Abstract
In order to study the clinical characteristics of intraventricular meningiomas, we analyzed retrospectively 25 patients and reviewed the literature with regard to incidence, clinical manifestation, imaging features, preoperative diagnosis, surgical findings, and histopathological results. Intraventricular meningiomas are quite rare, but they represent an important differential diagnosis of intraventricular neoplasms. Computed tomography or magnetic resonance imaging enable a correct diagnosis of intraventricular meningiomas in most of the cases. The tumors often grow slowly to a substantial size before they become symptomatic. The operative route should be selected according to the tumor’s location. Out of the 24 lateral ventricular meningiomas in our series, 20 were resected via a posterior parieto-occipital transcortical approach, two were resected via a transcallosal approach, and another two tumors, located in the frontal horn and body of the lateral ventricle, were resected via a frontal approach. A median suboccipital craniotomy was performed for the fourth ventricular meningioma. The parieto-occipital route for lateral ventricular meningiomas is a safe surgical approach, which is not necessarily associated with postoperative visual deficits. Piecemeal removal of the tumor can be safely and easily performed and special attention should be paid to the choroidal vessels intraoperatively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meningiomas are generally known to be solid tumors and their classical appearance on the computed tomography (CT) scan and magnetic resonance imaging (MRI) usually leads to a correct diagnosis. The primary occurrence of meningiomas in the ventricular system without dural attachment is extremely rare, with an incidence of 0.5–2% among all intracranial meningiomas [14, 22]. According to previous reports [1–3, 5, 6, 10, 17, 29], their distribution is 77.8% in the lateral ventricular trigone, 15.6% in the third ventricle and 6.6% in the fourth ventricle. Twenty–five patients with intraventricular meningiomas out of a series of 675 cases of meningiomas were treated in our hospital from September 1989 to September 2003, whose diagnosis was confirmed by operation and pathology. We analyzed retrospectively 25 cases and reviewed the literature with regard to incidence, clinical manifestation, imaging features, preoperative diagnosis, surgical findings, and histopathological results.
Materials and methods
Clinical materials
Eight patients were male and 17 were female, whose age ranged between 15 and 63 years old with a mean of 39 years in this series. The duration of initial symptoms prior to definitive diagnosis was 15 days to 10 years. Twenty–four tumors were located in the lateral ventricles and one in the fourth ventricle . One patient suffered from neurofibromatosis type II. Headache was seen in 21 patients and vomiting in 15 patients. Cognitive and personality disturbance, such as memory disturbance, mental exhaustion and dullness, were seen in 12 patients. Motor disturbance was noticed in eight patients, representing mostly a hemi- or monoparesis. Many complaints were episodic or transient, thus delaying the diagnosis in most patients. One case was found by CT scanning after head trauma by accident. The only case of fourth ventricular meningioma presented primarily with headaches, vertigo and ataxia. On neurologic examination the most common signs in patients with lateral ventricular meningiomas were papilledema (12 patients), corticospinal signs (seven patients) varying from spastic hemiparesis to mild hemi- or monoparesis, which was followed by homonymous hemianopia (five patients). Dysphasia was apparent in three patients. The symptoms and signs of the 25 patients are listed in Table 1.
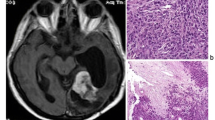
A preoperative cranial CT with contrast enhancement was performed in all patients. Seventeen tumors were located in the left lateral ventricle and seven were in the right lateral ventricle. Most of them arose typically in the trigone. Two meningiomas were found near the foramen of Monro, which extended to the opposite ventricle. Two tumors were located in the frontal horn and body of the lateral ventricle. One patient had neurofibromatosis (NF) type II who underwent a left acoustic neuroma resection with good results 8 years previously. There was one in the fourth ventricle. Tumor size ranged from 1.5 to 7 cm, with five tumors (20.8%) <3 cm and 20 tumors (83.3%) >3 cm in diameter. Increased density and smooth margins were present in most cases (19 patients). Calcification was found in eight cases. Lobulation and an irregular margin were seen in six cases. All tumors were contrast enhanced and enhancement was homogenous in 22 cases and heterogenous in three cases. Local dilatation of the posterior and temporal horn of the affected side was present in all trigonal ventricles. In the case of fourth ventricular meningioma, mild hydrocephalus was present. MRI was performed in 18 patients. The tumors were isointense with gray matter on both T1- and T2-weighted images with strong contrast enhancement. Homogenous gadolinium enhancement was present in 16 patients and heterogenous enhancement in two patients. Signal voids because of calcification were visible in six cases. Carotid and vertebral angiography was performed in four cases of lateral ventricular meningiomas. All four cases of lateral ventricular meningiomas obtained their vascular supply from both anterior and posterior choroidal circulations.
