Abstract
Door to balloon (D2B) time was reported an important factor of the clinical outcome of patients with ST-segment elevation myocardial infarction (STEMI) treated with primary percutaneous coronary intervention (PCI). D2B time is influenced by various factors; however, modifiable factors have not been adequately evaluated. The purpose of this study was to identify modifiable factors associated with prolonged D2B time. We historically included 239 consecutive STEMI patients who visited emergency department and underwent primary PCI between April 2013 and September 2016. We evaluated baseline characteristics, mode and timing of hospital arrival, symptoms and signs, treatment times and angiographic characteristics. Patients with D2B time > 90 min were compared with those with D2B time ≤ 90 min. Modifiable factors associated with prolonged D2B time (> 90 min) were analyzed by multivariable logistic regression model. The median D2B time for the entire cohort was 69 min (interquartile range 54–89) and 24% had a D2B time of > 90 min. Modifiable factors associated with prolonged treatment time (D2B time > 90 min) were electrocardiogram (ECG) to puncture time > 50 min [odds ratios (OR) 96.0, 95% confidence intervals (95% CI) 25.1–652.5, P < 0.0001), door to ECG time > 10 min (OR 49.8, 95% CI 11.8–357.5, P < 0.0001), and puncture to balloon time > 30 min (OR 48.5, 95% CI 12.0–333.8, P < 0.0001). ECG to puncture time > 50 min was the most important modifiable factor associated with prolonged D2B time in STEMI patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with ST-segment elevation myocardial infarction (STEMI) require rapid triage and early reperfusion therapy. Door to balloon (D2B) time was defined as the interval from arrival at the hospital where percutaneous coronary intervention (PCI) was performed to the first balloon inflation or device deployment. D2B time is an extremely important factor of survival in STEMI patients treated with primary PCI [1, 2]. Current guidelines suggest D2B time be less than 90 min [3, 4], the rate at which this is achieved has improved in recent years [2, 5]. However, in clinical practice, we also experience many cases that cannot be achieved D2B time ≤ 90 min. Although D2B time is influenced by various factors such as patient characteristics, hospital characteristics, health care practices and physician characteristics [6], modifiable factors associated with prolonged D2B time have not been adequately evaluated. The purpose of this study was to identify modifiable factors associated with prolonged D2B time.
Materials and methods
Study population
We conducted historical cohort study at a single center to identify factors associated with prolonged D2B time. We retrieved consecutive STEMI patients who visited at Tokyo Bay Medical Center (Urayasu, Japan) from April 2013 to September 2016. Of these, the patients who visited emergency department (ED), diagnosed as STEMI and underwent emergency primary PCI were included. Diagnosis of myocardial infarction (MI) was based on ESC/ACCF/AHA/WHF (European Society of Cardiology, American College of Cardiology Foundation, American Heart Association, and World Heart Federation) Third Universal Definition [7]. STEMI patients had ischemic symptoms, persistent ST-segment elevation on the electrocardiogram (ECG) and elevated biochemical marker of myocardial necrosis. The ECG of STEMI was defined as persistent ST-segment elevation 1 mm in 2 contiguous leads, a new or presumed new left bundle branch block, an isolated posterior MI and lead aVR ST elevation with infero-lateral ST depression. The following patients were excluded: patients who developed STEMI in hospital, patients who visited outpatient clinic, patients who underwent coronary artery bypass graft surgery without balloon inflation or device deployment and patients with aortic dissection or vasospasm. The diagnosis of STEMI was made by the emergency physician in Tokyo Bay Medical Center. The indication of primary PCI was as follows: (1) STEMI patients within 12 h of symptom onset; and (2) STEMI patients with symptoms lasting > 12 h in the presence of ongoing or recurrent symptoms including signs of heart failure, hemodynamic instability, or life-threatening arrhythmias. The cardiac catheterization laboratory was activated by the emergency physician or the interventional cardiologist using an emergency paging system. All patients were treated based on the current guidelines [3, 4]; primary PCI was performed using standard techniques by 3-experienced interventional cardiologists. The treatment strategies for each patient were left to the discretion of interventional cardiologists. Informed consent was obtained from all patients prior to PCI. This study complied with the Declaration of Helsinki and was approved by the review committee of Tokyo Bay Medical Center, Japan.
