Abstract
Background
Quadrigeminal cistern arachnoid cysts (QACs) are difficult to treat because of their deep location and the presence of nervous and vascular structures of the pineal–quadrigeminal region. There are several surgical procedures available for QACs, including craniotomy and cyst excision or fenestration, ventriculoperitoneal or cystoperitoneal shunting, and endoscopic fenestration. There is a debate about which method is the best.
Objective
The aim of this study is to evaluate the effectiveness and safety of endoscopic ventriculocystostomy (VC) and third ventriculostomy (ETV) for treatment of arachnoid cysts of the quadrigeminal cistern.
Methods
Twenty-eight patients with QACs who had undergone endoscopic treatment in our department between August 2007 and June 2014 were studied retrospectively. Patient age at the time of endoscopic treatment ranged from 5 months to 42 years, including 25 children (14 males and 11 females) and 3 adults (one male and two females). All patients presented with hydrocephalus and did not undergo shunting prior to neuroendoscopic surgery. The first endoscopic procedures included lateral ventricle cystostomy (LVC) together with ETV in 18 cases, third ventricle cystostomy (3rd VC) together with ETV in 3 cases, and double VC (3rd VC and LVC) together with ETV in 7 cases. Data were obtained on clinical and neuroradiological presentation, indications to treat, surgical technique, complications, and the results of clinical and neuroradiological follow-up.
Results
Complete success was achieved in 25 (89.3 %) of 28 cases. During the follow-up period, one case underwent endoscopic reoperation with success. Shunts were implanted in 2 patients due to progression of symptoms and increase in hydrocephalus after the first endoscopic operation. Shunt independency was achieved in 26 (92.9 %) of 28 cases. The cyst was reduced in size in 22 cases (78.6 %). Postoperative images showed a reduction in the size of the ventricles in 23 cases (82.1 %). There was no surgical mortality. Subdural collection developed in 4 cases (14.3 %) and required a transient subduroperitoneal shunt in 2 cases, whereas the other 2 patients were asymptomatic and did not require any surgical treatment.
Conclusions
VC together with ETV through precoronal approach is an effective treatment for symptomatic QACs and should be the initial surgical procedure. The surgical indications should include signs of elevated ICP (including increased head circumference), Parinaud syndrome, gait ataxia, and nystagmus. Also, surgery is indicated by progressive enlargement of the cyst and young children with large cysts even if the patients are asymptomatic. Contraindications to surgery include the absence of symptoms (older children and adult) and isolated developmental delay. The main criterion for successful surgery should be improvement of clinical symptoms instead of reduced cyst volume and/or ventricular size. Repeated endoscopic procedures may be considered only for the patients whose symptoms improved after first endoscopic operation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Endoscopic surgery has been advocated for treatment of arachnoid cysts. Shim et al. studied 209 patients with arachnoid cysts and suggested that endoscopic procedures were superior to large craniotomy or shunting, which are associated with a number of complications [1]. Many other authors have also stated that endoscopic therapy should be the first choice for the treatment of intracranial arachnoid cysts [2–6]. Quadrigeminal cistern arachnoid cysts (QACs) are rare, accounting for 5–10 % of all intracranial arachnoid cysts [7, 8]. Currently, there are three types of surgical methods for QACs: ventriculoperitoneal or cystoperitoneal shunting, microscopic craniotomy for cystocisternotomy and partial cyst excision, and endoscopic fenestration. To obtain more information about endoscopic surgery in order to further assess its role as a surgical method for treating patients with QACs, we obtained and analyzed the clinical data of 28 patients with QACs who have been performed with endoscopic ventriculocystostomy (VC) together with third ventriculostomy (ETV) in our department.
