Abstract
Purpose
Our aim is to present our experience in the management of pediatric meningiomas in the largest referral center in Egypt for pediatric tumors focusing on variables including clinical picture, anatomic location, histopathology, treatment strategies, and outcome together with their possible correlation to prognosis.
Methods
We retrospectively reviewed the medical records of 39 pediatric patients who were treated for CNS meningiomas in Children’s Cancer Hospital—Egypt (CCHE-57357) 2007–2017.
Results
The prevalence of pediatric meningioma was 1.42%. Four cases had type 2 neurofibromatosis (NFII). The mean age was 8.19 years. The presence of NFII was associated with challenging multiple lesions, older age of presentation and poorer prognosis and functional outcome. Convexity was the commonest location. Gross total resection (GTR) was achieved in 28 cases, subtotal resection (STR) in 8 cases, and biopsy was decided in 3 patients. Histopathological examination revealed WHO grade I in 16 patients and higher grades in 23 patients (59%). The 5-year overall survival (OS) rate was 87.8% while the 5-years event-free survival (EFS) rate was 85.6%. Tumor location, histopathology, and clinical presentation were not statistically correlated to prognosis.
Conclusions
Pediatric CNS meningiomas are uncommon pediatric tumors but of an aggressive clinical and pathological behaviors as compared to adult meningiomas. The presence of NFII is associated with a poorer prognosis and functional outcomes. Although being challenging, the maximum and safe surgical excision should be exercised even in recurrent cases in order to achieve the best outcome. Adjuvant radiotherapy provides good tumor control for inoperable residual atypical or anaplastic meningiomas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In contrast to adult population, meningioma is one of the rare pediatric neurological tumors and its incidence in the first two decades did not exceed 3.7% of all neurological tumors in this age group in the recent literature [1,2,3], and they constituted 2.7–4.6% of all intracranial meningiomas [3]. NFII is a common association and usually associated with multiple meningiomas in multiple locations [4]. Also, exposure to radiation is an established risk factor for the development of meningiomas and many cases were reported [5]. Some cases were reported with genetic abnormalities or familial cases without genetic abnormalities [6, 7]. Our aim is to present our experience in CCHE-57357, the largest referral center in Egypt and the region for pediatric tumors, in the management of pediatric meningiomas focusing on the different clinical variables including the clinical picture, anatomic location, pathological characteristics, different treatment strategies, and outcome together with their possible relation to prognosis.
Patients and methods
The records of all patients below 18 years old who were diagnosed to have CNS meningioma and managed at children cancer hospital Egypt between 2007 and 2017 were reviewed. All the clinical symptoms and signs, radiological imaging, pathological features, surgical and adjuvant therapies, and follow-up data were systematically reviewed.
This study was approved by our hospital board review committee and the medical ethics committee; informed consents were obtained from patients’ relatives for any procedure or treatment and for publication of relevant data.
Meningioma patients were grouped as convexity group that included all lesions related to cerebral or cerebellar hemispheres and whether any sinus was involved or not; skull base group that included those lesions with dural attachment to skull base, sellar region, sphenoid ridge, or posterior fossa base either in the cerebellopontine angle or foramen magnum; optic nerve group; spinal canal group, and intraventricular group. For statistical feasibility and due to their small patients’ numbers, the three latest groups were furtherly grouped together as “others” when the survival statistics were carried on.
Early postoperative MRI was performed to assess the extent of resection. Histopathological assessment included immunohistochemical studies for all cases to confirm the diagnosis of meningioma. Serial follow-up MRI with contrast was performed for all patients every 3 months in the first 2 years then every 6 months thereafter.
Statistical analysis
Patients’ characteristics were reported in counts and percentages for descriptive data. Pearson’s Chi square and Fisher’s exact tests were used to compare between similar descriptions made of the (GTR) and (STR/biopsy) groups, where Fisher’s exact test was used when more than 25% of the variable cells had an expected count less than 5. Survival analysis as overall survival (OS) and event-free survival (EFS) were estimated using the Kaplan-Meier method. Time to event was calculated as the duration from time of diagnosis till time of recurrence, progression, or death from any cause. The log-rank test was applied to compare between event-free survivals (EFSs) among different prognostic variables where P < 0.05 was considered statistically significant. The statistical analysis was performed using the statistical package IBM-SPSS, version 22.