Data collection
We obtained data including baseline characteristics, mode and timing of hospital arrival, symptoms and signs, procedure and angiographic characteristics, treatment times and in-hospital death from case databases and medical records. Baseline characteristics of the study population included age, gender and medical history. Mode and timing of hospital arrival included direct arrival by walk-in, STEMI diagnosis on arrival, weekday or weekend and off-hour presentation. Direct arrival by walk-in was defined as arriving hospital by self or private transportation, public transportation or walking to the hospital. STEMI diagnosis on arrival was defined as the patient who was diagnosed with STEMI and was transported by emergency medical service from the family physician or non-PCI-capable hospitals. Weekend was defined as Saturday, Sunday, or a slightly longer period, as a holiday/vacation. Off-hour presentation was defined as arriving hospital from 5 p.m. to 8 a.m. Symptoms and signs included patients’ symptom, systolic blood pressure, heart rate, congestive heart failure (Killip classification ≥ 2), cardiopulmonary arrest on arrival (CPAOA) and cardiogenic shock without CPAOA. Typical chest pain was defined as any symptom of chest pain or pressure due to myocardial ischemia. We did not consider the specific symptoms of shortness of breath, chest discomfort, nausea, vomiting, syncope, or none of those symptoms as typical chest pain. Cardiogenic shock was defined as a systolic blood pressure of less than 90 mmHg on arrival. Procedural and angiographic characteristics included intubation before procedure, mechanical support before procedure (temporary pacing, intra-aortic balloon pumping, percutaneous cardiopulmonary support device), access site, infarct-related artery location and pre-procedure TIMI flow grade 0. Treatment times included door to ECG, ECG to puncture time, and puncture to balloon time. Door to ECG time was defined as the interval from arrival at the hospital to obtaining an ECG. ECG to puncture time was defined as the interval form obtaining an ECG to start of PCI procedure. Puncture to balloon time was defined as the interval from start of PCI procedure to first balloon inflation or device deployment.
Statistical analysis
Continuous variables are expressed as mean and standard deviation (SD) or median values with interquartile range (IQR) based on their distributions. Categorical variables are expressed as number and percentages. Baseline characteristics, mode and timing of hospital arrival, symptoms and signs, procedure and angiographic characteristics, treatment times and in-hospital death were compared between D2B time > or ≤ 90 min using Student’s t test or Wilcoxon rank-sum test for continuous variables based on the distributions, and Chi square test or Fisher’s extract test for categorical variables when appropriate. When comparing continuous variables between more than 2 groups, we used Kruskal–Wallis test. To identify factors associated with prolonged D2B time (> 90 min), multivariate logistic regression model was constructed adjusting for the following clinically modifiable factors: door to ECG time > 10 min, ECG to puncture time > 50 min, and puncture to balloon time > 30 min. The results of the multivariate logistic regression model were expressed as odds ratios (OR) for the comparison of risk with 95% confidence intervals (CI). Two-tailed P < 0.05 was considered to be statistically significant. All statistical analyses were performed with JMP 13 (SAS Institute, Cary, NC, USA).