Patients and methods
Patients
A total of 28 cases with symptomatic QACs undergoing surgical treatment in Beijing Tiantan Hospital between August 2007 and June 2014 were selected. The patients who underwent previous shunts were not included in this study. Patient age at the time of endoscopy ranged from 5 months to 42 years, including 25 children (14 males and 11 females) and 3 adults (one male and two females). All patients presented with hydrocephalus. Signs of increased intracranial pressure (headache, drowsiness, bulging fontanel, visual impairment, and macrocrania) were the most common symptoms (24/28, 85.7 %). Psychomotor retardation and gait ataxia were each present in 5 patients (5/28, 17.9 %). Parinaud syndrome was present in 3 patients (3/28, 10.7 %). Diplopia, hemiparesis, esotropia, and nystagmus were each present in 1 patient (1/28, 3.6 %). All patients underwent cranial MRI and CT examinations before operation. All patients underwent the endoscopic procedure as the initial treatment. The clinical details of the 28 patients are presented in Table 1.
Operative technique
-
1.
LVC
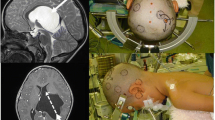
For cysts extending anteriorly toward the lateral ventricle, the endoscope was introduced through a point about 3 cm lateral to the midline and 1 cm anterior to the coronal suture to perform LVC. As determined on preoperative sagittal MRI, the position of the point varied according to the anatomy of the cyst and ventricle so that we could obtain an optimal trajectory to make the LVC fenestration with minimal manipulation. In infants, the entry point is located at the lateral margin of the anterior fontanel. An arc scalp incision and a frontal bur hole are performed to perform ETV and LVC together (Fig. 1). A rigid lens was inserted along a line directed to the imaging line which connected the bilateral external auditory foramens, but the direction deflected slightly to the median line to prevent injury to the thalamus. After using standard anatomical landmarks to confirm visual entry into the right lateral ventricle, the cyst can be observed to be bulging into the lateral ventricle and/or third ventricle (Fig. 2a, b). Then, the endoscope was advanced to the foramen of Monro. If possible, ETV was firstly performed because the bleeding may occur during LVC procedure, which may prevent ETV to be performed safely (Fig. 2c–e). After perforation of the floor of third ventricle, flow of CSF through the hole was usually seen, and the basilar artery in the interpeduncular cistern was inspected.
Fig. 1 Fig. 2 a After the endoscope enter lateral ventricle, the dome of the cyst wall can usually be recognized in the region of the ventricular trigone, medially to the choroid plexus. The upper right arrow directs to choroid plexus in right lateral ventricle, the lower right arrow and the left arrow direct to the dome of the cyst in right lateral ventricle. b See the dome of the cyst wall in the third ventricle and the floor of the third ventricle through the foramen of Monro. The upper right arrow directs to the floor of the third ventricle, the lower right arrow directs to the massa intermedia. The upper left arrow directs to the aqueduct, the lower left arrow directs to the dome of the cyst in third ventricle. c The floor of the third ventricle. The upper right arrow directs to saddle back, the lower right arrow directs to the basilar artery. d Perforation of the floor of third ventricle. e See the fenestration of the floor of third ventricle through the foramen of Monro. The upper right arrow directs to the fenestration of the floor of third ventricle, the lower right arrow directs to the dome of the cyst in third ventricle. f The dome of the cyst wall medially to the choroid plexus in right lateral ventricle is opened using electrocautery. g The arrow directs to the fenestration between cyst and lateral ventricle. h See the upper surface of cerebellum through the fenestration between cyst and lateral ventricle
After ETV, the dome of the cyst wall was opened using electrocautery, and the fenestration was enlarged by microscissors and monopolar coagulation (Fig. 2f–h). The cyst wall around fenestration was shrunken by electrocautery.
-
2.
3rd VC
In cases in which bulging of the cyst below the floor of the ventricular trigone is not evident on preoperative studies and the cysts extend anteriorly toward the third ventricle, the VC was created between the third ventricle and the cyst. The bur hole is placed more anteriorly in front of the coronal suture, about 3 cm lateral to the midline and 2 cm anterior to the coronal suture to obtain a trajectory that allows visualization of the posterior third ventricle. Once the third ventricle was entered, the cyst’s top wall came into view in the posterior aspect of the third ventricle. If possible, ETV was firstly performed. After this procedure, A 3rd VC was created.