Results
Among the 2734 children who were treated in our hospital between 2007 and 2017 for brain tumors, 39 (1.42%) cases were found to have CNS meningiomas. Of these 39 patients, 21 were males and 18 were females. Fifteen patients were younger than 7 years and 24 patients were older than 7 years. The mean age at presentation was 8.19 years. Patient’s characteristics are described in Table 1.
Four patients had NFII (10.2%) all of which presented at age more than 11 years old with challenging multiple lesions and a clinical picture of mass effect.
Locations of the lesions were diverse (Table 2); 35 patients had a lesion in a single location where four patients with NFII had multiple meningiomas in various locations. Tumors had convexity, skull base, optic nerve, ventricular, and spinal locations in 19, 15, 2, 5, and 6 patients, respectively.
The most common presentation was seizures in 17 patients (43.5%) and increased intracranial pressure in 17 patients (43.5%). Other clinical presentations are listed in Table 3.
GTR was achieved in 28 cases, where STR was done in 8 cases. Biopsy was decided in 3 patients; the first one was a 2-year-old kid who had a diffuse skull base lesion extending from the parasellar region to the posterior fossa and the biopsy revealed anaplastic meningioma, the second one had a large heavily calcified parasellar lesion. Intraoperatively, it was adherent to all of the surrounding blood vessels and attempts at excision were associated with massive bleeding; a third patient had an optic nerve lesion which was biopsied and revealed meningioma but the child’s parents refused further surgery. Details of surgical interference are showed in Tables 4 and 5.
Histopathological examination revealed meningioma WHO GI in 16 patients, atypical meningioma WHO GII in 11 patients and anaplastic meningioma WHO GIII in 12 patients. Four patients had NFII, two cases were WHO GI, one case was WHO GIII and in the fourth NFII patient who was operated upon by excision of optic nerve meningioma WHO GI, a progression of dorsal meningioma occurred and needed surgery and it turned to be atypical meningioma then the patient experienced another progression in a temporal meningioma and after its excision, the pathology revealed anaplastic meningioma WHO GIII. Mixed histological patterns were found in 12 specimens while presence of foci of higher WHO grade in the same patient was detected in five cases.
Radiotherapy was given for 19 patients all of which had atypical or anaplastic meningiomas; in five of them, STR was achieved while GTR was reached in the other 14 patients.
According to the performance measured for the patients in their last visit, 30 patients had good functional outcome, 21 had their WHO score (0), and nine patients had score of (1). Completely disabled patients according to this score were three patients. Kyphosis deformity was detected in two, among the spinal meningioma group, one of them was significant but stabilized with physiotherapy, brace, and walking aids.
One of the NFII patients with multiple meningiomata in various locations became completely blind and another NFII patient remained completely paraplegic. One case showed recurrence in the same site of the tumor after 4 months from complete excision and radiotherapy. Five cases died during the follow-up period; four patients died due to progression of the lesions and all of them were atypical or anaplastic meningiomas, and the fifth died from progression of a recurrent lesion. The mean follow-up period was 38.5 months.
The 5-year overall survival rate was 87.8% while the 5-year event-free survival rate was 85.6%. The EFS rates for different prognostic variables were also calculated. These variables included the age and gender of the child, the NFII status, the location of the lesion, the WHO grade, and the extent of surgical excision. The different variables assessed are listed in Table 6. None of the investigated variables showed significant statistical relationship to prognosis.
