Abstract
Background
Since the advent of primary percutaneous coronary intervention (PCI), studies have reported a declining incidence of left ventricular thrombus (LVT) following ST-elevation myocardial infarction (STEMI). We investigated the incidence and outcomes of early (pre-discharge) LVT in the contemporary era of PCI practice in a large cohort of STEMI patients.
Methods
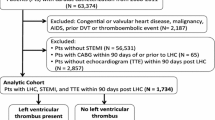
We retrospectively studied 2071 consecutive STEMI patients who underwent successful primary PCI. Screening echocardiography was performed within 24–48 h of admission. Patients with anterior STEMI were treated with intravenous heparin for 24–48 h until a first echocardiography test was performed. Patients with reduced ejection fraction (EF) ≤40% had a repeat test before hospital discharge (days 5–7). Heparin was continued in case of significant left ventricular dysfunction (EF < 35%) or apical akinesis or dyskinesis, until a second test ruled out LVT.
Results
LVT was diagnosed before hospital discharge in 31/2071 patients (1.5%), 28 of whom (90%) had anterior STEMI. Only 2/31 patients with LVT (6.5%) developed embolic events before discharge and 1/31 (3.2%) had an episode of upper gastrointestinal bleeding that required blood transfusion. There was no significant difference between the two groups regarding in-hospital STEMI-related complications, short- and long-term mortality. All LVTs resolved in subsequent echocardiograms within 6 months of discharge.
Conclusions
We report a low incidence of early LVT following STEMI. Further studies are needed to assess the efficacy and safety of a limited in-hospital anticoagulation protocol in STEMI patients with reduced EF.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Before the advent of primary percutaneous coronary intervention (PCI) for the treatment of ST-elevation myocardial infarction (STEMI), left ventricular thrombus (LVT) was a serious complication reported in up to 46% of patients following first anterior wall STEMI [1, 2]. The majority of LVT were found prior to hospital discharge and most disappeared within 6 months of anticoagulation therapy [3]. Major consequences of LVT included a high incidence (20%) of systemic embolism before discharge and conferred poor prognosis among patients with early LVT formation (detected within 72 h of hospital admission) [4–6]. Since the introduction of primary PCI, studies have reported a declining incidence of LVT after STEMI ranging from 2 to 4% in large studies. The steady decline in the incidence of LVT thrombus has been postulated to be related to improvements in PCI practice over the years [7–10]. While the incidence and outcomes of LVT in the pre-PCI era have been well studied, there are limited data on the possible implications of early LVT in the last decade of PCI practice. We aimed to investigate the incidence, natural history and outcomes of early (pre-discharge) LVT in a large cohort of STEMI patients undergoing primary PCI.
Methods
We performed a retrospective, single-center observational study at the Tel-Aviv Sourasky Medical Center, a tertiary referral hospital with a 24/7 PCI service [11–13]. Included were all 2219 consecutive patients admitted to the cardiac intensive care unit (CICU) with the diagnosis of STEMI between October 2007 and April 2016. We excluded patients who were discharged with a diagnosis other than STEMI (e.g., stress cardiomyopathy, myocarditis, n = 37), patients treated conservatively (n = 79), and patients who died before a first echocardiographic test was performed (n = 32). The final study population included 2071 patients, all of whom underwent primary PCI and had at least one echocardiographic study during their hospital stay. Patients’ baseline demographics, cardiovascular history, clinical risk factors, treatment, characteristics and laboratory results were all retrieved from the hospital electronic medical records.
The criteria for the diagnosis of STEMI were consistent with the 2012 European Society of Cardiology and 2013 AHA/ACC STEMI guidelines based on serial elevations of cardiac biomarkers, history of typical chest pain and electrocardiographic features. The electrocardiographic criterion for the diagnosis of ST-segment elevation was an ST-segment elevation ≥1 mm in >2 adjacent leads [14, 15].
All patients received a heparin bolus (4000 U) and dual antiplatelet therapy consisting of aspirin (a loading dose of 300 mg followed by 100 mg/day) and either clopidogrel (a loading dose of 300 mg followed by 75 mg/day), prasugrel (a loading dose of 60 mg followed by 10 mg/day) or ticagrelor (a loading dose of 180 mg followed by 90 mg/day). Patients who arrived at hospital by ambulance were administered aspirin and heparin while being transported. All patients were treated with heparin boluses during angioplasty, aiming to obtain an activated clotting time of 250–300 s in those treated with glycoprotein IIb/IIIa antagonists and an activated clotting time >300 s in the others. Glycoprotein IIb/IIIa antagonist was administered during PCI at the discretion of the senior operator.
