Abstract
Background
Current guidelines for the treatment of ST-segment elevation myocardial infarction (STEMI) recommend a door-to-balloon time (DBT) of ≤ 90 min for patients undergoing primary percutaneous coronary intervention (PCI). We aimed to investigate the possible impact of further reduction in DBT intervals beyond the 90 min cutoff on short and long-term outcomes among STEMI patients undergoing primary PCI.
Methods
We retrospectively studied 889 STEMI patients (median age 61 years, 83% men) who underwent successful primary PCI and had a DBT of ≤ 90 min. Patients were stratified according to DBT into 2 groups: < 60 min and 60–90 min. Patients records were assessed for the occurrence of in-hospital complications, 30-day and 1-year mortality.
Results
Patients having DBT < 60 min (n = 608, 68%) were more likely to present earlier, in daytime and weekdays, and had better post-procedural left ventricular ejection fraction and lower 30-day mortality (3% vs. 6%, p = 0.03). Mortality over 1-year was significantly lower among patients having DBT < 60 compared to DBT of 60–90 min (4.6% vs. 9.6%, p = 0.004). In a binary logistic regression model DBT < 60 min was associated with 51% risk reduction for 1-year mortality (OR 0.49, 95% CI 0.25–0.93, p = 0.03).
Conclusions
Among STEMI patients undergoing primary PCI within 90 min of admission DBT < 60 min was independently associated with better 1-year mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Early reperfusion with primary percutaneous coronary intervention (PCI) is currently the recommended treatment strategy for patients presenting with ST segment elevation myocardial infarction (STEMI) [1]. Door-to-balloon time (DBT) is related as the interval from arrival at the hospital until inflation of the balloon to restore flow in the occluded artery.
Studies showed a direct relationship between the duration of coronary occlusion and ischemic myocardial cell injury [2]. Thus, longer time to treatment results in higher mortality [3,4,5,6,7,8,9]. On that account DBT has emerged as key quality indicator for hospital performance [10, 11]. On basis of this time-dependent effect current clinical guidelines recommend that patients should be treated within a DBT of ≤ 90 min (Class I recommendation) [12, 13]. Numerous strategies have been proposed to reach this goal including the admission of patients directly to the cardiac catheterization laboratory or the cardiac intensive care unit bypassing the emergency room (ER) [14,15,16,17]. The utilization of these and other strategies enables many STEMI patients nowadays to be treated within recommended time intervals [18,19,20,21,22]. Limited data exists, however, whether further reduction in DBT beyond the 90-min benchmark has a beneficial effect on outcomes. We aimed to investigate the possible impact of further reduction in DBT intervals beyond the 90-min cutoff on short and long-term outcomes in STEMI patients undergoing primary PCI.
Methods
A retrospective, single-center observational study was performed at the Tel-Aviv Sourasky Medical Center, a tertiary referral hospital with a 24/7 primary PCI service.
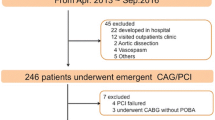
Included were all 1223 consecutive patients admitted between January 2013 and August 2017 with the diagnosis of acute STEMI subsequently treated with primary PCI (as previously described [23, 24]. We excluded patients transferred from other hospitals (n = 4), patients in whom information regarding survival during the first year after PCI was not available (n = 155) and patients with no documented DBT in medical records (n = 16). We further excluded patients with DBT > 90 min (n = 159). The final study population included 889 STEMI patients. Diagnosis of STEMI was established in accordance to published guidelines including a typical chest pain history, diagnostic electrocardiographic changes, and serial elevation of cardiac biomarkers [13]. Primary PCI was performed in patients with symptoms ≤ 12 h in duration, as well as in patients with symptoms lasting 12–24 h if pain consisted at the time of admission. Symptom duration was defined as the time from symptom onset (usually chest pain or discomfort) to ER/catheterization laboratory admission. Door-to-balloon time was defined as the time in minutes between a patient’s arrival at the hospital (taken from the computerized patient file) and the first balloon inflation or device deployment in the culprit artery as documented in the patient’s medical record. A culprit artery was defined as one with an identifiable thrombotic lesion on an angiogram corresponding to electrocardiographic changes. For the purpose of evaluating differences in patient characteristics and outcomes associated with DBT, we stratified patients into 2 groups: < 60 and 60–90 min. Baseline demographics, cardiovascular history, clinical risk factors, treatment characteristics and laboratory results were all retrieved from the hospital electronic medical records. Patient records were evaluated for in-hospital mortality and complications occurring during the hospitalization. These included cardiogenic shock or the need for intra-aortic balloon counterpulsation treatment, mechanical ventilation or heart failure episodes treated conservatively, clinically significant tachyarrhythmia’s, bradyarrhythmias requiring pacemaker and major bleedings (requiring blood transfusion). Assessment of survival for 1 year following hospital discharge was determined from computerized records of the population registry bureau.