Discussion
The prevalence of meningioma in our series among pediatric tumors treated in our hospital in the last 10 years was 1.42%, a finding that confirms the fact of being a rare pediatric tumor, this also can be extracted from the recent literature where the incidence of pediatric meningioma ranges from 2.1 to 3.7% [1,2,3] and it did not exceed 4.6% in previous reports [8]. Even among meningiomas of all ages, pediatric cases constituted only 1.9–2.7% of all meningiomas [1, 9, 10].
We had a nearly equal gender distribution with a very slight male predominance (1.1:1). It was pointed out in other pediatric meningiomas series that there was slight male predominance [3, 9,10,11,12,13,14]. This may be explained by the lack of the effect of estrogen and progesterone on tumor growth as compared to adult meningiomas where there is female predominance.
In the literature, the mean age of presentation ranged from 11.3 up to 15 years [2,3,4, 9, 10, 12, 14,15,16] and it was stated that pediatric meningiomas present late in the first decade or early in the second decade of life [13, 17]. In contrast to this, the mean age of presentation was 7.9 years in our study and this can be partially explained by the aggressive behavior or the higher pathological grade of our cases where atypical and anaplastic meningiomas exceeded the low grade subtype that was the commonest in the other series and it seems to have a more indolent course and present at an older age than the higher grades. However, and in accordance with literature [2, 10, 18, 19], the presence of infantile cases is exceedingly rare where only one case was reported in our series (2.5%) and it was an atypical meningioma with brain invasion which points to a tumor with aggressive behavior as reported in another series [10] where the only infantile case was a sarcomatous meningioma, a finding that confirms the relation between the age at presentation and histopathological grade of the meningioma.
The association between meningioma and NFII is well known and is heavily reported in pediatric meningioma series where the incidence of NFII ranged widely from 3.7 up to 45.5% [1, 8, 9, 11, 13,14,15, 17, 20,21,22,23,24] and while some series reported zero incidence of NFII cases, our series had a comparable incidence to most of literature (10%). NFII used to be considered a risk factor for development of meningiomas [4, 7] but its presence did not influence the clinical and pathological features of the meningiomas. All NFII cases in our study were characterized by presenting at an older age (more than 11 years old) and the mass effect of meningiomas was the cause of presentation or complaint in those patients. It should be noted also that the presenting lesions were either spinal (3 cases) or optic nerve sheath (1 case) although all the 4 cases had multiple lesions, a finding that should direct physicians to search for neurofibromatosis signs and lesions in those children present with meningiomas at these two specific anatomic locations.
Radiation exposure is considered as another risk factor for development of meningioma and according to some investigators, it was associated with 40% of the cases in their series [3]. In contrast to this, some other series [1, 13, 21] as well as ours did not include any radiation-induced meningioma. Some authors reported that the risk for development of high-dose cranial irradiation-induced meningioma was increasing with the length of follow-up [25].
The pathology of pediatric meningiomas as opposed to that of adults is characterized by being of higher grade and of mixed or multiple pattern. This was clearly evident in our series; 11 patients (28.2%) and 12 patients (30.7%) were atypical and anaplastic meningiomas, respectively while grade I cases represented 41% of our cases. On the other hand, in most adult meningioma series the high grades collectively represented a smaller number of cases that did not exceed 43% of cases in the largest series [26,27,28,29]. The higher prevalence of atypical and anaplastic meningiomas was reported also in other pediatric series where it reached nearly 73% of cases [30, 31]. Brain invasion was detected in three (7.6%) of our patients (two were WHO grade I and the third was grade II) which reflects a more aggressive behavior.
This aggressive behavior was reported by other investigators to be not only on the phenotypic level but also on the genotypic level and was reported in the immunohistochemical studies as well [16, 30, 31]. It was noted also in our series that in 12 patients, there was more than one histological variant while five patients had foci of different grades in the same location and we had a peculiar NFII patient who had the three grades of meningioma in separate locations, these findings could point to the effect of different molecular and genetic features as (merlin loss, DAL-1 loss, progesterone receptors expression, NF2 deletion, DAL-1 deletion, 1p, and 14 q deletions) and how they correlate with the different histological variants and grades as some investigators found in their results and hypothesized that each focus may progress according to its genetic alterations and they concluded also according to their findings that pediatric and NFII-associated meningiomas are more predisposed towards malignant progression and/or tend to progress at a more rapid rate than their sporadic adult counterparts [22].