Treatment and results
All meningiomas were microsurgically excised. Out of the 24 lateral ventricular meningiomas, 20 were resected via a posterior parieto-occipital transcortical approach. Two meningiomas which extended to the opposite side were resected via a transcallosal approach. Two tumors, located in the frontal horn and body of the lateral ventricle, were resected via a frontal approach. For the fourth ventricular meningioma a median suboccipital craniotomy was performed with opening of the foramen magnum. The tumor was removed through the foramen of Magendie with total resection. Out of the 24 lateral ventricular meningiomas, total resection was achieved in 21 cases and subtotal resection was performed in three cases, including two by transcallosal approach and one by parieto-occipital approach. All lateral ventricular meningiomas showed an attachment to the choroid plexus. Partial calcification was intraoperatively detected in eight tumors. An intraventricular drain was left in all patients after removal of lateral ventricular meningiomas for 5–7 days. No operative mortality was recorded. Histologic examinations revealed ten lateral ventricular meningiomas to be of the fibromatous type, seven of the meningotheliomatous type, two of angiomatous, two of mixed type and one each of transitional, psammomatous, and atypical type. The histological type of the fourth ventricular meningiomas was mixed.
Headache resolved in all patients mostly immediately after surgery. Three patients out of 12 with cognitive disturbance showed improvement and nine remained the same. Hemianopia improvement was seen in five out of seven cases of lateral ventricular meningioma. Motor disturbance resolved in six out of eight patients. Of the four patients presenting with vertigo, all had complete resolution after resection. Dysphasia also resolved in all three patients. Ataxia showed improvement in three of four patients. No postoperative hydrocephalus developed. In two cases, new hemianopia occurred postoperatively and remained unchanged during the long-term follow-up. One patient developed postoperative seizure that was controlled by appropriate antiepileptic medication. Postoperative hemiparesis occurred in three cases, which recovered in one case and remained unchanged in two cases. The patients were followed up from 6 months to 15 years. Two of three patients with subtotal resection recurred, which were reoperated without causing any new morbidity.
Discussion
Incidence
Meningiomas arising within the ventricular system constitute approximately 0.5–2% of all intracranial meningiomas. However, the incidence in our series is 3.7%. They most commonly arise in the trigone of the lateral ventricle, and they are slightly more common on the left. Meningiomas rarely may arise in the third ventricle, although this is more common in childhood [4, 20, 26]. A total of 532 intraventricular meningiomas had been reported up until 2003 [29]. Among them 414 occurred in the lateral ventricles (77.8%), 83 in the third ventricle (15.6%), and 35 in the fourth ventricle (6.6%). Intraventricular meningiomas show a female predominance of approximately 2:1, in which the representation by females varies from 41% to as high as 82% [4]. In our series, there were 17 females and eight males, showing a female preference. Although there is a wide age range, intraventricular meningiomas are most common over the age of 30 years, and the majority present in the third to the sixth decades [12, 14, 25].
Etiology and clinical manifestations
The origin of intraventricular meningiomas is uncertain, although they appear to arise either from the stroma of the choroid plexus or from rests of arachnoid tissue within the choroid[14]. This explains their frequent occurrence in the trigone, and at postmortem, they can be seen to arise from the choroid plexus via a vascular pedicle.