In some cases, the entire third ventricle was filled by the cyst. A VC was then firstly performed. After decompression of the cyst, the mammillary bodies and floor of the third ventricle usually become visible. Then, ETV can be safely performed.
-
3.
Double VC
In patients whose cysts extended toward both the lateral ventricle and the third ventricle, a double VC (between the lateral ventricle and the cyst and between the third ventricle and the cyst) and ETV were created (Fig. 3a).
Fig. 3 a Preoperative MRI. The red arrows represent the surgical paths to the doom of the cyst in lateral ventricle, third ventricle and the floor of third ventricle through one precoronal bur hole. b MRI image 3 months after surgery. The size of the cyst and ventricle was reduced substantially; the cerebellum was partially restored back to the former position. The red arrow shows that the recanalization of preoperative secondary aqueductal occlusion
Outcome assessment
The patients were clinically assessed postoperatively to determine any improvement of preoperative symptoms or the occurrence of postoperative complications. The CT scans of all the patients were obtained on the day of the surgery, after the procedure. The MRI scans were performed in the first postoperative week and repeated at 3 and 9 months after surgery. Subsequently, MRI was carried out annually. The results were compared with preoperative studies concerning any decrease in cyst size or improvement of hydrocephalus. Any recurrence or progression of symptoms was considered to be an indication for repeating MRI. Recurrence or progression of symptoms associated with an increase in cyst size and/or hydrocephalus on postoperative imaging was considered to be an indication for reoperation. Follow-up of the patients ranged from 8 to 89 months (mean, 48.75 months).
Results
Endoscopic treatment
The first endoscopic procedures included LVC together with ETV in 18 cases, 3rd VC together with ETV in 3 cases, and double VC (3rd VC and LVC) together with ETV in 7 cases.
Postoperative outcomes
Complete success (improvement of preoperative symptoms, normalization of head circumference growth, and control of hydrocephalus and cyst size with no further surgical procedure) was achieved in 25 (89.3 %) of 28 cases. During the follow-up period, one case (case 19) underwent endoscopic reoperation with success because of recurrence of the cyst and hydrocephalus 5 months later. In the operation, the fenestration was found to be closed, and a repeat endoscopic cyst fenestration was performed. In two other patients (case 11 and case 21), a shunt was implanted due to progression of symptoms and increase in hydrocephalus after the first operation. Therefore, shunt independency was achieved in 26 (92.9 %) of 28 cases.
After all the successful surgical procedures, intracranial hypertension symptoms completely disappeared in all patients who presented with such symptoms. Patients with Parinaud syndrome, gait ataxia, visual impairment, and nystagmus also all showed remarkable improvement. However, no improvement was observed with developmental delay.
Postoperative MRI showed a reduction in the cyst size (Fig. 2b) in 22 cases (78.6 %), whereas in the remaining 6 cases (21.4 %) the cyst size was unchanged. A postoperative decrease in ventricular size (Fig. 2b) was encountered in 23 cases (82.1 %).
Complications
There was no surgical mortality. Postoperative subdural hygroma occurred in 4 cases (14.3 %) and required a transient subduroperitoneal shunt in 2 cases, whereas the other 2 patients were asymptomatic and did not require any surgical treatment.
Discussion
Indications for surgery
Because of their intimate relationship with the dorsal midbrain, QACs produce distortion or compression of the cerebral aqueduct at an early stage; therefore, when symptomatic, they are almost invariably associated with hydrocephalus. Symptoms are usually related to hydrocephalus (macrocrania, headache, vomiting, lethargy, and papilledema), compression of cerebellum (gait ataxia), and dorsal midbrain (impairment of upward gaze and other ocular disorders, such as convergence spasmus, abnormality of the pupils, upper lid retraction). Some children also have developmental delay.