Results
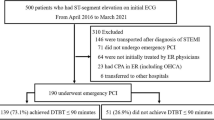
We enrolled 291 consecutive STEMI patients and 52 of these patients met exclusion criteria and 239 patients were included in this study (Fig. 1). The median D2B time for the entire cohort was 69 min (54–89) and 24% of patients had a D2B > 90 min (Fig. 2). Baseline characteristics, mode and timing of hospital arrival, symptoms and signs, procedure and angiographic characteristics and treatment times are shown in Tables 1 and 2. Overall, the mean age was 66 (14) years and 20.1% were female. Patients with D2B time > 90 min were more likely to have renal insufficiency without hemodialysis, previous cerebrovascular disease, absence of typical chest pain, to present with evidence of heart failure than patients with D2B time ≤ 90 min. Direct arrival by walk-in, intubation before procedure and mechanical support before procedure were significantly higher in patients with D2B time > 90 min than ≤ 90 min. There was no significant difference for the timing of hospital arrival (weekend and off-hour) between D2B time > 90 and ≤ 90 min. Median door to ECG time, ECG to puncture time, and puncture to balloon time were significantly longer in patients with D2B time > 90 min. Clinical outcomes including in-hospital death were significantly higher in patients with D2B time > 90 min compared with patients with D2B time ≤ 90 min (14.0 vs. 4.4%, P = 0.01). Door to ECG time > 10 min was more likely in patients with direct arrival by walk-in and absence of typical chest pain (Table 3). ECG to puncture time > 50 min was more likely in patients with direct arrival by walk-in, absence of typical chest pain, off-hour presentation and congestive heart failure (Table 4). Puncture to balloon time > 30 min was more likely in serious cases with congestive heart failure and those requiring intubation and/or mechanical device support (Table 5). Modifiable factors associated with prolonged D2B time are listed in Table 6. The clinically modifiable factors for prolonged D2B time including door to ECG time > 10 min, ECG to puncture time > 50 min, and puncture to ECG time > 30 min were identified. In the multivariate logistic model, modifiable factors associated with prolonged treatment time (D2B time > 90 min) were ECG to puncture time > 50 min (OR 96.0, 95% CI 25.1–652.5, P < 0.0001), door to ECG time > 10 min (OR 49.8, 95% CI 11.8–357.5, P < 0.0001), and puncture to balloon time > 30 min (OR 48.5, 95% CI 12.0–333.8, P < 0.0001).
Discussion
In this study, we showed that ECG to puncture time accounts for a substantial proportion of the delay in primary PCI for STEMI patients. In addition, ECG to puncture time > 50 min was the most important modifiable factor associated with prolonged D2B time in STEMI patients. ECG to puncture time is divided into appropriate interpretation of ECG and activation of cardiac catheterization laboratory. Appropriate interpretation of ECG leads to the activation of cardiac catheterization laboratory immediately. However, in clinical practice, we experience several cases that cannot be judged promptly. In this study, ECG to puncture time was prolonged in cases of direct arrival by walk-in, absence of typical chest pain, and congestive heart failure. The reason for this is not entirely clear; it might be because that ECG alone could not be judged. Therefore, laboratory, radiographic, and echocardiographic results might have been needed to activate catheterization team. Furthermore, activation process of cardiac catheterization laboratory was also important. In the present analysis, ECG to puncture time was prolonged during off-time presentation. This may be improved by specific hospital strategy such as expecting staff to arrive in the catheterization laboratory within 20 min after being paged and having an attending cardiologist always on site [8].
Door to ECG time was also important modifiable factor. Current ESC guideline emphasizes that a 12-lead ECG must be obtained as soon as possible with a target delay of ≤ 10 min [4]. However, recent study reported that the proportion of STEMI patients with door to ECG time > 10 min was high [9]. In this study, door to ECG time > 10 min was more likely in patients with direct arrival by walk-in and absence of typical chest pain. In the National Cardiovascular Data Registry (NCDR) Acute Coronary Treatment and Intervention Outcomes Network Registry–Get With the Guidelines (ACTION Registry–GWTG), about 40% of STEMI patients arrived hospital by walk-in [10]. Direct arrival by walk-in patients with STEMI compared with emergency medical service (EMS) transported patients do not receive a pre-hospital electrocardiogram and sufficient triage process, resulting in delayed ECG acquisition. In fact, in ACTION Registry–GWTG, the STEMI patients with direct arrival by walk-in had significantly delayed in door to ECG time compared with EMS transported patient (median door to ECG time, 8 vs. 5 min; P < 0.0001) [10]. In addition, about 20–30% of the STEMI patients do not have typical chest pain [11, 12]. The patients with the absence of typical chest pain experience significant delays in door to ECG time and treatment compared with patients who present with typical chest pain [13]. Immediate ECG at triage in the ED is the first STEMI care target to achieve timely intervention because obtaining an ECG as soon as possible and appropriate interpretation lead to activation of the cardiac catheterization laboratory promptly. However, current guidelines do not include a standardized approach to determine which STEMI patients with direct arrival by walk-in and absence of typical chest pain should receive an immediate ECG at triage in the ED. According to one retrospective study, a simple ECG prioritization rule based on age and presenting symptoms in the ED can identify patients during triage who are at high risk for STEMI and, therefore, should receive an immediate ECG [14].