Post-PCI anticoagulation was administered according to our local policy: Unless contraindicated (recent history of major bleeding, recent ischemic stroke, history of hemorrhagic stroke, active bleeding or other condition deemed very high risk for bleeding by the treating physician), all patients with anterior STEMI were treated with full dose intravenous heparin for 24–48 h until a first echocardiography test was performed. Heparin was continued in case of significant left ventricular dysfunction (EF < 35%) or apical akinesis or dyskinesis until a second echocardiography test ruled out LVT. Otherwise, anticoagulation treatment was deferred unless the echocardiographic examination demonstrated an LVT. Patients having non-anterior STEMI did not receive anticoagulation unless warranted for another indication (e.g., atrial fibrillation).
All patients underwent screening echocardiography within 24–48 h of admission. Repeat echocardiography was performed before discharge (within 4–7 days) in patients with STEMI who had an ejection fraction of 40% or less on their first echocardiography.
Echocardiography was performed using Philips iE33 (Philips Medical Systems, Andover, Massachusetts) and GE Vivid 3 (GE Healthcare, Waukesha, Wisconsin) models equipped with S5-1 transducers. Parasternal long- and short-axis, apical and 2–4 chambers views were obtained using standard transducer positions.
The 16-segment model was used for scoring the severity of segmental wall motion abnormalities, according to the American Society of Echocardiology [16]. LV wall motion was graded on a scale ranging from 1 to 5 (1 = normal motion, 2 = hypokinesia, 3 = akinesia, 4 = dyskinesia, 5 = signs of a left ventricular aneurysm). An LVT was defined as an echo-dense mass adjacent to an abnormally contracting myocardial segment. It had to be distinguishable from the underlying myocardium, have a clear thrombus-blood interface, and be visible in at least two transducer positions. If the diagnosis of LVT was suspected or could not be ruled out, serial echocardiographic tests were mandated to determine the final diagnosis.
Following a diagnosis of LVT all patients received triple anticoagulation therapy according to current guidelines which included aspirin, clopidogrel and warfarin (with target INR of 2–2.5) for at least 3 months [14, 15]. Warfarin was discontinued if follow-up echocardiography did not demonstrate LVT.
Analysis was performed retrospectively using the institution’s electronic records and database. Patients were followed for 30-day mortality, long-term mortality, hospital readmissions, and follow-up echocardiography. The study was approved by the institutional review board. Long-term mortality for all patients was assessed over a mean period of 1311 ± 906 days of follow-up (range 1–3133). Patients who had LVT were also assessed for hospital readmissions due to heart failure, myocardial infarction, stent thrombosis, stroke and bleeding episodes using electronic medical records for a time of 3 months following hospital discharge. In addition, patients with LVT were assessed for follow-up echocardiography performed within 3 and 6 months following hospital discharge.
Continuous variables are presented as mean ± standard deviation. Categorical variables were reported as counts and percentages. Comparisons between groups were made using the Whitney–Mann test or t test for continuous variables and Chi square analysis for categorical variables. Statistical significance was assumed at p value <0.05.
Results
A total of 2071 consecutive patients were included in the analysis. Echocardiography was performed in all patients within 24–48 h (mean 1 ± 0.4 days). A second echocardiographic study was performed in 614/2017 patients (29.6%) within 5 ± 1.2 days following admission. Extended heparin regimen was given to 213 patients. In 197/213 patients (92%), the heparin could be stopped after the second echocardiography.
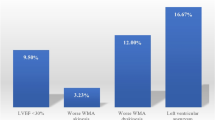
LVT was diagnosed before hospital discharge in 31/2071 patients (1.5%), 28 of whom (90%) had an anterior STEMI. Upon hospital admission, 11/31 patients with LVT (35%) were on aspirin, and 3/31 (9.7%) were on dual antiplatelet therapy (DAPT). In 15/31 patients (48.4%), an LVT was present on the first echocardiographic test, whereas in 16 patients (51.6%) LVT was only demonstrated on the second echocardiographic study. Patients who developed LVT after STEMI had lower left ventricular ejection fraction, higher peak CPK level, longer time from symptom onset until arrival to the emergency department, and prolonged time to reperfusion (Table 1).