Most of the clinical symptoms of intraventricular meningiomas are related to increased intracranial pressure, but symptoms can also be caused by direct pressure on the surrounding brain structures. The tumors often grow slowly to a substantial size before they become symptomatic, unless the lesion is located in a region where it interferes with CSF circulation early on. The clinical presentation is variable and usually occurs when the tumors are very large [14, 25]. Presentation with subarachnoid hemorrhage has been described [30]. The clinical presentation is indistinguishable from aneurysmal subarachnoid hemorrhage. As mentioned previously by Delandsheer [7] in his review of 175 cases from the literature, one can summarize that patients with lateral ventricular meningiomas often present with a clinical syndrome, suggesting both a posterior cranial fossa lesion and a cerebral hemisphere lesion with intermittent and paroxysmal nature of some symptoms.
Radiological appearance and diagnosis
CT and MRI now are the safest and certainly the most accurate modality for diagnosing these tumors. The appearance on imaging studies is similar to that of other meningiomas, being sharply defined and globular. On CT scans, these tumors are usually hyperdense with contrast enhancement and may contain foci of calcification [20–22]. Hydrocephalus produced by lateral intraventricular meningiomas is usually localized to the ipsilateral trigone and temporal horn [20]. Meningiomas are iso- or hypointense on T1-weighted MR images, and iso- or hyperintense on T2—weighted images with strong contrast enhancement. Areas of necrosis and cystic change may be present [15, 27, 29, 31]. In our series, homogenous gadolinium enhancement was present in 16 patients and heterogenous enhancement in two patients. In our opinion, in patients with medium-sized tumors, angiography is probably not needed since the blood supply from the choroidal arteries can be found after internal decompression of the tumor. However, when the tumor is large, the study may provide useful information on the location of the feeding arteries.
Intraventricular meningioma is the most common intraventricular tumor of the trigone in adults [16]. The main differential diagnosis of a tumor located in the trigone of the lateral ventricle should include choroid plexus papilloma in patients under 10 years of age; low-grade gliomas, such as ependymoma, oligodendroglioma, and low-grade astrocytoma, in patients between 10 and 40 years of age; and metastases, lymphoma, and meningioma after the fourth decade of life [16, 22, 24].
Operative technique and prognosis
Various surgical approaches to lateral ventricular meningiomas in their much more common trigonal location have been advocated in the past [29]. A transfrontal approach was reported by Busch. Cushing proposed a temporoparietal approach. In 1960, Cramer mentioned the merits of a posterior parieto-occipital incision, and Fornari et al. [12] systematically used this technique in their 1981 series. A parieto-occipital interhemispheric parasplenial approach with incision in the precuneal area was performed by Yasargil for surgical removal of splenial and para-atrial tumors or arterio-venous malformations [29]. The posterior middle frontal and posterior middle temporal approaches were suggested by several authors because of the advantage of an initial access to the anterior choroidal artery [4, 7, 8]. The posterior transcallosal approach was suggested by Kempe and Blaylock [19] to remove tumors in the ventricular trigone of the dominant hemisphere . Others also favored this approach with slight modifications [13, 18, 32]. This approach is useful to attack tumors occupying the middle body of both lateral ventricles and tumors with bilateral ventricular extension. However, a disconnection syndrome may develop when operated on by this approach. In our series of 24 lateral ventricular meningiomas, 20 were resected via a posterior parieto-occipital transcortical approach. The choroidal vessels can be controlled after debulking the tumor by piecemeal removal, usually lying underneath via the parieto-occipital route. Regarding the risk of