorly understood, though it appears to be unrelated to AD neurofibrillary pathology or cerebrovascular insufficiencies [30], and probably has multiple underlying causes. The relationship between TDP-43 and HS is complex. As shown here, both pathologies are more frequently seen in older, than in younger, individuals with or without AD (see also [1, 19]), but the relationship between them remains unclear. In a study of 306 elderly cases (including some with AD), TDP-43 pathology was significantly more common in cases with HS than in cases without HS [30]. Similar findings were reported by Amador-Ortiz et al. [1]. We also find that TDP-43 pathology is more common in cases of AD with HS than those without HS, especially in EOAD cases where this distinction is more strongly observed.
To our knowledge, there have been no previous studies which have specifically investigated the relationship between TDP-43 pathology and HS. In the present study, in EOAD, it seems that TDP-43 pathology and HS co-occur in most patients, though in LOAD, only about half of the patients with TDP-43 pathology also show HS. Bigio et al. [6] also noted that only 9 of 14 elderly cases of AD also displayed HS. This suggests that, as in EOAD, HS may relate to presence of TDP-43 pathology only in about half of the patients with LOAD, and there would appear to be other biological reasons for HS to occur in the remainder. Present and other [6] observations showing discordancy between the presence of TDP-43 pathology and HS might, therefore, argue that when TDP-43 and HS do occur together, this represents a coincidence of two relatively common pathologies in a single patient, rather than there being a direct causal link between the two. The relative paucity of TDP-43-ir neurones in CA1 and subiculum in cases where HS is not seen, even when florid TDP-43 changes are present in EC and FG, would support this argument of coincidence rather than causality. This discordancy is further illustrated by the present observations that only 4/5 cases of primary HS showed TDP-43 pathology. In another study, Amador-Ortiz et al. [1] similarly noted that only 13/21 (63%) cases of primary HS showed TDP-43 pathology. Moreover, the finding that 3 of the present 4 HS cases with TDP-43 pathology also had minor degrees of AD-type pathology, is possibly indicative of an evolving AD, and would emphasise that association between TDP-43 and AD in the majority of the elderly, rather than reflecting a causal relationship between HS and TDP-43 per se.
However, on the other hand, HS is usually seen in cases of FTLD with TDP-43, rather than tau, based pathology [1, 3], suggesting a direct linkage. Nonetheless, this relationship is imperfect with only about 75% of such TDP-43 positive cases showing HS and, as with AD, HS is again more commonly seen in older, than in younger, patients with FTLD [3].
The converging evidence from this and other studies is in keeping with the notion that age influences the development of TDP-43 pathology. Yet, age per se appears to provide an insufficient explanation for the available data. Why do some patients develop TDP-43 pathology whereas others of a similar age do not? The examination in this study of clinical phenotype in a subset of patients, mainly with early onset, is revealing. There was a strong bias towards an amnestic clinical presentation in patients with TDP-43 pathology and a non-amnestic, multidomain presentation in patients without TDP-43 pathology. These TDP-43 positive and negative cases did not differ in age of onset. Bigio et al. [6] also noted a strong bias towards an association between the presence of TDP-43 pathology and an amnestic presentation of AD. It is also pertinent that the amnestic presentation has previously been found [32] to be associated with predominant temporal/hippocampal atrophy—precisely those brain regions most affected here by TDP-43 pathology. By contrast, the multidomain presentation is associated with greater involvement of the temporoparietal cortex. The findings are in keeping with a previous report of greater hippocampal atrophy in AD patients with TDP-43 pathology compared to those without [19]. Clinical phenotype appears to be a strong predictor of TDP-43 pathology. We have previously found that amnestic presentations of AD become more prevalent with increasing age [32]. Thus, it may not be age per se that accounts for the observed ‘age effects’ in predicting TDP-pathology, but rather the dominance of memory loss as the presenting feature in elderly AD patients compared to younger-onset patients.
Interestingly, HS was also associated more commonly with an amnestic presentation of AD, a finding in keeping with reports of an association between HS and memory loss [30]. However, the effect was less robust than that seen for TDP-43, and disappeared when TDP-43-positive cases were excluded from the analysis. Cases with HS alone showed mostly the multidomain presentation.