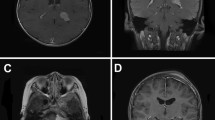
Safe gross total excision is the gold standard in the treatment of pediatric meningiomas and this was what we adopted (Fig. 1) and what was emphasized upon heavily in the literature even on multiple-staged surgeries besides it was favored by some authors for managing regrowth or recurrent cases [10].
A case of 12-year-old male with a right parasagittal pathologically proven transitional meningioma. a–c Preoperative contrast-enhanced MRI. d–f Early postoperative MRI showing total tumor excision. g–i MRI follow-up 6 months postoperatively showing no recurrence. j–l MRI follow-up 1 year postoperatively showing no recurrence
Every attempt for safe total excision was exercised and our whole armamentarium was directed towards this purpose. However, we believe that patient’s safety and good functional outcome must be taken into considerations when planning for the management of pediatric meningiomas and as GTR ensures higher PFS and protects the growing brain from radiation exposure, it entails many surgical challenges owing to some difficult locations and the large sizes reached by these meningiomas in a group of patients with small total blood volumes with all consequences of massive blood transfusions. In our series, GTR was achieved in 72.5% of our cases and this is comparable to other series in the literature with considerable number of cases that are statistically significant [23]. One hundred percent GTR was reported in series with small number of patients [10, 12, 32]. The exact obstacles hindering total excision was not referred to in the literature; however, in our series, the causes of subtotal resection were adherence to optic nerves, large vessels, pituitary stalk, and brain stem invasion in five skull base cases, hypothalamic involvement in a third ventricular meningioma besides the invasion of the spinal cord in two cases.
Intraventricular meningiomas in pediatric age group are not uncommon in contrast to adult population and were reported in the recent literature to have an incidence that ranged from 3 up to 22% among meningiomas in this age group [3, 9,10,11, 13, 23, 33]. This goes in accordance with what was found in our series where we had five intraventricular cases (12%) with the commonest location is the lateral ventricle; three in the atrium and one in the temporal horn, and one case was found to be in the third ventricle. All intraventricular cases in our series were operated through the shortest transcortical route; the three trigonal cases were excised through superior parietal lobule approach, the temporal horn case was approached through middle temporal gyrus approach while the third ventricular one was excised through middle frontal gyrus approach. We believe that transcortical approaches have lower complications than the transcallosal one; they allow for gross total excision as in our cases with easier manipulation, less brain retraction and better control of bleeding with fewer incidence of vascular insults. This can be also perceived from reviewing the literature where most of neurosurgeons preferred this approach [12, 33,34,35].
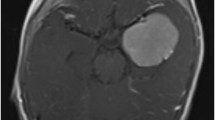
In their series, Dash et al. used the transcallosal route in one of their cases, while the rest of their series was approached via transcortical routes and they achieved gross total excision in all of their cases [12]. Orakdogen et al. also achieved total excision of a giant lateral intraventricular meningioma through the transcortical approach [35]. Even when the total resection was not achieved through the transcortical approach by some authors, they utilized the same approach in other sessions to achieve gross total resection successfully for a large intraventricular lesion extending in both lateral ventricles and through the foramen of monro into the third one [36]. Generally in the literature, the transcallosal approach was noticed to be used mainly in the third ventricular meningiomas [12, 33, 37]. In our series, we achieved GTR in all lateral ventricular cases (Fig. 2) and near total excision of the third ventricular one due to invasion of hypothalamus.
A case of 8-month-old male presented with left lateral intraventricular pathologically proven atypical meningioma. a and b a-c Preoperative contrast-enhanced MRI. c and d d-f Early postoperative MRI showing total tumor excision. MRI follow-up at 6 months (e and f g-i), 18 months (g and h j-l), and 24 months (i and j m-o) showed no tumor recurrence
Spinal pediatric meningiomas were also not uncommon in our series (15.3%) but it was of an unfavorable prognosis and this may be explained by its occurrence mainly in the context of NFII where the prognosis was affected by the concomitant intracranial lesions and the multiplicity of the spinal ones.
