Abstract
Several recent studies suggested that the door-to-balloon time (DTBT) for patients with ST-segment elevation myocardial infarction (STEMI) should be as short as possible, despite the existing guideline for STEMI. This study aimed to evaluate the clinical outcomes of the STEMI patient cohort having the highest proportion of patients treated with a DTBT of ≤ 30 min ever reported. We evaluated 527 consecutive patients with STEMI who underwent percutaneous coronary intervention between 2007 and 2015. The mean age was 68.0 ± 12.7 years, and the mean DTBT was 44.4 ± 33.1 min. The patients were classified into four groups according to the DTBT, and the relationship between the DTBT and clinical outcome was investigated. DTBTs were ≤ 30 min in 146 patients (27.7%), 31–60 min in 297 patients (56.4%), 61–90 min in 60 patients (11.4%), and > 90 min in 24 patients (4.6%). In-hospital mortality rates were 0.7, 5.0, 11.7, and 12.5% for DTBTs of ≤ 30, 31–60, 61–90, and > 90 min, respectively. In multivariate analysis, a DTBT ≤ 30 min (odds ratio [OR] 0.11, 95% confidence interval [CI] 0.01–0.91, p = 0.041), shock on arrival (OR 2.74, 95% CI 1.02–7.37, p = 0.046), and blood transfusion (OR 49.60, 95% CI 13.90–177.00, p < 0.001) were the independent predictors of in-hospital mortality. Patients with STEMI treated with a DTBT ≤ 30 min showed significantly better clinical outcomes than those treated with a DTBT > 30 min.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The door-to-balloon time (DTBT) is predictive of in-hospital mortality in patients with ST-segment elevation myocardial infarction (STEMI). Previous studies reported that patients with a DTBT > 90 min have a significant increase in mortality compared with those with a DTBT ≤ 90 min [1,2,3]. Thus, recent guidelines for STEMI recommended that recanalization should be accomplished within 90 min [4, 5], and currently, higher proportions of patients with STEMI are treated according to the guidelines [6, 7]. Consequently, DTBT reduction to ≤ 90 min has contributed to better clinical outcomes. However, the effect of further reduction in the DTBT within the time range that meets the guidelines has presented conflicting results [7,8,9]. These conflicting results have been attributed to different factors, such as change in the indication for primary percutaneous coronary intervention (PCI) during the course of the study period, heterogeneity of PCI strategies, and performance in individual PCI-capable hospitals, which are unavoidable in a large cohort study [8]. Furthermore, these studies have been conducted in large cohorts with a relatively small proportion of patients treated with a shorter DTBT, i.e., ≤ 30 min (3.8%) [9].
In this study, we sought to evaluate the effect of a shorter DTBT on clinical outcomes in a cohort with a larger proportion of STEMI patients with a DTBT ≤ 30 min in a single center with a homogeneous PCI procedure.
Methods
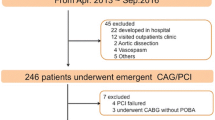
This was a single-center retrospective study of 527 consecutive patients with STEMI who underwent primary PCI between 2007 and 2015. Patients with cardiopulmonary arrest on arrival (40 patients) and onset-to-door time of ≥ 24 h (33 patients) during the study period were excluded. The diagnosis of STEMI was based on the European Society of Cardiology/American College of Cardiology Foundation/American Heart Association (AHA)/World Heart Federation’s universal definition of myocardial infarction, i.e., myocardial enzyme elevation and electrocardiogram showing ST-segment elevation in at least two contiguous leads or a new left bundle branch block [10]. Reperfusion was achieved at the time of the first balloon inflation or the first manual thrombus aspiration, if performed. The follow-up period for acute results was set at 30 days after admission or until hospital discharge, whichever came later. The patients were classified into four groups based on the DTBT, and we investigated the relationship between the DTBT and in-hospital mortality. We also studied clinical indices, including patient, lesion, and procedural characteristics, such as shock on arrival, blood transfusion, onset-to-balloon time, intra-aortic balloon pump (IABP) use, and renal dysfunction (estimated glomerular filtration rate < 30 ml/min/1.73 m2 [11]). The findings of Thrombolysis in Myocardial Infarction (TIMI) flow before and after PCI and final blush grade were also investigated.