The similarities in appearance and distribution of TDP-43 pathological changes in AD and a wide range of other neurodegenerative disorders might reasonably lead to the conclusion that such changes are not specific to any particular disease. Moreover, it is tempting to infer, from the increased frequency of such changes in older individuals with AD, that their presence reflects a pathological process associated with ageing or longevity, and one that is independent of the principal (AD) pathological changes. A challenge to such an interpretation, however, comes from the strong relationship reported here between clinical phenotype and TDP-43 pathology. The presence of prominent amnesia associated with a pathology that largely affects medial temporal lobe structures provides a coherent account, which suggests that TDP-43 may, after all, be integral to the pathology of at least some forms of AD.
References
Amador-Ortiz C, Lin W-L, Ahmed Z, Personett D, Davies P, Duara R, Graff-Radford NR, Hutton ML, Dickson DW (2007) TDP-43 immunoreactivity in hippocampal sclerosis and Alzheimer’s disease. Ann Neurol 61:435–445
Arai T, Mackenzie IRA, Hasegawa M, Nonaka T, Niizato K, Tsuchiya K, Iritani S, Onaya M, Akiyama H (2009) Phosphorylated TDP-43 in Alzheimer’s disease and dementia with Lewy bodies. Acta Neuropathol 117:125–136
Baborie A, Griffiths TD, Jaros E, Richardson A, Ferrari R, Moreno J, Momeni P, McKeith IG, Burn DJ, Duplessis D, Pal P, Rollinson S, Pickering-Brown SM, Thompson JC, Neary D, Snowden JS, Perry R, Mann DMA (2011) Pathological correlates of frontotemporal lobar degeneration in the elderly. Acta Neuropathol 121:365–373
Barker WW, Luis CA, Kashuba A, Luis M, Harwood DG, Loewenstein D, Waters C, Jimison P, Shepherd E, Sevush S, Graff-Radford N, Newland D, Todd M, Miller B, Gold M, Heilman K, Doty L, Goodman I, Robinson B, Pearl G, Dickson D, Duara R (2002) Relative frequencies of Alzheimer disease, Lewy body disease, vascular and frontotemporal dementia, and hippocampal sclerosis in the state of Florida Brain Bank. Alzheimer Dis Assoc Disord 16:203–212
Bigio EH (2011) TDP-43 variants of Frontotemporal lobar degeneration. J Mol Neurosci (in press)
Bigio EH, Mishra M, Hatanpaa KJ, White CL III, Johnson N, Rademaker A, Weitner BB, Deng H-X, Dubner SD, Weintraub S, Mesulam M (2010) TDP-43 pathology in primary progressive aphasia and frontotemporal dementia with pathologic Alzheimer disease. Acta Neuropathol 120:43–54
Braak H, Braak E (1991) Neuropathological stageing of Alzheimer-type pathological changes. Acta Neuropathol 82:239–259
Buratti E, Brindisi A, Pagini F, Baralle FE (2004) Nuclear factor TDP-43 binds to the polymorphic TG repeats in CFTR intron 8 and causes skipping of exon 9: a functional link with disease penetrance. Am J Hum Genet 74:1322–1325
Chui HC, Zarow C, Mack WJ, Ellis WG, Zheng L, Jagust WJ, Mungas D, Reed BR, Kramer JH, Decarli CC, Weiner MW, Vinters HV (2006) Cognitive impact of subcortical vascular and Alzheimer’s disease pathology. Ann Neurol 60:677–687
Crystal HA, Dickson D, Davies P, Masur D, Grober E, Lipton RB (2000) The relative frequency of ‘dementia of unknown etiology’ increases with age and is nearly 50% in nonagenerarians. Arch Neurol 57:713–719
Davidson Y, Kelley T, Mackenzie IR, Pickering-Brown SM, Du Plessis D, Neary D, Snowden JS, Mann DMA (2007) Ubiquitinated pathological lesions in frontotemporal lobar degeneration contain the TAR DNA-binding protein, TDP-43. Acta Neuropathol 113:521–533