Continuous variables were presented as mean ± standard deviation and compared with the independent sample t test when normally distributed. Median and interquartile range was used in cases of non-normally distributed continuous variables. These variables were compared with Mann–Whitney U test. Categorical variables are presented as percentages; p values were calculated with the Chi-squared test. Independent predictors of 1-year mortality were determined in a multivariate binary logistic regression model adjusted for all baseline variables found to be significant in the univariate analysis. Survival rates were described by the Kaplan–Meier method. A two-tailed p value of < 0.05 was considered significant for all analyses. All analyses were performed with the SPSS software (SPSS Inc., Chicago, IL).
Results
Study population included 889 STEMI patients (median age 61 years [Interquartile range 52–69], 83% men), 608 of whom (68%) had DBT < 60 min. Table 1 presents the baseline characteristics of patients with DBT under 60 min and patients with DBT between 60 and 90 min. Patients having DBT < 60 min were more likely to present to hospital earlier following symptom onset, at daytime, weekdays, and to bypass the emergency room. Table 2 presents the procedural outcomes and in-hospital complication of both patients groups. Compared to patients having a DBT of 60–90 min, patients with DBT < 60 min were less likely to have left ventricular (EF) ≤ 45% (51% vs.62%, p = 0.002) and had lower 30-day mortality (3% vs. 6%, p = 0.03). During 1-year follow–up, 55 (6.1%) of study patients died. Mortality was significantly lower among patients having DBT < 60 min (4.6% vs. 9.6%, log-rank p = 0.004, Fig. 1).
As presented in Table 3 in a multivariate binary logistic regression model DBT < 60 min was independently associated with 51% risk reduction for 1-year mortality (OR 0.49,95% CI 0.25–0.93, p = 0.03). Other factors independently associated with 1-year mortality risk included age > 60 years, hypertension and left ventricular EF ≤ 45%.
Discussion
The main finding of our study is that among STEMI patients undergoing primary PCI, further reduction in DBT, even among patients treated successfully within 90 min of admission is independently associated with better 1-year survival.
Primary PCI for STEMI patients has been recommended within a DBT of ≤ 90 min for over the last decade [13, 25]. Based on current guideline recommendations assessment of this cut-off became focus of large registries and was utilized as a major objective for quality assessment [10, 11]. Furthermore, the AHA/ACC launched a campaign named “door-to-balloon (D2B): an alliance for quality” aimed to increase the percentage of STEMI patients treated within DBT of ≤ 90 min. Studies showed that all these efforts brought remarkable improvement, enabling a large share of patients to be treated within the “acceptable” time intervals nowadays [19, 22].
Delay in primary PCI from the time of arrival at a medical center correlates with infarction size [26]. It is well established as well that prolonged DBT results in increased mortality [3,4,5, 27]. The specific shape of association is, however, a matter of debate. It is still unclear whether any postponement in treatment is harmful or outcome worsens only after an initial time delay [2, 28]. Pushing beyond the 90-min DBT benchmark is well possible nowadays raising the question what time interval should be desirable for STEMI patients today [19, 22, 29].
Most studies evaluating DBT restricted categorical modelling to cutoffs of 90 min or 2 h [5, 7, 8]. Others presented a statistical linear relationship between treatment delay and mortality risk describing time as continuous variable without being able to suggest target cutoffs for improved outcome [3, 6]. Limited data is present regarding DBT cutoffs under 90 min. Gibson et al. reported a significant fall in in-hospital mortality associated with a reduction of median DBT from 111 to 79 min over a time period of 20-years in patients enrolled in the National Registry of Myocardial Infarction (NRMI) [29]. This finding, however, was questioned by later observations from large databases failing to show improved short-term outcome despite significant decline in median DBT over the years [19, 22]. Berger et al. demonstrated improvement in 30-day survival when DBT was reduced from 90 to < 60 min. This report published over 20 years ago, included a limited amount of patients who were part of a larger multicenter trial (GUSTO-IIb) comparing thrombolytic therapy to PTCA, thus being limited to past pharmacological treatment protocols and prone to bias due to varying procedural quality between centers [4]. Another report presented an analysis of a large cohort of STEMI patients treated with primary PCI who were enrolled in the American college of cardiology national cardiovascular data registry [9]. Results showed increased in-hospital mortality for treatment delays even within the endorsed 90-min’ time interval with lowest mortality rates among patients with DBT below 30 min. Because data were collected from over 600 different catheterization laboratories results may be biased by inconsistent operator quality and different procedural protocols all affecting DBT. In contrast to the current study, both trials mentioned above failed to report outcomes later than 30 days after PCI.