With regard to the indications for surgery, it has been recommended that these indications should be strict, and surgeons should confirm whether a patient has the indications for surgery. For patients with symptoms, it is important to obtain a medical history and perform a physical examination, and evaluate diseases and assess the relationship between the cyst and symptoms for each patient before surgery is performed. The size of the cyst is not a factor affecting the clinical determination of surgery. But obvious cyst-related symptoms are an indication for surgery. For patients without symptoms, we believe that surgery is indicated in young children with large cysts even if the cyst is apparently well tolerated because a cyst may affect the development of the brain. However, surgical treatment should not be considered for older children and adults unless they have cyst-related symptoms.
In our series, symptoms of elevated ICP, Parinaud syndrome, gait ataxia, and nystagmus all improved in patients who underwent surgery which was successful, but developmental delay never regressed. This observation has also been reported by other authors [9]. Therefore, with regard to which symptoms indicate surgery, we would argue that surgical indications should include signs of elevated ICP (including increased head circumference), Parinaud syndrome, gait ataxia, and nystagmus. Also, surgery is indicated by progressive enlargement of the cyst and young children with large cysts even if the patients are asymptomatic. Contraindications to surgery include the absence of symptoms (older children and adult) and isolated developmental delay.
There is a debate about whether endoscopic treatment should be performed for the patients younger than 6 months with QACs. Almost all the patients younger than 6 months of age included in the study of Erşahin and Kesikçi [10], who underwent both cyst fenestration and ETV, required a ventriculoperitoneal (VP) shunt postoperatively. But in our group, endoscopy was successful in obtaining shunt independence in a patient younger than 6 months. And in the other report [9], there was also a patient younger than 6 months who got shunt independence after endoscopic fenestration. Our advice is that when a patient with QACs is younger than 6 months, if possible, the endoscopic treatment can be performed until the patient is older than 6 months.
There is also a debate about whether endoscopic treatment should be performed for the patients who have prior shunts. In the study of Nasser [9], all 4 patients who had prior shunts experienced progression of symptoms with an increase in cyst size after endoscopic treatment and required a new shunt placement later. The authors postulated that most of the patients who have preexisting shunts usually remain dependent on the device after endoscopic treatment. Accordingly, endoscopic cyst fenestration is not recommended by the authors in patients who have previously received a shunt. But in the group of Cinalli G [11], endoscopy was successful in obtaining shunt independence in 2 patients (50 %) in 4 patients who had already undergone shunt treatment. The authors believe that neuroendoscopic approaches can be considered an alternative method in the management of patients presenting with shunt malfunction.
In our series, there were also 2 patients who needed shunt after endoscopic treatment. Why is endoscopic treatment a failure in some patients? The reason maybe is that the hydrocephalus of most of the cases is obstructive in nature, but in some cases, the hydrocephalus is attributed to both aqueductal stenosis and deficiency of absorptive capacity for CSF. For the infants or neonates, this is probably due to immaturity of the subarachnoid space. For the patients who had prior shunts, this is probably due to loss of the ability of CSF absorption (shunt dependence).
Choice of surgical procedure
Cystoperitoneal shunting [12] or cyst-cisternal Shunting [13] may lead to early obliteration of the cyst but is associated with a high shunt malfunction rate (as high as 40 %) [12]. Craniotomy and cyst excision or fenestration carries the risk of significant complications such as neurological deficits (hemiparesis or oculomotor palsy), meningitis, subdural hematomas, and seizures. The significant potential morbidity of microsurgical fenestration and the high incidence of complications of shunting prompted neurosurgeons to search for an alternative procedure. The endoscope is an ideal instrument for exploration of fluid-filled cavities, and the close proximity of QACs to the ventricular system and/or the basal cisterns makes such lesions appropriate for endoscopic treatment. QACs are almost invariably associated with hydrocephalus, which makes endoscopic treatment often technically feasible because of the possibility of working in large spaces. Gangemi et al. [14] compared the results of the 16 reviewed cases treated by endoscopy with those of 20 cases treated by craniotomy and cyst excision, shunt of the cyst or ventricles or by combined procedures. The endoscopic group has shown a significantly higher rate (62.5 %) of patients completely cured than the surgical group (35 %). The other advantage of neuroendoscopy is that it avoids a major surgical procedure (craniotomy with the risk of some major complications), and it avoids shunt dependence and all the other shunt-related problems. Kanwaljeet Garg et al. [15] advice that different surgical procedure can be used according the different type of QACs. But there were no case of type 3 QACs (defined by Kanwaljeet Garg et al.) in our series. All the patients in our study were treated using endoscopic procedures.