Puncture to balloon time depends on comorbid conditions and PCI procedure. Additional time required to stabilize respiratory status and/or hemodynamic instabilities may all lead to prolonged puncture to balloon time. Therefore, in this study, puncture to balloon time > 30 min was more likely in serious cases with congestive heart failure and those requiring intubation and/or mechanical device. These conditions are not indications for intervention and it is necessary to improve PCI procedure to reduce puncture to balloon time. Several reports suggested that using a single universal guiding catheter and direct primary PCI without diagnostic angiography of non-culprit vessels significantly reduced puncture to balloon time [15, 16].
Study limitations
There are several limitations in this study. First, our study is a single-center, historical cohort study. Therefore, patients included in this study might be biased from selection bias, if any. Some important confounding factors also might not be recorded and not adjusted for the multivariable models as a result. Secondly, variability in diagnosis and treatment of STEMI between doctors might exist. Finally, our study was a historical cohort study; we could not discuss what method may shorten D2B time in STEMI patients.
Conclusions
In this study, ECG to puncture time > 50 min was the most important modifiable factor associated with prolonged door-to-balloon time in STEMI patients. Further studies will be necessary whether modification of ECG to puncture time might be a good target for shortening of D2B time in STEMI patients.
References
McNamara RL, Wang Y, Herrin J, Curtis JP, Bradley EH, Magid DJ, Peterson ED, Blaney M, Frederick PD, Krumholz HM, Investigators NRMI (2006) Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol 47:2180–2186
Nallamothu BK, Normand SL, Wang Y, Hofer TP, Brush JE Jr, Messenger JC, Bradley EH, Rumsfeld JS, Krumholz HM (2015) Relation between door-to-balloon times and mortality after primary percutaneous coronary intervention over time: a retrospective study. Lancet 385:1114–1122
O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW, American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines (2013) 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 127:e362–e425
Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC), Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, Borger MA, Di Mario C, Dickstein K, Ducrocq G, Fernandez-Aviles F, Gershlick AH, Giannuzzi P, Halvorsen S, Huber K, Juni P, Kastrati A, Knuuti J, Lenzen MJ, Mahaffey KW, Valgimigli M, van ‘t Hof A, Widimsky P, Zahger D (2012) ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 33:2569–2619
Menees DS, Peterson ED, Wang Y, Curtis JP, Messenger JC, Rumsfeld JS, Gurm HS (2013) Door-to-balloon time and mortality among patients undergoing primary PCI. N Engl J Med 369:901–909
Peterson MC, Syndergaard T, Bowler J, Doxey R (2012) A systematic review of factors predicting door to balloon time in ST-segment elevation myocardial infarction treated with percutaneous intervention. Int J Cardiol 157:8–23
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction, Katus HA, Lindahl B, Morrow DA, Clemmensen PM, Johanson P, Hod H, Underwood R, Bax JJ, Bonow RO, Pinto F, Gibbons RJ, Fox KA, Atar D, Newby LK, Galvani M, Hamm CW, Uretsky BF, Steg PG, Wijns W, Bassand JP, Menasché P, Ravkilde J, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Simoons ML, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos G, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood D, Smith SC, Hu D, Lopez-Sendon JL, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis S (2012) Third universal definition of myocardial infarction. Circulation 126:2020–2035