Dickson DW, Davies P, Bevona C, Van Hoeven FH, Factor SM, Grober E, Aronson MK, Crystal HA (1994) Hippocampal sclerosis: a common pathological feature in very old (> or = 80 years of age) humans. Acta Neuropathol 88:212–221
Farrer MJ, Hulihan MM, Kachergus JM, Dachsel JC, Stoessl AJ, Grantier LL, Calne S, Calne DB, Lechevalier B, Chapon F, Tsuboi Y, Yamada T, Gutmann L, Elibol B, Bhatia KP, Wider C, Vilarino-Guell C, Ross OA, Brown LA, Castanedes-Casey M, Dickson DW, Wszolek ZK (2009) DCTN1 mutations in Perry syndrome. Nat Genet 41:163–165
Galton CJ, Patterson K, Xuereb JH, Hodges JR (2000) Atypical clinical presentations of Alzheimer’s disease: a clinical, neuropsychological, neuroimaging and pathological study of 13 cases. Brain 123:484–498
Geser F, Winton MJ, Kwong LW, Xu Y, Igaz LM, Garruto RM, Perl DP, Galasko D, M-Y Lee V, Trojanowski JQ (2008) Pathological TDP-43 in parkinsonism dementia complex and amyotrophic lateral sclerosis. Acta Neuropathol 115:133–146
Geser F, Robinson JL, Malunda JA, Xie SX, Clark CM, Kwong LK, Moberg PJ, Moore EK, Van Deerlin VM, Lee VM-Y, Arnold SE, Trojanowski JQ (2010) Pathological 43-kDa transactivation response DNA-binding protein in older adult with and without severe mental illness. Arch Neurol 67:1238–1250
Hasegawa M, Arai T, Akiyama H, Nonaka T, Mori H, Hashimoto T, Yamazaki M, Oyanagi K (2007) TDP-43 is deposited in the Guam parkinsonism-dementia complex brains. Brain 130:1386–1394
Hu WT, Josephs KA, Knopman DS, Boeve BF, Dickson DW, Petersen RC, Parisi JE (2008) Temporal lobar predominance of TDP-43 neuronal cytoplasmic inclusions in Alzheimer’s disease. Acta Neuropathol 116:215–220
Josephs KA, Whitwell JL, Knopman DS, Hu WT, Stroh DA, Baker N, Rademakers R, Boeve BF, Parisi JE, Smith GE, Ivnik RJ, Petersen RC, Jack CR, Dickson DW (2008) Abnormal TDP-43 immunoreactivity in AD modifies clinicopathologic and radiologic phenotype. Neurology 70:1850–1857
Josephs KA, Hodges JR, Snowden JS, Mackenzie IR, Neumann M, Mann DM, Dickson DW (2011) Neuropathological background of phenotypical variability in frontotemporal dementia. Acta Neuropathol 122:137–154
Kadokura A, Yamazaki T, Lemere CA, Takatama M, Okamoto K (2009) Regional distribution of TDP-43 inclusions in Alzheimer disease (AD) brains: their relationship to AD common pathology. Neuropathology 29:566–573
King A, Sweeney F, Bodi I, Troakes C, Maekawa S, Al-Sarraj S (2010) Abnormal TDP-43 expression is identified in the neocortex in cases of dementia pugilistica, but is mainly confined to the limbic system in high and moderate stages of Alzheimer’s disease. Neuropathology 30:408–419
Leverenz JB, Agustin CM, Tsuang D, Peskind ER, Edland SD, Nochlin D, DiGiacano L, Bowen JD, McCormick WC, Teri L, Raskind MA, Kukull WA, Larson EB (2002) Clinical and neuropathological characteristics of hippocampal sclerosis. A community based study. Arch Neurol 59:1099–1106
Lippa CF, Rosso AL, Stutzbach LD, Neumann M, Lee VM-Y, Trojanowski JQ (2009) Transactive response DNA-binding protein 43 burden in familial Alzheimer disease and Down syndrome. Arch Neurol 66:1483–1488
Mackenzie IR, Rademakers R, Neumann M (2010) TDP-43 and FUS in amyotrophic lateral sclerosis and Frontotemporal dementia. Lancet Neurol 10:995–1007
Mann DMA (1988) Alzheimer’s disease and Down’s syndrome. Histopathology 13:125–138
McKhann G, Drachman D, Folstein M (1984) Clinical diagnosis of Alzheimer’s disease report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s disease. Neurology 34:939–944
Mirra SS, Heyman A, McKeel D (1991) The consortium to establish a registry for Alzheimer’s disease Part II. Standardization of the neuropathologic assessment of Alzheimer’s disease. Neurology 41:479–486