Endoscopic surgical procedure
There is controversy concerning the need for performing ETV simultaneously with ventriculocystostomy in the treatment of QACs. Cinalli G et al. [11] reported their series of 14 cases. Six patients underwent both VC and ETV, which was completely successful in all patients. Eight patients underwent only VC as the initial endoscopic procedure. This procedure was completely successful in only 1 patient. All the other 7 patients required a second procedure (repeated endoscopy or shunt treatment). We advice that VC should be performed together with ETV for the following two reasons: (1) chronic midbrain compression by the QACs may lead to secondary aqueductal occlusion. In this scenario, VC alone, although allowing for adequate cyst decompression, may not result in extraventricular CSF flow. The ETV serves the purpose of allowing trapped fluid to pass into the basal cisterns and bypass the occluded aqueduct to treat the hydrocephalus. (2) Fenestration of the deep cyst wall toward the basal cistern is another method to bypass the occluded aqueduct. But compared to this method, ETV is more safer and easier.
When ETV performed together with LVC, if possible, we advice that ETV should firstly be performed because it is more dangerous than LVC as ETV is performed in the third ventricle. The bleeding in LVC may prevent ETV to be performed safely. On the other hand, fenestration of the deep wall of the cyst, if ETV has already been performed, does not seem to add significant advantages, and can be omitted to increase the safety of the operation because ETV has opened the way of CSF in ventricular to pass into basal cisterns.
Choice of endoscopic surgical approach
Currently, three endoscopic approaches have been used in the management of QACs: suboccipital supracerebellar cyst fenestration approach [16], precoronal lateral ventricle–cystostomy approach [9–11, 14, 17–19], and precoronal third ventricle–cystostomy approach [9, 11, 14, 19, 20].
The suboccipital supracerebellar approach is made with a paramedian bur hole drilled 2 cm below the external occipital protuberance. The cyst is entered after removal of its posterior wall and the anterior wall is also fenestrated to communicate the cyst with the subarachnoid space. This approach takes advantages of the natural corridor that exists between the superior surface of the cerebellum and the tentorium. However, there are also some disadvantages related to this approach. First, the supracerebellar endoscopic approach may be more easily performed only when the cyst extends downward and posteriorly over the cerebellum to provide enough working space. Second, the endoscopic corridor between cerebellum and tentorium is rather small; the necessary retraction of the cerebellum may result in bleeding from the superior cerebellar bridging veins. Third, the deep incisural veins lie over the cyst wall and may be damaged during the endoscopic procedure; bleeding may not be controlled through the endoscope working channel, also because of the very deep cyst location, and may require the surgeon to enlarge the exposure for a microsurgical approach. Fourth, the transverse sinus region may cause significant hemorrhage. Finally, ETV cannot be performed through this approach.