Statistical analyses
We first determined the mean, median, and distribution of DTBTs. Differences in patients’ demographic and clinical characteristics were compared across the four DTBT groups (0–30, 31–60, 61–90, and > 90 min). The Cochran–Armitage test and Jonckheere–Terpstra test were used to examine the trend in the mortality rate and other clinical indices. Univariable analyses for in-hospital mortality were performed using the χ2 test. If the χ2 test was not applicable, the Fisher exact test and Student t test were used to analyze qualitative and normally distributed quantitative variables, respectively. Non-parametric values were compared with the Wilcoxon rank-sum test. Time intervals and peak creatine phosphokinase (CPK) levels showed a skewed distribution and were compared after logarithmic transformation. A multivariate logistic regression analysis was conducted for the following three factors: a DTBT ≤ 30 min, shock on arrival, and blood transfusion during hospitalization. A two-tailed p value < 0.05 was considered statistically significant. These statistical analyses were conducted using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Sample characteristics
The mean DTBT and number of patients each year during the study period are described in Fig. 1. Fifty-one patients (9.7%) had a history of myocardial infarction (MI), and 72 patients (13.7%) presented with shock on arrival. IABP support was performed in 99 patients (18.8%), and extracorporeal membrane oxygenation (ECMO) was performed in 14 patients (2.7%). The mean DTBT was 44.4 ± 33.1 min, 30-day mortality rate was 3.0%, and in-hospital mortality rate was 4.9%.
DTBT and clinical indices
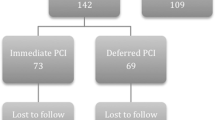
DTBTs were 0–30 min in 146 patients (27.7%), 31–60 min in 297 patients (56.4%), 61–90 min in 60 patients (11.4%), and > 90 min in 24 patients (4.6%). Patients with diabetes, renal dysfunction, IABP use, and blood transfusion were more frequently observed in the groups with a longer DTBT than in those with a shorter DTBT (Table 1). A higher proportion of patients with TIMI 3 flow and blush grade 3 after PCI was observed with a shorter DTBT than with a longer DTBT. Peak CPK levels were 2218 ± 2126, 2578 ± 2241, 2997 ± 2857, and 1273 ± 1138 IU/L for DTBTs ≤ 30, 31–60, 61–90, and > 90 min, respectively (p = 0.006). In cases, where the DTBT was within 90 min, the myocardial enzyme level was lower in patients with a shorter DTBT than in those with a longer DTBT (Table 2). Even though a DTBT ≤ 90 min was achieved in 95.4% of cases, a much shorter DTBT was associated with lower in-hospital mortality. In-hospital mortality rates were 0.7, 5.0, 11.7, and 12.5% for DTBTs ≤ 30, 31–60, 61–90, and > 90 min, respectively. The trend analysis showed that the longer DTBT was associated with higher in-hospital mortality (p ≤ 0.001) (Fig. 2).
Onset-to-balloon time and in-hospital mortality
We also categorized the patients according to the onset-to-balloon time (OTBT) and compared the mortality rates among the groups. We excluded eight patients owing to the absence of documented onset time data. The in-hospital mortality rates were 3.1% (n = 6), 6.5% (n = 11), 1.6% (n = 1), and 8.9% (n = 8) for OTBTs ≤ 120 (n = 196), 121–240 (n = 170), 241–360 (n = 63), and > 360 min (n = 90), respectively (p for trend = 0.982) (Table 3).