Numerous strategic approaches have been recommended to shorten the time interval from admission to treatment [17]. Bypassing the ER was first recommended by the European Society of Cardiology in 2012 [14]. Pre-hospital electrocardiogram (ECG) diagnosis is one of the strategies recommended by the D2B campaign. Prehospital ECG and subsequent direct ambulance admission bypassing the ER both showed significant impact on DBT [15, 16, 30]. Indeed, our data showed a higher probability of achieving shorter DBT when bypassing the ER.
Many STEMI networks accept primary PCI within 120 min after first medical contact based on recent guidelines [12, 13]. The organization of an optimal STEMI network needs to be customized and refined by regional health system. Components should include a system for early diagnosis, fast patient transfer, optimal door-to-device organization, and an experienced team of interventionists. Regular control of time delays in existing STEMI networks by running a registry is important to detect potential time delays and respective reasons and to improve the quality of such networks [30].
We acknowledge several important limitations of our study. This was a single-center retrospective and non-randomized observational study; thus findings might be attributed to biases related to unmeasured factors. We attempted to mitigate this effect through robust risk adjustment but cannot preclude the possibility of residual confounding by other non-measured patient or hospital factors associated with DBT time or mortality. In addition, as the study included only patients who were undergoing primary PCI, the results cannot be generalized to all STEMI patients.
Change history
15 November 2019
The original version of this article unfortunately contained a mistake. The name of the author Keren-Lee Rozenfeld was rendered wrongly. The correct name is shown above.
15 November 2019
The original version of this article unfortunately contained a mistake. The name of the author Keren-Lee Rozenfeld was rendered wrongly. The correct name is shown above.
References
Keeley EC, Boura JA, Grines CL (2003) Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 361(9351):13–20. https://doi.org/10.1016/S0140-6736(03)12113-7
Garcia-Dorado D, Theroux P, Elizaga J, Galinanes M, Solares J, Riesgo M, Gomez MJ, Garcia-Dorado A, Fernandez Aviles F (1987) Myocardial reperfusion in the pig heart model: infarct size and duration of coronary occlusion. Cardiovasc Res 21(7):537–544
De Luca G, Suryapranata H, Ottervanger JP, Antman EM (2004) Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation 109(10):1223–1225. https://doi.org/10.1161/01.CIR.0000121424.76486.20
Berger PB, Ellis SG, Holmes DR Jr, Granger CB, Criger DA, Betriu A, Topol EJ, Califf RM (1999) Relationship between delay in performing direct coronary angioplasty and early clinical outcome in patients with acute myocardial infarction: results from the global use of strategies to open occluded arteries in acute coronary syndromes (GUSTO-IIb) trial. Circulation 100(1):14–20
McNamara RL, Wang Y, Herrin J, Curtis JP, Bradley EH, Magid DJ, Peterson ED, Blaney M, Frederick PD, Krumholz HM, Investigators N (2006) Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol 47(11):2180–2186. https://doi.org/10.1016/j.jacc.2005.12.072
Nallamothu B, Fox KA, Kennelly BM, Van de Werf F, Gore JM, Steg PG, Granger CB, Dabbous OH, Kline-Rogers E, Eagle KA, Investigators G (2007) Relationship of treatment delays and mortality in patients undergoing fibrinolysis and primary percutaneous coronary intervention. The Global Registry of Acute Coronary Events. Heart 93(12):1552–1555. https://doi.org/10.1136/hrt.2006.112847
Brodie BR, Hansen C, Stuckey TD, Richter S, Versteeg DS, Gupta N, Downey WE, Pulsipher M (2006) Door-to-balloon time with primary percutaneous coronary intervention for acute myocardial infarction impacts late cardiac mortality in high-risk patients and patients presenting early after the onset of symptoms. J Am Coll Cardiol 47(2):289–295. https://doi.org/10.1016/j.jacc.2005.08.065