In-hospital outcomes
There was no difference between the two groups in 30-day mortality, and in-hospital STEMI-related complications including arrhythmias, heart failure, major bleeding and need for mechanical ventilation (Table 2). Only 2/31 patients with early LVT (6.5%) developed embolic events before discharge and 1/31 patient (3.2%) had an episode of upper gastrointestinal bleeding that necessitated blood transfusion.
Long-term outcomes
Follow-up data were available for 25/31 patients with early LVT within 3 months of discharge (2 patients died, 2 were visitors who returned to their country of origin and 2 patients were lost to follow-up). Follow-up echocardiograms were available for all 25 patients within 3 months of discharge. The mean time for echocardiography was 55 ± 26 days (range 30–90). In 4/25 patients (16%), an LVT was still observed. All remaining LVTs resolved in subsequent echocardiograms within 6 months of discharge. Five patients were readmitted to the hospital within 3 months of follow-up (1 due to documented ventricular tachycardia, 1 due to syncope and the rest due to non-specific chest symptoms). None of the readmissions was due to heart failure, bleeding or stroke.
Over a mean period of 1311 ± 906 days of follow-up (range 1–3133), no significant difference was found in mortality between patients with LVT and without LVT (12.9 vs. 6.5%, p = 0.34) (Fig. 1).
Discussion
The current study provides new data and insights concerning the incidence and outcomes of LVT among STEMI patients in the contemporary era of primary PCI practice. We demonstrated that early LVT formation following STEMI is a rare complication. We report an incidence of 1.5% among a large cohort of consecutive patients treated in our hospital over the last decade. The low incidence of early LVT thrombus following STEMI reported in our study is possibly related to improved PCI practice over the last decades but could also be ascribed to our anticoagulation policy. In our cohort, there was a large numerical difference in long-term survival in patients with and without LVT; however, this difference did not reach statistical significance. Given the low number of events, the lack of statistical significance should be interpreted with caution. The same is true for the other outcome measures reported in our study.
The pathogenesis of LVT formation is attributed to the combination of blood stasis, endothelial injury and hypercoagulability, collectively referred to as Virchow’s triad. Blood stasis is the result of myocardial stunning and regional wall akinesia/dyskinesia. Ischemia causes endothelial injury, triggers inflammatory changes and induces a hypercoagulable state [17, 18].
Anticoagulation has been shown to reduce the incidence of LVT after myocardial infarction [19–22], although some studies have failed to show that this reduction in LVT incidence is associated with a decrease in stroke events following myocardial infarction [20, 23]. Since the vast majority of LVTs following STEMI are formed within 2 weeks after the index event [24], when the components of Virchow’s triad are highest, it is reasonable to consider a short-term anticoagulation protocol for the prevention of LVT formation.
Currently, the 2013 American College of Cardiology (ACC)/American Heart Association (AHA) STEMI guidelines recommend oral anticoagulation with warfarin in addition to dual antiplatelet therapy in patients with LVT (class 2a recommendation) and for the prevention of LVT formation in patients with anterior apical akinesis or dyskinesis (class 2b recommendation) [14]. However, the routine use of anticoagulation following anterior STEMI with risk factors for LVT is controversial. A recent non-randomized study reported a high rate of in-hospital major bleeding in patients treated with warfarin for the prevention of LVT after STEMI and a higher rate of death, stroke and major bleeding at 180 days [25].
Our policy is to administer a limited (5–7 days) in-hospital anticoagulation protocol in selected patients (EF ≤ 35% or those with apical akinesis or dyskinesis) who do not seem be at a high-risk for bleeding until a second echocardiography test ruled out LVT. We have previously studied the safety of this protocol in 296 patients with anterior STEMI in our department. Continuous anticoagulation therapy for 5 days was associated with a low incidence of LVT formation without a significant increase in the risk of bleeding [26]. In our current cohort, the risk for major bleeding did not differ significantly between the two groups (3.2 vs. 4.6%, p = 0.71). Further prospective studies are needed to weigh the risks and benefits of such a limited short-term anticoagulation protocol.
Of note is that half of the LVTs in our study were not visualized on the first echocardiography performed within 24–48 h. This finding emphasizes the need for a repeat echocardiography study before discharge in patients at high risk for LVT formation following STEMI. Our follow-up data also support the available body of evidence that most LVTs after STEMI resolve within 3 months of anticoagulation therapy, probably emphasizing that anticoagulation may be withdrawn beyond that period.