Clinical features of hospital survivors and non-survivors
To determine the clinical features of hospital survivors (n = 501) and non-survivors (n = 26), clinical and procedural characteristics between the two groups were compared. The mean length of hospital stay was 20.8 ± 21.0 days. Among the 26 deceased patients, 10 patients died after 30 days during their primary admission period. Older patients (p < 0.001), female sex (p < 0.001), a DTBT > 30 min (p < 0.001), higher peak CPK level (p = 0.039), lower left ventricle ejection fraction (p < 0.001), history of MI (p = 0.008), anemia (p < 0.001), renal dysfunction (p < 0.001), shock on arrival (p < 0.001), blood transfusion (p < 0.001), IABP use (p < 0.001), and ECMO use (p = 0.003) were more frequently observed in the non-survivor group than in the survivor group in univariate analysis (Table 4). Poor myocardial perfusion according to TIMI flow and the blush grade after PCI was significantly more frequently observed in the non-survivor group than in the survivor group. Multivariate analysis revealed that a DTBT ≤ 30 min (odds ratio [OR] 0.11, 95% confidence interval [CI] 0.01–0.91, p = 0.041), shock on arrival (OR 2.74, 95% CI 1.02–7.37, p = 0.046), and blood transfusion (OR 49.60, 95% CI 13.90–177.00, p < 0.001) were independent predictors of in-hospital mortality (Table 5).
Discussion
In this study, we demonstrated that significant incremental improvement of in-hospital and 30-day mortality rate is associated with DTBT shortening among patients treated even within 90 min (p < 0.001 and p = 0.006, respectively). Furthermore, a DTBT within 30 min was proven to be an independent predictor of in-hospital mortality along with shock and blood transfusion. To the best of our knowledge, this is the first study conducted with the largest proportion (27.7%) of patients with earlier (≤ 30 min) revascularization among studies evaluating the prognosis of patients treated within the guideline-recommended DTBT (i.e., ≤ 90 min).
Since the American College of Cardiology/AHA guidelines for the management of acute MI established a DTBT of 90 min as the gold standard for primary PCI in 2004 [4], individual efforts in PCI-capable hospitals have been made to reduce the time to revascularization [12, 13]. In 2008, > 80% of patients who had undergone primary PCI for STEMI in the United States met the goal of a DTBT ≤ 90 min [6], although a significant number of patients were excluded in that registry. Furthermore, Rathore et al. [9] evaluated the effect of a shorter DTBT and suggested that DTBT reduction from 90 to 60 min and from 60 to 30 min was associated with lower mortality (0.8 and 0.5%, respectively). Moreover, the study concluded that the time to treatment should be as short as possible, even in centers currently providing primary PCI within 90 min. However, a study that analyzed the CathPCI Registry showed no improvement in mortality by shortening the DTBT. During the study period, the median DTBT was reduced from 83 min in 2005 to 67 min in 2009 (p < 0.001); nevertheless, unadjusted mortality or risk-adjusted mortality was not significant [7]. A further analysis on the same registry between 2005 and 2011 suggested that the discrepancy between a shorter DTBT and clinical outcome could be attributed to the growing and changing STEMI patient population from year to year, including the expanding use of PCI and the increased number of hospitals included in the study [8]. Thus, in a multicenter registry, potential heterogeneity in the chronology, institutional background, or operator experience and expertise may be problematic. Moreover, a deviated proportion of the mean DTBT among institutions might also affect findings; a hospital with a shorter mean DTBT is likely to provide a higher standard of care not only during PCI, but also during coronary care unit care or further treatment [9].
Furthermore, access site selection and intravascular ultrasonography (IVUS) use may affect the results. Although the sample size was relatively small in this single-center analysis, the PCI procedure was almost identical among patients. Transradial intervention was performed in 93.7% and IVUS in 90.5% of the patients, with mainly two registered interventional cardiologists. Hence, heterogeneity of the therapeutic procedure was minimal. In addition, this study’s patient cohort comprised a larger proportion of STEMI patients with a DTBT ≤ 30 min in a single center with a homogeneous PCI procedure.