Brodie BR, Stone GW, Cox DA, Stuckey TD, Turco M, Tcheng JE, Berger P, Mehran R, McLaughlin M, Costantini C, Lansky AJ, Grines CL (2006) Impact of treatment delays on outcomes of primary percutaneous coronary intervention for acute myocardial infarction: analysis from the CADILLAC trial. Am Heart J 151(6):1231–1238. https://doi.org/10.1016/j.ahj.2005.07.016
Rathore SS, Curtis JP, Chen J, Wang Y, Nallamothu BK, Epstein AJ, Krumholz HM, National Cardiovascular Data R (2009) Association of door-to-balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: national cohort study. BMJ 338:b1807. https://doi.org/10.1136/bmj.b1807
Krumholz HM, Bradley EH, Nallamothu BK, Ting HH, Batchelor WB, Kline-Rogers E, Stern AF, Byrd JR, Brush JE Jr (2008) A campaign to improve the timeliness of primary percutaneous coronary intervention: door-to-balloon: an alliance for quality. JACC Cardiovasc Interv 1(1):97–104. https://doi.org/10.1016/j.jcin.2007.10.006
Jacobs AK, Antman EM, Ellrodt G, Faxon DP, Gregory T, Mensah GA, Moyer P, Ornato J, Peterson ED, Sadwin L, Smith SC, American Heart Association’s Acute Myocardial Infarction Advisory Working G (2006) Recommendation to develop strategies to increase the number of ST-segment-elevation myocardial infarction patients with timely access to primary percutaneous coronary intervention. Circulation 113(17):2152–2163. https://doi.org/10.1161/CIRCULATIONAHA.106.174477
Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH, Accf, Aha, Scai (2012) 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv 79(3):453–495. https://doi.org/10.1002/ccd.23438
O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, American College of Cardiology F, American Heart Association Task Force on Practice G, American College of Emergency P, Society for Cardiovascular A, Interventions (2013) 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the American College of Emergency Physicians and Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv 82(1):E1–E27. https://doi.org/10.1002/ccd.24776
Task Force on the management of STseamiotESoC, Steg PG, James SK, Atar D, Badano LP, Blomstrom-Lundqvist C, Borger MA, Di Mario C, Dickstein K, Ducrocq G, Fernandez-Aviles F, Gershlick AH, Giannuzzi P, Halvorsen S, Huber K, Juni P, Kastrati A, Knuuti J, Lenzen MJ, Mahaffey KW, Valgimigli M, van ‘t Hof A, Widimsky P, Zahger D (2012) ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 33 (20):2569–2619. https://doi.org/10.1093/eurheartj/ehs215
Dorsch MF, Greenwood JP, Priestley C, Somers K, Hague C, Blaxill JM, Wheatcroft SB, Mackintosh AF, McLenachan JM, Blackman DJ (2008) Direct ambulance admission to the cardiac catheterization laboratory significantly reduces door-to-balloon times in primary percutaneous coronary intervention. Am Heart J 155(6):1054–1058. https://doi.org/10.1016/j.ahj.2008.01.014
Lubovich A, Dobrecky-Mery I, Radzishevski E, Samnia N, Matetzky S, Nagler R, Rosenschein U (2015) Bypassing the emergency room to reduce door-to-balloon time and improve outcomes of ST elevation myocardial infarction patients: analysis of data from 2004 to 2010 ACSIS registry. J Interv Cardiol 28(2):141–146. https://doi.org/10.1111/joic.12192
Bradley EH, Curry LA, Webster TR, Mattera JA, Roumanis SA, Radford MJ, McNamara RL, Barton BA, Berg DN, Krumholz HM (2006) Achieving rapid door-to-balloon times: how top hospitals improve complex clinical systems. Circulation 113(8):1079–1085. https://doi.org/10.1161/CIRCULATIONAHA.105.590133
Krumholz HM, Herrin J, Miller LE, Drye EE, Ling SM, Han LF, Rapp MT, Bradley EH, Nallamothu BK, Nsa W, Bratzler DW, Curtis JP (2011) Improvements in door-to-balloon time in the United States, 2005 to 2010. Circulation 124(9):1038–1045. https://doi.org/10.1161/CIRCULATIONAHA.111.044107
Menees DS, Peterson ED, Wang Y, Curtis JP, Messenger JC, Rumsfeld JS, Gurm HS (2013) Door-to-balloon time and mortality among patients undergoing primary PCI. N Engl J Med 369(10):901–909. https://doi.org/10.1056/NEJMoa1208200