Study limitations
First, this is a retrospective non-randomized study which may introduce detection and treatment bias. Second, our relatively small sample size of positive cases could limit comprehensive multivariate analysis concerning LVTs. Moreover, the low number of in-hospital events and absence of data on long-term outcomes (other than mortality) in patients without LVT dictate that outcome-related conclusions derived from lack of statistical significance be interpreted with caution. Third, a substantial number of LVT were detected only by the second echocardiography. Since this second echocardiography was missing in nearly 70% of patients, the true incidence of LVT might have been underestimated. In addition, we only report early LVTs detected during hospital stay while late LVT formation has been demonstrated in echocardiographic studies performed 1–3 months after discharge [27, 28]. Forth, non-contrast echocardiography has a low sensitivity and specificity. When compared to delayed enhancement cardiac magnetic resonance (CMR), non-contrast echocardiography has a 35% sensitivity for the diagnosis of LVT while contrast echo significantly improved the sensitivity for LVT diagnosis to 64% [29]. It is possible that some LVTs were missed in our cohort due to the use of non-contrast echocardiography. To enhance the detection power and reduce the false results associated with the use of non-contrast echocardiography, we used multiple tomographic planes, frequent adjustment of gain, depth focus, color Doppler with low scale as a contrast substitute and a high transducer frequency. Delayed enhancement CMR appears to be superior than other modalities for the detection of LVT thrombus [30]; however, the clinical significance of small LVTs detected only by CMR has not been clarified. Recent CMR studies have shown that LVTs can be present early post-MI and self-resolve thereafter [31]. Further studies are needed to elucidate the clinical significance of small LVTs detected only by CMR. Finally, information regarding long terms outcomes other than mortality for patients not having LVT (recurrent infarction, need for repeat revascularization, heart failure and stroke) was not available. Also, no information was present regarding administration of IIb/IIIa receptor blockers during primary PCI and the type of antiplatelet used throughout hospitalization and discharge prohibiting the possible evaluation of their long-term utilization [32, 33].
Conclusions
We demonstrated that the incidence of early LVT detected on non-contrast echocardiography is 1.5% in a large contemporary population.
Further prospective randomized studies are needed to weigh the risks and benefits of short-term anticoagulation after STEMI and to determine whether it improves outcomes.
References
Lamas GA, Vaughan DE, Pfeffer MA (1988) Left ventricular thrombus formation after first anterior wall acute myocardial infarction. Am J Cardiol 62(1):31–35
Asinger RW, Mikell FL, Elsperger J, Hodges M (1981) Incidence of left-ventricular thrombosis after acute transmural myocardial infarction. Serial evaluation by two-dimensional echocardiography. N Engl J Med 305(6):297–302. doi:10.1056/NEJM198108063050601
Keren A, Goldberg S, Gottlieb S, Klein J, Schuger C, Medina A, Tzivoni D, Stern S (1990) Natural history of left ventricular thrombi: their appearance and resolution in the posthospitalization period of acute myocardial infarction. J Am Coll Cardiol 15(4):790–800
Kupper AJ, Verheugt FW, Peels CH, Galema TW, Roos JP (1989) Left ventricular thrombus incidence and behavior studied by serial two-dimensional echocardiography in acute anterior myocardial infarction: left ventricular wall motion, systemic embolism and oral anticoagulation. J Am Coll Cardiol 13(7):1514–1520
Crawford TC, Smith WT, Velazquez EJ, Taylor SM, Jollis JG, Kisslo J (2004) Prognostic usefulness of left ventricular thrombus by echocardiography in dilated cardiomyopathy in predicting stroke, transient ischemic attack, and death. Am J Cardiol 93(4):500–503. doi:10.1016/j.amjcard.2003.10.056