5-aminolevulinic acid (5-ALA) is an evolving real-time intraoperative tool that aids in identification of the brain tumors and resection of residual parts and hence total excision can be reached. Its use in meningioma surgery was advocated by many authors who had reported their experience [38, 39]. In our institution, we utilized 5-ALA in one case of a 9-year-old patient who presented with a large parieto-occipital lesion that showed a good illumination after the fluorescence and total excision was achieved revealing atypical meningioma. Atypical meningioma was reported in other studies to show a good bright fluorescence [40], a finding that support the usefulness of 5-ALA in such infiltrative lesions especially when we take in consideration that the pediatric meningiomas are often of high grade or of mixed histopathology with high incidence of brain invasion.
Radiotherapy after gross total or subtotal excision in atypical and anaplastic meningiomas resulted in better outcome and stabilization of the lesions as evident by the 5-year overall survival and event-free survival of 87.8% and 85.6%, respectively (Fig. 3) and only one case showed recurrence in the same site of the lesion.
The mortality in our series (12.8%) is comparable to that reported in most of the series in the literature and in the largest series a mortality rate of 10.6% was reported [23], there was no intraoperative or perioperative mortality in our series and the cause of deaths was due to progression of the lesions that were WHO grade II or III or due to progression of the recurrence which is in accordance with the recent literature where the prognosis improved in the pediatric meningioma after advancement of the surgical techniques, adjuvant and supportive care.
The prognostic factors included the age, gender, NFII status, location of the meningioma, its grade, and the extent of surgical resection. Although the event-free survival rates were obviously higher for gross total resection group and low grade lesions, the P values were not statistically significant for all these factors, and this may be correlated to the small number of cases, but these factors were assessed by other investigators and were found to be the most important factors influencing the prognosis [13] while others mentioned the total excision [2, 21] and the initial histopathology [2] of the lesion as the main prognostic factors. In a larger series with a significant number of patients (87 cases), the authors found that only the WHO grade of the meningiomas was significantly related to the recurrence-free survival rates [23].
Further assessment and statistical analysis is required in the future for a larger scale of patients harboring this rare pediatric disease.
Conclusion
Pediatric CNS meningiomas are uncommon pediatric tumors but of an aggressive clinical and pathological behaviors as compared to adult meningiomas. The presence of NFII is associated with a poorer prognosis and functional outcomes. Although being challenging, the maximum and safe surgical excision should be exercised even in recurrent cases in order to achieve the best outcome. Adjuvant radiotherapy provides good tumor control for inoperable residual atypical or anaplastic meningiomas.