Total ischemic time is another significant predictor of prognosis in STEMI [14, 15]. Thus, we also categorized the patients according to onset-to-balloon time (OTBT) and compared the mortality rates among the groups. We excluded eight patients owing to the absence of documented onset time data. The in-hospital mortality rates were 3.1% (n = 6), 6.5% (n = 11), 1.6% (n = 1), and 8.9% (n = 8) for OTBTs ≤ 120 (n = 196), 121–240 (n = 170), 241–360 (n = 63), and > 360 min (n = 90), respectively (p for trend = 0.982). The cause of this less significant correlation between OTBT and mortality in our study, although uncertain, can be explained as follows: (1) determination of the exact onset time is sometimes difficult, especially in elderly patients [16] and (2) onset-to-door time (OTDT) is affected by the onset time. Patients having an attack at night had a significantly shorter OTDT because they tend to directly visit PCI-capable hospitals by ambulance [17]. Those with a more serious condition (likely to have a poor prognosis) tended to arrive at the hospital earlier, whereas those with a less serious condition (likely to have a good prognosis) tended to have a longer OTDT, as they stop at a local practitioner’s office or non-PCI-capable hospitals before arriving at PCI-capable hospitals. Our analysis revealed that patients, whose OTDT was ≤ 60 min (n = 146) had a significantly higher proportion of shock on arrival than those with a longer OTDT (n = 373) (20.5 vs. 11.0%; p = 0.007).
In this study, the incidence of blood transfusion was as high as 13.9%. Japanese patients, particularly the elderly patients, have a relatively small build and are prone to anemia during and after primary PCI, even in the absence of major bleeding. Moreover, although the prevalence of transradial approach is high, the mean nadir hematocrit was 30.6 ± 5.5% in all cohorts, and the proportion of the patients with nadir hematocrit < 25% was 14.8%, which was almost equivalent to the incidence of transfusion.
Blood transfusion was the most contributing risk factor of in-hospital mortality in multivariate analysis of our study. In a recent study concerning blood transfusion in anemic patients with acute coronary syndrome, blood transfusion was associated with a significantly increased adjusted hazard ratio for 30-day death of 3.94 [18]. Such worse outcomes by blood transfusion are considered causally related to the inflammatory response, ischemia, vasoconstriction, hemodynamic compromise due to bleeding, and subsequent cessation of anti-platelet drugs that may became a cause for stent thrombosis [18]. Aside from such relationship between blood transfusion and worse clinical outcome, patients with STEMI who require blood transfusion have a significantly higher incidence of various risk-related factors including advanced age, female sex, hypertension, diabetes, prior stroke, prior congestive heart failure, and chronic renal insufficiency [18, 19].
This study has several limitations. First, this was a single-center retrospective study. Only 26 in-hospital deaths of the 527 patients were reported. Thus, the study’s ability to detect significant correlates of adverse events was limited. Second, other potential confounders that could affect the DTBT, such as cognitive faculty, frailty, and other factors related to the severity of the patient’s condition, were not investigated. Third, despite the aforementioned postulations, the cause of less correlation between OTDT with mortality remains uncertain, which warrants further investigation. Fourth, although a longer DTBT was associated with a higher mortality rate, the other markers, including enzyme leakage and ejection fraction, did not show a relevant trend. Fifth, although the PCI procedure and standard of care for the patients were considered identical because of the nature of the study (single center and limited operators), the DTBT per se ranged from 9 to 628 min. Such a wide distribution of the DTBT may partly reflect the deviation of the severity of the patients among the four groups. In fact, the group with a DTBT > 90 min had a higher proportion of the previous MI and coronary artery bypass graft. Although a longer DTBT was associated with higher mortality, a longer DTBT per se may reflect the patients’ characteristics responsible for a poor prognosis.
Conclusions
Although the guidelines recommended a DTBT ≤ 90 min in PCI for patients with STEMI, incremental improvement of the survival rate is associated with further reduction of the DTBT among patients treated within 90 min. Moreover, the effort to further shorten the DTBT contributed to lower in-hospital mortality in patients with STEMI, especially when the DTBT was ≤ 30 min.
References
Berger PB, Ellis SG, Holmes DR, Granger CB, Criger DA, Betriu A, et al. Relationship between delay in performing direct coronary angioplasty and early clinical outcome in patients with acute myocardial infarction: results from the global use of strategies to open occluded arteries in Acute Coronary Syndromes (GUSTO-IIb) trial. Circulation. 1999;100(1):14–20.
Cannon CP, Gibson CM, Lambrew CT, Shoultz DA, Levy D, French WJ, et al. Relationship of symptom-onset-to-balloon time and DTBT with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283(22):2941–7.