Weinsaft JW, Kim HW, Shah DJ, Klem I, Crowley AL, Brosnan R, James OG, Patel MR, Heitner J, Parker M, Velazquez EJ, Steenbergen C, Judd RM, Kim RJ (2008) Detection of left ventricular thrombus by delayed-enhancement cardiovascular magnetic resonance prevalence and markers in patients with systolic dysfunction. J Am Coll Cardiol 52(2):148–157. doi:10.1016/j.jacc.2008.03.041
Shacham Y, Leshem-Rubinow E, Ben Assa E, Rogowski O, Topilsky Y, Roth A, Steinvil A (2013) Frequency and correlates of early left ventricular thrombus formation following anterior wall acute myocardial infarction treated with primary percutaneous coronary intervention. Am J Cardiol 111(5):667–670. doi:10.1016/j.amjcard.2012.11.016
Gianstefani S, Douiri A, Delithanasis I, Rogers T, Sen A, Kalra S, Charangwa L, Reiken J, Monaghan M, MacCarthy P (2014) Incidence and predictors of early left ventricular thrombus after ST-elevation myocardial infarction in the contemporary era of primary percutaneous coronary intervention. Am J Cardiol 113(7):1111–1116. doi:10.1016/j.amjcard.2013.12.015
Robinson AA, Jain A, Gentry M, McNamara RL (2016) Left ventricular thrombi after STEMI in the primary PCI era: a systematic review and meta-analysis. Int J Cardiol 221:554–559. doi:10.1016/j.ijcard.2016.07.069
Nikolsky E, Mehran R, Dangas GD, Yu J, Parise H, Xu K, Pocock SJ, Stone GW (2012) Outcomes of patients treated with triple antithrombotic therapy after primary percutaneous coronary intervention for ST-elevation myocardial infarction (from the Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction [HORIZONS-AMI] trial). Am J Cardiol 109(6):831–838. doi:10.1016/j.amjcard.2011.10.046
Flint N, Kaufman N, Gal-Oz A, Margolis G, Topilsky Y, Keren G, Shacham Y (2017) Echocardiographic correlates of left ventricular filling pressures and acute cardio-renal syndrome in ST segment elevation myocardial infarction patients. Clin Res Cardiol 106(2):120–126. doi:10.1007/s00392-016-1031-8
Shacham Y, Leshem-Rubinow E, Ben-Assa E, Roth A, Steinvil A (2014) Lower admission hemoglobin levels are associated with longer symptom duration in acute ST-elevation myocardial infarction. Clin Cardiol 37(2):73–77. doi:10.1002/clc.22215
Arbel Y, Shacham Y, Finkelstein A, Halkin A, Milwidsky A, Berliner S, Ziv-Baran T, Revivo M, Herz I, Keren G, Banai S (2014) Red blood cell distribution width (RDW) and long-term survival in patients with ST elevation myocardial infarction. Thromb Res 134(5):976–979. doi:10.1016/j.thromres.2014.08.016
American College of Emergency P, Society for Cardiovascular A, Interventions, O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW (2013) 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 61(4):e78–e140. doi:10.1016/j.jacc.2012.11.019
Task Force on the management of STseamiotESoC, Steg PG, James SK, Atar D, Badano LP, Blomstrom-Lundqvist C, Borger MA, Di Mario C, Dickstein K, Ducrocq G, Fernandez-Aviles F, Gershlick AH, Giannuzzi P, Halvorsen S, Huber K, Juni P, Kastrati A, Knuuti J, Lenzen MJ, Mahaffey KW, Valgimigli M, van’t Hof A, Widimsky P, Zahger D (2012) ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 33(20):2569–2619. doi:10.1093/eurheartj/ehs215
Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, Gutgesell H, Reichek N, Sahn D, Schnittger I et al (1989) Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 2(5):358–367
Delewi R, Zijlstra F, Piek JJ (2012) Left ventricular thrombus formation after acute myocardial infarction. Heart 98(23):1743–1749. doi:10.1136/heartjnl-2012-301962
Shacham Y, Leshem-Rubinow E, Ben Assa E, Rogowski O, Topilsky Y, Roth A, Steinvil A (2013) Comparison of C-reactive protein and fibrinogen levels in patients having anterior wall ST-Segment elevation myocardial infarction with versus without left ventricular thrombus (from a primary percutaneous coronary intervention cohort). Am J Cardiol 112(1):57–60. doi:10.1016/j.amjcard.2013.02.052
Turpie AG, Robinson JG, Doyle DJ, Mulji AS, Mishkel GJ, Sealey BJ, Cairns JA, Skingley L, Hirsh J, Gent M (1989) Comparison of high-dose with low-dose subcutaneous heparin to prevent left ventricular mural thrombosis in patients with acute transmural anterior myocardial infarction. N Engl J Med 320(6):352–357. doi:10.1056/NEJM198902093200604