References
Maranhao-Filho P, Campos JC, Lima MA (2008) Intracranial meningiomas in children: ten-year experience. Pediatr Neurol 39(6):415–417
Ravindranath K, Vasudevan MC, Pande A, Symss N (2013) Management of pediatric intracranial meningiomas: an analysis of 31 cases and review of literature. Childs Nerv Syst 29(4):573–582
Santos MV, Furlanetti L, Valera ET, Brassesco MS, Tone LG, de Oliveira RS (2012) Pediatric meningiomas: a single-center experience with 15 consecutive cases and review of the literature. Childs Nerv Syst 28(11):1887–1896
Kotecha RS, Junckerstorff RC, Lee S, Cole CH, Gottardo NG (2011) Pediatric meningioma: current approaches and future direction. J Neuro-Oncol 104(1):1–10
Kotecha RS, Pascoe EM, Rushing EJ, Rorke-Adams LB, Zwerdling T, Gao X, Li X, Greene S, Amirjamshidi A, Kim SK, Lima MA (2011) Meningiomas in children and adolescents: a meta-analysis of individual patient data. Lancet Oncol 12(13):1229–1239
Albrecht S, Goodman JC, Rajagopolan S, Levy M, Cech DA, Cooley LD (1994) Malignant meningioma in Gorlin’s syndrome: cytogenetic and p53 gene analysis. Case report. J Neurosurg 81:466–471
Sieb JP, Puist S-M, Buch A (1992) Familial CNS tumours. J Neurol 239:343–344
Gao X, Zhang R, Mao Y, Wang Y (2009) Childhood and juvenile meningiomas. Childs Nerv Syst 25(12):1571–1580
Lakhdar F, Arkha Y, El Ouahabi A, Melhaoui A, Rifi L, Derraz SE, El Khamlichi A (2010) Intracranial meningioma in children: different from adult forms? A series of 21 cases. Neurochirurgie 56(4):309–314
Mehta N, Bhagwati S, Parulekar G (2009) Meningiomas in children: a study of 18 cases. J Pediatr Neurosci 4(2):61–65
Caroli E, Russillo M, Ferrante L (2006) Intracranial meningiomas in children: report of 27 new cases and critical analysis of 440 cases reported in the literature. J Child Neurol 21(1):31–36
Dash C, Pasricha R, Gurjar H, Singh PK, Sharma BS (2016) Pediatric intraventricular meningioma: a series of six cases. J Pediatr Neurosci 11(3):193–196
Liu Y, Li F, Zhu S, Liu M, Wu C (2008) Clinical features and treatment of meningiomas in children: report of 12 cases and literature review. Pediatr Neurosurg 44(2):112–117
Thuijs NB, Uitdehaag BM, Van Ouwerkerk WJ, van der Valk P, Vandertop WP, Peerdeman SM (2012) Pediatric meningiomas in the Netherlands 1974–2010: a descriptive epidemiological case study. Childs Nerv Syst 28(7):1009–1015
Burkhardt JK, Neidert MC, Grotzer MA, Krayenbühl N, Bozinov O (2013) Surgical resection of pediatric skull base meningiomas. Childs Nerv Syst 29(1):83–87
Sandberg DI, Edgar MA, Resch L, Rutka JT, Becker LE, Souweidane MM (2001) MIB-1 staining index of pediatric meningiomas. Neurosurgery 48(3):590–597
Erdincler P, Lena G, Sarioğlu AC, Kuday C, Choux M (1998) Intracranial meningiomas in children: review of 29 cases. Surg Neurol 49(2):136–140
Molleston MC, Moran CJ, Roth KA, Rich KM (1994) Infantile meningioma. Pediatr Neurosurg 21(3):195–200
Perry A, Dehner LP (2003) Meningeal tumors of childhood and infancy: an update and literature review. Brain Pathol 13(3):386–408
Arivazhagan A, Devi BI, Kolluri SV, Abraham RG, Sampath S, Chandramouli BA (2008) Pediatric intracranial meningiomas–do they differ from their counterparts in adults? Pediatr Neurosurg 44(1):43–48
Li X, Zhao J (2009) Intracranial meningiomas of childhood and adolescence: report of 34 cases with follow-up. Childs Nerv Syst 25(11):1411–1417
Perry A, Giannini C, Raghavan R, Scheithauer BW, Banerjee R, Margraf L, Bowers DC, Lytle RA, Newsham IF, Gutmann DH (2001) Aggressive phenotypic and genotypic features in pediatric and NF2-associated meningiomas: a clinicopathologic study of 53 cases. J Neuropathol Exp Neurol 60(10):994–1003