Compared to the supracerebellar endoscopic approach, precoronal approach LVC and/or 3rd VC has below advantages: (1) it can be performed either through the lateral or the third ventricles using a standard precoronal bur hole. The lateral ventricle–cystostomy may be realized for large cysts that reach a sufficient lateral extension to bulge into the floor of the lateral ventricle and trigone. The third ventricle–cystostomy is indicated when the cyst extends upward and anteriorly protruding through the posterior wall of the third ventricle. If the cyst bulge into both lateral ventricle and third ventricle, double VC (3rd VC and LVC) can be performed together through one precoronal burr hole to get better result. (2) The fenestration is performed in a large cavity with consequent easier surgical maneuvers. (3) It enters the ventricular system first and then the cyst. This should minimize the escape of CSF into the subdural space, reducing the risk of postoperative subdural collections. (4) The precoronal approach may be more safer with no risk of damaging the deep incisural and quadrigeminal veins. (5) ETV can be finished simultaneously though this approach, which increases the chance of remission of the hydrocephalus.
Operative outcome
In the study of Erşahin and Kesikçi [10], endoscopic intervention was successful in 10 (58.8 %) of 17 patients with QACs. Endoscopic procedures were successful in all patients older than 6 months of age. However, 7 (87.5 %) of the 8 patients younger than 6 months old who had undergone both cyst fenestration and ETV needed a VP shunt. In the study of Cinalli [11], complete success was achieved in 7 (50 %) of 14 cases of QACs operated on by endoscopy. With QACs operated on by endoscopy with a mean follow-up of 55 months, among the 10 patients in whom endoscopy was performed as a primary treatment, 1 required the insertion of a VP shunt in the long term (overall success rate 90 %), and 4 patients required a repeat endoscopic procedure. None of the 6 patients operated on using ventriculocystostomy and ETV required any further surgery; however, 7 of the 8 patients operated on by ventriculocystostomy without ETV underwent reoperation (repeat endoscopic cyst fenestration in 4 cases and shunt reimplantation in 3 cases). In the study of Nasser [9], endoscopy was successful in obtaining shunt independency in 13 (92.9 %) of 14 patients without prior shunts; nevertheless, none of the 4 patients with prior shunts was able to become shunt independent. In the present study, complete success was achieved in 25 (89.3 %) of 28 cases. The difference between our series and the other reported series is that all the patients in our series did not undergo shunting prior to neuroendoscopic surgery, and only 2 patients are younger than 6 months old. On the other hand, in our series, postoperative MRI showed a reduction in the cyst size in 22 cases (78.6 %), whereas in the remaining 6 cases (21.4 %), the cyst size was unchanged. A postoperative decrease in ventricular size was encountered in 23 cases (82.1 %). We speculate that the main criterion for successful surgery should be improvement of clinical symptoms instead of reduced cyst volume and/or ventricular size.
During the follow-up period, one case (case 19) had recurrence of the cyst and hydrocephalus 5 months later after the first endoscopic procedure and underwent endoscopic reoperation with success. In the operation, the fenestration was found to be closed. In two other patients (case 11 and case 21), a shunt was implanted due to progression of symptoms and increase in hydrocephalus after the first operation. For the case 19, the symptoms improved after endoscopic operation for 5 months, which show that the endoscopic procedure was effective for the patient and the reason for recurrence is closed fenestration. So, repeated endoscopic procedures may be considered for this kind of patients. For the case 11 and case 21, we do not advice repeated endoscopic procedures because the patients never improved after the endoscopic treatment. The reason of the failure of endoscopic procedures for these patients maybe deficiency or loss of the ability of CSF absorption, which need a shunt rather than repeated endoscopic procedures.
Conclusions
The data of our review, showing a similar rate of good results in the endoscopic surgical groups, suggest that endoscopic fenestration should be performed as the first procedure for patients with symptomatic QACs because it is less invasive and avoids shunt dependency. The endoscopic procedure should include precoronal approach LVC and/or 3VC and ETV. Only the combination of these 2 procedures offers the highest success rate with a single endoscopic procedure.