Bradley EH, Herrin J, Wang Y, Barton BA, Webster TR, Mattera JA, Roumanis SA, Curtis JP, Nallamothu BK, Magid DJ, McNamara RL, Parkosewich J, Loeb JM, Krumholz HM (2006) Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med 355:2308–2320
Takakuwa KM, Burek GA, Estepa AT, Shofer FS (2009) A method for improving arrival-to-electrocardiogram time in emergency department chest pain patients and the effect on door-to-balloon time for ST-segment elevation myocardial infarction. Acad Emerg Med 16:921–927
Mathews R, Peterson ED, Li S, Roe MT, Glickman SW, Wiviott SD, Saucedo JF, Antman EM, Jacobs AK, Wang TY (2011) Use of emergency medical service transport among patients with ST-segment—elevation myocardial infarction findings from the National Cardiovascular Data Registry Acute Coronary Treatment Intervention Outcomes Network Registry-Get with the Guidelines. Circulation 124:154–163
Fujino M, Ishihara M, Ogawa H, Nakao K, Yasuda S, Noguchi T, Ozaki Y, Kimura K, Suwa S, Fujimoto K, Nakama Y, Morita T, Shimizu W, Saito Y, Hirohata A, Morita Y, Inoue T, Okamura A, Uematsu M, Ako J, Nakai M, Nishimura K, Miyamoto Y, Investigators J-MINUET (2017) Impact of symptom presentation on in-hospital outcomes in patients with acute myocardial infarction. J Cardiol 70:29–34
Canto AJ, Kiefe CI, Goldberg RJ, Rogers WJ, Peterson ED, Wenger NK, Vaccarino V, Frederick PD, Sopko G, Zheng ZJ, Canto JG (2012) Differences in symptom presentation and hospital mortality according to type of acute myocardial infarction. Am Heart J 163:572–579
Canto JG, Shlipak MG, Rogers WJ, Malmgren JA, Frederick PD, Lambrew CT, Ornato JP, Barron HV, Kiefe CI (2000) Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA 283:3223–3229
Glickman SW, Shofer FS, Wu MC, Scholer MJ, Ndubuizu A, Peterson ED, Granger CB, Cairns CB, Glickman LT (2012) Development and validation of a prioritization rule for obtaining an immediate 12-lead electrocardiogram in the emergency department to identify ST-elevation myocardial infarction. Am Heart J 163:372–382
Torii S, Fujii T, Mutakami T, Nakazawa G, Ichiji T, Nakano M, Ohno Y, Shinozaki N, Yoshimachi F, Ikari Y (2017) Impact of a single universal guiding catheter on door-to-balloon time in primary transradial coronary intervention for ST segment elevation myocardial infarction. Cardiovasc Interv Ther 32:114–119
Plourde G, Abdelaal E, Bataille Y, MacHaalany J, Déry JP, Déry U, Larose É, Larochellière R, Gleeton O, Barbeau G, Roy L, Costerousse O, Bertrand OF (2013) Effect on door-to-balloon time of immediate transradial percutaneous coronary intervention on culprit lesion in ST-elevation myocardial infarction compared to diagnostic angiography followed by primary percutaneous coronary intervention. Am J Cardiol 111:836–840
Acknowledgements
We thank the members of the cardiac catheterization laboratory and the emergency department at Tokyo Bay Urayasu Ichikawa Medical Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has conflicts of interest to disclose regarding this study.
Rights and permissions
About this article
Cite this article
Noguchi, M., Ako, J., Morimoto, T. et al. Modifiable factors associated with prolonged door to balloon time in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Heart Vessels 33, 1139–1148 (2018). https://doi.org/10.1007/s00380-018-1164-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-018-1164-y