Rushing EJ, Olsen C, Mena H, Rueda ME, Lee YS, Keating RF, Packer RJ, Santi M (2005) Central nervous system meningiomas in the first two decades of life: a clinicopathological analysis of 87 patients. J Neurosurg Pediatr 103(6):489–495
Teixidor P, Guillén A, Cruz O, Costa JM (2008) Intracranial meningiomas in children: report of 10 cases. Neurocirugia (Asturias, Spain) 19(5):434–439
Strojan P, Popović M, Jereb B (2000) Secondary intracranial meningiomas after high-dose cranial irradiation: report of five cases and review of the literature. Int J Radiat Oncol Biol Phys 48(1):65–73
Bi WL, Corroller T, Greenwald NF, Huynh E, Abedalthagafi M, Aizer A, Santagata S, Al-Mefty O, Alexander B, Dunn IF, Huang R (2017) Radiographic prediction of meningioma grade and genomic profile. J Neurol Surg Part B: Skull Base 78(S 01):A109
Gousias K, Schramm J, Simon M (2016) The Simpson grading revisited: aggressive surgery and its place in modern meningioma management. J Neurosurg 125(3):551–560
Lee SH, Lee YS, Hong YG, Kang CS (2014) Significance of COX-2 and VEGF expression in histopathologic grading and invasiveness of meningiomas. Apmis 122(1):16–24
Sade B, Chahlavi A, Krishnaney A, Nagel S, Choi E, Lee JH (2007) World Health Organization grades II and III meningiomas are rare in the cranial base and spine. Neurosurgery 61(6):1194–1198
Babu S, Uppin SG, Uppin MS, Panigrahi MK, Saradhi V, Bhattacharjee S, Sahu BP, Purohit AK, Challa S (2011) Meningiomas: correlation of Ki67 with histological grade. Neurol India 59(2):204–207
Hui M, Uppin MS, Saradhi MV, Sahu BP, Purohit AK, Sundaram C (2015) Pediatric meningiomas an aggressive subset: a clinicopathological and immunohistochemical study. J Postgrad Med 61(1):32–35
Nazeem WM, El-Beltagy M, Kamal HM (2012) Intracranial meningiomas in children: surgical experience. Egypt J Neurol, Psychiatry Neurosurg 49(3):219–224
Li Z, Li H, Jiao Y, Ma J, Wang S, Cao Y, Zhao J (2018) Clinical features and long-term outcomes of pediatric intraventricular meningiomas: data from a single neurosurgical center. Neurosurg Rev 41(2):525–530
Liu M, Wei Y, Liu Y, Zhu S, Li X (2006) Intraventricular meninigiomas: a report of 25 cases. Neurosurg Rev 29(1):36–40
Orakdöğen M, Somay H, Berkman Z, Aker F (2009) Giant intraventricular meningioma in childhood. İstanbul Tıp Fakültesi Dergisi 72(2):58–60
Kwee LE, van Veelen-Vincent ML, Michiels EM, Kros JM, Dammers R (2015) The importance of microsurgery in childhood meningioma: a case report. Childs Nerv Syst 31(1):161–165
Song KS, Park SH, Cho BK, Wang KC, Phi JH, Kim SK (2008) Third ventricular chordoid meningioma in a child: case report. J Neurosurg Pediatr 2(4):269–272
Millesi M, Kiesel B, Mischkulnig M, Martínez-Moreno M, Wöhrer A, Wolfsberger S, Knosp E, Widhalm G (2016) Analysis of the surgical benefits of 5-ALA–induced fluorescence in intracranial meningiomas: experience in 204 meningiomas. J Neurosurg 125(6):1408–1419
Motekallemi A, Jeltema HR, Metzemaekers JD, van Dam GM, Crane LM, Groen RJ (2015) The current status of 5-ALA fluorescence-guided resection of intracranial meningiomas—a critical review. Neurosurg Rev 38(4):619–628
Scheichel F, Ungersboeck K, Kitzwoegerer M, Marhold F (2017) Fluorescence-guided resection of extracranial soft tissue tumour infiltration in atypical meningioma. Acta Neurochir 159(6):1027–1031
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
El Beltagy, M.A., Enayet, A., Atteya, M.M. et al. Management of pediatric CNS meningiomas: CCHE-57357 experience in 39 cases. Childs Nerv Syst 35, 1323–1331 (2019). https://doi.org/10.1007/s00381-019-04156-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-019-04156-6