References
Shim KW, Lee YH, Park EK et al (2009) Treatment option for arachnoid cysts. Childs Nerv Syst 25(11):1459–1466
Greenfield JP, Souweidane MM (2005) Endoscopic management of intracranial cysts. Neurosurg Focus 19(6):E7
Nowosławska E, Polis L, Kaniewska D et al (2006) Neuroendoscopic techniques in the treatment of arachnoid cysts in children and comparison with other operative methods. Childs Nerv Syst 22(6):599–604
Gui SB, Wang XS, Zong XY et al (2011) Assessment of endoscopic treatment for middle cranial fossa arachnoid cysts. Childs Nerv Syst 27(7):1121–1128
Gui SB, Wang XS, Zong XY et al (2011) Suprasellar cysts: clinical presentation, surgical indications, and optimal surgical treatment. BMC Neurol 11:52
Gui S, Zong X, Li C et al (2013) Endoscopic treatment of convexity arachnoid cysts. Childs Nerv Syst 29(3):505–508
Rengachary SS, Watanabe I (1981) Ultrastructure and pathogenesis of intracranial arachnoid cysts. J Neuropathol Exp Neurol 40(1):61–83
Di Rocco C, Caldarelli M (1993) Supratentorial interhemispheric and pineal region cysts. In: Intracranial Cyst Lesions, Raimondi AG, Choux M, Di Rocco C (eds). New York, Berlin: Springer − Verlag Chap 11: 153-168
El-Ghandour NM (2013) Endoscopic treatment of quadrigeminal arachnoid cysts in children. J Neurosurg Pediatr 12(5):521–528
Erşahin Y, Kesikçi H (2009) Endoscopic management of quadrigeminal arachnoid cysts. Childs Nerv Syst 25(5):569–576
Cinalli G, Spennato P, Columbano L et al (2010) Neuroendoscopic treatment of arachnoid cysts of the quadrigeminal cistern: a series of 14 cases. J Neurosurg Pediatr 6(5):489–497
Raffel C, McComb JG (1988) To shunt or to fenestrate: which is the best surgical treatment for arachnoid cysts in pediatric patients? Neurosurgery 23(3):338–342
Ohnishi YI, Fujimoto Y, Taniguchi M et al (2007) Neuroendoscopically assisted cyst-cisternal shunting for a quadrigeminal arachnoid cyst causing typical trigeminal neuralgia. Minim Invasive Neurosurg 50(2):124–127
Gangemi M, Maiuri F, Colella G et al (2005) Endoscopic treatment of quadrigeminal cistern arachnoid cysts. Minim Invasive Neurosurg 48(5):289–292
Garg K, Tandon V, Sharma S et al (2014) Quadrigeminal cistern arachnoid cyst: a series of 18 patients and a review of literature. Br J Neurosurg 12:1–7
Ruge JR, Johnson RF, Bauer J (1996) Burr hole neuroendoscopic fenestration of quadrigeminal cistern arachnoid cyst: technical case report. Neurosurgery 38(4):830–837
Choi JU, Kim DS, Huh R (1999) Endoscopic approach to arachnoid cyst. Childs Nerv Syst 15(6-7):285–291
Sengul G, Tuzun Y, Cakir M et al (2012) Neuroendoscopic approach to quadrigeminal cistern arachnoid cysts. Eurasian J Med 44(1):18–21
Inamasu J, Ohira T, Nakamura Y et al (2003) Endoscopic ventriculo-cystomy for non-communicating hydrocephalus secondary to quadrigeminal cistern arachnoid cyst. Acta Neurol Scand 107(1):67–71
Hayashi N, Endo S, Tsukamoto E et al (1999) Endoscopic ventriculocystocisternostomy of a quadrigeminal cistern arachnoid cyst. Case report. J Neurosurg 90(6):1125–1128
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Rights and permissions
About this article
Cite this article
Gui, S., Bai, J., Wang, X. et al. Assessment of endoscopic treatment for quadrigeminal cistern arachnoid cysts: A 7-year experience with 28 cases. Childs Nerv Syst 32, 647–654 (2016). https://doi.org/10.1007/s00381-015-2962-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2962-5