McNamara RL, Wang Y, Herrin J, Curtis JP, Bradley EH, Magid DJ, et al. Effect of DTBT on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006;47:2180–6.
American College of Emergency Physicians; Society for Cardiovascular Angiography and Interventions, O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):e78–140.
Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology (ESC), Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, Borger MA, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33(20):2569–619.
Krumholz HM, Herrin J, Miller LE, Drye EE, Ling SM, Han LF, et al. Improvements in door-to-balloon time in the United States, 2005 to 2010. Circulation. 2011;124(9):1038–45.
Menees DS, Peterson ED, Wang Y, Curtis JP, Messenger JC, Rumsfeld JS, et al. Door-to-balloon time and mortality among patients undergoing primary PCI. N Engl J Med. 2013;369(10):901–9.
Nallamothu BK, Normand SL, Wang Y, Hofer TP, Brush JE Jr, Messenger JC, et al. Relation between door-to-balloon times and mortality after primary percutaneous coronary intervention over time: a retrospective study. Lancet. 2015;385(9973):1114–22.
Rathore SS, Curtis JP, Chen J, Wang Y, Nallamothu BK, Epstein AJ, et al. Association of door-to-balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: national cohort study. BMJ. 2009;338:b1807.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. Circulation. 2012;126(16):2020–35.
Imai E, Horio M, Nitta K, Yamagata K, Iseki K, Hara S, et al. Estimation of glomerular filtration rate by the MDRD study equation modified for Japanese patients with chronic kidney disease. Clin Exp Nephrol. 2007;11(1):41–50.
Nguyen B, Fennessy M, Leya F, Nowak W, Ryan M, Freeberg S, et al. Comparison of primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction during and prior to availability of an in-house STEMI system: early experience and intermediate outcomes of the HARRT program for achieving routine D2B times < 60 minutes. Catheter Cardiovasc Interv. 2015;86(2):186–96.
Bradley EH, Nallamothu BK, Herrin J, Ting HH, Stern AF, Nembhard IM, et al. National efforts to improve door-to-balloon time results from the door-to-balloon alliance. J Am Coll Cardiol. 2009;54(25):2423–9.
Heitzler VN, Babić Z, Milicić D, Starcević B, Mirat J, Strozzi M, et al. Evaluation of importance of door-to-balloon time and total ischemic time in acute myocardial infarction with ST-elevation treated with primary percutaneous coronary intervention. Acta Clin Croat. 2012;51(3):387–95.
Solhpour A, Chang KW, Arain SA, Balan P, Loghin C, McCarthy JJ, et al. Ischemic time is a better predictor than door-to-balloon time for mortality and infarct size in ST-elevation myocardial infarction. Catheter Cardiovasc Interv. 2016;87(7):1194–200.
Davis LL. Determining time of symptom onset in patients with acute coronary syndromes: agreement between medical record and interview data. Dimens Crit Care Nurs. 2015;34(4):222–31.
Mizuguchi Y, Shibutani H, Hashimoto S, Yamada T, Taniguchi N, Nakajima S, et al. Onset-to-device time of patients who arrive at off-hours: importance of prehospital management and public awareness for patients with ST-segment elevation myocardial infarction. Cardiovasc Ther. 2016;34(6):475–81.
Rao SV, Jollis JG, Harrington RA, Granger CB, Newby LK, Armstrong PW, et al. Relationship of blood transfusion and clinical outcomes in patients with acute coronary syndromes. JAMA. 2004;292(13):1555–62.
Morrow DA, Antman EM, Charlesworth A, Cairns R, Murphy SA, de Lemos JA, et al. TIMI risk score for ST-elevation myocardial infarction: a convenient, bedside, clinical score for risk assessment at presentation: an intravenous nPA for treatment of infarcting myocardium early II trial substudy. Circulation. 2000;102(17):2031–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Yamada, T., Takahashi, A., Mizuguchi, Y. et al. Impact of shorter door-to-balloon time on prognosis of patients with STEMI—single-center analysis with a large proportion of the patients treated within 30 min. Cardiovasc Interv and Ther 34, 97–104 (2019). https://doi.org/10.1007/s12928-018-0521-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-018-0521-1