Mentias A, Raza MQ, Barakat AF, Youssef D, Raymond R, Menon V, Simpfendorfer C, Franco I, Ellis S, Tuzcu EM, Kapadia SR (2017) Effect of shorter door-to-balloon times over 20 years on outcomes of patients with anterior ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am Heart J Cardiol 120(8):1254–1259. https://doi.org/10.1016/j.amjcard.2017.07.006
Khoury S, Carmon S, Margolis G, Keren G, Shacham Y (2017) Incidence and outcomes of early left ventricular thrombus following ST-elevation myocardial infarction treated with primary percutaneous coronary intervention. Clin Res Cardiol 106(9):695–701. https://doi.org/10.1007/s00392-017-1111-4
Flynn A, Moscucci M, Share D, Smith D, LaLonde T, Changezi H, Riba A, Gurm HS (2010) Trends in door-to-balloon time and mortality in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Arch Intern Med 170(20):1842–1849. https://doi.org/10.1001/archinternmed.2010.381
Flint N, Kaufman N, Gal-Oz A, Margolis G, Topilsky Y, Keren G, Shacham Y (2017) Echocardiographic correlates of left ventricular filling pressures and acute cardio-renal syndrome in ST segment elevation myocardial infarction patients. Clin Res Cardiol 106(2):120–126. https://doi.org/10.1007/s00392-016-1031-8
Khoury S, Steinvil A, Gal-Oz A, Margolis G, Hochstatd A, Topilsky Y, Keren G, Shacham Y (2018) Association between central venous pressure as assessed by echocardiography, left ventricular function and acute cardio-renal syndrome in patients with ST segment elevation myocardial infarction. Clin Res Cardiol. https://doi.org/10.1007/s00392-018-1266-7
Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC Jr, American College of C, American Heart A, Canadian Cardiovascular S (2004) ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction–executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction). J Am Coll Cardiol 44 (3):671–719. https://doi.org/10.1016/j.jacc.2004.07.002
Stone GW, Dixon SR, Grines CL, Cox DA, Webb JG, Brodie BR, Griffin JJ, Martin JL, Fahy M, Mehran R, Miller TD, Gibbons RJ, O’Neill WW (2007) Predictors of infarct size after primary coronary angioplasty in acute myocardial infarction from pooled analysis from four contemporary trials. Am Heart J Cardiol 100(9):1370–1375. https://doi.org/10.1016/j.amjcard.2007.06.027
Cannon CP, Gibson CM, Lambrew CT, Shoultz DA, Levy D, French WJ, Gore JM, Weaver WD, Rogers WJ, Tiefenbrunn AJ (2000) Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. Jama 283(22):2941–2947
Reimer KA, Vander Heide RS, Richard VJ (1993) Reperfusion in acute myocardial infarction: effect of timing and modulating factors in experimental models. Am Heart J Cardiol 72(19):13G–21G
Gibson CM, Pride YB, Frederick PD, Pollack CV Jr, Canto JG, Tiefenbrunn AJ, Weaver WD, Lambrew CT, French WJ, Peterson ED, Rogers WJ (2008) Trends in reperfusion strategies, door-to-needle and door-to-balloon times, and in-hospital mortality among patients with ST-segment elevation myocardial infarction enrolled in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J 156(6):1035–1044. https://doi.org/10.1016/j.ahj.2008.07.029
Curtis JP, Portnay EL, Wang Y, McNamara RL, Herrin J, Bradley EH, Magid DJ, Blaney ME, Canto JG, Krumholz HM, National Registry of Myocardial I (2006) The pre-hospital electrocardiogram and time to reperfusion in patients with acute myocardial infarction, 2000–2002: findings from the National Registry of Myocardial Infarction-4. J Am Coll Cardiol 47(8):1544–1552. https://doi.org/10.1016/j.jacc.2005.10.077
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
The study protocol was approved by the local institutional ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informal consent
All persons gave their informed consent prior to their inclusion in the study.
Rights and permissions
About this article
Cite this article
Zahler, D., Lee-Rozenfeld, K., Ravid, D. et al. Relation of lowering door-to-balloon time and mortality in ST segment elevation myocardial infarction patients undergoing percutaneous coronary intervention. Clin Res Cardiol 108, 1053–1058 (2019). https://doi.org/10.1007/s00392-019-01438-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-019-01438-6