Nakashima-Yasuda H, Uryu K, Robinson J, Xie SX, Hurtig H, Duda JE, Arnold SE, Siderowf A, Grossman M, Leverenz JB, Woltjer R, Lopez OL, Hamilton R, Tsuang DW, Galasko D, Masliah E, Kaye J, Clark CM, Montine JB, Lee VM-Y, Trojanowski JQ (2007) Co-morbidity of TDP-43 proteinopathy in Lewy body related diseases. Acta Neuropathol 114:221–229
Nelson PT, Scmitt FA, Lin Y, Abner EL, Jicha GA, Patel E, Thomason PC, Neltner JH, Smith CD, Santacruz KS, Sonnen JA, Poon LW, Gearing M, Green RC, Woodward JL, Van Eldik LJ, Krysio RJ (2011) Hippocampal sclerosis in advanced age: clinical and pathological features. Brain 134:1506–1518
Petrovich H, Ross GW, Steinhorn SC, Abbott RD, Markesbery W, Davis D, Nelson J, Hardman J, Curb JD, Blanchette PL, Launer LJ, Yano K, Markesbery WR (2005) AD lesions and infarcts in demented and non-demented Japanese-American men. Ann Neurol 57:98–103
Snowden JS, Stopford CL, Julien CL, Thompson JC, Davidson Y, Gibbons L, Pritchard A, Lendon CL, Richardson AM, Varma A, Neary D, Mann DMA (2007) Cognitive phenotypes in Alzheimer’s disease and genetic risk. Cortex 43:835–845
Stopford CL, Snowden JS, Thompson JC, Neary D (2008) Variability in cognitive presentation of Alzheimer’s disease. Cortex 44:185–195
Uryu K, Nakashima-Yasuda H, Forman MS, Kwong LK, Clark CM, Grossman M, Miller BL, Kretzschmar HA, Lee VM-Y, Trojanowski JQ, Neumann M (2008) Concomitant TAR-DNA-binding protein 43 pathology is present in Alzheimer disease and corticobasal degeneration but not in other tauopathies. J Neuropathol Exp Neurol 67:555–564
Wang HY, Wang IF, Bose J, Shen CK (2004) Structural diversity and functional implications of the eukaryotic TDP gene family. Genomics 83:130–139
Yokota O, Davidson Y, Arai T, Hasegawa M, Akiyama H, Ishizu H, Terada S, Sikkink S, Pickering-Brown S, Mann DMA (2010) Effect of topographical distribution of α-synuclein pathology on TDP-43 accumulation in Lewy body disease. Acta Neuropathol 120:789–801
Yokota O, Davidson Y, Bigio EH, Ishizu H, Terada S, Arai T, Hasegawa M, Akiyama H, Sikkink S, Pickering-Brown S, Mann DMA (2010) Phosphorylated TDP-43 pathology and hippocampal sclerosis in progressive supranuclear palsy. Acta Neuropathol 120:55–66
Zarow C, Sitzer TE, Chui HC (2008) Understanding hippocampal sclerosis in the elderly: epidemiology, characterisation and diagnostic issues. Curr Neurol Neurosci Rep 8:363–370
Acknowledgments
We thank Helen Morpeth in Pathological Services at Salford Royal Foundation Trust for technical assistance. We acknowledge the assistance of Professor Martin Rossor at Institute of Neurology, Queen Square, London in the collection and characterisation of some of the familial Alzheimer’s disease cases. The work of the Manchester Brain Bank, the Thomas Willis Brain Bank, Oxford, and the Institute of Psychiatry Brain Bank is supported by wholly or in part by Alzheimer’s Research UK and the Alzheimer’s Society through the Brains for Dementia Research Initiative. SR is supported by The Sir John Fisher Foundation. MME is grateful for support from the UK National Institute for Health Research via the Biomedical Research Centre.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Davidson, Y.S., Raby, S., Foulds, P.G. et al. TDP-43 pathological changes in early onset familial and sporadic Alzheimer’s disease, late onset Alzheimer’s disease and Down’s Syndrome: association with age, hippocampal sclerosis and clinical phenotype. Acta Neuropathol 122, 703–713 (2011). https://doi.org/10.1007/s00401-011-0879-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-011-0879-y