damage to the optic radiation, the parieto-occipital approach does not itself cause visual damage. The optic radiation runs inferolaterally to the ventricles as shown by anatomic studies [11], and the ventricular trigone can be reached through a parietooccipital route without interrupting the optic radiation. Two meningiomas which extended to the opposite side were resected via a transcallosal approach without occurrence of disconnection sydrome. Two tumors, located in the frontal horn and body of the lateral ventricle, were resected via a frontal approach. During the operative procedure, special attention should be paid to choroidal vessels. In our opinion, the size, location and vascularity of the tumors are the main risk factors for total resection. Cortical incision should be carefully planned before operation, Internal decompression of the tumor, when necessary, should be considered in order to minimize brain retraction, and thus to minimize the postoperative neurological deficits. And occlusion of the choroidal artery branches should be done as early as possible. The operative microscope, microsurgical technique and use of the ultrasonic aspirator allow a piecemeal and almost total removal of such tumors. The operative mortality reported in the majority of the series ranged from 0 to 42% [12]. In one series none of the patients died after microsurgical procedures. Out of the 24 lateral ventricular meningiomas, total resection was achieved in 21 cases and subtotal resection was performed in three cases, including two by transcallosal approach and one by parieto-occipital approach. Postoperative epileptic seizures were reported in 29% of patients operated on via a parieto-occipital route in one series [12]. The transcotical-transventricular approach involves incision in the brain parenchyma and risk of seizure. In our series, one patient developed postoperative seizure that was controlled by appropriate antiepileptic medication. In our group, an intraventricular drain was left in all patients for lateral-ventricular tumors for about 5–7 days, which we think is a effective to avoid postoperative hydrocephalus by draining out the blood in ventricular system. Two of three patients with subtotal resection recurred during the follow-up periods and were reoperated without causing any new morbidity. Subtotal resection is the main cause of recurrence. As intreventricular meningiomas are benign tumors, reoperation is recommended according to the size and location of recurrent tumors. Although the specific biological response of radiotherapy on meningiomas is not well understood, it is clear that the response occurs slowly and progressively. We think radiotherapy can be used as an adjunctive treatment for residual tumors, even for small tumors.
In conclusion, intraventricular meningiomas represent an important differential diagnosis of intraventricular neoplasms. CT or MRI imagings enable a correct diagnosis of intraventricular meningioas in most of the cases. Microsurgical techniques allow a piecemeal and almost total removal of such tumors. The operative route should be selected according to the tumor location. Special attention should be paid to choroidal vessels. The parieto-occipital transcotical route for lateral ventricular meningioas is a safe surgical approach, which is not necessarily associated with postoperative visual deficits.
References
Bret P, Gharbi S, Cohadon F, Remond J (1989) Meningioma of the lateral ventricle. Three recent cases. Neurochirurgie 35:5–12
Caner H, Acikgoz B, Ozgen T, Colak A, Onol B (1992) Meningiomas of the lateral ventricle. Report on six cases. Neurosurg Rev 15:303–306
Ceylan S, Ilbay K, Kuzeyli K, Kalelioglu M, Akturk F, Ozoran Y (1992) Intraventricular meningioma of the fourth ventricle. Clin Neurol Neurosurg 94:181–184
Criscuolo GR, Symon L (1986) Intraventricular meningioma. A review of 10 cases of the National Hospital, Queen Square (1974–1985) with reference to the literature. Acta Neurochir (Wien) 83:83–91
Cummings TJ, Bentley RC, Gray L, Check WE, Lanier TE, McLendon RE (1999) Meningioma of the fourth ventricle. Clin Neuropathol 18:265–269