Kontny F, Dale J, Abildgaard U, Pedersen TR (1997) Randomized trial of low molecular weight heparin (dalteparin) in prevention of left ventricular thrombus formation and arterial embolism after acute anterior myocardial infarction: the Fragmin in Acute Myocardial Infarction (FRAMI) study. J Am Coll Cardiol 30(4):962–969
Smith P, Arnesen H, Holme I (1990) The effect of warfarin on mortality and reinfarction after myocardial infarction. N Engl J Med 323(3):147–152. doi:10.1056/NEJM199007193230302
Vaitkus PT, Barnathan ES (1993) Embolic potential, prevention and management of mural thrombus complicating anterior myocardial infarction: a meta-analysis. J Am Coll Cardiol 22(4):1004–1009
Udell JA, Wang JT, Gladstone DJ, Tu JV (2010) Anticoagulation after anterior myocardial infarction and the risk of stroke. PLoS One 5(8):e12150. doi:10.1371/journal.pone.0012150
Visser CA, Kan G, Lie KI, Durrer D (1983) Left ventricular thrombus following acute myocardial infarction: a prospective serial echocardiographic study of 96 patients. Eur Heart J 4(5):333–337
Le May MR, Acharya S, Wells GA, Burwash I, Chong AY, So DY, Glover CA, Froeschl MP, Hibbert B, Marquis JF, Dick A, Blondeau M, Bernick J, Labinaz M (2015) Prophylactic warfarin therapy after primary percutaneous coronary intervention for anterior ST-segment elevation myocardial infarction. JACC Cardiovasc Interv 8(1):155–162. doi:10.1016/j.jcin.2014.07.018
Shacham Y, Birati EY, Rogovski O, Cogan Y, Keren G, Roth A (2012) Left ventricular thrombus formation and bleeding complications during continuous in-hospital anticoagulation for acute anterior myocardial infarction. Isr Med Assoc J 14(12):742–746
Solheim S, Seljeflot I, Lunde K, Bjornerheim R, Aakhus S, Forfang K, Arnesen H (2010) Frequency of left ventricular thrombus in patients with anterior wall acute myocardial infarction treated with percutaneous coronary intervention and dual antiplatelet therapy. Am J Cardiol 106(9):1197–1200. doi:10.1016/j.amjcard.2010.06.043
Osherov AB, Borovik-Raz M, Aronson D, Agmon Y, Kapeliovich M, Kerner A, Grenadier E, Hammerman H, Nikolsky E, Roguin A (2009) Incidence of early left ventricular thrombus after acute anterior wall myocardial infarction in the primary coronary intervention era. Am Heart J 157(6):1074–1080. doi:10.1016/j.ahj.2009.03.020
Weinsaft JW, Kim J, Medicherla CB, Ma CL, Codella NC, Kukar N, Alaref S, Kim RJ, Devereux RB (2016) Echocardiographic algorithm for post-myocardial infarction LV thrombus: a gatekeeper for thrombus evaluation by delayed enhancement CMR. JACC Cardiovasc Imaging 9(5):505–515. doi:10.1016/j.jcmg.2015.06.017
Weinsaft JW, Kim HW, Crowley AL, Klem I, Shenoy C, Van Assche L, Brosnan R, Shah DJ, Velazquez EJ, Parker M, Judd RM, Kim RJ (2011) LV thrombus detection by routine echocardiography: insights into performance characteristics using delayed enhancement CMR. JACC Cardiovasc Imaging 4(7):702–712. doi:10.1016/j.jcmg.2011.03.017
Delewi R, Nijveldt R, Hirsch A, Marcu CB, Robbers L, Hassell ME, de Bruin RH, Vleugels J, van der Laan AM, Bouma BJ, Tio RA, Tijssen JG, van Rossum AC, Zijlstra F, Piek JJ (2012) Left ventricular thrombus formation after acute myocardial infarction as assessed by cardiovascular magnetic resonance imaging. Eur J Radiol 81(12):3900–3904. doi:10.1016/j.ejrad.2012.06.029
Lee SY, Hong MK, Shin DH, Kim JS, Kim BK, Ko YG, Choi D, Jang Y, Kim HS, Valgimigli M, Palmerini T, Stone GW (2017) Clinical outcomes of dual antiplatelet therapy after implantation of drug-eluting stents in patients with different cardiovascular risk factors. Clin Res Cardiol 106(3):165–173. doi:10.1007/s00392-016-1035-4
Cassese S, Byrne RA, Ndrepepa G, Schunkert H, Fusaro M, Kastrati A (2015) Prolonged dual antiplatelet therapy after drug-eluting stenting: meta-analysis of randomized trials. Clin Res Cardiol 104(10):887–901. doi:10.1007/s00392-015-0860-1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Khoury, S., Carmon, S., Margolis, G. et al. Incidence and outcomes of early left ventricular thrombus following ST-elevation myocardial infarction treated with primary percutaneous coronary intervention. Clin Res Cardiol 106, 695–701 (2017). https://doi.org/10.1007/s00392-017-1111-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-017-1111-4