de la Sayette V, Rivaton F, Chapon F, Hubert P, Ganem F, Houtteville JP (1991) Meningioma of the third ventricle. Computed tomography and magnetic resonance imaging. Neuroradiology 33:354–356
Delandsheer JM (1965) Meningiomas of the lateral ventricle. Neurochirurgie 11:3–83
Delatorre E, Alexander E Jr, Davis CH Jr, Crandell DL (1963) Tumors of the lateral ventricles of the brain. Report of eight cases, with suggestions for clinical management. J Neurosurg 20:461–470
Delfini R, Acqui M, Oppido PA, Capone R, Santoro A, Ferrante L (1991) Tumors of the lateral ventricles. Neurosurg Rev 14:127–133
Diaz P, Maillo A, Morales F, Gomez–Moreta JA, Hernandez J (1990) Multiple meningiomas of the fourth ventricle in infancy: case report. Neurosurgery 26:1057–1060
Ebeling U, Reulen HJ (1988) Neurosurgical topography of the optic radiation in the temporal lobe. Acta Neurochir (Wien) 92:29–36
Fornari M, Savoiardo M, Morello G, Solero CL (1981) Meningiomas of the lateral ventricles. Neuroradiological and surgical considerations in 18 cases. J Neurosurg 54:64–74
Gilsbach JM, Eggert HR, Hassler W (1985) Possibilities and limits of the midline interhemispheric approach. Acta Neurochir Suppl (Wien) 35:84–88
Guidetti B, Delfini R, Gagliardi FM, Vagnozzi R (1985) Meningiomas of the lateral ventricles. Clinical, neuroradiologic, and surgical considerations in 19 cases. Surg Neurol 24:364–370
Hattingen E, Pilatus U, Good C, Franz K, Lanfermann H, Zanella FE (2003) An unusual intraventricular haemangiopericytoma: MRI and spectroscopy. Neuroradiology 45:386–389
Jelinek J, Smirniotopoulos JG, Parisi JE, Kanzer M (1990) Lateral ventricular neoplasms of the brain: differential diagnosis based on clinical, CT, and MR findings. AJNR Am J Neuroradiol 11:567–574
Johnson MD, Tulipan N, Whetsell WO, Jr (1989) Osteoblastic meningioma of the fourth ventricle. Neurosurgery 24:587–590
Jun CL, Nutik SL (1985) Surgical approaches to intraventricular meningiomas of the trigone. Neurosurgery 16:416–420
Kempe LG, Blaylock R (1976) Lateral-trigonal intraventricular tumors. A new operative approach. Acta Neurochir (Wien) 35:233–242
Kendall B, Reider–Grosswasser I, Valentine A (1983) Diagnosis of masses presenting within the ventricles on computed tomography. Neuroradiology 25:11–22
Kloc W, Imielinski BL, Wasilewski W, Stempniewicz M, Jende P, Karwacki Z (1998) Meningiomas of the lateral ventricles of the brain in children. Childs Nerv Syst 14:350–353
Lang I, Jackson A, Strang FA (1995) Intraventricular hemorrhage caused by intraventricular meningioma: CT appearance. AJNR Am J Neuroradiol 16:1378–1381
Lapras C, Deruty R, Bret P (1984) Tumors of the lateral ventricles. Adv Tech Stand Neurosurg 11:103–167
Majos C, Cucurella G, Aguilera C, Coll S, Pons LC (1999) Intraventricular meningiomas: MR imaging and MR spectroscopic findings in two cases. AJNR Am J Neuroradiol 20:882–885
Mani RL, Hedgcock MW, Mass SI, Gilmor RL, Enzmann DR, Eisenberg RL (1978) Radiographic diagnosis of meningioma of the lateral ventricle. Review of 22 cases. J Neurosurg 49:249–255
Markwalder TM, Markwalder RV, Markwalder HM (1979) Meningioma of the anterior part of the third ventricle. Case report. J Neurosurg 50:233–235
McDermott MW (2003) Intraventricular meningiomas. Neurosurg Clin N Am 14:559–569
Morrison G, Sobel DF, Kelley WM, Norman D (1984) Intraventricular mass lesions. Radiology 153:435–442
Nakamura M, Roser F, Bundschuh O, Vorkapic P, Samii M (2003) Intraventricular meningiomas: a review of 16 cases with reference to the literature. Surg Neurol 59:491–503; discussion 503–494
Smith VR, Stein PS, MacCarty CS (1975) Subarachnoid hemorrhage due to lateral ventricular meningiomas. Surg Neurol 4:241–243
Tekkok IH, Cagavi F, Gungen Y (2002) FLAIR-positive MRI in an unenhancing meningioma of the third ventricle. Br J Neurosurg 16:392–393
Waga S, Shimosaka S, Kojima T (1985) Arteriovenous malformations of the lateral ventricle. J Neurosurg 63:185–192
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, M., Wei, Y., Liu, Y. et al. Intraventricular meninigiomas: a report of 25 cases. Neurosurg Rev 29, 36–40 (2006). https://doi.org/10.1007/s10143-005-0418-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-005-0418-1